Abstract
Objective
Positive psychological characteristics have been linked to superior cardiac outcomes. Accordingly, in this exploratory study, we assessed positive psychology interventions in patients who had recently undergone a procedure to treat cardiovascular disease.
Method
Participants were randomly assigned to receive one of three different six-week face-to-face interventions or a wait-list control condition. We assessed intervention feasibility and compared changes in psychological outcome measures post-intervention (7 weeks) and at follow-up (15 weeks) between intervention and control participants. Across the interventions, 74% of assigned sessions were completed.
Results
When comparing outcomes between interventions and control participants (N=55 total), there were no between-group differences post-intervention, but at follow-up intervention participants had greater improvements in happiness (β=14.43, 95% confidence interval [CI]=8.66–20.2, p<.001), depression (β=−3.87, 95% CI=−7.72 to 0.02, p=.049), and hope (β=7.12, 95% CI=1.25–13.00, p=.017), with moderate-large effect sizes. Efficacy of the three interventions was similar.
Conclusions
Future studies are needed to identify an optimal positive psychology intervention for cardiac patients.
Keywords: interventions, happiness, positive psychology, coronary artery disease
Introduction
Coronary artery disease (CAD) is the leading cause of death worldwide (1). making it a major public health problem. Positive psychological constructs, such as optimism and positive affect, are associated with reduced mortality in patients with and without pre-existing cardiac disease (2–4), along with fewer rehospitalizations in heart failure patients (5) and increased survival following cardiac surgery (6). Such effects on cardiac health appear to be independent of negative affective states (4), suggesting that it is not simply an absence of depression that confers the cardiovascular benefit associated with positive emotions.
An intervention that boosts positive psychological well-being has the potential to improve outcomes in patients with cardiovascular disease. Positive psychology interventions (PPIs) aim to cultivate positive psychological states (e.g., optimism, gratitude, positive affect) through systematic exercises, such as performing kind acts, writing a letter of gratitude, or using personal strengths (7–9). These exercises are straightforward, require minimal provider training, and have been found to consistently and substantially increase well-being and reduce depression in healthy persons (10). However, despite the association of positive psychological states with superior cardiac outcomes, there has been little study of PPIs or related programs in cardiac patients (11–13), and none outside the United States.
Accordingly, we adapted three different PPIs based on the literature (7, 8, 14–17) and performed a randomized, controlled pilot trial to determine the feasibility and preliminary efficacy of these interventions compared to a wait-list control condition in a cohort of patients with CAD who had undergone a recent cardiovascular procedure. We hypothesized, similar to effects in American cohorts, that the interventions would be feasible (over two-thirds of participants completing at least 4 of 6 sessions) and that there would be moderate effects of the intervention on outcome variables, both with respect to pre/post changes and when compared to control participants.
Method
Participants and Recruitment
The study was approved by the Ethics Committee at The University of Isfahan. We identified patients who had coronary artery bypass surgery (CABG) or percutaneous coronary intervention (PCI) at one of two local medical centers within the preceding 5 months and lived in the immediate Isfahan area where the study occurred. Both CABG and PCI are utilized for patients with significant stenosis of one or more coronary vessels, signaling that study participants had clinically significant coronary artery disease.
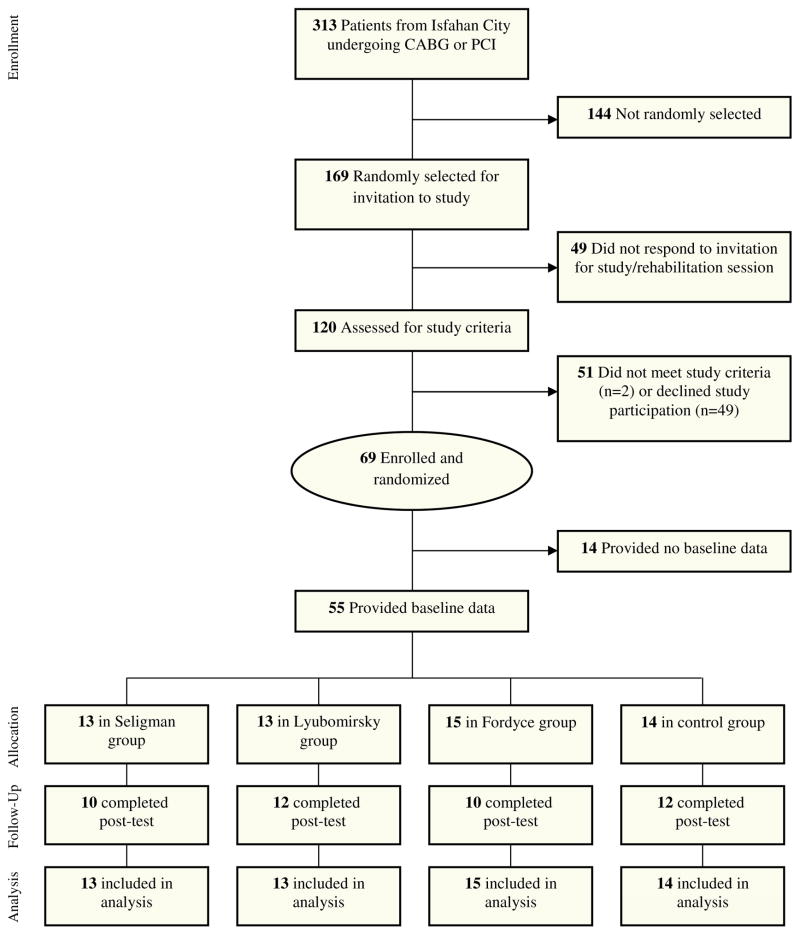
Figure 1 provides a CONSORT diagram of study recruitment and enrollment. Randomly selected patients from this cohort were invited to a study introduction session. At the pre-study session, staff outlined the study rationale, intervention procedures, and follow-up assessments. Patients were excluded if they had a major medical condition limiting their ability to participate or current treatment with antidepressants or psychotherapy (to avoid confounding effects of the intervention). Those willing to participate and meeting study criteria completed written informed consent and baseline self-report questionnaires prior to the first study meeting.
Figure 1.
Procedures
Enrolled participants were randomly assigned to one of three PPIs (Seligman, Lyubomirsky, Fordyce; see below) or a wait-list control. PPI participants received a 6-week intervention, described below. Wait-list participants attended a total of four study-related appointments (introduction session, baseline assessment, and follow-up assessments at 7 and 15 weeks), and had no other study appointments or interventions outside of their treatment as usual for the duration of the study.
PPI participants underwent an in-person group training program comprised of six weekly 90 minute sessions. Each week, participants received a new intervention packet with activities designed to build on previously-learned skills while also emphasizing novelty and variety. The PPIs (Table 1) were based on published work from authors well-known in the scientific literature and lay press (7, 8, 14–16), and designed in conjunction with a rehabilitation cardiologist to ensure that participants could safely complete them.
Table 1.
Intervention details and weekly topics
| Seligman group intervention | |
| Week 1: Increasing satisfaction about the past | Recognize responsibility in past events, express gratitude, and practice forgiveness. |
| Week 2: Enhancing happiness in the present | Plan pleasurable activities and identify activities that lead to ‘flow’ experiences. |
| Week 3: Optimism about the future | Notice negative thoughts and events as they occur, and then reframe them in a more positive and controllable way. |
| Week 4: Renewing strength and virtue | Identify a ‘signature strength’ from a list of 24 personal strengths. |
| Week 5: Valuing and using strengths and virtues | Use a signature strength in daily activities and identify strengths in their partners and children. |
| Week 6: Enhancing meaning in life | Use a signature strength in a way that furthers a cause larger than oneself. |
| Lyubomirsky group intervention | |
| Week 1: Experiencing positive emotions | Consciously work to act as though happy, reflect upon and savor positive life events, and practice five acts of kindness. |
| Week 2: Enhancing social relationships and physical activity | Nurture social relationships through being open, making eye contact, and consciously acknowledging friends and loved ones. Create a physical activity plan to exercise at a moderate pace for most days of the week. |
| Week 3: Cultivating optimism and gratitude | Visualize best possible future self, and identify and record events for which you are grateful. |
| Week 4: Developing positive coping skills | Consider the insignificance of daily worries 150 years from now, and use this realization to divert social comparison and over-thinking. Reframe cardiac or other negative life events as a way to improve yourself. |
| Week 5: Forgiveness and spirituality | Identify and forgive others by contemplating their motives for engaging in hurtful behavior. Practice prayer or another spiritual activity daily. |
| Week 6: Commitment to goals, flow, and mindfulness | Develop a plan to work toward a personal goal, to spend more time in high-challenge, high-skill situations in order to increase ‘flow experiences’, and to meditate daily |
| Fordyce group intervention | |
| Week 1: Increasing activity and social relationships | Increase the time engaged in enjoyable activities, socialize with others, and enhance close relationships by maintaining communication. |
| Week 2: Increasing productivity and organization | Enhance productivity and organizational skills by identifying, prioritizing, and completing daily activities that are gratifying and important. |
| Week 3: Reducing worry and setting realistic goals | Record worrying thoughts and notice whether they come true. Set attainable goals for the week and notice how it feels to achieve or not achieve those goals. |
| Week 4: Cultivating optimism and focusing on the present | Positively reframe several past events, present situations, and future goals. Focus attention on the present and really experience the sensations of sight, touch, sound, and smell. |
| Week 5: Focusing on positive personality traits | Overcome fears about others’ opinions, accept yourself, and initiate contact with people you would like to meet, in order to foster authenticity, self-esteem and extraversion. |
| Week 6: Prioritizing positive thoughts and feelings | Make happiness a priority by acknowledging and then setting aside negative emotions, as well as performing acts that bring happiness into your life. |
During each 90-minute session, a study trainer reviewed the strategies introduced in the prior session. Participants then described their experiences completing the assigned positive psychology exercises and received feedback and support from other group members. The trainer then presented the details and rationale for up to three strategies for the week. Next, the trainer described specific exercises to implement these strategies and allowed participants to practice them in the group. In addition, participants were encouraged to perform at least one exercise using each strategy prior to the next group session. Participants were also guided in the continued use of exercises in their daily lives, and at the final group session, received a chart to guide future exercise completion.
Interventions
All PPI interventions were delivered by the first author (Gh.N.). The trainer became familiarized with the work of each of the three researchers linked to the PPIs via reading their seminal academic and popular press books and discussions of the work with senior mentors. The interventions were subsequently developed based on this work and these discussions, and they were piloted the interventions via individual interventions with students and other healthy adults, and group meetings, to allow refinement of the interventions and to provide experience delivering them.
Seligman group intervention
This intervention was developed using exercises and techniques outlined in published studies (7, 8) and the lay book Authentic Happiness (17) from Dr. Seligman’s research program. The exercises in this intervention focused on enhancing positive feelings (‘Pleasant life’), using personal strengths (‘Engagement life’), and finding meaning (‘Meaningful life’).
Lyubomirsky group
These activities were crafted based on research from Dr. Lyubomirsky’s group (14, 18–20) and her book The How of Happiness. Like the Seligman group, the Lyubomirsky intervention focused on optimism and gratitude. However, it also included exercises on spirituality and the development of strategies for active coping.
Fordyce group
These activities were adapted from a positive emotion-based cognitive behavioral therapy intervention (15, 16). Like the other programs, the Fordyce program utilized exercises related to optimism and becoming present-oriented. In contrast to the Seligman and Lyubomirsky interventions, the Fordyce intervention also focused on increasing organizational skills, setting realistic goals, and developing positive personality traits. See Table 1 for weekly topics from all three interventions.
Data Collection
Baseline sociodemographic and medical characteristics were collected from participants. Self-report assessments using standardized instruments were completed by participants at enrollment and then in person at Week 7 (post-intervention) and Week 15 (follow-up). For PPI participants, feasibility data (e.g., completion of each session, total number of sessions completed) was recorded by study staff each week.
Outcome Measures
The Oxford Happiness Inventory (OHI) (21)
The OHI is a 29-item measure of happiness, with scores ranging from 0 to 87. Information about internal consistency, reliability, and construct validity of the Persian translation of the instrument is provided by Alipour and Norbala (22). In this study, internal consistency was excellent (α=.93).
Beck Depression Inventory-II (BDI-II) (23)
The BDI-II contains 21 items measuring depressive symptoms over the preceding two weeks. The range of scores is between 0 and 63. Ghassemzadeh and colleagues (24) reported high internal consistency of its Persian version (α=.87) and acceptable test-retest reliability (r=.74) in an Iranian sample (23). Our internal consistency was good (α=.85).
Satisfaction With Life Scale (SWLS)
The SWLS (25) is a 5-item instrument, scored from 5 to 35, that measures global satisfaction with life. Prior studies have reported adequate validity and reliability for this scale, with α=.79-.89 (26). The SWLS has also been utilized and validated previously in Persian (27). Cronbach’s alpha was acceptable (α=0.69) in our sample.
Dispositional Hope Scale (DHS)
This is a 12-item scale examining trait optimism/hope, with 4 distracter items (28). Though the 8 active items (total score 8–64) are split into items on agency and pathways/implementation, the DHS allows for a unidimensional measurement of hope and has been previously validated and tested in Persian (29). In our sample Cronbach’s alpha was α=0.64, within the acceptable range (30).
Study Aims and Statistical Analysis
An intent-to-treat model was utilized for all participants who provided baseline data. For primary analyses, given the similarities among the PPIs, participants were divided into two groups: those receiving any PPI and those receiving the control condition. Secondarily, to explore differences in feasibility and effects among the different PPIs, the participants were divided and compared across all four groups (three PPIs and the control condition).
Baseline study outcome measure values were calculated using estimated means from random effects models described below. Baseline data (baseline characteristics and self-report measures) were compared between PPI and non-PPI participants using chi-square variables (or Fisher’s exact test when indicated) for categorical outcomes and independent-samples t tests for continuous variables. For the four-group comparisons, baseline characteristics were compared similarly using chi-square analysis and ANOVA.
Study aim #1: Feasibility
For the primary study aim (feasibility), we summarized rates of exercise completion and proportions of participants completing the majority of exercises among all PPI participants using descriptive statistics. We then compared completion rates across the three PPI groups using ANOVA.
Study aim #2: Exploration of pre/post change within the same group on outcome variables from baseline
To assess changes in the outcome variables within each group, we utilized random effects regression models, with a random intercept for each patient. We examined change from baseline on each of the study outcome measures, both immediately post-intervention (7 weeks) and at follow-up (15 weeks), for the PPI participants as a whole and control participants for our main Aim #2 analysis. We then calculated and compared pre/post differences for each specific PPI. For the combined PPI (n=41) group, effect size (Cohen’s d) for each outcome measure was calculated using the estimated mean difference in the variable divided by the standard deviation at baseline.
Study Aim #3: Exploration of between-group differences in improvement from baseline
We examined between-group (any PPI vs. no PPI) differences on study outcomes at 7 and 15 weeks for our main Aim #3 efficacy analyses. We then compared each active PPI group to the control condition (for this last exploratory analysis, given multiple comparisons [three comparisons at two timepoints], a full Bonferroni correction would set significance at p=.0083).
Analyses were completed using Stata 11.0 (StataCorp, College Station, TX). Except as noted above, significance was set at two-tailed p<.05.
Results
Enrollment and Retention
Overall, 120 CABG/PCI patients attended the study introductory session, and 69 (58%) were ultimately enrolled and randomized. Of these, 14 patients provided no self-report outcome data, leaving 55 participants for analysis (Figure 1). There were no significant differences in baseline characteristics between those participants with available data and dropouts, though dropouts trended toward higher rates of CABG (57.1% dropout vs. 30.9% retained; χ2=3.32; p=.07).
Baseline Data
Baseline characteristics of participants are outlined in Table 2. Mean age was 56.6 +/− 8.7, 42 (76%) were men, and diabetes (n=14; 25%) was the most common medical comorbidity. There were no differences in characteristics (all p>.05) between PPI (n=41) and control (n=14) participants. Across the four study conditions, only history of prior depression differed across groups (Fisher’s exact test; p=.028; Table 2).
Table 2.
Baseline characteristics of study participants
| Total Sample (N=55) | Seligman Group (N=13) | Lyubomirsky Group (N=13) | Fordyce Group (N=15) | Control Group (N=14) | p*** | |
|---|---|---|---|---|---|---|
| Sociodemographic Characteristics | ||||||
| Male sex | 42 (76.3) | 9 (69.2) | 11 (84.6) | 13 (86.7) | 9 (64.3) | .41 |
| Age (mean [SD]) | 56.6 (8.7) | 55.8 (5.3) | 59.2 (11.5) | 54.7 (10.1) | 56.9 (6.7) | .58 |
| High school education or less | 37 (66.3) | 9 (69.2) | 9 (69.2) | 10 (66.7) | 9 (64.3) | .99 |
| Married | 49 (89.1) | 11 (84.6) | 12 (92.3) | 14 (93.3) | 12 (85.7) | .84 |
| Behavioral and Psychiatric Characteristics | ||||||
| Prior depression** | 17 (31.5) | 4 (30.8) | 8 (66.6) | 3 (20) | 2 (15.4) | .028 |
| Weekly or greater exercise* | 16 (30.8) | 4 (30.8) | 4 (33.3) | 3 (23.1) | 5 (35.7) | .91 |
| Medical Characteristics | ||||||
| Recent CABG | 17 (30.9) | 7 (53.8) | 4 (30.8) | 3 (20) | 3 (21.4) | .20 |
| Diabetes | 14 (25.4) | 5 (38.5) | 2 (15.4) | 4 (26.7) | 3 (21.4) | .58 |
| Hypertension | 9 (16.3) | 1 (7.7) | 1 (7.7) | 5 (33.3) | 2 (15.4) | .20 |
| Current smoking* | 7 (13.5) | 2 (16.6) | 2 (15.4) | 1 (7.1) | 2 (15.4) | .88 |
| Baseline Study Outcome Measures | ||||||
| OHI (mean [SD]) | 43.6 (13.4) | 45.8 (13.5) | 38.4 (13) | 46.3 (13.4) | 43.4 (13.2) | .29 |
| BDI-II (mean [SD]) | 15.1 (9.2) | 10.7 (9.1) | 18.0 (9.2) | 16.3 (8.9) | 15.2 (8.9) | .18 |
| SWLS (mean [SD]) | 15.1 (3.5) | 14.8 (3.5) | 15.9 (3.7) | 15.3 (3.4) | 14.5 (3.6) | .49 |
| DHS (mean [SD]) | 71.9 (9.1) | 70.1 (8.9) | 69.9 (9.2) | 73.0 (9.9) | 74.2 (9.2) | .99 |
n=52
n=54
compared across all 4 treatment conditions
Note. All data are N (%) unless otherwise specified; baseline study outcome measures estimated from random effects model. BDI-II = Beck Depression Inventory-II; CABG = Coronary Artery Bypass Graft; DHS = Dispositional Hope Scale; OHI = Oxford Happiness Inventory; SD = Standard Deviation; SWLS = Satisfaction with Life Scale
Study aim #1: Feasibility (primary aim)
Overall, 32/41 PPI participants (78%) completed a majority of the weekly sessions (≥4 of 6), and 183/246 total sessions (74%) were completed. In the Seligman group, 10/13 participants (77%) completed a majority of weekly sessions, with a total of 55 (71%) of sessions completed. In Lyubomirsky, 8/13 (62%) completed a majority of sessions, with 65% exercise completion, and in Fordyce 14/15 (93%) completed a majority, with 86% overall completion. There was a significant effect of group on exercise completion (F=3.88; p=.029), and on post-hoc pairwise comparisons, the Fordyce group was associated with greater exercise completion than Lyubomirsky (p=.035).
Study aim #2: Pre/post change from baseline on outcome variables (Table 3)
Table 3.
Pre/post changes in study outcome variables in PPI and control participants
| Condition | Coefficient | 95% CI | p | Effect size (d) |
|---|---|---|---|---|
| Happiness (Oxford Happiness Inventory) | ||||
| Post-intervention (7 weeks) | ||||
| PPI (N=41) | 5.04 | 2.42, 7.68 | < .001 | .97 |
| Control (N=14) | 0.03 | −5.95, 6.02 | .99 | -- |
| Follow-up (15 weeks) | ||||
| PPI | 5.62 | 2.84, 8.40 | <.001 | 1.08 |
| Control | −8.54 | −14.53, −2.54 | .005 | -- |
| Depression (Beck Depression Inventory-II) | ||||
| Post-intervention (7 weeks) | ||||
| PPI | −0.27 | −2.23, 1.69 | .79 | .07 |
| Control | −0.77 | −4.17, 2.63 | .66 | -- |
| Follow-up (15 weeks) | ||||
| PPI | −2.54 | −4.60, −0.47 | .016 | .65 |
| Control | 1.21 | −2.19, 4.62 | .49 | -- |
| Satisfaction (Satisfaction with Life Scale) | ||||
| Post-intervention (7 weeks) | ||||
| PPI | 1.41 | 0.17, 2.64 | .026 | .50 |
| Control | 1.68 | −0.69, 4.06 | .17 | -- |
| Follow-up (15 weeks) | ||||
| PPI | 1.32 | 0.01, 2.62 | .048 | .47 |
| Control | 0.08 | −2.18, 2.34 | .95 | -- |
| Hope (Dispositional Hope Scale) | ||||
| Post-intervention (7 weeks) | ||||
| PPI | 0.007 | −2.75, 2.76 | .99 | .01 |
| Control | −4.44 | −10.98, 2.02 | .18 | -- |
| Follow-up (15 weeks) | ||||
| PPI | −1.89 | −4.81, 1.03 | .21 | .25 |
| Control | −8.71 | −14.66, −2.76 | .004 | -- |
Note. Effect size not recorded for control condition given small N.
CI = Confidence Interval; PPI = Positive Psychology Intervention
Among those assigned to a PPI (n=41), there were pre-post (week 7) improvements in happiness (OHI; estimated mean difference [EMD]=5.04 points [95% confidence interval, CI]= 2.42–7.68, p<.001; effect size d=.97) and life satisfaction (SWLS; EMD=1.41 points, 95% CI=0.17–2.64, p=.026; d=.50). At follow-up (week 15), there were improvements from baseline in happiness (EMD=5.62 points, 95% CI=2.84–8.40, p<.001; d=1.1), depression (BDI-II; EMD −2.54 points, −4.60 to −0.47, p=0.16; d=.65), and life satisfaction (EMD 1.32 points, 95% CI=0.01–2.62, p=.048; d=.47).
On changes by individual PPI, the Lyubomirsky group was associated with significant pre/post improvements in happiness (OHI) at 7 and 15 weeks, and the Seligman group was associated with significant improvements in life satisfaction (SWLS) at both timepoints. However the extent of pre/post improvement was not different by PPI group status on any of the outcome measures at either timepoint. Finally, among control participants, at 15 weeks there was significant worsening of happiness (OHI) and hope (DHS) from baseline (see Table 3).
Study aim #3: Exploration of between-group differences in improvement from baseline (Table 4)
Table 4.
Between-group comparisons on study outcome measures
| Primary analysis: Participants receiving PPI (n=41) vs. control (n=14) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Outcome | Coefficient | 95% CI | p | Effect size (d) | Coefficient | 95% CI | p | Effect size (d) |
| Post-intervention (7 weeks) | Follow-up (15 weeks) | |||||||
| OHI | 5.14 | −0.54, 10.82 | 0.08 | 0.85 | 14.43 | 8.66, 20.20 | < 0.001 | 2.38 |
| BDI-II | 0.44 | −3.34, 4.22 | 0.82 | 0.11 | −3.87 | −7.72, −0.02 | 0.049 | −0.96 |
| SWLS | −0.28 | −2.83, 2.27 | 0.83 | −0.11 | 1.23 | −1.27, 3.73 | 0.33 | 0.49 |
| DHS | 4.78 | −1.38, 10.93 | 0.13 | 0.81 | 7.12 | 1.25, 13.00 | 0.017 | 1.20 |
| Secondary analyses: Individual PPIs vs. control | ||||||||
| Outcome | Coefficient | 95% CI | p | Coefficient | 95% CI | p | ||
| Post-intervention (7 weeks) | Follow-up (15 weeks) | |||||||
| Seligman vs. control | ||||||||
| OHI | 4.26 | −2.97, 11.49 | 0.25 | 11.35 | 4.27, 18.40 | 0.002 | ||
| BDI-II | 0.70 | −4.12, 5.53 | 0.78 | −2.01 | −6.74, 2.72 | 0.41 | ||
| SWLS | 1.25 | −1.89, 4.38 | 0.44 | 2.83 | −0.18, 5.84 | 0.07 | ||
| DHS | 4.93 | −2.62, 12.48 | 0.20 | 9.09 | 1.84, 16.35 | 0.014 | ||
| Lyubomirsky vs. control | ||||||||
| OHI | 6.96 | −0.13, 14.05 | 0.054 | 18.20 | 10.9, 25.44 | < 0.001 | ||
| BDI-II | 2.05 | −2.68, 6.78 | 0.40 | −4.56 | −9.39, 0.28 | 0.07 | ||
| SWLS | −1.70 | −4.78, 1.38 | 0.28 | −0.49 | −3.58, 2.59 | 0.76 | ||
| DHS | 5.90 | −1.53, 13.34 | 0.12 | 9.22 | 2.04, 16.41 | 0.012 | ||
| Fordyce vs. control | ||||||||
| OHI | 4.60 | −2.5, 11.71 | 0.20 | 14.49 | 6.48, 22.5 | < 0.001 | ||
| BDI-II | −1.69 | −6.43, 3.06 | 0.49 | −5.29 | −10.65, 0.05 | 0.052 | ||
| SWLS | −0.29 | −3.36, 2.78 | 0.85 | 1.21 | −2.15, 4.56 | 0.48 | ||
| DHS | 3.59 | −3.83, 11.02 | 0.34 | 1.19 | −6.79, 9.16 | 0.77 | ||
Note: Effect size not calculated for individual PPIs because of small N.
BDI-II = Beck Depression Inventory-II; DHS = Dispositional Hope Scale; OHI = Oxford Happiness Inventory; SWLS = Satisfaction with Life Scale.
When comparing all PPI participants to those receiving the control intervention, there were no between-group differences in change from baseline on the four outcome measures at 7 weeks. However, at 15 weeks, PPI participants had greater improvements in happiness (EMD=14.43; 95% CI=8.66–20.2; p<.001; d=2.38), depression (EMD= −3.87 95% CI −7.72 to −0.02; p=.049; d=.96), and hope (DHS; EMD=7.12, 95% CI 1.25–13.00; p=.017; d=1.26).
When comparing specific PPI groups with the control condition (Table 4), each of the three treatment conditions were associated with significantly greater improvements in happiness (OHI) score at 15 weeks than the control condition. In life satisfaction (SWLS) at 15 weeks, the Seligman and Lyubomirsky, but not the Fordyce group, were associated with significantly greater improvements.
Discussion
We found that in-person administration of three different group-based PPIs was feasible in a population of patients with cardiovascular disease. Across the PPIs, over three-quarters of participants completed a majority of sessions and 74% of exercises overall were completed. Despite the small size of this exploratory study, the PPIs were also associated with significantly greater improvements in happiness, depression, and hope at 15 weeks compared to a wait-list control condition, with moderate to large effect sizes, suggesting a substantial effect of the intervention on these proximal psychological outcomes.
The between-group differences on study outcomes grew over time, becoming statistically significant at 15 weeks. In general, the improvements at the initial post-intervention assessment (7 weeks) in the PPI group were maintained at 15 weeks, while in the control condition these measures worsened over time, resulting in greater differences at the final timepoint. These results suggest a durable effect of the PPIs for at least two months after the intervention, consistent with prior PPI studies finding sustained effects of PPIs on psychological outcomes (8, 31).
Regarding individual PPIs, while there were some differences in effects by specific PPI (e.g., greater improvement in happiness with Lyubomirsky and greater improvement in life satisfaction in Seligman), these differences did not reach statistical significance, given the very small sample sizes in each individual condition. These between-PPI differences did not nearly reach the magnitude of the differences between the PPIs and control, suggesting that selection of any of these PPIs would likely be adequate to impact the psychological outcomes of interest, especially optimism/hope and positive affect.
Regarding an explanation for the higher rates of completion in the Fordyce group than in Lyubomirsky, there are several potential possibilities. One possibility is related to session content. The Fordyce group utilized simpler and more introspective, concise, and general interventions and topics that may have been more acceptable and easy to complete. In contrast, the Lyubomirsky intervention was more intensive and required participants to complete kind acts for others (which may have been physically or emotionally challenging), create a physical activity plan (which may have been difficult), and focus on spirituality/prayer (which may not have matched all participants’ beliefs or goals). At the same time, these activities in the Lyubomirsky group, while more challenging, may have also been more effective, given that despite the lower completion rates, this was the only individual condition to result in significantly greater happiness.
Overall, the lack of differences among PPIs is not surprising, given that there was moderate overlap in constructs targeted by each intervention, such as optimism, gratitude, forgiveness, flow, and mindfulness. Further study exploring potential superiority of one PPI over another could identify an optimal PPI to target specific outcomes (e.g., depression, optimism) that are associated with major medical outcomes, including survival, in cardiac patients (32).
This study adds to the limited literature utilizing PPIs in persons with heart disease. Members of our team completed a smaller (N=28) three-arm trial of a phone-based PPI (most similar to the Lyubomirsky group in this trial) in patients with acute coronary syndrome or heart failure. In that trial, the intervention was feasible, with high rates of exercise completion, and the PPI was associated with greater improvements in nearly all psychological measures compared to active control (Relaxation Response) and attentional control conditions (11). In addition, a somewhat-related positive affect intervention led to improved physical activity in a trial of PCI patients (33). Finally, members of our team also completed a study of a PPI, compared to a subsequently enrolled treatment as usual cohort, among 48 patients suffering an acute coronary syndrome. Participants receiving the PPI had greater improvements in positive affect, depression, and anxiety, though not dispositional optimism, compared to those in treatment as usual (13).
To our knowledge, this is the first trial to investigate in-person PPI delivery in cardiac patients, contemporaneously evaluate these three specific interventions, and assess outcomes over multiple timepoints. Importantly, this was also the first such investigation outside of the United States, a critical step in determining the generalizability and acceptability of these interventions in non-Western populations. Thus far, the vast majority of PPIs in any population have been studied in the U.S. and Western Europe, and there had been no prior study of PPIs in cardiac populations outside the U.S. These results—which are highly similar to those seen in prior studies both in terms of feasibility and impact—suggest that PPIs may be more broadly applicable to Western and non-Western cohorts.
Boosting positive affect, life satisfaction, and optimism may have critical cardiac effects, given that these constructs are related to reduced risk for developing heart disease (34), fewer readmissions for heart disease, and lower mortality (3, 32, 35–37). Positive psychological well-being may physiologically influence cardiovascular outcomes via improved neuroendocrine function (2, 38), reduced inflammation (39), and improved heart rate, blood pressure, and immune system function (36, 40, 41). These beneficial cardiac effects may also be mediated by health behaviors, as optimism in particular is associated healthier diet, more physical activity, greater medication adherence, and lower rates of smoking (32, 42–44).
Given these factors, and the feasibility and suggestion of efficacy of PPIs in this study, next-wave studies of PPIs are indicated. These could include factorial trials that determine the most effective components/aspects of PPIs (e.g., optimal content, duration) (45), or a larger placebo-controlled trial of a PPI that is adequately powered to detect between-group differences on health behaviors, cardiac biomarkers, and medical events.
This preliminary study had multiple limitations. Participants were drawn from a single city within Iran, and a substantial minority of approached patients declined participation. The small sample sizes completing each PPI intervention limited our ability to detect differences in efficacy among these different treatments, and the small number of participants in the control condition likewise limited our ability to detect differences in outcomes between PPIs and controls. In addition, given that the wait-list control was not attention-matched, it is possible that the PPIs’ effects were related to non-specific effects of attention rather than the specific PPI content. This preliminary analysis also did not assess cardiac events or cardiac health behaviors.
In conclusion, a set of three PPIs in cardiac patients was feasible and associated with improvements in hope/optimism, happiness, and depression compared to a control condition. Given the potential cardiovascular benefits of increasing optimism and positive affect, further study of these simple PPIs is indicated to assess their effects on important cardiac outcomes.
Acknowledgments
The authors would like to thank Iran Zamin Cardiac Rehabilitation Center and Sina Cardiovascular Hospital for hosting this study.
This study was supported by Center of Excellence for Psychology of Spirituality and Happiness, The University of Isfahan, Isfahan, Iran. Investigator time for data analysis and manuscript preparation for CC, SB, and JH was supported by the National Institutes of Health—National Heart, Lung, and Blood Institute grant number R01HL113272.
Footnotes
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mortality GBD Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers. 2009;77(6):1747–76. doi: 10.1111/j.1467-6494.2009.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasmussen HN, Scheier M, Greenhouse J. Optimism and physical health: a meta-analytic review. Annals of Behavioral Medicine. 2009;37(3):239–56. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 5.Konstam V, Salem D, Pouleur H, Kostis J, Gorkin L, Shumaker S, et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. SOLVD Investigations. Studies of Left Ventricular Dysfunction Investigators. Am J Cardiol. 1996;78(8):890–5. doi: 10.1016/s0002-9149(96)00463-8. [DOI] [PubMed] [Google Scholar]
- 6.Chocron S, Etievent J, Viel J, Dussaucy A, Clement F, Kaili D, et al. Preoperative quality of life as a predictive factor of 3-year survival after open heart operations. The Annals of Thoracic Surgery. 2000;69(3):722–7. doi: 10.1016/s0003-4975(99)01329-6. [DOI] [PubMed] [Google Scholar]
- 7.Seligman M, Rashid T, Parks A. Positive psychotherapy. The American Psychologist. 2006;61(8):774–88. doi: 10.1037/0003-066X.61.8.774. [DOI] [PubMed] [Google Scholar]
- 8.Seligman M, Steen T, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. The American Psychologist. 2005;60(5):410–21. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 9.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65(5):467–87. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 10.Bolier L, Haverman M, Westerhof G, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huffman J, Mastromauro C, Boehm J, Seabrook R, Fricchione G, Denninger J, et al. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 2011;6(2):e14. doi: 10.4081/hi.2011.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charlson M, Boutin-Foster C, Mancuso C, Peterson J, Ogedegbe G, Briggs W, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases. Contemporary Clinical Trials. 2007;28:748–62. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Huffman JC, Millstein RA, Mastromauro CA, Moore SV, Celano CM, Bedoya CA, et al. A Positive Psychology Intervention for Patients with an Acute Coronary Syndrome: Treatment Development and Proof-of-Concept Trial. J Happiness Stud. 2015 Oct 18; doi: 10.1007/s10902-015-9681-1. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyubomirsky S. The How of Happiness: A Scientific Approach to Getting the Life You Want. New York: Penguin Press; 2008. [Google Scholar]
- 15.Fordyce M. Development of a program to increase personal happiness. Journal of Counseling Psychology. 1977;24(6):511–21. [Google Scholar]
- 16.Fordyce M. A program to increase happiness: further studies. Journal of Counseling Psychology. 1983;30(4):480–98. [Google Scholar]
- 17.Seligman M. Authentic Happiness: Using the New Positive Psychology to Realize Your Potential for Lasting Fulfillment. New York: Free Press; 2002. [Google Scholar]
- 18.Lyubomirsky S, Dickerhoof R, Boehm J, Sheldon KM. Becoming happier takes both a will and a proper way: An experimental longitudinal intervention to boost well-being. Emotion. 2011;11:391–402. doi: 10.1037/a0022575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyubomirsky S, Sheldon K, Schkade D. Pursuing happiness: the architecture of sustainable change. Rev Gen Psychol. 2005;9:111–31. [Google Scholar]
- 20.Sheldon K, Lyubomirsky S. How to increase and sustain positive emotion: the effects of expressing gratitude and visualizing best possible selves. J Posit Psychol. 2006;1:73–82. [Google Scholar]
- 21.Argyle M, Martin M, Crossland J. Happiness as a function of personality and social encounters. In: Forgas JP, Innes JM, editors. Recent Advances in Social Psychology: An International Perspective. North Holland: Elsevier; 1989. pp. 189–203. [Google Scholar]
- 22.Alipour A, Nor-bala A. Introductory survey on validity and reliability of Oxford Happiness Inventory in Tehran universities. Journal of Thought and Behavior. 1999;5:55–63. [Google Scholar]
- 23.Beck A, Steer R, Brown G. Manual for Beck Depression Inventory-II (BDI-II) San Antonio, TX: Psychology Corporation; 1996. [Google Scholar]
- 24.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory--Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21(4):185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 25.Diener E, Emmons R, Larsen R, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment. 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 26.Pavot W, Diener E. Review of the Satisfaction With Life Scale. Psychological Assessment. 1993;5(2) [Google Scholar]
- 27.Bayani AA, Kouchaki AM, Goudarzi H. The Reliability and validity of the satisfaction with life scale. Developmental Psychology. 2007;3:259–65. [Google Scholar]
- 28.Snyder C, Harris C, Anderson J, Holleran S, Irving L, Sigmon S, et al. The will and the ways: development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology. 1991;60(4):570–85. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- 29.Kermani Z, Khodapanahi M, Heidari M. Psychometric features of the Snyder Hope Scale. Journal of Applied Psychology. 2011;5(3):7–23. [Google Scholar]
- 30.Kline P. The handbook of psychological testing. 2. London ; New York: Routledge; 2000. [Google Scholar]
- 31.Fredrickson B, Cohn M, Coffey K, Pek J, Finkel S. Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology. 2008;95(5):1045–62. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DuBois C, Beach S, Kashdan T, Nyer M, Park E, Celano C, et al. Positive psychological attributes and cardiac outcomes: associations, mechanisms, and interventions. Psychosomatics. 2012;53(4):303–18. doi: 10.1016/j.psym.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong SC, Hollenberg JP, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med. 2012;172(4):329–36. doi: 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kubzansky L, Thurston R. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry. 2007;64(12):1393–401. doi: 10.1001/archpsyc.64.12.1393. [DOI] [PubMed] [Google Scholar]
- 35.Tindle H, Chang Y, Kuller L, Manson J, Robinson J, Rosal M, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120(8):656–62. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiology of Aging. 2005;26(Suppl 1):108–12. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 37.Boehm J, Peterson C, Kivimaki M, Kubzansky L. A prospective study of positive psychological well-being and coronary heart disease. Health Psychology. 2011;30(3):259–67. doi: 10.1037/a0023124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Endrighi R, Hamer M, Steptoe A. Associations of trait optimism with diurnal neuroendocrine activity, cortisol responses to mental stress, and subjective stress measures in healthy men and women. Psychosom Med. 2011;73(8):672–8. doi: 10.1097/PSY.0b013e31822f9cd7. [DOI] [PubMed] [Google Scholar]
- 39.Brouwers C, Mommersteeg P, Nyklicek I, Pelle A, Westerhuis B, Szabo B, et al. Positive affect dimensions and their association with inflammatory biomarkers in patients with chronic heart failure. Biol Psychol. 2013;92(2):220–6. doi: 10.1016/j.biopsycho.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 40.Pressman S, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–71. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 41.Dockray S, Steptoe A. Positive affect and psychobiological processes. Neuroscience & Biobehavioral Reviews. 2010;35(1):69–75. doi: 10.1016/j.neubiorev.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tindle H, Davis E, Kuller L. Attitudes and cardiovascular disease. Maturitas. 2010;67(2):108–13. doi: 10.1016/j.maturitas.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: the zutphen elderly study. J Psychosom Res. 2007;63(5):483–90. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 44.Huffman JC, DuBois CM, Mastromauro CA, Moore SV, Suarez L, Park ER. Positive psychological states and health behaviors in acute coronary syndrome patients: A qualitative study. J Health Psychol. 2014 doi: 10.1177/1359105314544135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Collins L, Dziak J, Li R. Design of experiments with multiple independent variables: a resource management perspective on complete and reduced factorial designs. Psychol Methods. 2009;14(3):202–24. doi: 10.1037/a0015826. [DOI] [PMC free article] [PubMed] [Google Scholar]