Abstract
Objective Peer victimization (PV) is a key interpersonal stressor that can be traumatizing for youth. This study evaluated the relationships between overt, relational, reputational, and cyber PV and adolescents’ somatic complaints and sleep problems. Symptoms of depression and social anxiety were examined as potential mediators. Method Adolescents (N = 1,162; M age = 15.80 years; 57% female; 80% Hispanic) were assessed at three time points, 6 weeks apart, using standardized measures of PV, depression, social anxiety, sleep problems, and somatic complaints. Structural equation modeling evaluated key study aims. Results Relational, reputational, and cyber PV, but not overt PV, were directly or indirectly associated with subsequent somatic complaints and/or sleep problems. Depression and social anxiety mediated relationships between relational PV and health outcomes, whereas reputational PV was indirectly associated with somatic complaints via depression only. Discussion The stress of PV may contribute to adolescents’ sleep problems and somatic complaints and has implications for pediatric psychologists.
Keywords: adolescence, cyber victimization, depression, peer victimization, physical health, social anxiety
Peer victimization (PV), or being the recipient of physical or psychological harm from peers (De Los Reyes & Prinstein, 2004), is potentially traumatizing to youth (Storch & Esposito, 2003), and can adversely affect their mental and physical health. PV experiences have been associated with youths’ internalizing symptoms, such as depression and social anxiety (La Greca & Harrison, 2005; Reijntjes, Kamphuis, Prinzie, & Telch, 2010), and with physical or somatic symptoms, such as headaches, stomachaches, and pain (Rigby, 2001, 2003). However, research on the health effects of PV among adolescents is scant and has not included a comprehensive assessment of both traditional and cyber forms of PV. In addition, studies have largely used cross-sectional designs (Rigby, 2001, 2003) and have given limited attention to psychological processes that might underlie associations between PV and adolescents’ health problems. Based on these gaps, the current study examined the prospective relationship between PV experiences and adolescents’ physical health problems, as well as potential mediators of these associations.
The physical health problems we focused on were somatic complaints and sleep problems. Somatic complaints were examined because they have been associated with the development of multiple psychological and physical health problems, such as a poorer quality of life and reduced ability to engage in leisure and daily activities (Hunfeld et al., 2001) and increased use of analgesic medication (Fichtel & Larsson, 2002). Sleep difficulties were examined because they have been implicated in the development of chronic health problems, such as obesity/overweight (Shiromani, Horvath, Redline, & Van Cauter, 2012), hypertension (Javaheri, Storfer-Isser, Rosen, & Redline, 2008), and poor pain modulation (Lee et al., 2013). In addition, sleep deficits can adversely affect adolescents’ attention processes and their behavioral and emotional control (Dahl & Lewin, 2002).
PV Prevalence and Linkages With Somatic Complaints and Sleep Problems
Several types of PV have been identified. Traditional types include: overt (i.e., being threatened or physically harmed), relational (i.e., being socially excluded), and reputational (i.e., being embarrassed by peers or the target of rumors) (De Los Reyes & Prinstein, 2004). Cyber PV refers to being the recipient of peer aggression (of all PV types) that occurs via electronic media, such as text messages or social networking sites (Landoll, La Greca, Lai, Chan, & Herge, 2015).
Overall rates of PV among adolescents are high. Approximately 25% of public schools consider traditional forms of PV to be a daily or weekly problem (Dinkes, Cataldi, & Lin-Kelly, 2007), and other estimates suggest that approximately 50% of adolescents (aged 13–16 years) experience traditional PV at least once during an academic year (Rigby, 1998). In particular, relational and reputational types of PV are the most common among adolescents and are strongly linked to psychological distress, such as feelings of depression and social anxiety (De Los Reyes & Prinstein, 2004; La Greca & Harrison, 2005; Siegel et al., 2009). In contrast, overt PV has not been related to psychological distress when other forms of PV are considered (e.g., La Greca & Harrison, 2005; Storch, Masia-Warner, Crisp, & Klein, 2005).
Prevalence rates for cyber PV among adolescents often range from 6% to 30% (e.g., Kowalski & Limber, 2007; Li, 2007; Patchin & Hinduja, 2012) but have been reported to be as high as 72% (Juvonen & Gross, 2008). These rates may underestimate aversive cyber experiences, given the rapidly increasing use of smartphones and mobile devices among youth ages 12–17 years (Lenhart, 2015; Madden, Lenhart, Duggan, Cortesi, & Gasser, 2013). Cyber PV is primarily associated with adolescent depression (e.g., Kowalski, Giumetti, Schroeder, & Lattanner, 2014), although such data are largely correlational.
Among early adolescents, traditional PV has been linked to concurrent somatic symptoms, such as heart palpitations and breathing problems, digestive problems, and poorer general health (Houbre, Tarquinio, Thuillier, & Hergott, 2006; Natvig, Albrektsen, & Qvarnstrom, 2001; Rigby, 1998). Rigby (1999) also found that PV assessed in the 8th and 9th grades predicted adolescents’ somatic problems (e.g., colds, headaches, stomachaches) in the 11th and 12th grades. Similarly, Biebl, DiLalla, Davis, Lynch, & Shinn (2011) found that youth (n = 16) who reported chronic PV across three time points (at ages 5, 10–18, and 12–20 years) were more likely to report general health problems (which included headaches and sleep problems) than those with variable levels of PV or who were not victims, although these results held only for girls.
Despite these important findings, none of the above studies assessed the impact of cyber PV, even though it differs from traditional PV in important ways. Cyber PV may be more damaging to youth because it has the potential for the perpetrator to be anonymous and for a large audience to witness the victimization; it also has fewer constraints on when and where the victimization occurs (Sticca & Perren, 2013). We could find only one study that examined linkages between cyber PV and somatic or sleep problems in youth (Sourander et al., 2010). This study of middle school youth in Finland found that victims of cyber PV concurrently reported more headaches, abdominal pain, and trouble falling asleep than nonvictims.
The present study extended the above literature by examining both traditional and cyber PV as prospective predictors of youths’ somatic complaints and sleep difficulties. We focused on high-school-aged adolescents who are underrepresented in studies of the health impact of PV, but who report high levels of relational and reputational PV (La Greca & Harrison, 2005; Siegel et al., 2009). Older adolescents also may be more vulnerable to being the victim of peers’ cyber attacks than younger adolescents, given that older youth are high users of cell phones, social networking sites, and the Internet (Lenhart, 2015; Madden et al., 2013).
Symptoms of Depression and/or Social Anxiety as Mediators
We examined depressive symptoms and social anxiety as possible mediators between adolescent PV and subsequent physical health problems (somatic complaints, sleep problems). To our knowledge, this issue has not been addressed in prior research. However, relational, reputational, and cyber forms of PV have been strongly linked with adolescents’ symptoms of depression and/or social anxiety, both concurrently and prospectively (e.g., Reijntjes et al., 2010; Siegel et al., 2009). Moreover, symptoms of depression and anxiety have been associated with somatic complaints and/or sleep problems (e.g., Alfano, Ginsburg, & Kingery, 2007; Bardone et al., 1998; Rohde, Lewinsohn, & Seeley, 1994; Sareen et al., 2006). Thus, a potential scenario is that PV leads to feelings of depression and/or social anxiety, which in turn contribute to adolescents’ somatic complaints and sleep difficulties.
Evaluating symptoms of both depression and social anxiety as potential mediators might inform future prevention and intervention efforts. If both types of internalized distress mediate between PV and adolescent health problems, it would suggest that their shared variance of negative affect or emotional distress (Clark & Watson, 1991; Garber & Weersing, 2010) could be the underlying mechanism; this might lead to interventions that address adolescents’ negative feelings in the face of PV (e.g., La Greca et al., 2014). On the other hand, if only depression or only social anxiety serves as a mediator, it would suggest that the underlying mechanisms might be specific either to depression (such as hopelessness [Abramson, Metalsky, & Alloy, 1989] or low positive affect [Anderson & Hope, 2008]) or to social anxiety (such as social threat appraisals [Bar-Haim et al., 2007] or autonomic arousal [Anderson & Hope, 2008]). Differential mediators might lead to different intervention strategies to mitigate PV’s health impact.
Other Considerations: Ethnicity and Gender
This study focused on adolescents from predominantly Hispanic backgrounds, extending earlier work that focused almost exclusively on youth from nonminority backgrounds (e.g., Biebl et al., 2011; Rigby, 1999; Sourander et al., 2010). Hispanic youth represent the largest ethnic minority in the United States (U.S. Census Bureau, 2012). Despite the call for research on PV using diverse samples (Hawker & Boulton, 2000; Storch, Nock, Masia-Warner, & Barlas, 2003), most studies have not included a sizable representation of Hispanic youth, thus limiting the generalizability of existing findings. Although available data are scant, Nansel and colleagues (2001) surveyed over 15,000 U.S. students in grades 6 through 10, finding that Hispanic youth reported marginally higher involvement in bullying, but not in being victimized, than youth from other ethnic groups.
In evaluating associations between traditional PV, cyber PV, and adolescents’ somatic complaints and sleep problems, we considered potential gender differences in the study variables. Gender differences have been found in adolescent PV (girls report more relational victimization and boys report more overt victimization; La Greca & Harrison, 2005; Siegel et al. 2009), and in internalized distress (girls report more social anxiety and depressive symptoms than boys; Essau, Lewinsohn, Seeley, & Sasagawa, 2010; Hyde, Mezulis, & Abramson, 2008).
Based on the above, we evaluated ethnic and gender differences in our study sample. As appropriate, we also controlled for ethnicity and gender when evaluating the associations between PV and youths’ somatic complaints/sleep problems.
Study Aims and Hypotheses
In summary, our study aims were to examine the relationship between traditional and cyber PV experiences and subsequent physical health problems (i.e., somatic complaints and sleep problems) among high-school-aged adolescents, and to examine depression and social anxiety as potential mediators of these associations. We focused on high-school-aged adolescents as they are underrepresented in studies of the health impact of PV, and also because they may be at greater risk for cyber PV than younger children and adolescents.
We hypothesized that adolescents reporting more relational, reputational, and cyber PV (but not overt PV) would subsequently report more somatic complaints and sleep difficulties, and that these associations would be mediated by symptoms of both depression and social anxiety. Such information could prove useful for developing evidence-based health promotion programs and also could assist and inform pediatric psychologists and health-care providers who encounter adolescents with unexplained somatic complaints and/or sleep problems.
Method
Participants
Participants were 1,162 adolescents, 13–19 years of age (M = 15.80; SD = 1.20; 57% female), recruited from high schools in an urban area of the Southeastern United States. The sample was predominantly Hispanic (Ethnicity: 80% Hispanic; Race: 84% = White, 12% = Black, 4% = Asian), similar to the composition of the broader community (Ethnicity: 66% Hispanic; Race: 78% = White, 19% = Black, 2% = Asian) (U.S. Census Bureau, 2013).
Procedure
The project was part of a larger study of adolescent peer relations, and was approved by the University institutional review board and the local school district. Two schools that were representative of the broader school district were approached for participation and agreed; project staff met with teachers and students to describe the project. The project was described as a study of adolescent peer experiences that included questions related to positive and negative peer interactions, mood symptoms, social support, and physical health. Teachers (mainly from the science department) distributed parental letters and consent forms to approximately 2,250 adolescents, and adolescents completed assent forms before participation. Overall participation rates were at least 52%. This percentage is likely lower than the actual rate, as many adolescents were enrolled in multiple classes taught by participating teachers and, owing to confidentiality, data were not available on students’ overlapping enrollment. Of the adolescents who returned consents (n = 1,434), 86% had parental consent or adolescent consent (if≥18 years) to participate; of these, 60 were excluded (20 were non-English speakers and 40 were no longer enrolled in the school at the time of testing). This resulted in 1,177 eligible consenting adolescents. A total of 1,162 adolescents participated in at least one study time point1; analytic procedures accommodated missing data, so the full sample was included in the analyses. Those who participated at all three time points did not differ from those participating at only one or two time points on any of the demographic or Time 1 variables.
Teachers received $20 gift cards for collecting consent forms, and adolescents participating at each school were enrolled in a raffle to receive one of three gift cards ($20–$50) at each time point. Adolescents were assessed during the spring of 2011 at three time points, approximately 6 weeks apart. We selected the spring semester to ensure that adolescents were well into the school year and familiar with each other; the assessments occurred at the beginning, middle, and end of the spring semester, as determined by the school district’s academic calendar and testing schedule. This time frame also is consistent with prior research on PV (e.g., Siegel et al., 2009). Questionnaires were completed during class time, supervised by trained assistants.
Measures
Demographic Variables
Adolescents reported their age, grade, gender, ethnicity, and race. These demographics were considered as possible control variables in subsequent analyses.
Peer Victimization
At Time 1, the Revised Peer Experiences Questionnaire (R-PEQ; De Los Reyes & Prinstein, 2004) assessed relational, reputational, and overt victimization (three items per subscale). Items included: “Some peers left me out of an activity that I really wanted to be included in” (relational PV), “A teen gossiped about me so others would not like me” (reputational PV), and “A peer hit, kicked, or pushed me in a mean way” (overt PV). Participants rated how often each event occurred in the past 2 months (1 = never, 5 = a few times a week). Internal consistencies were consistent with previous research (e.g., Siegel et al., 2009): overt PV α = .66, relational PV α = .74, reputational PV α = .79.
Cyber Victimization
At Time 1, the Cyber Peer Experiences Questionnaire (C-PEQ; Landoll et al., 2015) assessed cyber PV with nine items (e.g., “A peer posted pictures of me that made me look bad via electronic media,” “A peer sent me a mean message via electronic media,” “A peer posted mean things about me publicly via electronic media”). Adolescents rated how often each event occurred over the past 2 months (1 = never, 5 = a few times a week). Internal consistency was α = .78. One item (“A peer I wanted to be friends with via electronic media ignored my friend request”) was removed owing to a poor factor loading (<.40) when assessing model fit in our path analyses, resulting in an eight-item measure for our path models. Cyber PV shows low to moderate correlations with traditional forms of PV (see Table I). Confirmatory factor analyses have indicated that cyber PV, as measured by the C-PEQ, is separate and distinct from overt, relational, and reputational PV (Landoll et al., 2015).
Table I.
Descriptive Statistics and Correlations Among the Study Variables
| Variable (range) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Mean (SD) or (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (girls = 1) | 1 | 57% | ||||||||||
| 2. Age | − .04 | 1 | 15.80 (1.20) | |||||||||
| 3. Hispanic | .04 | −.02 | 1 | 80% | ||||||||
| 4. R-PEQ relational PV T1 | .10** | −.04 | −.08** | 1 | 1.63 (.63) | |||||||
| (1–5)a | ||||||||||||
| 5. R-PEQ reputational PV T1 | .15*** | −.04 | −.09** | .39*** | 1 | 1.51 (.70) | ||||||
| (1–5)a | ||||||||||||
| 6. R-PEQ overt PV T1 | −.15*** | −.09** | −.07* | .26*** | .47*** | 1 | 1.32 (.50) | |||||
| (1–5)a | ||||||||||||
| 7. C-PEQ cyber PV T1 | .10*** | −.07* | −.08* | .45*** | .56*** | .39*** | 1 | 1.35 (.39) | ||||
| (1–5)a | ||||||||||||
| 8. CES-D depression T2 | .10*** | −.02 | −.06 | .27*** | .28*** | .20*** | .26*** | 1 | 11.96 (8.58) | |||
| (0–54)b | ||||||||||||
| 9. SAS-A Anxiety T2 | .11*** | −.03 | −.08** | .39*** | .22*** | .15*** | .23*** | .45*** | 1 | 36.22 (13.52) | ||
| (5–90)b | ||||||||||||
| 10. Sleep deficit T3 (0–4)b | .14*** | −.06 | −.01 | .09** | .20*** | .11** | .20*** | .27*** | .15*** | 1 | 1.00 (1.22) | |
| 11. Excess sleep T3 | .03 | −.03 | −.01 | .14*** | .17*** | .09** | .19*** | .20*** | .14*** | .12*** | 1 | .53 (.73) |
| (0–2)b | ||||||||||||
| 12. YSR somatic T3 | .19*** | −.04 | −.01 | .20*** | .25*** | .12*** | .25*** | .42*** | .26*** | .52*** | .27*** | 3.14 (3.38) |
| (0–18)b |
Note. R-PEQ = Revised Peer Experiences Questionnaire; C-PEQ = Cyber Peer Experiences Questionnaire; CES-D = Center for Epidemiological Studies—Depression Scale; SAS-A = Social Anxiety Scale for Adolescents; YSR = Youth Self Report, Somatic Complaints Subscale.
aMean value scores are means.
bMean value scores are sums.
*p < .05; **p < .01; ***p < .001.
Depressive Symptoms
At Time 2, the Center for Epidemiological Studies—Depression Scale (CES-D; Radloff, 1977) assessed depressive symptoms over the past week with 20 items (e.g., “I felt that I could not shake off the blues even with help from my family or friends”). Two items (“I did not feel like eating; my appetite was poor” and “My sleep was restless”) were removed owing to possible overlap with the measures of somatic complaints and sleep problems, resulting in an 18-item measure. Adolescents rated items using a 4-point scale (0 = rarely or none of the time, 3 = most or all of the time) and a total score was calculated. The CES-D is a widely used measure with demonstrated convergent validity with clinical interviews for depression (Chabrol, Montovany, Chouicha, & DuConge, 2002). In this sample, internal consistency for the abbreviated measure was α = .86.
Social Anxiety
At Time 2, the 18-item Social Anxiety Scale for Adolescents (SAS-A; La Greca & Lopez, 1998) assessed symptoms of social anxiety (e.g., “I worry about what others think of me”) over the previous 2 months. The SAS-A does not contain any items related to somatic or sleep concerns, and thus it has no overlap with the outcome measures of somatic complaints and sleep problems. Adolescents rated items on a 5-point scale (1 = not at all to 5 = all the time) and a total score was calculated. The SAS-A has demonstrated strong construct validity with adolescents (Inderbitzen-Nolan & Walters, 2000; Storch, Masia-Warner, Dent, Roberti, & Fisher, 2004), including Hispanic adolescents (La Greca, Ingles, Lai, & Marzo, 2015), and has been used extensively to assess adolescent social anxiety (La Greca & Harrison, 2005; Siegel et al., 2009). In this sample, internal consistency was α = .94.
Somatic Complaints
At Time 3, the 9-item Somatic Symptom Subscale of the Youth Self-Report (YSR; Achenbach & Rescorla, 2001) assessed somatic symptoms over the past month. Items include having “physical problems without a known medical cause,” such as “headaches” or “nausea,” and were rated on a 3-point scale (0 = not true, 2 = very true or often true). A total score was calculated; internal consistency was α = .84 in this sample.
Sleep Problems
Three items assessed sleep problems at Time 3. Although studies often have used “trouble sleeping” as a general indicator of sleep problems (e.g., Johnson & Breslau, 2001), we attempted to further clarify the specific type of sleep problems by including three items that assessed sleep problems in youth following natural disasters (e.g., Herge, et al., 2011; La Greca et al., 2010; Lai, La Greca, Auslander, & Short, 2013). The two sleep deficit items (i.e., “I have trouble falling asleep,” and “I have trouble staying asleep”) were derived from an item on the PTSD-Reaction Index (Steinberg, Brymer, Decker, & Pynoos, 2004) that asks about “trouble going to sleep” or “waking up” during the night. The one sleep excess item (“I sleep more than usual”) was derived from depression measures appropriate for youth, such as the Beck Depression Inventory (Beck, Steer, & Brown, 1996). Using the same format as the YSR, participants rated the sleep symptoms over the past month (0 = not true, 2 = very true or often true). A total score was calculated for the two sleep deficit items (α = .73).
Data Analytic Plan
Data were examined for missingness, outliers, normality, and linear relationships between variables. To handle individual item-level missing data, full information maximum likelihood estimation procedures were used (Muthen & Muthen, 2011); all 1,162 participants were included in the analyses. None of the variables displayed significant levels of skewness (>3) or kurtosis (>10) (Kline, 2011).
Before evaluating the overall study aim, latent variables were created for several constructs. Specifically, items from the Time 1 R-PEQ and C-PEQ were used to create latent variables for relational, reputational, overt, and cyber PV. Further, items from the Time 3 somatic complaint subscale of the YSR and the two sleep deficit items were used to create latent variables for somatic complaints and sleep deficits, respectively. Depressive symptoms (Time 2 total score), social anxiety symptoms (Time 2 total score), and excess sleep (Time 3 item) were treated as observed variables. Demographic variables that were significantly correlated with study variables were controlled in the path models, noted at the bottom of each Figure.
Structural Equation Modeling (SEM) was used to examine the overall study aims.2 Separate models were run to evaluate the two outcomes of “somatic complaints” and “sleep problems” (i.e., sleep deficits and excess sleep). Also, separate models were run to evaluate depressive symptoms and social anxiety as possible mediators between PV and the physical health outcomes, resulting in four SEM models total. We expected relational, reputational, and cyber PV to be associated with the somatic and (the two) sleep outcomes via the pathways of depression and social anxiety, and thus 18 possible mediating pathways were evaluated.
Owing to the large sample size, the chi-square value was not considered to be a good indicator of model fit (Kline, 2011). Instead, overall model fit was assessed with the root-mean-square error of approximations (RMSEA < 0.06; Kline, 2011), the comparative fit index (CFI ≥ 0.90; Carlo, Knight, McGinley, Zamboanga, & Jarvis, 2010), and the standardized root mean square residual (SRMR < 0.08; Kline, 2011).
Results
Descriptive Statistics: Means and Intercorrelations Among Study Variables
Means were computed for each study variable (see Table I). At Time 1, adolescents reported the following levels of PV: relational = 1.63, reputational = 1.51, overt = 1.32, and cyber = 1.35, which are similar to means obtained in previous community-based studies of adolescents (e.g., La Greca & Harrison, 2005; Landoll et al., 2015; Siegel et al., 2009). Ninety-two percent of the adolescents reported at least one single PV experience; 8% (n = 98) reported no PV at all. Fewer youth reported experiencing PV “at least 1–2 times” on average in the past 2 months (relational PV: 32.7%; reputational PV: 25.8%; overt PV: 14.8%; cyber PV: 8.4%), consistent with previous research (Wang, Iannotti, & Nansel, 2009). Adolescents’ levels of social anxiety (SAS-A M = 36.22) were comparable to previous studies (La Greca & Harrison, 2005; Siegel et al., 2009), as were depressive symptoms (CES-D M = 13.69, SD = 9.75; abbreviated measure: M = 11.96) (Rushton, Forcier, & Schectman, 2002). Based on clinical cutoffs (SAS-A ≥ 50; CES-D ≥ 16), 16.8% of the adolescents reported elevated social anxiety and 33.0% reported elevated symptoms of depression.
On average, adolescents reported about three somatic complaints (M = 3.14) and their frequency of sleep difficulties fell between “never” and “sometimes.” Sleep deficits and sleep excess were related but distinct (r = .12). In general, sleep deficits and sleep excess were significantly related to all types of PV (r’s = .09–.20), to symptoms of social anxiety and depression (r’s = .14–.27) and to concurrent somatic symptoms (r’s = .27–.52) (see Table I).
Table I also reveals significant, positive associations between each PV type and each health outcome (r’s = .09–.25).
Demographic variables that displayed significant correlations with study variables were controlled in the analyses. For all the structural models, and as noted at the bottom of Figures 1 and 2, Hispanic ethnicity was associated with less Time 1 relational, reputational, overt, and cyber PV (p’s < .05). In addition, Hispanic ethnicity was related to less Time 2 social anxiety (p < .01) in the models testing social anxiety. Across the models, female gender was associated with greater Time 1 relational, reputational, and cyber PV, less overt PV, and greater Time 3 somatic complaints and sleep deficits (all p’s < .01). Also, girls reported more depressive symptoms and social anxiety than boys. Older age was associated with less Time 1 overt and cyber PV.
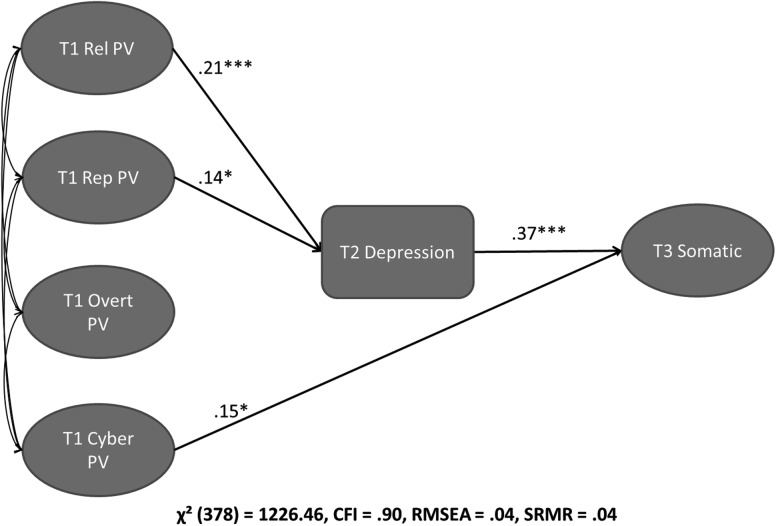
Figure 1.
Structural model: Time 1 peer victimization and Time 2 depressive symptoms predicting Time 3 somatic symptoms.
Significant control variables:
Relational PV on gender (β = .11, p < .01), ethnicity (β = −.11, p < .01).Reputational PV on gender (β = .19, p < .001), ethnicity (β = −.11, p < .001).Overt PV on gender (β = −.20, p < .001; ethnicity (β = −0.08, p < .05; age (β = −.10, p < .01).Cyber PV on gender (β = .11, p < .001); ethnicity (β = −.10, p < .01); age (β = −.05, p < .05).Depression on gender (β = .13, p < .001).Somatic complaints on gender (β = .11, p < .01).
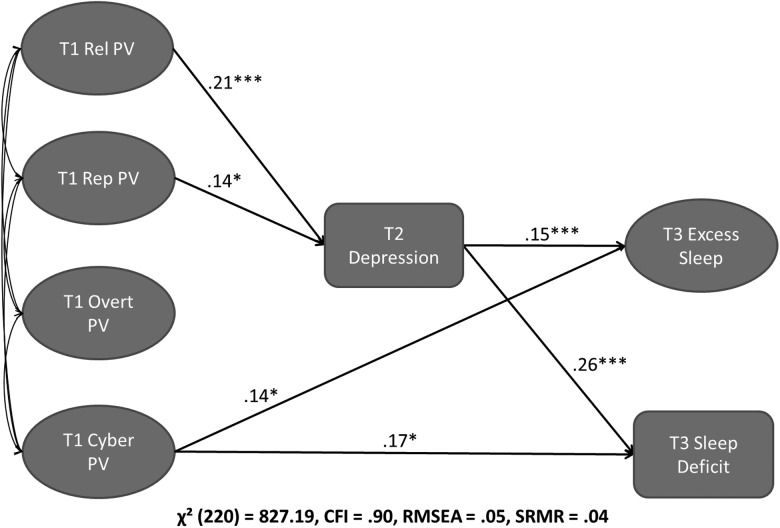
Figure 2.
Structural model: Time 1 peer victimization and Time 2 depressive symptoms predicting Time 3 sleep symptoms.
Significant control variables:
Relational PV on gender (β = .11, p < .01), ethnicity (β = −.11, p < .01).Reputational PV on gender (β = .19, p < .001), ethnicity (β = −.11, p < .001).Overt PV on gender (β = −.19, p < .001; ethnicity (β = −0.08, p < .05; age (β = −.10, p < .01).Cyber PV on gender (β = .12, p < .001); ethnicity (β = −.09, p < .01); age (β = −.06, p < .05).Depression on gender (β = .12, p < .001).Sleep deficit on gender (β = .10, p < .05).
Prospective Associations Between PV and Physical Health Outcomes With Depression and Social Anxiety as Mediators
Models With Depressive Symptoms
A structural model was tested with depressive symptoms as a mediator between PV and somatic complaints (Model 1) and it displayed adequate fit with the data (see Table II for fit statistics).3 As depicted in Figure 1, relational PV (β = .21) and reputational PV (β = .14) were associated with depressive symptoms, and depressive symptoms were related to greater somatic complaints, suggesting that depressive symptoms may mediate between these forms of PV and somatic complaints. In fact, two (of three hypothesized) significant indirect relationships were found: between relational PV and somatic complaints (β = .08), and between reputational PV and somatic complaints (β = .05) (see Figure 1 and Table II). Cyber PV was directly associated with somatic complaints (β = .15). As expected, no paths were significant for overt PV.
Table II.
Summary of Findings From the Structural Models
| Model | Direct predictor of outcome | Mediator | Significant indirect pathway(s) | Outcome | Overall model fit statistics |
|---|---|---|---|---|---|
| 1 | Cyber PV | Depression | Relational PV mediated by depression | Somatic complaints | χ2 (378) = 1,226.46, CFI = .90, RMSEA = .04, SRMR = .04 |
| (β = .15*) | (β = .08***) | ||||
| Reputational PV mediated by depression | |||||
| (β = .05*) | |||||
| 2 | Cyber PV | Depression | Relational PV mediated by depression | Sleep deficits | χ2 (220) = 827.19, CFI = .90, RMSEA = .05, SRMR = .04 |
| (β = .17*) | (β = .06***) | ||||
| 2 | Cyber PV | Depression | Relational PV mediated by depression | Excess sleep | χ2 (220) = 827.19, CFI = .90, RMSEA = .05, SRMR = .04 |
| (β = .14*) | (β = .03**) | ||||
| 3 | Cyber PV | Social anxiety | Relational PV mediated by social anxiety | Somatic complaints | χ2 (376) = 1,207.22, CFI = .90, RMSEA = .04, SRMR = .05 |
| (β = .16*) | (β = .09***) | ||||
| 4 | Cyber PV | Social anxiety | Relational PV mediated by social anxiety | Sleep deficits | χ2 (218) = 806.29, CFI = .90, RMSEA = .05, SRMR = .05 |
| (β = .21**) | (β = .06**) | ||||
| 4 | Cyber PV | Social anxiety | Relational PV mediated by social anxiety | Excess sleep | χ2 (218) = 806.29, CFI = .90, RMSEA = .05, SRMR = .05 |
| (β = .14*) | (β = .04*) |
*p < .05, **p < .01, ***p < .001.
The next structural model was tested with depressive symptoms as a mediator between PV and sleep problems (Model 2), and it displayed adequate fit with data (see Table II and Figure 2). Relational and reputational PV were associated with depressive symptoms, and depressive symptoms were related to sleep deficits (β = .26) and excess sleep (β = .15), suggesting that depressive symptoms may mediate between these forms of PV and sleep problems. Two (of six hypothesized) significant indirect relationships were found: between relational PV and both sleep deficits (β = .06) and sleep excess (β = .03). Direct paths were observed between cyber PV and both sleep deficits (β = .17) and sleep excess (β = .14). No paths were significant for overt PV.
Models With Social Anxiety Symptoms
Similar to the above, Model 3 examined social anxiety as a mediator between PV and somatic complaints, and it displayed adequate fit with the data (see Table II).4 Only relational PV was associated with social anxiety (β = .46, p < .001), which in turn was related to somatic complaints (β = .20, p < .001). One significant indirect relationship (of three hypothesized) was found between relational PV and somatic complaints (β = .09, p < .001). As with Model 1 (for depression) we found a direct pathway between cyber PV and somatic complaints (β = .16), and no significant paths for overt PV. In addition, reputational PV was not directly or indirectly associated with somatic complaints.
Finally, Model 4 examined social anxiety as a mediator between PV and sleep problems, and also displayed adequate fit (see Table II). Only relational PV was associated with social anxiety (β = .46, p < .001), which in turn was related to sleep deficits (β = .12, p < .01) and sleep excess (β = .09, p < .05). Two (of six hypothesized) significant indirect relationships were found: between relational PV and sleep deficits (β = .06, p < .01) and between relational PV and sleep excess (β = .04, p < .05). As with Model 2 (for depression), we found direct pathways between cyber PV and both sleep deficits (β = .21, p < .01) and excess sleep (β = .14, p < .05), and no significant paths for overt PV. Reputational PV was not associated with sleep problems.
Discussion
Although PV is common during adolescence (De Los Reyes & Prinstein, 2004) and cyber PV appears to be on the rise (Madden et al., 2013), little is known about the ways PV may affect adolescents’ health. To our knowledge, this is the first study to examine comprehensively and prospectively the associations between relational, reputational, overt, and cyber PV and older adolescents’ somatic complaints and sleep problems, and to evaluate potential mediating pathways that underlie these associations. Key findings are discussed below.
Cyber PV as a Potential Contributor to Somatic Complaints and Sleep Problems
Perhaps the most striking finding from the current study pertains to cyber PV, which has not been studied previously in relation to older adolescents’ health and sleep concerns. Our findings indicate that aversive peer experiences that occur via technology, such as having an embarrassing photo sent to peers or a mean message posted on the Internet, may contribute directly to adolescents’ somatic complaints and sleep difficulties, even when taking into account the potential overlap between cyber PV and more traditional types of PV.
There are several reasons why cyber PV may be particularly harmful to adolescents’ health and sleep. Cyber victimization possesses fewer time and location constraints (i.e., texting or online postings can occur any time, regardless of location) and can be distributed to a wide audience (Sticca & Perren, 2013). Technology also makes it difficult for adolescents to escape the reach of cyber PV, compared with other forms of PV. Thus, it is not surprising that cyber PV might make adolescents “feel sick” (e.g., report nausea, headaches) and possibly lead them to have trouble sleeping, especially falling or staying asleep. Because adolescents frequently are online, texting friends, or using social media in the evening, even after “lights out,” an aversive cyber experience has high potential for interfering with their sleep (Van den Bulck, 2007).
Interestingly, neither depressive symptoms nor social anxiety appeared to mediate associations between adolescents’ cyber PV and their somatic complaints or sleep difficulties, even though bivariate correlations revealed that cyber PV was significantly related to depressive symptoms and to social anxiety. Perhaps other strong emotions, such as fear, panic, or anger, function as mediators between cyber PV and adolescent health. It also is possible that cyber PV leads to a strong physiological stress response, such as altered levels of cortisol or blood pressure (Stroud et al., 2009), that in turn affects adolescents’ somatic symptoms and sleep difficulties. Knack, Jensen-Campbell, and Baum (2011) recently found that early adolescents who experienced PV exhibited altered cortisol levels and reported more frequent health problems and health care visits. Although findings were mixed, there was some support for the role of cortisol activity in mediating the pathway between PV and certain health outcomes. Further research that examines potential physiological pathways between cyber PV and health and sleep outcomes in adolescents would be important and desirable.
Furthermore, it is possible that adolescents’ internalized distress (e.g., symptoms of depression and social anxiety) moderates, rather than mediates, associations between cyber PV and physical health. This notion would be consistent with Biebl and colleagues’ (2011) findings, in a very small sample, that health problems were highest among youth who reported both PV and emotional distress. Research with younger adolescents (Salmivalli, Sainioa, & Hodgesac, 2013) also reveals that not all youth who are the targets of cyber PV report depressive symptoms. Additional multiwave studies are needed to better understand mechanisms that link cyber PV with poorer adolescent health and sleep disturbances, particularly in light of the high and increasing use of technology among older adolescents (Madden et al., 2013).
Overall, our findings indicate that cyber PV experiences may contribute directly to adolescents’ somatic complaints and sleep difficulties. Pediatric psychologists and other health care providers might do well to assess adolescents’ peer experiences, especially cyber PV, when they encounter youth with unexplained physical complaints, such as headaches, nausea, and digestive problems. In addition, sleep problems, most notably sleep deficits, could signal that an adolescent is experiencing cyber PV. Alternatively, when treating adolescents who report cyber PV, health care providers should be prepared to assess for and help protect against the possible development of somatic and sleep problems.
Internal Distress as a Potential Mediator Between Relational PV and Health
A second key finding was that symptoms of depression and social anxiety might mediate associations between relational PV and adolescents’ somatic complaints and sleep difficulties. Adolescents who are the targets of relational PV, such as by being socially excluded, often by friends, consistently report high levels of social anxiety and depression (La Greca & Harrison, 2005; McLaughlin, Hatzenbuehler, & Hilt, 2009; Siegel et al., 2009). Our findings significantly extend this line of research by indicating that adolescents who are relationally victimized not only experience internalized distress, but also are likely to report health and sleep problems.
These findings suggest the possibility that shared elements of social anxiety and depression, such as negative emotionality (Garber & Weersing, 2010), could underlie the link between relational PV and adolescents’ health and sleep problems. Alternatively, given relational PV’s stronger associations with social anxiety (β = .46) than with depressive symptoms (β = .21), consistent with prior research (e.g., La Greca & Harrison, 2005), it is possible that the physiological reactivity associated with social anxiety (Beidel, Turner, & Dancu, 1985) could contribute to adolescents’ somatic and sleep problems. In this scenario, depressive symptoms might link PV with health and sleep outcomes owing to its high co-occurrence with social anxiety (Garber & Weersing, 2010). Further research that examines specific emotional and physiological pathways that contribute to the health and sleep effects of relational PV would be informative.
In contrast, reputational PV, or being the target of peers’ efforts to cause embarrassment or damage one’s reputation, was linked with adolescents’ somatic complaints only via its association with depressive symptoms. Consistent with our findings, other adolescent studies have found reputational PV to be associated with depressive symptoms (McLaughlin et al., 2009) but not with social anxiety (Siegel et al., 2009). This suggests the possibility that reputational PV may lead to feelings of hopelessness or anhedonia that are specific to depression (Abramson et al., 1989), and which, in turn, might interfere with sleep and contribute to somatic complaints.
Overall, our findings for reputational PV appear a bit more limited than those for cyber or relational PV. One caveat, however, is that the most adverse aspect of reputational PV, which is a public effort to damage one’s reputation, may have been captured by our measure of cyber PV. Specifically, several items on the C-PEQ reflect reputational PV that is perpetrated electronically (e.g., “A peer posted pictures of me that made me look bad via electronic media,” and “A peer posted mean things about me publicly via electronic media”). Our findings suggest that the more public and widespread efforts are to damage adolescents’ reputations, the more likely the adolescent victims will display health and sleep problems.
Finally, as with previous research, overt PV was not linked with any internalizing (e.g., Siegel et al., 2009; Storch et al., 2005) or physical health outcomes, when other types of PV were controlled. In the present study, overt PV was infrequent, its frequency declined with adolescent age, and it co-occurred with both relational and cyber PV (e.g., correlations of .47 and .56, respectively). In all likelihood, the null findings reflect that youth who experience overt PV also experience other forms of PV, which are related to somatic complaints and sleep difficulties.
Other Considerations: Ethnicity and Gender
A strength of our study was its focus on a sample of predominantly Hispanic adolescents, extending previous research that has focused almost exclusively on youth from nonminority backgrounds. Interestingly, we found that Hispanic adolescents reported lower levels of each type of PV compared with their non-Hispanic peers. Previous findings have been mixed regarding the associations between Hispanic ethnicity and PV (e.g., Juvonen, Graham, & Schuster, 2003; Nansel et al., 2001). Our results are consistent with Nansel et al. (2001) who did not find Hispanic youth to be more vulnerable to PV than youth from other ethnic groups. In fact, in our study, Hispanic adolescents were less likely to report each type of PV than other youth (although the magnitudes of the effects were small). Our study was conducted in South Florida, where Hispanic youth represent the majority population, and which may have protected them, to a certain extent, from experiencing PV relative to their non-Hispanic peers. Majority group status might also explain why Hispanic adolescents in our study reported less social anxiety than other youth. The limited research that exists has not found ethnic differences in social anxiety (Ginsburg, La Greca, & Silverman, 1998; Ginsburg & Silverman, 1996), suggesting that group status, rather than ethnicity, may impact adolescents’ experience of internalized distress.
Concerning gender differences, our findings are consistent with prior studies finding that boys report more overt PV than girls (e.g., Prinstein, Boergers, & Vernberg, 2001), and girls report more relational and reputational PV than boys (La Greca & Harrison, 2005; Peskin, Tortolero, & Markham, 2006). Further, our findings that girls report more internalizing symptoms (Essau et al., 2010; Hyde et al., 2008; La Greca & Harrison, 2005) and health complaints (Fichtel & Larsson, 2002; Hunfeld et al., 2001; Titova et al., 2015) are also consistent with the existing literature. Future studies might consider whether girls or boys are at greater risk for experiencing the negative psychological and physical health effects of PV.
Finally, our finding that older age is associated with less overt PV is consistent with the literature (e.g., Wang et al., 2009). As adolescents age, their peer aggression may focus on more subtle and less observable ways to harm others.
Strengths and Limitations
The study’s strengths include a large community sample of adolescents, assessments conducted across a 3-month period, a comprehensive evaluation of PV experiences that included cyber PV, and efforts to examine potential mediating pathways. Nevertheless, several limitations should be considered.
First, we relied on adolescents’ self-reports, as is typical of research on PV (De Los Reyes & Prinstein, 2004; McLaughlin et al., 2009; Wang, Iannotti, Luk, & Nansel, 2010). Although adolescents may be the best informants for their peer relationships and for internalized distress (La Greca & Lemanek, 1996), future studies might incorporate additional informant sources, such as peer or parent reports. Medical records or physician visits also could be used to index health complaints. Second, our assessment of sleep problems was limited by a small number of items; more detailed parent- and child-report measures or biotrackers could be used in future studies to assess sleep difficulties. In general, efforts to incorporate physiological measures (e.g., cortisol, blood pressure, or heart rate reactivity) could help to elucidate biological pathways linking PV with health and sleep difficulties. Third, we focused on social anxiety as a potential mediator because of its strong association with adolescent PV in previous studies. However, future investigations might also consider the role of other types of anxiety (e.g., generalized anxiety, panic) in understanding the relationships between PV and physical health problems. Fourth, adolescents predominantly came from Hispanic backgrounds and rates of participation were somewhat low; thus, caution is needed in generalizing this study’s findings. Fifth, we drew on a community sample of adolescents with relatively low levels of psychological and physical distress. Future research with clinically distressed populations may be beneficial for understanding the health impact of PV. Sixth, the amount of variance accounted for in the statistical models was low to moderate, as is typical of research on PV, given that other biological, genetic, and environmental variables play a role in psychological and physical health (Reijntjes et al., 2010). Seventh, our data collection occurred over a 3-month period, which may have been too brief to detect meaningful changes and may have contributed to some overlap of measurements. We were unable to control for prior levels of depressive, social anxiety, or physical health symptoms (see Footnote 2), perhaps owing to the relatively short period in between assessments. We also were unable to determine if PV occurred at one time point or was ongoing. As a result, our prospective findings are suggestive and warrant replication. Future prospective studies might use measures of mediating processes that are more sensitive to change over short periods, and/or consider conducting assessments across longer time intervals, such as 1 year or longer, to better evaluate directionality and causality.
Despite the above, the study significantly extends previous research by examining the health effects of PV among older adolescents, an understudied population, and by comprehensively assessing PV, including cyber PV. This study also draws attention to psychological processes (e.g., negative emotionality) that might underlie associations between PV and adolescents’ health problems.
Conclusions and Implications
The findings hold important implications for pediatric psychologists. First, it would be useful to routinely assess adolescents’ peer relationships and ask about PV and cyber PV, when encountering adolescents with unexplained physical or sleep complaints. Similarly, it would be useful to assess physical health symptoms in youth who disclose PV concerns. Second, health promotion efforts directed toward developing better sleep hygiene (e.g., Dewald-Kaufmann, Oort, & Meijer, 2014) might address how peer experiences affect sleep, perhaps by incorporating psychoeducation on the safe and appropriate use of social media and by encouraging teens to reduce their technology use before bedtime. Finally, programs to reduce bullying and PV (e.g., Cowie & Olafsson, 2001; Stevens, De Bourdeaudhuii, & Van Oost, 2000) could be adapted to foster ways of coping with symptoms of depression and social anxiety, as well as to facilitate appropriate in-person and online peer relationship skills to limit or reduce adolescents’ future PV experiences. Such programs also might target adolescents’ physical health and sleep problems as important intervention outcomes, in addition to their psychological functioning.
Funding
This research was supported in part by a Cooper Fellowship Award (PI = La Greca) and by the National Institute of Child and Human Development (T32HD07510; “Health Behavior Research in Minority Pediatric Populations”).
Conflicts of interest: None declared.
Footnotes
1 At Time 1, 1,067 adolescents participated; at Time 2, 1,047 adolescents participated; and at Time 3, 1,000 adolescents participated. Nonparticipation was predominantly owing to school absence on testing days.
2 We first attempted to run the structural models with PV assessed at Time 1, the mediator at Time 2 (controlling for Time 1), and physical health symptoms at Time 3 (controlling for Time 1 and Time 2). However, due to the strong correlations among study constructs across time points, this model proved a poor fit for the data for both mediators: for depressive symptoms (e.g., for the outcome of somatic complaints: CFI = .73, RMSEA = .05, SRMR = .09) and social anxiety symptoms (e.g., for the outcome of somatic complaints: CFI = .67, RMSEA = .06, SRMR = .09). It was evident from the factor loadings that nearly all of the variance in the mediator and outcome variables was being accounted for by their earlier (Time 1 and/or Time 2) control variables and the fit could not be sufficiently improved to justify this model structure. For example, correlations between Time 1 and Time 2 social anxiety (r = .76) and depression (r = .62) were high, as were correlations between Time 1 and Time 3 somatic complaints (r = .61). Thus, the prospective models were run without controls for prior levels of the mediator or outcome variables.
3 In our depression models (Models 1 and 2), the R2 for depression was 14%, for somatic symptoms was 26%, for sleep deficit symptoms was 16%, and for excess sleep was 7%.
4 In our social anxiety models (Models 3 and 4), the R2 for social anxiety was 22%, for somatic symptoms was 16%, for sleep deficit symptoms was 10%, and for excess sleep was 6%.
References
- Abramson L. Y, Metalsky G. I., Alloy L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review , 96, 358–372. [Google Scholar]
- Achenbach T. M., Rescorla L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Alfano C. A., Ginsburg G. S., Kingery J. N. (2007). Sleep-related problems among children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry , 46, 224–232. [DOI] [PubMed] [Google Scholar]
- Anderson E., Hope D. A. (2008). A review of the tripartite model for understanding the link between anxiety and depression in youth. Clinical Psychology Review , 28, 275–287. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y., Lamy D., Pergamin L., Bakermans-Kranenburg M. J., van Ijzendoorn M. H. (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin , 133, 1–24. [DOI] [PubMed] [Google Scholar]
- Bardone A. M., Moffitt T. E., Caspi A., Dickson N., Stanton W. R., Silva P. A. (1998). Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. Journal of the American Academy of Child and Adolescent Psychiatry , 37, 594–601. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., Brown G. K. (1996). Manual for the beck depression inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beidel D. C., Turner S. M., Dancu C. V. (1985). Physiological, cognitive and behavioral aspects of social anxiety. Behaviour Research and Therapy , 23, 109–117. [DOI] [PubMed] [Google Scholar]
- Biebl S. J. W., DiLalla L. F., Davis E. K., Lynch K. A., Shinn S. O. (2011). Longitudinal associations among peer victimization and physical and mental health problems. Journal of Pediatric Psychology , 36, 868–877. [DOI] [PubMed] [Google Scholar]
- Carlo G., Knight G., McGinley M., Zamboanga B., Jarvis L. (2010). The multidimensionality of prosocial behaviors and evidence of measurement equivalence in Mexican American and European American early adolescents. Journal of Research on Adolescence , 20, 334–358. [Google Scholar]
- Chabrol H., Montovany A., Chouicha K., DuConge E. (2002). Study of the CES-D on a sample of 1,953 adolescent students. Encephale , 28, 429–432. [PubMed] [Google Scholar]
- Clark L. A., Watson D. (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology , 100, 316–336. [DOI] [PubMed] [Google Scholar]
- Cowie H., Olafsson R. (2001). The role of peer support in helping the victims of bullying in a school with high levels of aggression. School Psychology International , 21, 79–95. [Google Scholar]
- Dahl R. E., Lew D. S. (2002). Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health , 31, 175–184. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Prinstein M. J. (2004). Applying depression-distortion hypotheses to the assessment of peer victimization in adolescents. Journal of Clinical Child and Adolescent Psychology , 33, 325–335. [DOI] [PubMed] [Google Scholar]
- Dewald-Kaufmann J. F., Oort F. J., Meijer A. M. (2014). The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: A randomized controlled trial. Journal of Child Psychology and Psychiatry , 55, 273–283. [DOI] [PubMed] [Google Scholar]
- Dinkes R., Cataldi E. F., Lin-Kelly W. (2007). Indicators of school crime and safety: 2007. Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education. [Google Scholar]
- Essau C. A., Lewinsohn P. M., Seeley J. R., Sasagawa S. (2010). Gender differences in the developmental course of depression. Journal of Affective Disorders , 127, 185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtel A., Larsson B. (2002). Psychosocial impact of headache and comorbidity with other pains among Swedish school adolescents. Headache: The Journal of Head and Face Pain , 42, 766–775. [DOI] [PubMed] [Google Scholar]
- Garber J., Weersing V. R. (2010). Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology , 17, 293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg G., La Greca A. M., Silverman W. S. (1998). Social anxiety in children with anxiety disorders. Relation with social and emotional functioning. Journal of Abnormal Child Psychology , 26, 175–185. [DOI] [PubMed] [Google Scholar]
- Ginsburg G. S., Silverman W. K. (1996). Phobic and anxiety disorders in Hispanic and Caucasian youth. Journal of Anxiety Disorders , 10, 517–528. [Google Scholar]
- Hawker D. S., Boulton M. J. (2000). Twenty years’ research on peer victimization and psychosocial maladjustment: A meta-analytic review of cross-sectional studies. Journal of Child Psychology and Psychiatry , 41, 441–455. [PubMed] [Google Scholar]
- Herge W. M., La Greca A. M., Flitter C., Auslander B., Thomas J. F., Short M. (2011, April). Predictors of children’s sleep disruption following a natural disaster. Presented at the biennial National Conference on Pediatric Psychology, San Antonio, TX. [Google Scholar]
- Houbre B., Tarquinio C., Thuillier I., Hergott E. (2006). Bullying among students and its consequences on health. European Journal of Psychology of Education , 21, 183–208. [Google Scholar]
- Hunfeld J. A. M., Perquin C. W., Duivenvoorden H. J., Hazebroek-Kampschreur A. A. J. M., Passchier J., van Suijlekom-Smit L. W. A., van der Wouden J. C. (2001). Chronic pain and its impact on quality of life in adolescents and their families. Journal of Pediatric Psychology , 26, 145–153. [DOI] [PubMed] [Google Scholar]
- Hyde J. S., Mezulis A. H., Abramson L. Y. (2008). The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review , 115, 291–313. [DOI] [PubMed] [Google Scholar]
- Inderbitzen-Nolan H. M., Walters K. S. (2000). Social Anxiety Scale for Adolescents: Normative data and further evidence of construct validity. Journal of Clinical Child Psychology , 29, 360–371. [DOI] [PubMed] [Google Scholar]
- Javaheri S., Storfer-Isser A., Rosen C. L., Redline S. (2008). Sleep quality and elevated blood pressure in adolescents. Circulation , 118, 1034–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson E. O., Breslau N. (2001). Sleep problems and substance use in adolescence. Drug and Alcohol Dependence , 64(1), 1–7. [DOI] [PubMed] [Google Scholar]
- Juvonen J., Graham S., Schuster M. A. (2003). Bullying among young adolescents: The strong, the weak, and the troubled. Pediatrics , 112, 1231–1237. [DOI] [PubMed] [Google Scholar]
- Juvonen J., Gross E. F. (2008). Extending the school grounds? Bullying experiences in cyberspace. Journal of School Health, 78, 496–505. [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2011). Principles and practice of structural equation modeling (3rd ed). New York, NY: The Guilford Press. [Google Scholar]
- Knack J. M., Jensen-Campbell L. A., Baum A. (2011). Worse than sticks and stones? Bullying is associated with altered HPA axis functioning and poorer health. Brain and Cognition , 77, 183–190. [DOI] [PubMed] [Google Scholar]
- Kowalski R. M., Giumetti G. W., Schroeder A. N., Lattanner M. R. (2014). Bullying in the digit age: A critical review and meta-analysis of cyberbullying research among youth. Psychological Bulletin , 140, 1073–1137. [DOI] [PubMed] [Google Scholar]
- Kowalski R. M., Limber S. P. (2007). Electronic bullying among middle school students. Journal of Adolescent Health , 41, S22–S30. [DOI] [PubMed] [Google Scholar]
- La Greca A. M., Harrison H. M. (2005). Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? Journal of Clinical Child and Adolescent Psychology , 34, 49–61. [DOI] [PubMed] [Google Scholar]
- La Greca A. M., Ingles C. J., Lai B. S., Marzo J.C. (2015). Social Anxiety Scale for Adolescents: Factorial invariance across gender and age in Hispanic adolescents. Assessment , 22, 224–232. [DOI] [PubMed] [Google Scholar]
- La Greca A. M., Lai B. S., Auslander B., Short M., Thomas J. F., Herge W., Taylor C., Silverman W. (2010, August). The impact of natural disasters on children’s physical health. In A. M. La Greca (Chair), Health outcomes in children affected by trauma. Presented at the biennial meeting of the International Congress of Behavioral Medicine, Washington, DC. [Google Scholar]
- La Greca A. M., Lemanek K. (1996). Assessment as a process in pediatric psychology. Journal of Pediatric Psychology , 21, 137–151. [DOI] [PubMed] [Google Scholar]
- La Greca A. M., Lopez N. (1998). Social anxiety among adolescents: Linkages with peer relations and friendships. Journal of Abnormal Child Psychology , 26, 83–94. [DOI] [PubMed] [Google Scholar]
- La Greca A. M., Mufson L., Ehrenreich-May J., Girio-Herrera E., Chan S. F., Ehrlich C. (2014, October). Developing a school-based preventive intervention (PEERS/UTalk) for peer victimized adolescents at risk for social anxiety disorder and depression: Results from an open trial. Presented at the National Conference in Clinical Child and Adolescent Psychology, Lawrence, KS. [Google Scholar]
- Lai B. S., La Greca A. M., Auslander B. A., Short M. B. (2013). Children’s symptoms of posttraumatic stress and depression after a natural disaster: Comorbidity and risk factors. Journal of Affective Disorders , 146, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landoll R. R., La Greca A. M., Lai B. S., Chan S. F., Herge W. M. (2015). Cyber victimization: Prospective associations with adolescent social anxiety and depressive symptoms. Journal of Adolescence , 42, 77–86. [DOI] [PubMed] [Google Scholar]
- Lee Y. C., Lu B., Edwards R. R., Wasan A. D., Nassikas N. J., Clauw D. J., Solomon D. H., Karlson E. W. (2013). The role of sleep problems in central pain processing in rheumatoid arthritis. Arthritis and Rheumatism , 65(1), 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A. (2015). Teens, social media, and technology: Overview 2015. Report of the Pew Research Center, April 2015. Retrieved from www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/ [Google Scholar]
- Li Q. (2007). New bottle but old wine: A research of cyberbullying in schools. Computers in Human Behavior , 23, 1777–1791. [Google Scholar]
- Madden M., Lenhart A., Duggan M., Cortesi S., Gasser U. (2013). Teens and technology 2013. Washington, DC: Pew Internet and American Life Project. [Google Scholar]
- McLaughlin K. A., Hatzenbuehler M. L., Hilt L. M., (2009). Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting and Clinical Psychology , 77, 894–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen L., Muthen B. (2011). MPlus (Version 6.11) [Computer software]. Los Angeles, CA: Muthen & Muthen. [Google Scholar]
- Nansel T. R., Overpeck M., Pilla R. S., Ruan W. J., Simons-Morton B., Scheidt P. (2001). Bullying behaviors among US youth: Prevalence and association with psychosocial adjustment. Journal of the American Medical Association , 285, 2094–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natvig G. K., Albrektsen G., Qvarnstrom U. (2001). School-related stress experience as a risk factor for bullying behavior. Journal of Youth and Adolescence , 30, 561–575. [Google Scholar]
- Patchin J., Hinduja S. (2012). Cyberbullying: An update and synthesis of the research. In Patchin J., Hinduja S. (Eds.), Cyberbullying prevention and response: Expert perspectives (pp. 13–35). New York, NY: Routledge. [Google Scholar]
- Peskin M. L., Tortolero S. R., Markham C. M. (2006). Bullying and victimization among Black and Hispanic adolescents. Adolescence , 41, 467–484. [PubMed] [Google Scholar]
- Prinstein M. J., Boergers J., Vernberg E. M. (2001). Overt and relational aggression adolescents: Social-psychological adjustment of aggressors and victims. Journal of Clinical Child Psychology , 4, 479–491. [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement , 1, 385–401. [Google Scholar]
- Reijntjes A., Kamphuis J. H., Prinzie P., Telch J. (2010). Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse & Neglect , 34, 244–252. [DOI] [PubMed] [Google Scholar]
- Rigby K. (1998). The relationship between reported health and involvement in bully/victim problems among male and female secondary schoolchildren. Journal of Health Psychology , 3, 465–476. [DOI] [PubMed] [Google Scholar]
- Rigby K. (1999). Peer victimisation at school and the health of secondary school students. British Journal of Educational Psychology , 69, 95–104. [DOI] [PubMed] [Google Scholar]
- Rigby K. (2001). Health consequences of bullying and its prevention in schools. In Juvonen J., Graham S. (Eds.), Peer harassment in school: The plight of the vulnerable and victimized (pp. 310–331). New York, NY: Guilford Press. [Google Scholar]
- Rigby K. (2003). Consequences of bullying schools. Canadian Journal of Psychiatry , 48, 583–590. [DOI] [PubMed] [Google Scholar]
- Rohde P., Lewinsohn P. M., Seeley J. R. (1994). Are adolescents changed by an episode of major depression? Journal of American Academy of Child and Adolescent Psychiatry , 33, 1289–1298. [DOI] [PubMed] [Google Scholar]
- Rushton J. L., Forcier M., Schectman R. M. (2002). Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. Journal of the American Academy of Child & Adolescent Psychiatry , 41, 199–205. [DOI] [PubMed] [Google Scholar]
- Salmivalli C., Sainio M., Hodges E. V. E. (2013). Electronic victimization: Correlates, antecedents, and consequences among elementary and middle school students. Journal of Clinical Child and Adolescent Psychology , 42, 442–453. [DOI] [PubMed] [Google Scholar]
- Sareen J., Jacobi F., Cox B. J., Belik S. L., Clara I., Stein M. B. (2006). Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Archives of Internal Medicine , 166, 2109–2116. [DOI] [PubMed] [Google Scholar]
- Shiromani P. J., Horvath T., Redline S., Van Cauter E. (Eds.) (2012). Sleep loss and obesity: Intersecting epidemics. New York, NY: Springer Science + Business Media. [Google Scholar]
- Siegel R. S., La Greca A. M., Harrison H. M. (2009). Peer victimization and social anxiety in adolescents: Prospective and reciprocal relationships. Journal of Youth and Adolescence , 38, 1096–1109. [DOI] [PubMed] [Google Scholar]
- Sourander A., Brunstein Klomek A., Ikonen M., Lindroos J., Luntamo T., Koskelainen M., Ristkari T., Helenius H. (2010). Psychosocial risk factors associated with cyberbullying among adolescents: A population-based study. Archives of General Psychiatry , 67, 720–728. [DOI] [PubMed] [Google Scholar]
- Steinberg A. M., Brymer M. J., Decker K. B., Pynoos R. S. (2004). The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports , 6, 96–100. [DOI] [PubMed] [Google Scholar]
- Stevens V., De Bourdeaudhuij I., Van Oost P. (2000). Bullying in Flemish schools: An evaluation of anti-bullying intervention in primary and secondary schools. The British Journal of Educational Psychology , 70, 195–210. [DOI] [PubMed] [Google Scholar]
- Sticca F., Perren S. (2013). Is cyberbullying worse than traditional bullying? Examining the differential roles of medium, publicity, and anonymity for the perceived severity of bullying. Journal of Youth and Adolescence , 42, 739–750. [DOI] [PubMed] [Google Scholar]
- Storch E. A., Esposito L. E. (2003). Peer victimization and posttraumatic stress among children. Child Study Journal , 33, 91–98. [Google Scholar]
- Storch E. A., Masia-Warner C., Crisp H., Klein R. G. (2005). Peer victimization and social anxiety in adolescence: A prospective study. Aggressive Behavior , 31, 437–452. [Google Scholar]
- Storch E. A., Masia-Warner C., Dent H. C., Roberti J. W., Fisher P. H. (2004). Psychometric evaluation of the Social Anxiety Scale for Adolescents and the Social Phobia and Anxiety Inventory for Children: Construct validity and normative data. Anxiety Disorders , 18, 665–679. [DOI] [PubMed] [Google Scholar]
- Storch E. A., Nock M. K., Masia-Warner C., Barlas M. E. (2003). Peer victimization and social-psychological adjustment in Hispanic and African-American children. Journal of Child and Family Studies , 12, 439–452. [Google Scholar]
- Stroud L. L., Foster E., Papandonatos G. D., Handwerger K., Granger D. A., Kivlighan K. T., Niaura R. (2009). Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology , 21, 47–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titova O. E., Hogenkamp P. S., Jacobsson J. A., Feldman I., Schioth H. B., Benedict C. (2015). Associations of self-reported sleep disturbance and duration with academic failure in community-dwelling Swedish adolescents: Sleep and academic performance at school. Sleep Medicine , 16(1), 87–93. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (2012). Hispanic Heritage Month 2012. Retrieved from http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb12-ff19.html [Google Scholar]
- U.S. Census Bureau (2013). State & County QuickFacts. Retrieved from http://quickfacts.census.gov/qfd/states/12/12086.html [Google Scholar]
- Van den Bulck J. (2007). Adolescent use of mobile phones for calling and for sending text messages after lights out: Results from a prospective cohort study with a one-year follow-up. Sleep , 30, 1220–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Iannotti R. J., Luk J. W., Nansel T. R. (2010). Co-occurrence of victimization from five types of bullying: Physical, verbal, social exclusion, spreading rumors, and cyber. Journal of Pediatric Psychology , 35, 1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Iannotti R. J., Nansel T. R. (2009). School bullying among adolescents in the United States: Physical, verbal, relational, and cyber. Journal of Adolescent Health , 45, 368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]