Abstract
Objective
Reintervention rates are higher for endovascular aneurysm repair (EVAR) compared with open repair (OR) mostly due to treatment for endoleaks, while open surgical operations for bowel obstruction and abdominal hernias are higher following OR. However, readmission rates for non-operative conditions and complications that do not require an intervention following either EVAR or OR are not well documented. We sought to determine reasons for all-cause readmissions within the first year following open AAA repair and EVAR.
Methods
Patients who underwent elective AAA repair in California over a six-year period were identified from the Health Care and Utilization Project (HCUP) State Inpatient Database (SID). All patients who had a readmission in the state of California within one year of their index procedure were included for evaluation. Readmission rates as well as primary and secondary diagnoses associated with each readmission were analyzed and recorded.
Results
From 2003-2008, there were 15,736 operations for elective aneurysm repair, 9,356 EVARs (60%) and 6,380 open repairs (40%). Postoperatively, there was a 52.1% readmission rate after OR and a 55.4% readmission rate following EVAR at one year (p=0.0003). The three most common principle diagnoses associated with readmission after any type of AAA repair were failure to thrive, cardiac issues, and infection. When stratified by repair type, patients who underwent open repair were more likely to be readmitted with primary diagnoses associated with failure to thrive (p<0.0001), cardiac complications (p= NS), and infection (p= NS) compared to EVAR. Those who underwent EVAR were more likely, however, to be readmitted with primary diagnoses of device-related complications (p=0.05), cardiac complications, and infection.
Conclusion
Total readmission rates within one year of elective AAA repair are greater following EVAR than with open repair. Reasons for readmission vary between the two cohorts, but are related to the magnitude of open surgery following OR, device issues after EVAR, and the usual cardiac and infectious complications following either. Systems-based analysis of these causes of readmission can potentially improve patient expectations and care following elective aneurysm repair.
INTRODUCTION
Since it was first described in 1991, endovascular aneurysm repair (EVAR) has become the preferred method of treatment for patients with abdominal aortic aneurysms (AAA).1 Early studies have documented well improvement in operative mortality and initial complication rates following EVAR.2 However, longer-term followup has suggested that the early benefit of EVAR might be lost several years after surgery.3 The reasons for the convergence of success rates are multifactorial, and often related to the high number of secondary interventions in the EVAR cohort. Second interventions are reported to be as high as 20% and have an increased morbidity and mortality in patients requiring them.4 What remains challenging to track, however, and perhaps the reason for the scarcity of literature related to are non-operative readmissions. The importance of understanding all-cause readmissions, particularly non-operative causes, is highlighted in other surgical procedures where they increase the risk of future complications and subsequent mortality up to 11%.5
The purpose of this study was to use a statewide database to evaluate the incidence of all post-operative readmissions within one year following elective AAA repair in the state of California. The differences in these readmission rates between EVAR and open repair were compared, as well as the actual causes and diagnoses of readmissions between the two cohorts. Predictive demographic factors associated with readmission within one year of an elective AAA repair were examined to better understand systems-based issues surrounding readmission.
METHODS
The State Inpatient Database (SID) developed as part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality, identified adults who underwent open repair or endovascular repair of infrarenal AAA between 2003 and 2008. Patients were identified using International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes for intact AAA (441.4, 441.9). For the purpose of this study, we excluded patients identified with ICD-9 codes for ruptured AAA (441.3, 441.5). Extremes of age were also considered likely outliers, so inclusion criteria for this study was limited to those between 40-90. Patients were then subdivided according to International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes, 38.44 for open repair and 39.71 for endovascular repair. All patients at risk for one-year readmission following elective AAA repair were included in this study.
The SID contains a range of data collected from discharge inpatient hospital records including demographics, ICD-9-CM codes for primary and secondary diagnoses and procedures, admission source, length of stay, discharge disposition, inpatient mortality, and hospital characteristics. This database also allows for identification of patient readmissions within one full year in the state of CA. It attempts to capture patient data characteristics from the readmission, including primary and secondary diagnoses. Multiple readmissions from the same patient within one year counted toward the total number of readmissions for that cohort.
For purposes of analysis, patient race was categorized as white or non-white. Patients’ primary expected payer was categorized as private, Medicare, Medicaid, or other. Comorbidity illnesses present on the index admission were summarized using the Charlson Index, which considers co-morbid conditions as predictors of ten-year mortality. To perform a longitudinal analysis, unique patient identifiers were used to determine whether a single patient had a subsequent hospital admission within the subsequent year. Patient identifiers were not consistent across years and therefore prevented analysis of patients across multiple years.
Because multiple types of codes exist for all types of readmissions, and to create more broad categories of reasons for readmission, we arbitrarily divided principle and secondary diagnoses into systems-based problems, and included several different conditions under one larger medical diagnosis (Table 1). For instance, readmission diagnoses documented as pneumonia organism not otherwise specified (NOS) (486), respiratory failure (51881), obstructive chronic bronchitis with active exacerbation (49121), food/vomit pneumonitis (5070), post-traumatic pulmonary insufficiency (5185) and surgical complication: respiratory system (9972) were combined to create “pulmonary” classification for reason for readmission.
Table 1.
Specific ICD-9 diagnostic codes used to categorize readmission causes into groups of system-based criteria.
| Failure to thrive | V5789 | Rehabilitation procedure nec | DVT/PE | 4538 | Venous thrombosis nec | Distal embolization | 44422 | Lower extremity embolism |
| V5873 | Aftercare following surgery/circulatory system-nec | 41519 | Other pulmonary embolism, infarct | Device/Aneurysm-related | 4414 | Abdominal aortic aneurysm | ||
| V571 | Physical therapy nec | Pulmonary | 486 | Pneumonia-organism NOS | 99674 | Complication other vascular device/graft | ||
| V5849 | Other postoperative aftercare | 51881 | Respiratory failure | 99662 | React- other vascular device/graft | |||
| 2765 | Hypovolemia | 49121 | Obstructive chronic bronchitis with active exacerbation | 9972 | Surgical complication peri vascular system | |||
| 27651 | Dehydration | 5070 | Food/vomit pneumonitis | |||||
| Cardiac | 4280 | Congestive heart failure | 5185 | Post traumatic pulmonary insufficiency | ||||
| 41401 | Coronary atherosclerosis native vessel | 9972 | Surgical complication: respiratory system | |||||
| 41071 | Subendothelial infarct: initial | GI | 9974 | Surgical complication: GI tract | ||||
| 42731 | Atrial fibrillation | 5770 | Acute pancreatitis | |||||
| 78659 | Chest pain nec | 00845 | Clostridium difficile infection | |||||
| 42781 | Sinoatrial node dysfunction | SBO | 56081 | Intestinal adhesion with obstruction | ||||
| 78650 | Chest pain NOS | 5609 | Intestinal obstruction NOS | |||||
| Infection | 99859 | Other postoperative infection | Renal | 5849 | Acute renal failure NOS | |||
| 0389 | Septicemia NOS | CVA | 43491 | Cerebral arterial occlusion NOS with infarction | ||||
| 5990 | Urinary tract infection NOS | Wound | 55321 | Incisional hernia | ||||
| 03811 | Staph aureus septicemia | 99813 | Seroma procedure culture | |||||
| 99831 | Disruption of internal operative wound |
We analyzed the 41 most frequent diagnoses and included these in follow-up evaluation. This captured over 95% of the patients with readmissions, and clear outliers, those diagnoses that were clearly unrelated to a patient's aneurysm repair, were excluded. These were infrequent and were almost exclusively related to malignancies.
Statistical Analysis
Both SAS (version 9.2) and Stata (version 11) software were used for statistical analyses. Chi-square analysis and t-test were used to compare outcome variables as appropriate. Overall readmission rates were estimated using Kaplan-Meier analysis. Comparison of these estimates by surgical type was performed using the log-rank test. A modified Cox proportional hazards modeling with adjustment for patient and hospital characteristics was used to adjust for patient mix on readmission rates between the two surgical procedures. Patient characteristics included age, gender, race, insurance status, obesity, complicated diabetes mellitus (DM), complicated hypertension (HTN), peripheral vascular disease, (PVD), chronic obstructive pulmonary disease (COPD), and end stage renal disease (ESRD).
RESULTS
Between 2003 and 2008, there were 17,749 AAAs treated in the state of CA. 1,648 (9.2%) ruptured AAAs were excluded from this analysis. This left 16,101 elective AAA repairs performed over this period. 365 patients were further excluded for various reasons, including extremes of age, incomplete or omitted data, or inconsistent information from the subsequent follow-up period. The remaining 15,736 patients had elective AAA repairs performed during the study period. 9,356 (59.5%) of these patients had an EVAR while 6,380 (40.5%) had an open repair.
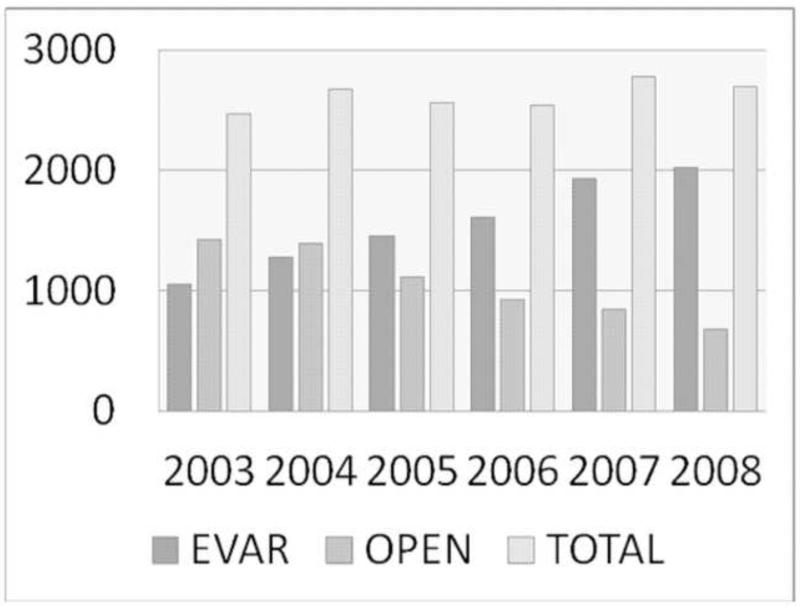
Analysis of the annual trends between EVAR and open repair revealed an increase in the total number of elective aneurysm repairs performed from 2003-2008 (Figure 1). In 2003, 2,475 elective AAA repairs were performed. By 2008, this number had increased to 2,701. There existed a gradual but consistent increase in the number of EVARs performed (1,052 in 2003 to 2,023 in 2008) and a corresponding decrease in the number of elective open repairs performed (1,423 to 678).
Figure 1.
Over the course of the study period (2003-2008), the number of total aneurysms repaired in the State of California has remained relatively constant. Endovascular repair (EVAR) has, however, replaced OPEN repair as the treatment method of choice.
The baseline demographics between the two populations were heterogeneous (Table 2). The mean age of patients undergoing EVAR was 75 years, compared with open repair, which was 72 years (p<0.0001). There was also a larger percentage of male patients in the EVAR group compared with the open repair group (84.7% vs. 75.6%, p<0.0001). Patients who had an EVAR were more likely to have complicated DM, while patients having an open repair were more likely to have complicated HTN, COPD, and have private insurance compared with Medicaid or Medicare. Patients undergoing an open repair had a higher Charlson Index score and more likely to have a score greater than or equal to 2 (55.52% for open repair vs. 51.73% for EVAR, P<0.0001). There was no difference between the two groups with respect to race, obesity, PVD, or ESRD.
Table 2.
Comparison of baseline demographics and comorbidities of all patients in the State of California undergoing aneurysm repair from 2003-2008.
| EVAR | OR | p-value | |
|---|---|---|---|
| Age (y) | 75 | 72 | <0.0001 |
| Male Gender (%) | 84.7 | 75.6 | <0.0001 |
| White Race (%) | 81.1 | 81.5 | NS |
| Private Insurance (%) | 15.3 | 20.8 | <0.0001 |
| Charlson Index ≥ 2 (%) | 51.7 | 55.5 | <0.0001 |
| Obesity (%) | 7.2 | 7.0 | NS |
| CHF | 9.8 | 14.1 | <0.0001 |
| Complicated DM (%) | 1.7 | 1.2 | 0.01 |
| Complicated HTN (%) | 9.0 | 10.9 | 0.0001 |
| PVD (%) | 98.8 | 98.5 | NS |
| COPD (%) | 29.2 | 37.7 | <0.0001 |
| ESRD (%) | 8.6 | 9.1 | NS |
Surgical outcomes
The overall operative mortality for all elective AAA repairs in the state of CA during the study period was 3.5%. This was significantly higher following open repair than with EVAR (6.7% vs. 1.4%, P<0.0001). The mean length of stay (LOS) at the surgical hospitalization was also significantly higher following open repair (10.5 days vs. 3.7 days, P<0.0001). Early readmission rates (within 30 days of surgery) also were higher for the open surgery group (20.0% vs. 17.4%, P=0.0003). Patients were more likely to be discharged as a routine disposition (i.e. not to a nursing facility or rehab center) following EVAR (84.3% vs. 57.7%, P <0.0001).
Readmissions
Patients were evaluated for readmissions to an inpatient hospital within one year of their index admission (Table 3). In contrast to early readmission rates, the 90-day readmission rates were only slightly greater following open repair (31.3% vs. 29.7%), but this did reach statistical significance (P=0.046). However, by one year from surgery there was a significantly higher readmission rate following EVAR compared with open repair (55.4% vs. 52.1%, P=0.0003). The mean number of days to the first readmission was significantly longer after EVAR (83 days vs. 57 days, P<0.0001) and the mean length of stay during the first readmission was significantly shorter with EVAR (2 days vs. 8 days, P<0.0001). At one year, the risk adjusted mortality was significantly greater for open repair (7.79% vs. 2.44%, P<0.0001). However, this significance was lost after the hospitalization for the surgical procedure was removed from the analysis. The adjusted mortality at one year excluding the index admission was 1.08% for EVAR and 1.24% for open repair (P=0.37).
Table 3.
Readmission data of patients undergoing endovascular repair or open repair.
| EVAR (%) | OPEN (%) | p-value | |
|---|---|---|---|
| Readmission within 30 days | 17.4 | 20.0 | 0.0003 |
| Readmission within 90 days | 29.7 | 31.3 | 0.046 |
| Readmission within 1 year | 55.4 | 52.1 | 0.0003 |
| Days to readmission | 83 | 57 | <0.0001 |
| LOS at first readmission* | 2 | 8 | <0.0001 |
| 1- year risk adjusted mortality* | 2.44% | 7.79% | <0.0001 |
| Adjusted mortality after index admission | 1.08% | 1.24% | 0.373 |
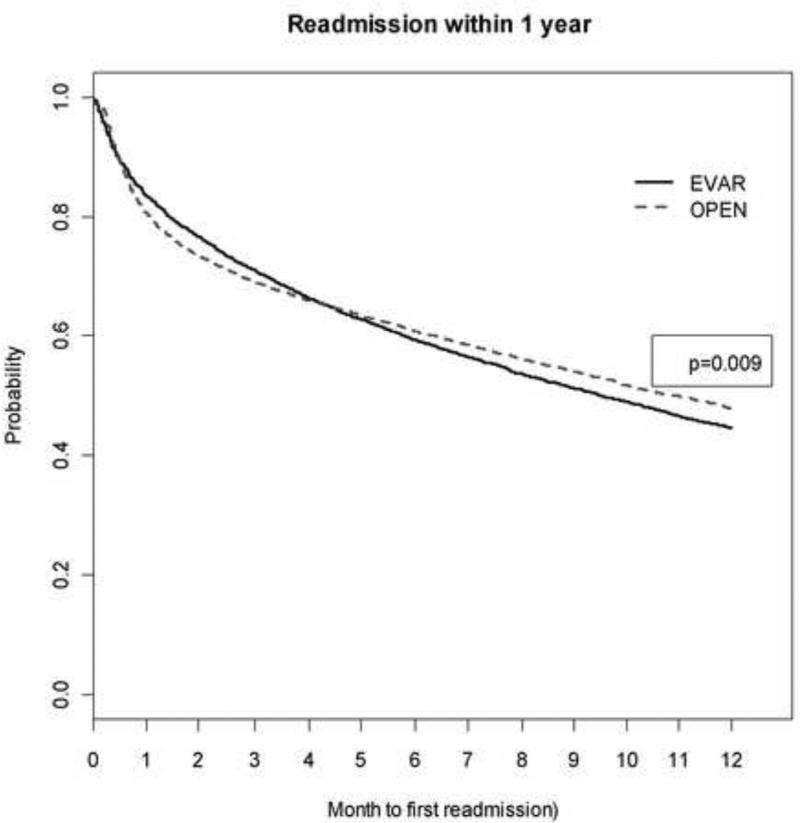
Kaplan-Meier analysis confirmed similar outcomes at one year for the two cohorts (Figure 2). Early in the post-operative period, patients undergoing open repair were more likely to be readmitted to the hospital. This advantage, however, was lost by approximately four months following the procedure. At one year following the surgical procedure, patients who had undergone EVAR were more likely to be readmitted (P=0.009). Diagnoses associated with readmissions were evaluated between the two groups. When all diagnoses were considered, there were a greater number of diagnoses associated with readmissions within one year following open repair (Table 4). Specifically, patients who had open repair were more likely to be readmitted within one year with diagnoses of failure to thrive, cardiac, pulmonary, or gastrointestinal complications, infection, pulmonary embolism/deep venous thrombosis (PE/DVT), and small bowel obstruction (SBO). Patients who underwent elective EVAR were more likely to be readmitted within the first year for device or aneurysm-related complications. They were also slightly more likely to be readmitted with a diagnosis of a wound complication, although this was not statistically significant (P=0.12).
Figure 2.
Kaplan-Meier estimates of freedom from readmission. At one-year followup patients undergoing endovascular repair have a higher likelihood of readmission compared to open repair.
Table 4.
All diagnoses associated with readmission within one year after aneurysm repair.
| EVAR (%) | OPEN (%) | p-value | |
|---|---|---|---|
| Failure to thrive | 19.7 | 28.4 | <0.0001 |
| Cardiac | 34.9 | 39.7 | <0.0001 |
| Infection | 15.7 | 19.2 | 0.0001 |
| Device/aneurysm | 12.6 | 10.4 | 0.0059 |
| Pulmonary | 9.8 | 13.3 | <0.0001 |
| Renal | 8.9 | 9.6 | NS |
| CVA | 1.8 | 1.8 | NS |
| GI | 2.6 | 7.2 | <0.0001 |
| Wound | 5.2 | 4.4 | NS |
| Embolism | 0.9 | 1.0 | NS |
| PE/DVT | 0.4 | 0.9 | 0.006 |
| SBO | 0.3 | 1.4 | <0.0001 |
The primary diagnoses associated with readmission were also evaluated to see if this was different than considering all diagnoses during readmission. Once again the most common primary diagnoses for readmission for both groups were failure to thrive, cardiac complications, and infection (Table 5). The difference was statistically higher in open repair compared with EVAR (11.63% vs. 3.97%, P<0.0001); however, it was not significant in the latter two. Other statistically significant diagnoses associated with readmission following open repair included pulmonary complications (4.9%, P=0.009), gastrointestinal complications (3.8%, P< 0.0001), PE/DVT (0.54%, P=0.03), and SBO (1.1%, P<0.0001). Patients who had an EVAR were more likely to be readmitted with a primary diagnosis of wound complications (2.9%, P=0.02) and device/aneurysm-related complications, although this did not reach statistical significance (5.5%, P=0.055).
Table 5.
Primary diagnosis listed per readmission within one year after aneurysm repair.
| EVAR (%) | OPEN (%) | p-value | |
|---|---|---|---|
| Failure to thrive | 3.97 | 11.63 | <0.0001 |
| Cardiac | 8.61 | 7.81 | NS |
| Infection | 6.84 | 7.09 | NS |
| Device/aneurysm | 5.54 | 4.50 | 0.055 |
| Pulmonary | 3.62 | 4.90 | 0.009 |
| Renal | 1.45 | 1.22 | NS |
| CVA | 1.45 | 1.19 | NS |
| GI | 1.20 | 3.85 | <0.0001 |
| Wound | 2.89 | 1.98 | 0.02 |
| Embolism | 0.25 | 0.22 | NS |
| PE/DVT | 0.22 | 0.54 | 0.03 |
| SBO | 0.22 | 1.12 | <0.0001 |
Cox-regression analysis revealed factors more likely associated with readmission within one year for all patients in the cohort (Table 6). Open repair was a negative predictor for readmission (HR 0.862, CI= 0.804-0.924). Females were more likely to be readmitted, as were older patients and patients with more comorbidities as measured by Charlson Index. Other predictors of readmission within one year included Medicaid insurance, increased LOS at surgery, CHF, and complicated HTN. Peripheral vascular disease conferred a protective advantage against readmission (0.675, CI= 0.536-0.851). Race, DM, and COPD were not associated with an increased risk of readmission within the first year following their surgical procedure.
Table 6.
Predictors of readmission within one year after aneurysm repair.
| Factor | Hazard ratio | LCI | UCI | P-value |
|---|---|---|---|---|
| Open Repair | 0.862 | 0.804 | 0.924 | <0.0001 |
| Female | 1.091 | 1.005 | 1.184 | 0.0066 |
| Age | 1.012 | 1.008 | 1.017 | <0.0001 |
| Charlson Index 2 | 1.358 | 0.913 | 2.022 | 0.0473 |
| Charlson Index 3 | 1.656 | 1.106 | 2.481 | 0.0013 |
| Medicaid | 1.220 | 0.986 | 1.508 | 0.0159 |
| LOS | 1.014 | 1.011 | 1.017 | <0.0001 |
| CHF | 1.324 | 1.205 | 1.455 | <0.0001 |
| HTN | 1.306 | 1.205 | 1.415 | <0.0001 |
| PVD | 0.675 | 0.536 | 0.851 | 0.0009 |
DISCUSSION
Multiple randomized and nonrandomized controlled trials have demonstrated an early morbidity and mortality advantage following EVAR compared with open repair of elective AAA repair.6,7,8 Interestingly, when pooled trial data has been compared for high risk patients this early advantage was not confirmed.9 Similarly, most large studies demonstrated no survival advantage when longer follow-up was performed.2,6 There still remains some doubt in the literature the exact reasons for loss of the survival advantage with longer-term followup, and may simply represent the comorbid cardiovascular factors of many patients undergoing elective aneurysm repair, whether open or EVAR.
Our goal in this study was to use an administrative database to identify all patients in the state of California who underwent elective AAA repair and track their readmissions through the first year. Early mortality outcomes are in agreement with other studies, with operative mortality of 1.4% following EVAR and 6.7% following open repair, comparable to those found in the DREAM trial2 (1.7% and 6%, respectively). Because the patient cohorts in this current study were not homogenous, this likely had an impact on overall patient outcomes, and is an acknowledged issue with administrative databases. We found in the state of California that patients who had EVAR were more likely to be older, male, and less likely to have private insurance. However, patients undergoing open repair were more likely to be sicker with more comorbidities. The mean Charlson Index value for patients with an open repair was significantly higher than EVAR (1.72 vs. 1.67, P<0.0001). Patients with open repair were more likely to have a history of CHF, complicated diabetes mellitus, and complicated hypertension. This selection bias of offering healthier patients EVAR may explain in part the increased early mortality following open repair in the state of California.
Analysis of the readmission data, the focus of this study, highlights some interesting factors about this cohort. First, readmission rates of 55.4% and 52.1% within one year following the two procedures seemed excessive at first glance. While not every one of these subsequent admissions can be directly related to the patients’ aneurysm repairs, it underscores the fact that patients with aneurysmal disease mostly have significant comorbidities and are of the age that return to the hospital at a surprisingly high rate in the first year following their surgery. It is plausible that the true incidence of readmissions is often underreported, albeit a number of them not necessarily as a direct result of the surgical procedure. A patient may present to an outside institution or even to a different service within the same hospital. Often these readmissions will not be viewed as a consequence of the initial procedure, and often goes unbeknownst to the original surgeon. One of the strengths of the particular database used in this study is it captures readmissions within the entire state, so much less likely to underestimate true readmission rates.
Obviously, when combining readmission diagnoses, the current data suggests that a significant percentage of readmissions are related to the original operation. Admission diagnoses coded as primary during readmission include failure to thrive and cardiac complications, and were significantly higher in the open group, highlighting the more invasive nature and a predictably more difficult recovery process. This assertion is supported by a longer length of stay at the initial hospitalization, fewer number of days to the first readmission, and a longer length of stay at readmission. Second, it also suggests that in the state of California that sicker patients had an open repair, as documented by a larger percentage of patients who had CHF, COPD, and a higher Charlson Index score having OR over EVAR. This clearly documents the evolution and ultimate preference of EVAR to now replace open repair in the uncomplicated aneurysm patient. Finally, given the preference towards EVAR, more challenging anatomy patients are likely undergoing open repair, potentially with suprarenal clamping, which is also making the operations longer, more challenging, and potentially with worse early results. These factors may have certainly then contribute to a longer and more challenging post-operative course, increasing early readmission rates.
It is not a surprise that in state of California that early operative outcomes favor EVAR. In addition to the improved mortality, EVAR had a lower 30-day readmission rate, longer time to the first readmission, and shorter hospitalization at that first readmission. This is a comparable result to the VA population, where in a review of over forty-five thousand patients who underwent elective AAA repair, Bush et al. found a significantly lower 30-day mortality and complication rate following EVAR. The median length of stay was shorter for EVAR both in the ICU (1 day vs. 4 days) as well the hospital (3 days vs. 7 days).10 What focusing on early outcomes fails to discover, however is the readmission rates. Despite the greater number of overall readmission diagnoses associated with open repair early on in the initial postoperative recovery, by four months following surgery there was crossover where now EVAR readmssions overtook This trend continued and became statistically significant at one year and beyond. Open repair actually conferred an advantage against readmission compared with EVAR (OR= 0.862) at the one-year point, a seemingly counterintuitive finding. Kaplan-Meier analysis documents this (Figure 2), demonstrating fairly parallel lines between the two groups with respect to readmission rates after the first 120 days. Furthermore, the significantly higher 1-year mortality rate for OR can largely be contributed to the greater number of deaths at the surgical hospitalization. Once this hospitalization was removed from the analysis, the predicted one year mortality rate for EVAR was 1.08% and for open repair was 1.24%, which was not statistically significant (P=0.372).
When looking at readmission rates, the use of the HCUP SID allowed us to track patients by index hospitalization as well as all subsequent readmissions within the first year of surgery. To improve the precision of the causes for readmission we compared both all diagnoses as well as only primary diagnoses. The most common primary diagnoses associated with readmissions following either cohort were failure to thrive, cardiac complications, and infection. However, at 11.63%, only failure to thrive was significantly higher in the open group. Cardiac complications and infection were similar between the two groups. This was despite the significantly higher number of patients in the open repair group who had CHF. The significant number of readmissions associated with primary diagnoses of cardiac complications and infection is not surprising given the age of the population and baseline comorbidities. Other studies have demonstrated similar results. 11,12,13 There were also a significant number of patients with COPD at baseline in this study (29.2% in the EVAR and 37.7% in the open repair group). The link between tobacco use as well as aneurysm formation and growth is well documented.14 Interestingly, this seemed to predict a higher number of subsequent pulmonary readmissions in the open repair group only, arguing that EVAR is reasonable in the patient with significant pulmonary comorbidities.
One surprising finding is the wound complication readmission rate following EVAR. We anticipated that wound issues would be greater following OR, as has been found in previous studies, where laparotomy related complications have been reported to be as high as 23% in other surgical cohorts,15 compared with as low as 2% following open femoral access.16,17 However, this was not replicated in our cohort analysis. This suggests that focusing on lower-profile devices or more percutaneous access might further improve readmission rates after EVAR.18 Although incisional hernia was included in the category of wound complication readmission, it is probable that many of these do not develop or are evaluated until greater than one year following surgery.
Finally, focusing on predictors of readmission may help with system-based approaches towards improving outcomes after aneurysm repair. In this study, for all types of aneurysm repair, predictors of readmission within the first year for either type of repair include female gender (HR= 1.09), older age (HR= 1.01), and those patients with Medicaid insurance (HR= 1.22). Not surprisingly patients who are sicker (Charlson index 2 and 3) and those patients with an increased length of stay during their hospitalization were also at a greater risk of readmission within the first year. These risk factors should also be incorporated into pre-operative discussions about realistic expectations as to the function and quality-of-life after aneurysm repair, whether open or EVAR.
There are obvious limitations to this database analysis, and issues with administrative databases are acknowledged and well-documented in the literature. Miscoded events and incomplete coding are not uncommon events during hospitalizations and can account for a certain amount of error in this study. Principle diagnoses tend to be accurate; however, secondary diagnoses and comorbid diagnoses are often underreported. Furthermore, actual causes of readmission using a database of this sort can be difficult to identify due to accurate reasoning by the abstractor of the billing versus what the physician determines, and can make analysis challenging. Also the admission may or may not even be related to the actual surgery, for example, being admitted with a heart attack 9 months after surgery may have happened with a procedure or not. Finally, there is no way to know the number of patients who were readmitted to hospitals outside of the state of California. We still feel this particular database analysis is useful in determining relatively accurate readmission rates and causes after aneurysm repair.
CONCLUSION
In summary, total readmission rates within one year of elective AAA repair are greater following EVAR compared with open repair. Reasons for readmissions vary between the two cohorts. Further prospective studies should be performed to confirm those patients that are at increased risk of readmission following elective AAA repair. In addition, systems-based analysis of these causes of readmission can potentially improve patient expectations and care following elective aneurysm repair.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 2011 Western Vascular Society Annual Meeting, September 17-20, 2011 Kauai, HI
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
REFERENCES
- 1.Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991;5:491–9. doi: 10.1007/BF02015271. [DOI] [PubMed] [Google Scholar]
- 2.Prinnsen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, Balm R, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607–18. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 3.Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG. EVAR trial participants. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1): Randomized controlled trial. Lancet. 2005;365:2179–86. doi: 10.1016/S0140-6736(04)16979-1. [DOI] [PubMed] [Google Scholar]
- 4.Giles KA, Landon BE, Cotterill P, O'Malley AJ, Pomposelli FB, Schermerhorn ML. Thirty-day mortality and late survival with reinterventions and readmissions after open and endovascular aortic aneurysm repair in Medicare beneficiaries. J Vasc Surg. 2011;53:6–13e1. doi: 10.1016/j.jvs.2010.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Utzolino S, Kaffarnik M, Keck T, Berlet M, Hopt UT. Unplanned discharges from a surgical intensive care unit: Readmissions and mortality. J Crit Care. 2010;25:375–81. doi: 10.1016/j.jcrc.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: Randomized controlled trial. Lancet. 2004;364:843–8. doi: 10.1016/S0140-6736(04)16979-1. [DOI] [PubMed] [Google Scholar]
- 7.Matsumura JS, Brewster DC, Makaroun MS, Naftel DC. A multicenter controlled clinical trial of open versus endovascular treatment of abdominal aortic aneurysm. J Vasc Surg. 2003;37:262–71. doi: 10.1067/mva.2003.120. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg RK, Chuter TA, Sternbergh WC, 3rd, Fearnot NE. Zenith AAA endovascular graft: Intermediate-term results of the US multicenter trial. J Vasc Surg. 2004;39:1209–18. doi: 10.1016/j.jvs.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Sicard GA, Zwolak RM, Sidawy AN, White RA, Siami FS. Endovascular abdominal aortic aneurysm repair: Long-term outcome measures in patients at high-risk for open surgery. J Vasc Surg. 2006;44:229–36. doi: 10.1016/j.jvs.2006.04.034. [DOI] [PubMed] [Google Scholar]
- 10.Bush RL, Johnson ML, Collins TC, Henderson WG, Khuri SF, Yu HJ, et al. Open versus endovascular abdominal aortic aneurysm repair in VA hospitals. J Am Coll Surg. 2006;202:577–87. doi: 10.1016/j.jamcollsurg.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Blankensteijn JD, deJong SE, Prinssen M, Van der Ham AC, Buth J, van Sterkenburg SMM. Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms. NEJM. 2005;352:2398–2405. doi: 10.1056/NEJMoa051255. [DOI] [PubMed] [Google Scholar]
- 12.Brewster DC, Geller SC, Kaufman JA, Cambria RP, Gertler JP, LaMuraglia GM, et al. Initial experience with endovascular aneurysm repair: Comparison of early results with outcome of conventional open repair. J Vasc Surg. 1998;27:992–1003. doi: 10.1016/s0741-5214(98)70002-3. [DOI] [PubMed] [Google Scholar]
- 13.Dalainas I, Nano G, Casana R, Tealdi D. Mid-term results after endovascular repair of abdominal aortic aneurysms: A four-year experience. Eur J Vasc Endovasc Surg. 2004;27:319–23. doi: 10.1016/j.ejvs.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Lederle FA, Johnson GR, Wilson SE, Chute EP, Hye RJ, Makaroun MS, et al. the ADAM VA Cooperative Study Investigators The aneurysm detection and management study screening program: Validation cohort and final results. Arch Intern Med. 2000;160:1425–30. doi: 10.1001/archinte.160.10.1425. [DOI] [PubMed] [Google Scholar]
- 15.Murray BW, Cipher DJ, Pham BT, Anthony T. The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg. 2011 doi: 10.1016/j.amjsurg.2011.06.014. in press. [DOI] [PubMed] [Google Scholar]
- 16.Malwaki AH, Hinchliffe RJ, Holt PJ, Loftus IM, Thompson MM. Percutaneous access for endovascular aneurysm repair: A systematic review. Eur J Vasc Endovasc Surg. 2010;39:676–82. doi: 10.1016/j.ejvs.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Slappy AL, Hakaim AG, Oldenburg WA, Paz-Fumagalli R, McKinney JM. Femoral incision morbidity following endovascular aortic aneurysm repair. Vasc Endovascular Surg. 2003;37:105–9. doi: 10.1177/153857440303700204. [DOI] [PubMed] [Google Scholar]
- 18.Al-Khatib WK, Dua MM, Zayed MA, Harris EJ, Dalman RL, Lee JT. Percutaneous EVAR in females leads to fewer wound complications. Ann Vasc Surg. 2012;26:476–82. doi: 10.1016/j.avsg.2011.11.026. [DOI] [PubMed] [Google Scholar]