Abstract
Introduction:
Smoke-free legislation has been a great success for tobacco control but its impact on smoking uptake remains under-explored. We investigated if trends in smoking uptake amongst adolescents differed before and after the introduction of smoke-free legislation in the United Kingdom.
Methods:
Prevalence estimates for regular smoking were obtained from representative school-based surveys for the four countries of the United Kingdom. Post-intervention status was represented using a dummy variable and to allow for a change in trend, the number of years since implementation was included. To estimate the association between smoke-free legislation and adolescent smoking, the percentage of regular smokers was modeled using linear regression adjusted for trends over time and country. All models were stratified by age (13 and 15 years) and sex.
Results:
For 15-year-old girls, the implementation of smoke-free legislation in the United Kingdom was associated with a 4.3% reduction in the prevalence of regular smoking (P = .029). In addition, regular smoking fell by an additional 1.5% per annum post-legislation in this group (P = .005). Among 13-year-old girls, there was a reduction of 2.8% in regular smoking (P = .051), with no evidence of a change in trend post-legislation. Smaller and nonsignificant reductions in regular smoking were observed for 15- and 13-year-old boys (P = .175 and P = .113, respectively).
Conclusions:
Smoke-free legislation may help reduce smoking uptake amongst teenagers, with stronger evidence for an association seen in females. Further research that analyses longitudinal data across more countries is required.
Implications:
Previous research has established that smoke-free legislation has led to many improvements in population health, including reductions in heart attack, stroke, and asthma. However, the impacts of smoke-free legislation on the rates of smoking amongst children have been less investigated. Analysis of repeated cross-sectional surveys across the four countries of the United Kingdom shows smoke-free legislation may be associated with a reduction in regular smoking among school-aged children. If this association is causal, comprehensive smoke-free legislation could help prevent future generations from taking up smoking.
Introduction
Comprehensive smoke-free legislation has been heralded as one of the great successes of tobacco control for a generation, with the four countries of the United Kingdom amongst the first jurisdictions worldwide to adopt it.1,2 Its implementation is associated with several health benefits including improvements in respiratory health in bar workers, reductions in hospital admission for myocardial infarctions, stroke, and asthma in the general population and a reduction in perinatal complications for both pregnant women and their babies.3–7 An extensive international literature has also documented the adverse health effects of exposure to secondhand smoke (SHS) in adults and children.8–11 Fetuses, infants and children are particularly susceptible. In children, SHS exposure increases the risk of sudden infant death, lower respiratory infections (particularly bronchiolitis), asthma and middle ear disease, as well as impairing lung function.
In addition to the direct health benefits, support for smoke-free legislation has been shown to increase following implementation and this has been accompanied by changing social norms about the acceptability both of smoking and of exposing others to SHS.12,13 In Scotland, there was an increase in quitting behavior around the implementation of the ban, followed by a short-term reduction in smoking prevalence in adults but this was not sustained beyond a year.14 Exposure of children to SHS in the home similarly decreased.15,16
Legislation in the four UK countries is similar and broadly meets the definition of comprehensive smoke-free legislation as recommended by the WHO FCTC Article 8 legislation, that is, a ban on smoking in all enclosed public places and workplaces, including bars, restaurants and public transportation.17 Within the United Kingdom, it was implemented first in Scotland in March 2006, then in Wales and Northern Ireland in April 2007 and in England the following July.18 The few exemptions include designated rooms in hotels, care homes and hospices across the United Kingdom.8 In UK adult prisons, smoking is not allowed in communal spaces, but has been allowed in cells and exercise yards. In Scotland and Wales mental health units are also exempted.8
Long-term smoking patterns are typically established in adolescence, with earlier uptake linked to heavier smoking and a lower likelihood of future quitting.19–21 Although smoke-free legislation has been introduced in over 100 countries, most have still not implemented comprehensive legislation. It is possible that comprehensive smoke-free legislation could play an important role in preventing smoking uptake but to our knowledge, this specific hypothesis has not previously been studied.
In this article, we investigate whether trends in smoking uptake amongst children (aged 13 and 15 years) differed before and after the introduction of the comprehensive smoking ban in the four UK countries.
Methods
Data on smoking prevalence among 13- and 15-year-old school children (stratified by sex) were obtained for the four UK countries from four repeat cross sectional surveys: the Smoking, Drinking and Drug Use Among Young People in England survey (SDDYP), the Scottish Schools Adolescent Lifestyle and Substance Use Survey (SALSUS), the Health Behaviour in School-aged Children (HBSC) survey in Wales22–24 and the Young Persons’ Behaviour & Attitudes Survey (YPBAS) in Northern Ireland. The SDDYP and SALSUS are conducted biennially and were chosen in preference to the HBSC surveys in these countries as they are only conducted every 4 years. The HBSC in Wales was generally conducted every 2 years while the YPBAS in Northern Ireland was carried out every 3–4 years. Each survey series asked about smoking using similar questionnaire items, with regular smoking defined as smoking at least one cigarette per week. Children aged 13 and 15 years were studied, since data for these age groups were consistently available across the different surveys and over time. Data on regular smoking prevalence together with available information on sample sizes were extracted from published data. Agencies holding the data were also contacted for further data when required. Year of implementation of smoke-free legislation were entered into the dataset. Ethical approvals for data collection were obtained by survey organizers.
Data were analyzed using segmented linear regression.25 The percentage of regular smokers was the outcome and each annual prevalence estimate from each country contributed one data point. Linear and quadratic terms in time were included to account for secular trends in smoking prevalence. The immediate effect of the intervention was modeled by a dummy variable indicating whether the observation was pre- or post-intervention. To allow for a change in trend in the years following the intervention an additional term, time post intervention, was included. Time invariant differences between countries were modeled as a set of dummy variables with England as the reference country.
Our statistical model is, therefore:
where time and time2 are linear and quadratic terms in years to account for secular trends; interv equals 0 pre-intervention and 1 for the year of intervention onwards; postslope is a count variable of years which starts at 1 from the intervention implementation year but is 0 prior to the intervention; and ε is an error term.
All models were stratified by age (13 and 15 years) and sex. Analyses were run using Stata SE 13.1.
Results
Data were available for 55 time points for the four UK countries (see Supplementary Tables 1 and 2 for full data by country, year, age and sex). A downward trend in recent years was noted for all four countries. For example, the prevalence in 15-year-old boys in England fell from 24% in 1982 to 8% in 2013; equivalent figures for 15-year-old girls in England were 25% to 8%. Across all countries and all years, the mean prevalence (and SD) of self-reported smoking was: 17.6% (SD 5.91) for 15-year-old boys; 23.1% (SD 5.99) for 15-year-old girls; 5.75% (SD 2.59) for 13-year-old boys; and 8.44% (SD 4.01) for 13-year-old girls.
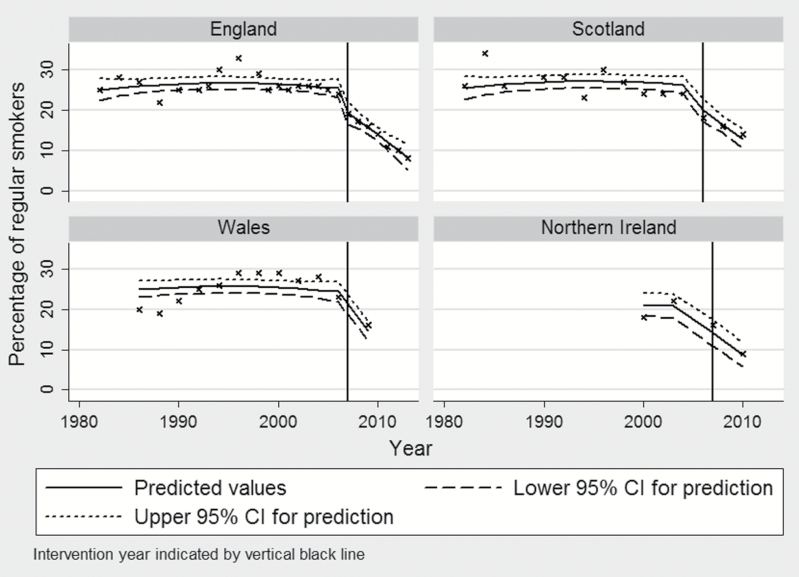
Table 1 shows associations between the introduction of smoke-free legislation and self-reported regular smoking from four separate regression models for each age-sex group (Figure 1 and Supplementary Figures 1–3 depict the results graphically).
Table 1.
Associations Between Smoke-Free Public Places Legislation and Regular Smoking in Adolescents
| Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|
| β | P | Lower 95% CI | Upper 95% CI | β | P | Lower 95% CI | Upper 95% CI | |
| 15-year olds | ||||||||
| Step-change | −3.527 | .175 | −8.681 | 1.628 | −4.307 | .029 | −8.162 | −0.452 |
| Trend change | 0.137 | .842 | −1.240 | 1.514 | −1.516 | .005 | −2.546 | −0.486 |
| Time | 0.005 | .988 | −0.687 | 0.697 | 0.275 | .291 | −0.243 | 0.792 |
| Time2 | −0.011 | .386 | −0.036 | 0.014 | −0.010 | .284 | −0.029 | 0.009 |
| England | REF | REF | REF | REF | REF | REF | REF | REF |
| Scotland | 0.905 | .475 | −1.625 | 3.435 | 0.419 | .658 | −1.473 | 2.311 |
| Wales | −3.205 | .020 | −5.879 | −0.532 | −0.988 | .325 | −2.987 | 1.012 |
| Northern Ireland | −5.439 | .011 | −9.561 | −1.317 | −5.155 | .002 | −8.237 | −2.072 |
| R 2 | 0.6616 | 0.8157 | ||||||
| 13-year olds | ||||||||
| Step-change | −1.634 | .113 | −3.666 | 0.399 | −2.756 | .051 | −5.524 | 0.011 |
| Trend change | 0.078 | .773 | −0.465 | 0.621 | −0.126 | .733 | −0.866 | 0.613 |
| Time | −0.039 | .777 | −0.312 | 0.234 | 0.384 | .043 | 0.013 | 0.756 |
| Time2 | −0.003 | .518 | −0.013 | 0.007 | −0.013 | .056 | −0.027 | 0.000 |
| England | REF | REF | REF | REF | REF | REF | REF | REF |
| Scotland | 1.670 | .002 | 0.672 | 2.668 | 1.505 | .031 | 0.147 | 2.864 |
| Wales | 2.358 | .000 | 1.304 | 3.412 | 5.763 | .000 | 4.328 | 7.198 |
| Northern Ireland | 0.257 | .752 | −1.368 | 1.883 | 0.550 | .619 | −1.663 | 2.764 |
| R 2 | 0.7262 | 0.7884 | ||||||
CI = confidence interval; REF = reference group.
Figure 1.
Model predictions for regular smoking amongst 15-year-old females in the four countries of the United Kingdom.
We found that implementation of the smoke-free legislation was followed by a reduction in regular smoking but, the reduction was only statistically significant for 15-year-old girls. In this group, implementation of smoke-free legislation was associated with a reduction in regular smoking by 4.3% (95% confidence interval [CI] −8.1, −0.45; P = .029). In addition, the prevalence of regular smoking fell by an additional 1.5% per annum post-legislation in this group (95% CI −2.5, −0.49; P = .005). Among 13-year-old girls, the prevalence of regular smoking reduced by 2.8% but this change just failed to reach statistical significance (95% CI −5.5, 0.011; P = .051). There was no evidence of a change in trend post legislation in this age-sex group.
Boys also experienced reductions in the prevalence of regular smoking, but these changes were smaller than their female peers and not statistically significant. Among 15-year-old boys, smoking prevalence fell by 3.5% (95% CI −8.7, +1.6; P = .175) while 13-year-old boys experienced a reduction of 1.6% (95% CI −3.7, +0.4; P = .113).
To ensure that our results were not unduly influenced by countries with few post-intervention data points only, we carried out sensitivity analysis of data from England only and found similar results (Supplementary Table 3).
Discussion
In this study, we tested two a priori hypotheses: first, whether the prevalence of smoking amongst children at age 13 and age 15 differs before and after smoke-free legislation; and second, if the longer-term trend in smoking amongst children changed following the policy. The results from our study suggest that the implementation of smoke-free legislation may have a differential effect on boys and girls in the UK countries. Declines in smoking prevalence amongst school children were associated with the introduction of comprehensive smoke-free legislation within the different UK countries, but only reached statistical significance for 15-year-old females. The results are consistent with a reduction in initiation of smoking amongst the other age-sex groups (as indicated by the direction of effect, with wide 95% CIs), but there was limited statistical power due to few post-observation time points.
Our analysis is based on data which are intended to be representative of school-aged children in the four countries of the United Kingdom. However, some limitations should be noted. First, this analysis cannot establish causality between the introduction of smoke-free legislation and changes in children’s smoking uptake but rather only demonstrates an association. Second, while we have taken care to establish the comparability of questions between countries and over time, survey methods and response rates varied. Third, we have limited power to detect changes in longer-term trends following the intervention and repeating this analysis after more time has elapsed may be helpful. It is possible that future analyses may find similar associations exist amongst males—once adequate power is available to detect smaller effects. Fourth, we lacked information on potentially important covariates (eg, parental home smoking, youth working) which would have allowed better investigation of the legislation’s impact. Lastly, it is possible other policies or interventions may have been introduced around the time of smoke-free legislation (eg, increases in the legal purchasing age) and were responsible for the observed changes. However, disentangling causality may be particularly problematic since smoke-free legislation could have indirectly contributed to the implementation of other interventions by encouraging awareness and debate about tobacco control amongst policymakers and the general public which in turn produced a facilitative environment for tobacco control. For example, smoke-free legislation in public places in Spain was found to encourage tobacco control activities in hospitals.26
There is evidence smoke-free legislation may help trigger smoking cessation for some people, but the effect appears short-lived.27 However, an effect on smoking initiation amongst adolescents would potentially have long-lasting benefits for future generations. Previous research found smoke-free environments in general are associated with reduced likelihood of teenagers initiating smoking,28,29 suggesting an effect is plausible. Indeed, qualitative evidence reported smoke-free legislation itself may result in families avoiding smoking in the home or in front of children, assisting in denormalization of smoking behaviour.30 The public debate that frequently accompanies the introduction of smoke-free legislation may act as an important trigger in this regard. Ethnographic evidence also exists for young people’s subcultures to shift in response to smoke-free legislation,31 making night-time environments (such as pubs/nightclubs) also worthy of investigation. The comprehensive nature of the legislation may therefore serve both to denormalize smoking and alter social environments. This may make the initiation of smoking less likely and could therefore provide the mechanisms by which smoke-free legislation has an effect on adolescent uptake. It is possible the impact of certain types of environment on males and females may differ,32 but this hypothesis needs further examination.
Smoking is an important contributor to gender differences in mortality, accounting for 40% to 60% of the gender gap, but concerns exist that the future burden in females will increase substantially.33 It is possible smoke-free legislation may reduce smoking uptake amongst girls which has important implications for gender equity in the future tobacco epidemic. However, a study of the Spanish experience with smoke-free policy found no effect on smoking prevalence in 15–24-year-olds, with no difference by gender.34
UK smoke-free legislation has previously been found to result in significant declines in SHS in primary school children but the limited available evidence suggests it may have widened inequalities in exposure.35,36 Our results suggest smoke-free legislation may help reduce smoking uptake amongst teenagers, as well as reduce the harmful effects of SHS and triggering smoking cessation. However, investigating impacts on equity of this potential effect is important, since lifelong impacts on inequalities could occur.
Our study provides, to our knowledge, the first evidence to suggest that smoke-free legislation could reduce smoking uptake. Further research analyzing longitudinal data across more countries is required to establish if the association observed is causal. Cross-national comparative research may help determine which aspects of implementation are associated with the greatest reductions in smoking uptake amongst children.
Supplementary Material
Supplementary Tables 1–3 and Figures 1–3 can be found online at http://www.ntr.oxfordjournals.org
Funding
This study received no dedicated funding. SVK was funded by the Chief Scientist Office at the Scottish Health Directorates as part of the of the Evaluation of Social Interventions programme at the MRC/CSO Social & Public Health Sciences Unit (MC_UU_12017/4). GD was funded by the Medical Research Council as part of the Social Patterning of Health over the Lifecourse programme (MC_UU_12017/5).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors would like to thank the children who participated and the researchers responsible for data collection of the original surveys. We would like to particularly acknowledge the help of Mervyn Wilson of the Public Health Information and Research Branch in Northern Ireland’s Department of Health, Social Services and Public Safety who provided access to unpublished data.
References
- 1. Gruer L, Tursan d’Espaignet E, Haw S, Fernández E, Mackay J. Smoke-free legislation: global reach, impact and remaining challenges. Public Health. 2012;126(3):227–229. doi:10.1016/j.puhe.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 2. Pell JP, Haw S. The triumph of national smoke-free legislation. Heart. 2009;95(17):1377–1379. doi:10.1136/hrt.2009.176230. [DOI] [PubMed] [Google Scholar]
- 3. Pell JP, Haw S, Cobbe S, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359(5):482–491. doi:10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 4. Mackay DF, Nelson SM, Haw SJ, Pell JP. Impact of Scotland’s smoke-free legislation on pregnancy complications: retrospective cohort study. PLoS Med. 2012;9(3):e1001175. doi:10.1371/journal.pmed.1001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free legislation and hospitalizations for childhood asthma. N Engl J Med. 2010;363(12):1139–1145. doi:10.1056/NEJMoa1002861. [DOI] [PubMed] [Google Scholar]
- 6. Semple S, Maccalman L, Naji AA, et al. Bar workers’ exposure to second-hand smoke: the effect of Scottish smoke-free legislation on occupational exposure. Ann Occup Hyg. 2007;51(7):571–580. doi:10.1093/annhyg/mem044. [DOI] [PubMed] [Google Scholar]
- 7. Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328(7446):977–980. doi:10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Royal College of Physicians. Passive Smoking and Children: A Report of the Royal College of Physicians. London, United Kingdom: Royal College of Physicians; 2010. www.rcplondon.ac.uk/sites/default/files/documents/passive-smoking-and-children.pdf Accessed October 23, 2015. [Google Scholar]
- 9. Scientific Committee on Tobacco and Health (SCOTH). Secondhand Smoke: Review of Evidence Since 1998. Update of Evidence on Health Effects of Secondhand Smoke. London, United Kingdom: Department of Health; 2004. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4101474 Accessed October 23, 2015. [Google Scholar]
- 10. US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 11. International Agency for Research on Cancer, World Health Organization. Evaluating the Effectiveness of Smoke-Free Policies. Lyon, France: International Agency for Research on Cancer; 2009:9283230132 www.iarc.fr/en/publications/pdfs-online/prev/handbook13/handbook13.pdf Accessed October 23, 2015. [Google Scholar]
- 12. Phillips R, Amos A, Ritchie D, Cunningham-Burley S, Martin C. Smoking in the home after the smoke-free legislation in Scotland: qualitative study. BMJ. 2007;335(7619):553. doi:10.1136/bmj.39301.497593.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown A, Moodie C, Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine Tob Res. 2009;11(8):924–932. doi:10.1093/ntr/ntp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fong GT, Hyland A, Borland R, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control. 2006;15(suppl 3):iii51–iii58. doi:10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Akhtar PC, Haw SJ, Currie DB, Zachary R, Currie CE. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18(5):409–415. doi:10.1136/tc.2009.030627. [DOI] [PubMed] [Google Scholar]
- 16. Holliday J, Moore G, Moore L. Changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales: a repeated cross-sectional study. BMC Public Health. 2009;9(1):430. doi:10.1186/1471-2458-9-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. WHO Framework Convention on Tobacco Control: Guidelines for Implementation of Article 5. 3 Article 8 Article 11 and Article 13. Geneva, Switzerland: World Health Organization; 2009:9241598220. [Google Scholar]
- 18. Cairney P. The role of ideas in policy transfer: the case of UK smoking bans since devolution. J Eur Public Policy. 2009;16(3):471–488. doi:10.1080/13501760802684718. [Google Scholar]
- 19. Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. The course of early smoking: a population-based cohort study over three years. Addiction. 1998;93(8):1251–1260. doi:10.1046/j.1360-0443.1998.938125113.x. [DOI] [PubMed] [Google Scholar]
- 20. Green MJ, Leyland AH, Sweeting H, Benzeval M. Socioeconomic position and adolescent trajectories in smoking, drinking, and psychiatric distress. J Adolesc Health. 2013;53(2):202–208.e202. doi:10.1016/j.jadohealth.2013.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. doi:10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Currie C, Zanotti C, Morgan A. et al. , eds. Social Determinants of Health and Well-Being Among Young People. Health Behaviour in School-Aged Children (HBSC) Study: International Report From the 2009/2010 Survey. Copenhagen, Denmark: WHO Regional Office for Europe; 2012. [Google Scholar]
- 23. Henderson H, Nass L, Payne C, Phelps A, Ryley A. Smoking, Drinking and Drug Use Among Young People in England in 2012. London, United Kingdom: Health and Social Care Information Centre; 2013. www.hscic.gov.uk/catalogue/PUB11334 Accessed July 31, 2015. [Google Scholar]
- 24. Central Survey Unit. Young Persons’ Behaviour & Attitudes Survey 2010. Belfast, Northern Ireland: Northern Ireland Statistics & Research Agency; 2011. www.csu.nisra.gov.uk/survey.asp14.htm Accessed November 22, 2014. [Google Scholar]
- 25. Lagarde M. How to do (or not to do)…Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27(1):76–83. doi:10.1093/heapol/czr004. [DOI] [PubMed] [Google Scholar]
- 26. Martinez C, Fu M, Martinez-Sanchez J, et al. Tobacco control policies in hospitals before and after the implementation of a national smoking ban in Catalonia, Spain. BMC Public Health. 2009;9(1):160. doi:10.1186/1471-2458-9-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Federico B, Mackenbach JP, Eikemo TA, Kunst AE. Impact of the 2005 smoke-free policy in Italy on prevalence, cessation and intensity of smoking in the overall population and by educational group. Addiction. 2012;107(9):1677–1686. doi:10.1111/j.1360-0443.2012.03853.x. [DOI] [PubMed] [Google Scholar]
- 28. Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ. 2000;321(7257):333–337. doi:10.1136/bmj.321.7257.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Farkas AJ, Gilpin EA, White MM, Pierce JP. Association between household and workplace smoking restrictions and adolescent smoking. JAMA. 2000;284(6):717–722. doi:10.1001/jama.284.6.717. [DOI] [PubMed] [Google Scholar]
- 30. Final Report of the Devolution and Constitutional Change Programme. Devolution and Constitutional Change: An ESRC Research Programme 2006. www.devolution.ac.uk/final_report.htm Accessed September 6, 2012.
- 31. Kelly BC. Smoke-free air policy: subcultural shifts and secondary health effects among club-going young adults. Sociol Health Illn. 2009;31(4):569–582. doi:10.1111/j.1467-9566.2008.01150.x. [DOI] [PubMed] [Google Scholar]
- 32. Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60(8):1681–1692. doi:http://dx.doi.org/10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 33. McCartney G, Mahmood L, Leyland AH, Batty GD, Hunt K. Contribution of smoking-related and alcohol-related deaths to the gender gap in mortality: evidence from 30 European countries. Tob Control. 2011;20(2):166–168. doi:10.1136/tc.2010.037929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Regidor E, de Mateo S, Ronda E, et al. Heterogeneous trend in smoking prevalence by sex and age group following the implementation of a national smoke-free law. J Epidemiol Community Health. 2011;65(8):702–708. doi:10.1136/jech.2009.091181. [DOI] [PubMed] [Google Scholar]
- 35. Brown T, Platt S, Amos A. Equity impact of interventions and policies to reduce smoking in youth: systematic review. Tob Control. 2014;23:e98–e105 doi:10.1136/tobaccocontrol-2013-051451. [DOI] [PubMed] [Google Scholar]
- 36. Moore GF, Holliday JC, Moore LAR. Socioeconomic patterning in changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales. Nicotine Tob Res. 2011;13(10):903–910. doi:10.1093/ntr/ntr093. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.