Abstract
Background
Medication dosing errors remain commonplace and may result in potentially life-threatening outcomes, particularly for pediatric patients where dosing often requires weight-based calculations. Novel medication delivery systems that may reduce dosing errors resonate with national healthcare priorities. Our goal was to evaluate novel, prefilled medication syringes labeled with color-coded volumes corresponding to the weight-based dosing of the Broselow Tape, compared to conventional medication administration, in simulated prehospital pediatric resuscitation scenarios.
Methods
We performed a prospective, block-randomized, cross-over study, where 10 full-time paramedics each managed two simulated pediatric arrests in situ using either prefilled, color-coded-syringes (intervention) or their own medication kits stocked with conventional ampoules (control). Each paramedic was paired with two emergency medical technicians to provide ventilations and compressions as directed. The ambulance patient compartment and the intravenous medication port were video recorded. Data were extracted from video review by blinded, independent reviewers.
Results
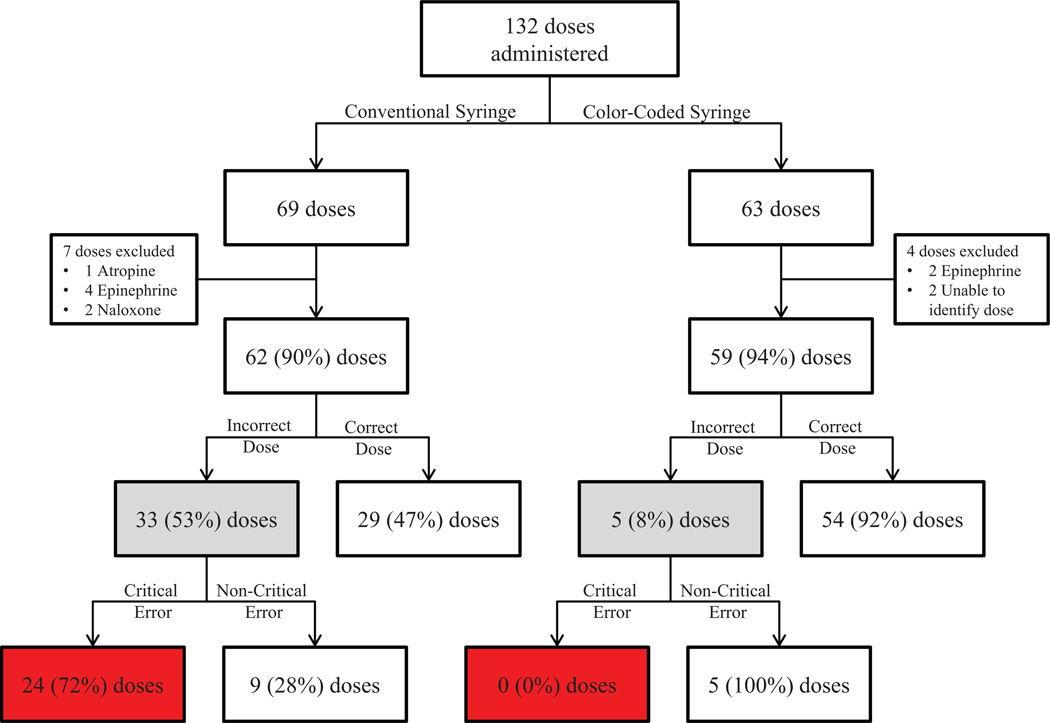
Median time to delivery of all doses for the intervention and control groups was 34 (95% CI: 28–39) seconds and 42 (95% CI: 36–51) seconds, respectively (difference = 9 [95% CI: 4–14] seconds). Using the conventional method, 62 doses were administered with 24 (39%) critical dosing errors; using the prefilled, color-coded syringe method, 59 doses were administered with 0 (0%) critical dosing errors (difference = 39%, 95% CI: 13–61%).
Conclusions
A novel color-coded, prefilled syringe decreased time to medication administration and significantly reduced critical dosing errors by paramedics during simulated prehospital pediatric resuscitations.
Keywords: Cardiac arrest, Pediatrics, Medication administration, Dosing error, Simulation, Emergency medical services
1. Introduction
Medication errors are committed by healthcare providers, including physicians, nurses and paramedics, in virtually all health-care settings.1–7 Since the release of the Institute of Medicine’s (IOM) 1999 report addressing errors in healthcare, increased emphasis has been placed on reducing medical errors from faulty processes, systems, and environments that lead well-meaning clinicians to make mistakes or fail to prevent them.8
One of the highest risks for medication error exists during pediatric emergencies, particularly in the prehospital setting. A single paramedic is often exclusively responsible for gathering and analyzing pertinent information, making prompt decisions, and performing advanced interventions prior to the transfer of a critically ill patient to the emergency department (ED). Often this must be done amidst social chaos and under psychologically stressful conditions, increasing the potential for medication errors.
The color-coded Broselow™ Pediatric Emergency Tape (Vital Signs, Inc., Totowa, NJ) was developed to standardize both weight assessment and drug dosing for pediatric patients in a successful effort to decrease dosing errors. It is one of the most reliable and commonly used tools for pediatric resuscitations.9–12 Unfortunately, this approach does not eliminate dosing errors as clinicians must still determine the volumes of medications from ampoules in order to deliver the correct dose. Translation of medications from the Broselow Tape has been proposed; yet to our knowledge, no one has attempted to develop color-coded, prefilled syringes that could be used in conjunction with the Broselow Tape to facilitate timely and accurate drug administration in the prehospital environment.13
The objective of this study was to compare novel, prefilled medication syringes labeled with color-coded volumes corresponding to the weight-based dosing of the Broselow Tape to conventional methods of drug administration in simulated prehospital pediatric resuscitations. We hypothesized that time of preparation to administration of drugs would be shorter, and the proportion of dosing errors would be lower when using prefilled, color-coded syringes (intervention) when compared to conventional medication preparations (control).
2. Methods
2.1. Study design
We performed a prospective, block-randomized, cross-over study with data collected during two standardized simulated pediatric cardiac arrest scenarios on May 17, 2011 and repeated on June 16, 2011 (Fig. 1). The prehospital environment was recreated by conducting simulations in situ, or inside working, off duty ambulances, with the same medication kits used in the field. Consistent with standard practice, we provided two fire-fighter/emergency medical technicians to assist with resuscitation by performing chest compressions and bag-valve-mask ventilations at the direction of the paramedic. Pediatric cardiac arrest scenarios were developed and face validity was assessed by a panel of experts in pediatric emergency medicine, prehospital emergency care and further adapted to local protocols and paramedic scope of practice. Scenarios were piloted and refined prior to implementation (Appendix A). For purposes of prehospital resuscitation, epinephrine and atropine were developed as color-coded syringes for use in this study (Fig. 2).
Fig. 1.
Study design schematic.
Fig. 2.
Color-coded, prefilled syringes.
Prior to beginning simulations, each participant was instructed to manage the scenario, treat with medications as they would in normal practice using the Broselow Tape for determining dosages and verbalize their medication orders. Before the experimental method scenarios, subjects received a 3-min training (i.e., pre-recorded video instruction and hands-on use) of the prefilled, color-coded syringes. Specific training was not given prior to conventional medication administration scenarios to reflect current practice. A scenario moderator read details of the case presentation to the study subject prior to entering the patient care compartment of the ambulance.
On the first day, each participant was randomly assigned by a study investigator (ADS) using a fair coin to a scenario involving a simulated patient 8 years of age and using their standard medication kit or a simulated patient 8 months of age and using the same kit but with prefilled, color-coded medication syringes in place of conventional ampoules. Each subject then participated in the other scenario following a 10 min intermission. During simulations, moderators made written notations without interference in simulation dynamics.
Upon completion of both scenarios, each subject completed a closed-response survey. Subjects provided demographics, rated adequacy of training with the Broselow Tape, standard medication kits and prefilled, color-coded syringes, ease of use of both medication delivery systems, perceived scenario difficulty, confidence inaccuracy of using prefilled, color-coded syringes, and whether they believed prefilled, color-coded syringes would be a safer alternative to dose calculation during resuscitations (Appendix B). Subjects returned four weeks later repeating the scenarios in reverse order utilizing the opposite medication delivery system for each scenario and completed an identical survey.
2.2. Selection of participants
This study was performed at Denver Health Medical Center in Denver, CO, USA and study participants were recruited from the Denver Health Paramedic Division: an urban advanced life support agency for the City and County of Denver. Paramedics respond to approximately 90,000 9-1-1 calls annually (4500 involving patients <15 years of age) and transport approximately 50,000 individuals (2900 involving patients <15 years of age) to area hospitals. Among these, paramedics attempt resuscitation on approximately 350 adult and 15 pediatric out-of-hospital cardiac arrests. An email was sent to all 270 paramedics inviting them to participate in this study and a convenience sample was used. Subjects were blinded to study purpose during recruitment to minimize preparation bias. However, subjects were unblinded to study objectives during con-sent and when introduced to the prefilled, color-coded syringe just prior to the simulations.
Participation was completely voluntary and subjects were compensated for their time. The study was approved by the Colorado Multiple Institutional Review Board and written informed consent was obtained from all subjects prior to participation.
2.3. Measurements
Video recordings were used to capture medication choice, volume delivered and elapsed time. We used the BabySIM® and PediaSIM® simulation manikins and two digital audio/video recorders, one focused on the IV port and mounted directly above the manikin (215 PTZ with 12× optical, 4× digital zoom [Axis Communications, Lund, Sweden]) and another mounted in the ambulance’s corner (212 PTZ with 3× zoom [Axis Communications, Lund, Sweden]) to capture activity overview. METIVision (CAE Healthcare, Saint-Laurent, Quebec, Canada), a fully integrated, digital audio/visual management system captured and stored simulation data.
Video review was conducted by eight research assistants blinded to study goals and were divided into four, two-person groups. Each pair was assigned a set of videos to independently abstract either dose or timing data, for either the control or the intervention system. Groups were trained separately by a study investigator to apply a standardized approach to reviewing videos to maximize valid and reliable data collection. A study investigator served to adjudicate all disagreements.
2.4. Outcomes
The primary outcome was elapsed time (seconds) from initiation of medication preparation to completed administration. Only active preparation times of medication and actions involving delivery of medication were summed for each elapsed time interval. Pauses for assessments, spontaneous questions to the simulation moderator, or inactivity between rounds of medications were not included in elapsed times. Secondary outcomes were “dosing errors” and “critical dosing errors” based upon doses published on the Broselow Tape.
2.5. Data management and statistical analyses
Data were manually collected by trained research assistants and entered into an electronic spreadsheet (Microsoft Excel, Microsoft Corporation, Redmond, WA) by a study investigator. Data were then transferred into native SAS format (dfPower DBMS Copy, DataFlux Corporation, Cary, NC) and analyses performed using SAS Version 9.3, SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC) or Stata Version 12 (Stata Corporation, College Station, TX).
Medians with interquartile ranges (IQRs) were calculated for all continuous data and percentages with 95% confidence intervals (CIs) for all categorical data. Consistent with institutional policy and previously used standards, doses deviating more or less than 10% from the published Broselow Tape dose were considered “dosing errors”.7, 14, 15 As a Broselow Tape dose is indicated for a range of weights within each color zone, a non-critical dosing error range was calculated by applying the milligram/kilogram dose (based upon the median weight and the published medication dose for each Broselow Tape color zone) to the lightest and heaviest weights inclusive to that zone. For example, the published epinephrine dose for a child in the “red zone, 8–9 kg” is 0.085 mg with a median weight of 8.5 kg producing a 0.01 mg/kg dose. The weights inclusive of the red zone were considered to be 7.51–9.49 kg, thus indicating an acceptable range of doses to be within 0.0751 mg to 0.0949 mg (Appendix C). Applying the more or less than 10% deviation criteria to that range, doses administered <90% of the minimum dose or >110% of the maximum dose were designated “critical dosing errors.” Using the example, epinephrine doses given <90% of 0.0751 mg or >110% of 0.0949 mg were designated “critical dosing errors” for a child in the red zone.
The Wilcoxon signed rank test was used to compare paired median values, and the Wilcoxon rank sum test to compare independent median values. Nonparametric point estimates and 95% CIs were estimated using the centile and cendif functions in Stata for paired and independent comparisons, respectively. Calculation of median differences using these methods may differ slightly from the value obtained from simple subtraction of group medians. No adjustments were made for multiple comparisons but variance estimates were adjusted for clustering at the level of the paramedic. Unless stated otherwise, the unit of analysis was medication dose.
2.6. Sample size
Using medication dose as the unit of analysis, we used a two-sided alpha of 0.05, accounted for clustering effects at the level of the participant and scenario, and incorporated an adjustment for non-normality for the distributions of data when determining the number of required participants. Ultimately, we estimated requiring 10 participants, 40 simulated scenarios, and approximately 120 medication doses administered to obtain a power of 95% to identify a mean difference of 15 s (standard deviation = 10 s) in administration time between control and intervention methods. Although no published data supports a clinically meaningful minimum difference in administration of resuscitation medications, we believed a difference of 15 s might be clinically meaningful, especially in a cardiac arrest scenario.
3. Results
Ten paramedic participants completed both study days. Median age of participants was 31 (IQR: 28–37) years and 8 (80%) had between 6 and 15 years of experience. 132 doses of medications were administered, 69 (52%) using the conventional delivery method and 63 (48%) using the prefilled, color-coded syringe method. Two doses of naloxone were given during scenarios using the conventional method but were excluded from analyses as matching color-coded syringes were not created for this study. During video review of the intravenous port, 5 (7%) and 4 (5%) doses, respectively, were unconfirmed due to an obstructed view and also excluded from analyses. Thus, 121 total doses (62 using the conventional method and 59 using the prefilled, color-coded syringe method) of epinephrine and atropine were included in the analyses (Fig. 3).
Fig. 3.
Medication doses administered, stratified by study arm and outcomes.
Comparative timing data were available only for the arrest simulation of the 8 year old. At the completion of the first day, it was discovered that the overview video feed of the scenario involving the 8 month old had not recorded. Video confirmed data for 29 doses using the conventional method and 29 doses for the prefilled, color-coded syringe method. Median elapsed time for preparation to delivery of all doses for the control and intervention was 42 (95% CI: 36–51) seconds and 34 (95% CI: 28–39) seconds, respectively (difference = 9 [95% CI: 4–14] seconds).
Using the conventional method, 8 of 10 (80%) participants made one or more critical dosing errors and 7 of 10 (70%) made one or more dosing errors (Fig. 4a). Of the 62 doses administered, 33 (53%,95% CI: 27–80%) resulted in dosing errors, with 24 (39%, 95% CI:15–63%) classified as critical dosing errors (Table 1). 8 critical over-doses and 3 critical under-doses occurred during management of the simulated 8 month old, and 6 critical over-doses and 7 critical under-doses occurred during management of the simulated 8 year old (Fig. 5a).
Fig. 4.
Panel A. Dosing errors by participant using the conventional method (N = 62 total doses). Panel B. Dosing errors by participant using the color-coded, prefilled method (N = 59 total doses).
Table 1.
Frequency of errors among paramedics using conventional syringes versus color-coded syringes.
| Conventional syringe |
Color-coded syringe |
Absolute difference (95% CI) | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Total number of doses given | 62 | 59 | ||||
| Number of dosing errorsa | 33 | 53 | 5 | 8 | 45 | 15–75 |
| Number of doses outside of the Broselow range | 31 | 50 | 4 | 7 | 43 | 16–71 |
| Number of critical dosing errorsb | 24 | 39 | 0 | 0 | 39 | 13–61c |
Abbreviations: CI = confidence interval.
An incorrect dose was defined by a dose that was greater than or less than 10% the published Broselow Tape dose.
Critical dosing error was defined by a mg/kg dose <10% for the published lower weight range of >10% for the published upper weight range within a color zone.
95% CI was estimated by adding 1 to the 0 column because the asymptotic 95% CI could not be calculated with a 0 value while accounting for clustering at the paramedic level.
Fig. 5.
Panel A. Percent error by participant and drug administered using the conventional syringe method. Panel B. Percent error by participant and drug administered using the color-coded syringe method.
Using the prefilled, color-coded syringe method, 0 of the 10 (0%) participants made a critical dosing error, while 3 of 10 (30%) made at least one dosing error (Fig. 4b). Of the 59 doses administered, 5 (8%, 95% CI: 0–20%) resulted in dosing errors with 0 (0%, 95% CI:0–6%) classified as critical dosing errors (Table 1 and Fig. 5b).
Participants rated the difficulty of each scenario similarly. On a five-point Likert scale where 1 defined “very difficult” and 5 defined “very easy”, the median values for the 8 year-old scenario were 4 (IQR: 3–5) for color-coded and 3 (IQR: 2–4) for conventional syringe methods. For the 8 month-old scenario, the median values were 3.5 (IQR: 2–4) for the color-coded and 4 (IQR: 3–4) for the conventional syringe methods. Median estimates of training adequacy of the Broselow Tape System was 3 (IQR: 3–3), color-coded syringe was 3.5 (IQR: 3–4), and standard syringe was 4 (IQR:3.5–4), where 1 represented “poor – I need more training” and 4 represented “confident – I understand it completely”. Comparing ease of use between the color-coded and conventional syringe systems resulted in median ratings of 5 (IQR: 4–5) and 4 (IQR: 3–4) (p < 0.001), respectively. Of the 10 participants, 9 (90%) indicated the prefilled, color-coded syringe would increase their confidence in accurately dosing a pediatric patient and would be a safer alter-native to dose calculation when compared to standard syringe methods.
4. Discussion
Conducted in a prehospital setting, this study shows the use of a novel prefilled, color-coded syringe system reduces time required to prepare and deliver medications, reduces overall dosing errors, and eliminates critical dosing errors during simulated pediatric resuscitations by eliminating calculation as part of the cognitive process, utilizes pediatric specific volume preparations, and employs color designations identifying correct medication volumes. To our knowledge, this is the first study with paramedics to demonstrate the effectiveness of this type of medication administration system and provides evidence for the development of a comparable Broselow Tape-based syringe system for use by pre-hospital emergency care personnel during pediatric resuscitations.
There is an abundance of evidence reporting rates and types of medication errors in the hospital setting, but a relative paucity of direct evidence of medication errors in the pre-hospital environment.16 Data published on the incidence of clinical error is limited to retrospective chart reviews and self-reporting methodology, but reveals paramedics commit dosing errors 49–63% of the time with miscalculation as a primary cause.4, 17–21 Simulation data also confirms medication dosing errors are common among currently practicing paramedics with calculation errors again identified as a major cause.15, 22–24 Deficiencies in mathematics and application of mathematical principles have been investigated in students and currently practicing paramedics. Without aids, cross-sectional examination in classroom settings reveals errors occur in one third to one half of all medication calculations.25–28 The combination of clinical, simulation and classrooom research suggests the occurrence of medication dosing errors in the prehospital environment is greatly underestimated, unrecognized, and poses an implicit safety risk to pediatric patients.
While implementation of Broselow color-coded systems in pediatric care settings reduces calculation burden and decreases medication dosing errors, they still occur; and, can lead to a clinically significant adverse event.13, 25–28 In our study, all doses were predetermined by the use of the Broselow Tape; thus, only a single calculation was required using current practice to determine the correct volume required for delivering the indicated dose. The prefilled, color-coded syringe method removes that calculation altogether and its use was associated with elimination of critical dosing errors.
Without regular practice and familiarity with small doses – and corresponding small volumes – utilized for pediatric patients, a dosing error during a pediatric emergency may go unrecognized even by a seasoned provider. In our study, two subjects administered multiple 10-fold overdoses using standard practice. 61 (98%) of the 62 control doses were given directly from the medication ampoule containing an adult dose. Only one subject utilized a stopcock and smaller syringe to prepare a single dose of medication (given at the correct dose); yet afterwards, gave the rest of medications directly from the ampoules as well. While timing data reveals this practice is comparable in time to delivery compared to the intervention, this practice likely contributed to inaccuracy resulting in the high rate of critical dosing errors observed. The prefilled, color-coded syringe system contains only the highest pediatric dose; and with traditional volume graduations replaced by color-coded volume markings on the syringe, dose (via volume) accuracy is visually distinct.
The 2009 National Hospital Ambulatory Care Survey reported that only 5.3% of the 28.3 million patients who were age fifteen years or younger were transported to the ED by ambulance.29 As a majority of transports to EDs are non-emergent, presumably only a small fraction of that 5.3% was actually critically ill. This study’s cohort was recruited from a high volume, urban ALS trans-port agency. In doing so, we aimed to sample paramedics with the most opportunities possible for exposure to pediatric emergencies and use of the conventional medication system in place. The study results suggest even the busiest paramedics may never have sufficiently frequent exposure to critically ill children to be consistently proficient in calculating and preparing the variable doses indicated by weight-based protocols.
This study has several potential limitations. We recognize the data lost the first day as a result of recording failure may have affected the power of timing results; however, the significant reduction in the severity and frequency of dosing errors seen with the pre-filled, color-coded syringes may have a more meaningful impact on prehospital care than further shortening of time to medication delivery. As a concept, prefilled syringes have been shown to decrease time to medication administration and dosing error.30 To our knowledge, prefilled, color-coded syringes specific for individual medications are not yet commercially manufactured with standardized pediatric volumes, and have not been evaluated in pediatric resuscitations. As such, results of this simulation study may not translate to actual patient care. The study cohort included actively practicing paramedics, using the same medication kits containing the conventional medication delivery system used in their clinical practices; thus, satisfactory training and familiarity with it was presumed. It is possible the proximity of the brief color-coded syringe method training to the utilization of it within the scenario biased timing results toward improved performance with the intervention. However, this was necessary to provide sub-jects with minimum level of familiarity with the new system in order to use it. Misclassification bias may have been introduced during data extraction from video clips. To minimize such bias, research assistants were trained and worked independently, and a study investigator only served to adjudicate any discrepancies or disagreements at the time of data entry. Finally, this study was performed in one setting using paramedics from a single emergency medical services system, and therefore may not generalize to other settings or paramedics. We believe, however, that standardization of medication syringes will inherently reduce time to medication administration and dosing errors regardless of the setting.
5. Conclusions
In summary, a novel color-coded prefilled syringe decreased time to medication administration and significantly reduced critical dosing errors by paramedics during simulated prehospital pediatric resuscitations. Implementing standardized, mechanically and visually simple systems that eliminate calculations during prehospital management of pediatric emergencies may facilitate appropriate patient care and contribute to improved outcomes.
Supplementary Material
Acknowledgments
We would like to thank Christine Black, Mark Brownson, Claire Chappell, Amy Dear-Ruel, Melissa O’Meara, Ramya Mishra, Adam Plate, and Ashley Phipps for their participation as research assistants; Kevin Kaucher, PharmD for development of study materials including medication vials; Comilla Sasson, MD, MS, PhD for her suggestions related to the manuscript; and the EMTs and firefighters who assisted as scenario team members, and the paramedics who participated as study subjects.
Funding
This study was funded by an unrestricted grant from the COPIC Medical Foundation, Denver, CO. The COPIC Medical Foundation had no role in the design, conduct, or reporting of this study. Dr. Haukoos was supported, in part, by an Independent Scientist Award (K02HS017526) from the Agency for Healthcare Research and Quality and an Investigator-Initiated Grant (R01AI106057) from the National Institutes of Health. No other authors were directly or indirectly supported by funding during this study. Dr. Hernandez holds a pending patent for the color-coded, prefilled syringes used in this study but has not marketed or received payment for them. None of the other authors have financial interest in the color-coded-prefilled syringes.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resuscitation.2015.07.035
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2015.07.035.
Presented, in part, at the American Heart Association Resuscitation Science Symposium, Los Angeles, CA, November 4, 2012.
Authors’ contributions
Mr. Stevens and Dr. Haukoos had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses. Color-coded syringe design: Hernandez. Study concept: Hernandez, Haukoos. Study design: Stevens, Hernandez, Jones, Blumen, Moreira, Hopkins,Sande, Bakes, Haukoos. Acquisition of data: Stevens, Hernandez, Jones, Blumen, Sande. Statistical analyses: Stevens, Hopkins, Haukoos. Interpretation of results: Stevens, Hernandez, Moreira, Hopkins, Haukoos. Drafting of the manuscript: Stevens, Haukoos. Critical revision of the manuscript for important intellectual con-tent: Stevens, Hernandez, Jones, Blumen, Moreira, Hopkins, Sande, Bakes, Haukoos. Obtained funding: Hernandez. Administrative, technical, or material support: Stevens, Jones, Blumen, Hopkins, Haukoos. Study supervision: Haukoos.
References
- 1.Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–1903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- 2.Doherty C, Mc Donnell C. Tenfold medication errors: 5 years’ experience at a university-affiliated pediatric hospital. Pediatrics. 2012;129:916–924. doi: 10.1542/peds.2011-2526. [DOI] [PubMed] [Google Scholar]
- 3.Ghaleb MA, Barber N, Franklin BD, Wong IC. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child. 2010;95:113–118. doi: 10.1136/adc.2009.158485. [DOI] [PubMed] [Google Scholar]
- 4.Hoyle JD, Davis AT, Putman KK, Trytko JA, Fales WD. Medication dosing errors in pediatric patients treated by emergency medical services. Prehosp Emerg Care. 2012;16:59–66. doi: 10.3109/10903127.2011.614043. [DOI] [PubMed] [Google Scholar]
- 5.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 6.Maidment ID, Lelliott P, Paton C. Medication errors in mental healthcare: a systematic review. Qual Saf Health Care. 2006;15:409–413. doi: 10.1136/qshc.2006.018267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcin JP, Dharmar M, Cho M, et al. Medication errors among acutely ill and injured children treated in rural emergency departments. Ann Emerg Med. 2007;50:361–367. 367.e1–367.e2. doi: 10.1016/j.annemergmed.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.To Err is Human: Building a Safer Health System. Institute of Medicine; 1999,2012. [Google Scholar]
- 9.Krieser D, Nguyen K, Kerr D, Jolley D, Clooney M, Kelly AM. Parental weight estimation of their child’s weight is more accurate than other weight estimation methods for determining children’s weight in an emergency department? Emerg Med J. 2007;24:756–759. doi: 10.1136/emj.2007.047993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubitz DS, Seidel JS, Chameides L, Luten RC, Zaritsky AL, Campbell FW. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann Emerg Med. 1988;17:576–581. doi: 10.1016/s0196-0644(88)80396-2. [DOI] [PubMed] [Google Scholar]
- 11.Luten RC, Zaritsky A, Wears R, Broselow J. The use of the Broselow tape in pediatric resuscitation. Acad Emerg Med. 2007;14:500–501. doi: 10.1197/j.aem.2007.02.015. author reply 1–2. [DOI] [PubMed] [Google Scholar]
- 12.So TY, Farrington E, Absher RK. Evaluation of the accuracy of different methods used to estimate weights in the pediatric population. Pediatrics. 2009;123:e1045–e1051. doi: 10.1542/peds.2008-1968. [DOI] [PubMed] [Google Scholar]
- 13.Luten R. Error and time delay in pediatric trauma resuscitation: addressing the problem with color-coded resuscitation aids. Surg Clin N Am. 2002;82:303–314. vi. doi: 10.1016/s0039-6109(02)00007-5. [DOI] [PubMed] [Google Scholar]
- 14.McPhillips HA, Stille CJ, Smith D, et al. Potential medication dosing errors in outpatient pediatrics. J Pediatr. 2005;147:761–767. doi: 10.1016/j.jpeds.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 15.Lammers R, Byrwa M, Fales W. Root causes of errors in a simulated prehospital pediatric emergency. Acad Emerg Med. 2012;19:37–47. doi: 10.1111/j.1553-2712.2011.01252.x. [DOI] [PubMed] [Google Scholar]
- 16.O’Connor RE, Slovis CM, Hunt RC, Pirrallo RG, Sayre MR. Eliminating errors in emergency medical services: realities and recommendations. Prehosp Emerg Care. 2002;6:107–113. doi: 10.1080/10903120290938913. [DOI] [PubMed] [Google Scholar]
- 17.Hobgood C, Xie J, Weiner B, Hooker J. Error identification, disclosure, and reporting: practice patterns of three emergency medicine provider types. Acad Emerg Med. 2004;11:196–199. [PubMed] [Google Scholar]
- 18.Cushman JT, Fairbanks RJ, O’Gara KG, et al. Ambulance personnel perceptions of near misses and adverse events in pediatric patients. Prehosp Emerg Care. 2010;14:477–484. doi: 10.3109/10903127.2010.497901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hobgood C, Bowen JB, Brice JH, Overby B, Tamayo-Sarver JH. Do EMS. personnel identify, report, and disclose medical errors? Prehosp Emerg Care. 2006;10:21–27. doi: 10.1080/10903120500366011. [DOI] [PubMed] [Google Scholar]
- 20.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehosp Emerg Care. 2006;10:457–462. doi: 10.1080/10903120600885100. [DOI] [PubMed] [Google Scholar]
- 21.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehosp Emerg Care. 2007;11:80–84. doi: 10.1080/10903120601021358. [DOI] [PubMed] [Google Scholar]
- 22.Lammers RL, Byrwa MJ, Fales WD, Hale RA. Simulation-based assessment of paramedic pediatric resuscitation skills. Prehosp Emerg Care. 2009;13:345–356. doi: 10.1080/10903120802706161. [DOI] [PubMed] [Google Scholar]
- 23.LeBlanc VR, MacDonald RD, McArthur B, King K, Lepine T. Paramedic performance in calculating drug dosages following stressful scenarios in a human patient simulator. Prehosp Emerg Care. 2005;9:439–444. doi: 10.1080/10903120500255255. [DOI] [PubMed] [Google Scholar]
- 24.Leblanc VR, Regehr C, Tavares W, Scott AK, Macdonald R, King K. The impact of stress on paramedic performance during simulated critical events. Prehosp Disaster Med. 2012;27:369–374. doi: 10.1017/S1049023X12001021. [DOI] [PubMed] [Google Scholar]
- 25.Bernius M, Thibodeau B, Jones A, Clothier B, Witting M. Prevention of pediatric drug calculation errors by prehospital care providers. Prehosp Emerg Care. 2008;12:486–494. doi: 10.1080/10903120802290752. [DOI] [PubMed] [Google Scholar]
- 26.Eastwood K, Boyle MJ, Williams B. Mathematical and drug calculation abilities of paramedic students. Emerg Med J. 2012;30:241–242. doi: 10.1136/emermed-2011-200929. [DOI] [PubMed] [Google Scholar]
- 27.Eastwood KJ, Boyle MJ, Williams B. Paramedics’ ability to perform drug calculations. West J Emerg Med. 2009;10:240–243. [PMC free article] [PubMed] [Google Scholar]
- 28.Hubble MW, Paschal KR, Sanders TA. Medication calculation skills of practicing paramedics. Prehosp Emerg Care. 2000;4:253–260. doi: 10.1080/10903120090941290. [DOI] [PubMed] [Google Scholar]
- 29.National Hospital Ambulatory Medical Care Survey, Emergency Department Survey. National Center for Health Statistics; 2009. [Google Scholar]
- 30.Adapa RM, Mani V, Murray LJ, et al. Errors during the preparation of drug infusions: a randomized controlled trial. Br J Anaesth. 2012;109:729–734. doi: 10.1093/bja/aes257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.