Abstract
Objectives:
We examine how the likelihood of smoking cessation among smokers and patterns of adherence to smoking cessation differ by partnership status, partnership changes, and partners’ smoking behavior. The data are a nationally representative sample of smokers in middle and older age from the Health and Retirement Study (1992–2010).
Method:
We use multivariate logistic regression models to analyze the likelihood of smoking cessation among smokers and then estimate adherence to smoking cessation using discrete-time event history models.
Results:
Those partnered with smokers and those whose partners relapse into smoking are much less likely than the unpartnered to quit smoking and adhere to smoking cessation. Respondents partnered with non-smokers and those whose partners quit smoking are more likely to quit smoking than the unpartnered. Those recently widowed, divorced, and repartnered have similar smoking changes to the consistently unpartnered.
Discussion:
Being partnered does not always mean healthier behavior changes. Rather, the association between partnership status and smoking changes depends greatly on the health behavior changes of the partner. The partnership context at the time of smoking cessation sets the stage for longer term patterns of adherence, shaping health in older age.
Keywords: Couples, Health and Retirement Study, Health behaviors, Older Age, Smoking
Smoking cessation and other healthy behavior changes are important in middle and older age, especially when managing a variety of new chronic illnesses that are common during this life stage (Lichtenstein et al., 2006; Margolis, 2013a, 2013b). The likelihood of an individual making healthy changes and adhering to them may depend on whether that person is partnered, their partner’s health behaviors and changes, and the dynamics of the dyad. The marital relationship is one of the most important relationships for influencing health behaviors and ultimately mortality (Umberson, 1987). Marital relationships may be even more salient for the health of older adults because as individuals age they tend to focus more of their time and resources on their primary social relationships, like marriage (Carstensen, 1992; Williams & Umberson, 2004). It may be particularly difficult for one middle or older aged spouse to make a behavior change if the other spouse does not, or it may be easier for spouses to quit together if they encourage each other because smoking is a social behavior, and because of the increased importance and typical duration of the marital relationship in middle and older age (Falba & Sindelar, 2008).
Many studies have documented large differences in health and health behaviors by union status, showing that married people report better health (Williams & Umberson, 2004), healthier behaviors (Umberson, 1992), and lower mortality (Manzoli, Willari, Pirone, & Boccio, 2007) than the unmarried. However, recent research has shown that not all partners have a positive influence on health (Bove, Sobal, & Rauschenbach, 2003; DeVault, 1991; Reczek, 2012) and the ways in which health behaviors are affected by partnership status and partnership transitions may depend on the partner’s positive or negative health-related behaviors. Research has mainly ignored heterogeneity in spousal influence on health behaviors among married couples. This means that little is known about how the health behavior changes of unmarried individuals compare to those who are married to partners with different health behaviors or how gaining or losing a partner may affect health behavior changes differently.
In this article, we document great diversity in patterns of smoking cessation, an important health behavior change, by specific partnership context that takes into account partnership status, partner’s smoking, and partnership changes. We compare the unpartnered with partnered respondents whose partners have different smoking behavior and those who undergo partnership transitions. The study makes two clear contributions to the literature on marriage and health in older age. First, we analyze patterns of health behaviors by partner characteristics using longitudinal data. This allows for more valid estimates of the impact partner support has on health than do cross-sectional analyses which may obscure important variation within union status groups and lead to biased results. Second, we show that partnership context at the time of smoking cessation sets the stage for the longer-term pattern of adherence, shaping health in older age. In the following sections, we review past research that examines union status and health, and union status and smoking cessation specifically. Then, we explore why partnership context is important for the health behaviors of middle and older age adults.
Union Status and Health
Married people report better health (Williams & Umberson, 2004), healthier behaviors (Umberson, 1992) and have lower mortality (Manzoli et al., 2007) than those who are not married, even after accounting for age, race, and socioeconomic status. The health advantage of the married is due in part to selection (Goldman, 2001), but spousal influence, support, and social control over risky health behaviors also play a role (Carr & Springer, 2010; Umberson, 1987, 1992). Social control over a partner’s health behavior may be direct, through sanctioning or impeding a behavior, or may be more indirect through the internalizing of norms about the behavior (Reczek, 2012; Umberson, 1987). A partner can also offer emotional support, encouragement, or help set goals about making a healthy change, especially when a couple is involved in a joint behavior change (Falba & Sindelar, 2008). The internal dynamics of couples differ, but convergence theory suggests that the behaviors of spouses will become more similar over time (Falba & Sindelar, 2008; Leonard & Mudar, 2004). This may be because of sustained social control of one partner over the behaviors of the other. It may also be because the members of the couple share an environment, resources, and social networks over time and these factors may influence one or both of their behaviors (Meyler, Stimpson & Peek, 2007). Physical and emotional closeness may enhance the convergence of couples over time, if high marital quality leads to similar views regarding health. Both social control theory and convergence theory highlight the link between the context of the partnership and the health behaviors of both partners. However, it remains unclear whether a spouse with unhealthy behaviors will become more like their healthy spouse or the reverse.
Recent research has shown that having a partner is not always good for one’s health. Instead, there is variation among married persons and partner’s health behaviors are important for shaping one’s own behaviors and health outcomes (Carr & Springer, 2010). A partner’s health behaviors can either positively or negatively affect one’s own health behaviors (Bove et al., 2003; DeVault, 1991; Reczek, 2012). For example, a partner can positively influence health behaviors through shared healthy eating, encouraging exercise, or motivating smoking cessation (Umberson, 1987, 1992), but a partner’s behaviors can also be detrimental to health by reinforcing negative behaviors like smoking (Reczek, 2012; Umberson, 1987, 1992). For example, York Cornwell and Waite (2012) found that having a partner is not associated with healthy hypertension management among older adults, and hypothesized that this may be due to differences in partner characteristics that were not available for analysis in their study. Given that partner influence can be either positive or negative, grouping together all married people and comparing them to the unmarried may obscure important variation in the relationships between partnership status, partner’s health behaviors, and one’s own health behaviors and may underestimate the long-term implications of partnership context for health. Examining how spouses both help and harm the health and health behaviors of their partner is a key direction for aging research (Carr and Springer, 2010), which has been challenging due to the lack of appropriate dyadic data. Instead, many studies focus on differences in health behaviors and outcomes by partnership status (Liu & Umberson, 2008), and far fewer explore the characteristics of partners (Kravdal, 2008).
Smoking Cessation and Union Status
Smoking cessation and adherence are important to examine for two reasons. First, smoking is a behavior that is clearly detrimental to health. Quitting is recommended for the management of many chronic illnesses and can increase remaining years of life, even when quitting in middle age (Doll, Peto, Boreham, & Sutherland, 2004; Lichtenstein et al., 2006). Second, partner’s smoking is clearly important for smoking cessation and adherence, which may be in part due to direct and indirect social control within the couple (Umberson 1987, 1992) or behavior diffusion (Reczek, 2012). Individuals are more likely to stop smoking if their partners are non-smokers than if they smoke (McBride et al., 1998; Monden, van Lenthe, de Graaf, & Kraaykamp, 2003) and smoking cessation of married people is more likely if their spouse also quits (Falba & Sindelar, 2008). Partner’s smoking is also associated with lower adherence to smoking cessation in the short-term (Coppotelli & Orleans, 1985; Mermelstein, Cohen, Lichtenstein, Baer, & Kamarck, 1986), over a 2-year period (Franks, Pienta, & Wray, 2002) and among pregnant women (Kahn, Certain, & Whitaker, 2002). No existing research has examined how patterns of smoking cessation and adherence of the unpartnered compare to the partnered with different types of smoking behavior and also those who undergo different partnership transitions. This is important because partnership status, like health behaviors, is not static and without examining changes in both partnership and smoking, we only get one part of the picture of how partnership is associated with health behaviors.
A focus on partner smoking and smoking cessation among older adults has been neglected by prior research, but the health behaviors of older people are important for three reasons. First, it may be difficult for one spouse to make a behavior change if the other spouse does not because people become more set in their ways and more addicted to smoking, or because partners become more similar over time (Meyler et al., 2007). Second, smoking cessation is advised when doctors diagnose many chronic illnesses that are common in middle and older age (Lichtenstein et al., 2006) and past research has shown that a new chronic condition can trigger smoking cessation not only for the new patient (Margolis, 2013a), but also for the patient’s spouse (Margolis, 2013b). A partner’s health behaviors and changes may be extremely important in older age, because new illnesses are common and spouses may be most beneficial for health when taking a “crisis caregiver” role (Idler, Boulifard, & Contrada, 2012). Third, socioemotional selectivity theory posits that as individuals age their social networks shrink and they dedicate more time and resources to their more intimate relationships like marriage (Carstensen, 1992; Williams & Umberson, 2004). The marital relationship has been found to be one of the most important relationships for health behaviors and mortality (Umberson, 1987) and its importance may be magnified in older ages due to the increased focus on the marital relationship.
The Present Study
In this article, we examine how the likelihood of smoking cessation among smokers and how patterns of adherence to smoking cessation differ by partnership status, partnership changes, and partners’ smoking behavior. We extend previous research in four ways. First, we examine partnership status, partner smoking, and partnership changes over time and examine how these factors are associated with respondents’ smoking cessation and adherence over the medium term. This allows us to examine patterns of smoking changes for respondents with steady smoking and non-smoking partners, respondents with a partner that either starts or stops smoking, respondents who remain unpartnered, and those who undergo partnership changes such as widowhood, separation/divorce, and repartnering. The variation we document highlights the potential bias in cross-sectional estimates of differences in health behaviors by partnership status. Additionally, we highlight how partnership context at the time of smoking cessation sets the stage for longer term patterns of adherence, shaping health trajectories in older age. This highlights the lasting repercussions of dyadic dynamics for health and aging. Second, our sample is nationally representative of smokers in middle and older age, observed over a 20-year period, allowing the examination of smoking changes and adherence over the medium term. Previous studies have focused on younger samples and a much shorter period (Homish & Leonard, 2005; McBride et al., 1998; Pollak & Mullen, 1997; Woodby, Windsor, Snyder, Kohler, & Diclemente, 1999). Third, because both partners are respondents, health behaviors are all self-reported, which are higher quality data than those reported by only one partner used in other research (Coppotelli & Orleans, 1985; Fuller, 2010). Fourth, we include controls for age, race, education, new health events, work, and level of prior smoking, factors which have been shown to also affect changes in smoking (Margolis, 2013a, 2013b), and some of which medical studies could not include (Pollak & Mullen, 1997; Woodby et al., 1999).
Method
Sample
For this study, we use the Health and Retirement Study (HRS), an aging study that is nationally representative of the U.S. population above age 50. The study uses a multistage area probability sample of households, with oversamples of African Americans, Hispanics, and Floridians. Interviews were conducted in-person or on the telephone. Detailed information on the study design, sample, and response rates is available (Heeringa & Connor, 1995). The longitudinal nature of the data allow for the analysis of changes in smoking behavior among a representative sample of older Americans and if respondents are married or cohabiting, their partners are also interviewed and self-report their own smoking behavior. With these data, we also observe many other factors associated with smoking changes such as demographic factors, work, and health.
We focus on smokers in middle and older age (ages 50–85) interviewed between 1992 and 2010. This age range is chosen because many respondents make behavior changes during this time, in part to manage new chronic conditions that arise. Above age 85, smoking is less prevalent and changes are less common. Of the 6,712 respondents who we observe smoking, we exclude respondents who were part of the AHEAD study cohort because questions about smoking were different (n = 771, 11.5%) and respondents who participated in fewer than two consecutive interviews with complete information on key variables (n = 691, 10.3%). The analytic sample includes 5,250 respondents and 33,807 person-interviews, 78% of all observed smokers. These respondents are analyzed until they leave the study due to mortality (30% of smokers are reported dead during the study period), the end of the study period, when they age out of the sample at age 86, or are lost to follow-up which is uncommon in this sample (Heeringa & Connor, 1995). Because of the study design, many respondents have partners who are also study respondents. Partners within the study age range are included as respondents. Partners outside of the study age range are excluded from the analytic sample, but their smoking behavior is analyzed as partner data for the included respondent.
We also analyze adherence to smoking cessation among smokers who quit and whether adherence to cessation depends on partnership status and partner’s smoking. Adherence is examined among all respondents who quit smoking and are followed for at least one subsequent interview (n = 2,285). The length of adherence is measured from the first observed smoking cessation (which for 85% of respondents is the only instance of smoking cessation observed) to the interview when respondents report smoking again, or are censored because of death, attrition, or the end of the follow-up period. This analysis captures the broad smoking trajectory, but does not capture short-term smoking changes because interviews are about 2 years apart. Thus, these data provide a conservative estimate of the amount of change.
Measures
The first dependent variable is stopping smoking, because smoking cessation is an important part of chronic disease management and healthy aging. In each interview, participants were asked, “Do you smoke cigarettes now?” Smoking cessation is defined by whether the respondent reported smoking in one interview, but reported not smoking in the subsequent interview.
The key explanatory variable examines the respondents’ partnership status and smoking status of his or her partner at interview t and interview t − 1. Constructing our key independent variable using data on partnership status, and respondents’ and partners’ smoking allows us to examine more categories than could be studied if using only one wave of data. A mutually exclusive and time-varying categorical variable is used: (a) unpartnered at interviews t − 1 and t, (b) partnered with a smoker at interviews t − 1 and t, (c) partnered with a non-smoker at interviews t − 1 and t, (d) partnered, and partner quits smoking between interviews t − 1 and t, (e) partnered, and partner relapses into smoking between interviews t − 1 and t (98% of those who “start” smoking are former smokers), (f) widowed between interview t − 1 and t, (g) separated/divorced between interview t − 1 and t, (h) gained partner between interview t − 1 and t, or (i) missing either partnership status or partner’s smoking data in interview t − 1 or t. Among respondents who experience a partnership transition (widowed, separated/divorced/gained partner), we do not distinguish the current or former partner’s smoking due to small samples (e.g. widowed by former smoker vs. widowed by non-smoker).
We also include a number of confounding factors. Demographic variables are age at interview, sex, years of education, and race/ethnicity coded as: non-Hispanic black, non-Hispanic white, and Hispanic/other race. We control whether the respondent reported any new chronic health conditions for which smoking cessation is recommended (hypertension, heart disease, diabetes, lung disease, stroke, and cancer) and also the number of existing chronic conditions reported in the previous wave. Labor force participation is coded as not working, working part-time, or full-time, and is included because work context also shapes smoking behavior. Both health variables and labor force participation are time-varying. To take into account the fact that some members of the analytic sample died during the period of analysis, we include a dummy variable for whether the respondent died during the study. Last, we include the number of cigarettes smoked at the previous interview to capture the fact that smoking is addictive and it will be more difficult to quit for the heaviest smokers.
Analytical Approach
First, we use logistic regression models to analyze the likelihood of smoking cessation among those who smoked at the previous interview. We examine how the likelihood of stopping smoking varies by partnership and partner’s smoking. Multivariate models control for respondents’ age, sex, education, race/ethnicity, new and existing chronic conditions, labor force participation, cigarettes smoked at the previous interview, and a dummy for whether they died during follow-up. Then, we estimate the predicted probabilities of smoking cessation by partnership status and partner’s smoking, holding other variables at their mean levels. To account for the non-independence of observations for each individual, we estimate the models on pooled data using robust standard errors.
Second, we address whether there are differences by partnership status and partner smoking in adherence to smoking cessation. We chart adherence with Kaplan–Meier survival curves. Then, we estimate adherence using a discrete-time event history framework, estimating binary logistic regression models on pooled person-interview observations. This method is ideal because it is not biased by censoring and allows time-varying covariates (Allison, 1982). It is also more appropriate than continuous survival analysis because the data on health behaviors are available at each biennial interview, not at the exact time that the change occurs. We estimate the conditional probability of smoking relapse, given that the individual has stopped smoking at an earlier interview. Respondents cease contributing person-interviews when they revert back to smoking or are censored, either because of the end of the study, death, or attrition. First, we examine whether there are differences in adherence to smoking cessation by partnership and partner’s smoking when controlling for the number of months between interviews, and years since the change was made. Then we control for sex, education, race, new chronic conditions, work status, and whether the respondent died.
Results
Table 1 presents characteristics of the analytic sample (N = 5,250). The distributions of the independent variables are shown in the right column. The left column shows the percentage in each category that quits smoking. Fifty two percent of respondents are observed stopping smoking during the study period. The frequency of smoking cessation varies by respondents’ partnership status and partner’s smoking behavior over the study period. Smoking cessation is more common among those who are continuously partnered with a non-smoker (68.3%) or continuously partnered in both waves to someone who also quits smoking (67.6%). Smoking cessation is less common among respondents who are partnered with a smoker (52.3%) or those who get separated or divorced during the same time period (50.6%). Those who are continuously unpartnered have a higher probability of smoking cessation (59.5%) than those who are partnered with smokers but lower than those partnered with non-smokers.
Table 1.
Characteristics of the Analytic Sample, Health and Retirement Study 1992–2010 (N = 5,250)
| % Observed quitting | % or mean (SD) of analytic sample | |
|---|---|---|
| Percent of respondents observed quitting smoking (1992–2010) | NA | 52.27 |
| Partnership status and partner smokinga | ||
| Unpartnered in previous and current interview | 59.46 | 31.72 |
| Partnered in previous and current interview: partner smokes both interviews | 52.27 | 17.09 |
| Partnered in previous and current interview: partner non-smoker at both interviews | 68.30 | 36.75 |
| Partnered in previous and current interview: partner stops smoking | 67.61 | 2.85 |
| Partnered in previous and current interview: partner relapses into smoking | 62.60 | 1.32 |
| Widowed since last interview: former partner smoker or non-smoker | 57.31 | 2.13 |
| Separated/divorced since last interview: former partner smoker or non-smoker | 50.57 | 1.23 |
| Gained partner since last interview: new partner smoker or non-smoker | 56.57 | 1.16 |
| Missing partnership or partner smoking data in previous or current interview | 51.25 | 5.75 |
| Demographic characteristics | ||
| Age at first interview | NA | 55.62 (5.4) |
| % Female | 52.48 | 49.87 |
| % Male | 52.05 | 50.13 |
| Educational attainment in years | NA | 11.73 (3.1) |
| Race/ethnicity | 51.23 | 71.43 |
| Non-Hispanic White | 54.39 | 18.21 |
| Non-Hispanic Black | 55.70 | 10.36 |
| Hispanic/other | ||
| Health status | ||
| Reports at least one new smoking-related chronic condition (1992–2010) | 61.74 | 63.18 |
| Reports no new smoking-related chronic conditions (1992–2010) | 36.01 | 36.82 |
| Number of existing chronic conditions (at first interview) | ||
| None | 52.33 | 53.58 |
| One | 53.43 | 29.70 |
| Two | 52.31 | 11.94 |
| Three or more | 44.22 | 4.78 |
| Other characteristics | ||
| Labor force participation | ||
| Not working | 51.68 | 37.33 |
| Working part-time | 51.16 | 13.10 |
| Working full-time | 53.00 | 49.56 |
| Cigarettes smoked at first interview | NA | 17.37 (13.3) |
| Reported dead during follow-up | NA | 30.29 |
| Number of interviews | NA | 6.44 (2.7) |
a Tabulated for all interviews except the first in order to incorporate changes between interview t − 1 and t.
Table 2 presents results from logistic regression models predicting smoking cessation by partnership status and partner’s smoking. The unpartnered are not the least likely to stop smoking. Two groups of partnered smokers have significantly lower odds of smoking cessation than the unpartnered—those whose partners smoked at both interviews [odds ratio (OR) = 0.73], and those whose partners relapsed into smoking between the previous and current interview (OR = 0.51). There are three groups of respondents who experienced a partnership change from the previous to current wave, including those who are widowed, separated or divorced, or gained a partner since the previous interview. These groups are small, limiting statistical power to differentiate them from the reference group. However, the odds ratios are similar and are all lower than one. If they are combined into one group, they are significantly less likely to stop smoking than those who are unpartnered in both interviews (results not shown). Other partnered groups are significantly more likely to stop smoking than the unpartnered—those partnered with a non-smoker (OR = 1.26), and those whose partner quits smoking (OR = 4.10).
Table 2.
Summary of Logistic Regression Analysis Predicting Smoking Cessation Among Smokers, Health, and Retirement Study 1992–2010 (N = 5,250)
| Bivariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | B | SE B | OR | B | SE B | OR | ||
| Partnership status and partner smokinga
(unpartnered in previous and current interview) | ||||||||
| Partnered in previous and current interview: partner smokes both interviews | –0.47 | .062 | 0.62 | *** | –0.32 | .065 | 0.73 | *** |
| Partnered in previous and current interview: partner non-smoker at both interviews | 0.17 | .046 | 1.19 | *** | 0.23 | .049 | 1.26 | *** |
| Partnered in previous and current interview: partner stops smoking | 1.25 | .086 | 3.49 | *** | 1.41 | .093 | 4.10 | *** |
| Partnered in previous and current interview: partner relapses into smoking | –0.62 | .228 | 0.54 | ** | –0.68 | .240 | 0.51 | ** |
| Widowed since last interview: former partner smoker or non-smoker | –0.20 | .142 | 0.81 | –0.23 | .152 | 0.79 | ||
| Separated/divorced since last interview: former partner smoker or non-smoker | –0.29 | .178 | 0.75 | –0.21 | .194 | 0.81 | ||
| Gained partner since last interview: new partner smoker or non-smoker | –0.20 | .187 | 0.81 | –0.19 | .118 | 0.83 | ||
| Missing partnership or partner smoking data in previous or current interview | –2.32 | .108 | 0.09 | *** | 0.06 | .118 | 1.06 | |
| Age | 0.04 | .002 | 1.04 | *** | 0.01 | .003 | 1.01 | * |
| Female (male) | –0.05 | .036 | 0.95 | –0.07 | .042 | 0.93 | ||
| Education | 0.01 | .006 | 1.01 | 0.03 | .007 | 1.03 | *** | |
| Race (non-Hispanic White) | ||||||||
| Non-Hispanic Black | 0.16 | .047 | 1.17 | *** | 0.11 | .055 | 1.12 | * |
| Hispanic or other | 0.23 | .059 | 1.26 | *** | 0.24 | .074 | 1.27 | ** |
| Any new smoking-related condition (none)a | 1.15 | .044 | 3.15 | *** | 0.95 | .047 | 2.60 | *** |
| Number of existing smoking-related conditionsa | 0.09 | .017 | 1.10 | *** | 0.09 | .019 | 1.09 | *** |
| Cigarettes smoked per day (previous wave)a | –0.02 | .002 | 0.98 | *** | –0.02 | .002 | 0.98 | *** |
| Whether died during study period | –0.04 | .041 | 0.95 | –0.00 | .048 | 0.99 | ||
| Labor force status (not working)a | ||||||||
| Part-time | –0.14 | .056 | 0.86 | ** | –0.03 | .062 | 0.97 | |
| Full-time | –0.44 | .041 | 0.64 | *** | –0.14 | .051 | 0.87 | ** |
| Constant | –2.63 | .254 | 0.07 | *** | ||||
| X 2 | 901.0 | |||||||
Notes: OR = odds ratio.
aNotes time-varying variable.
*p < .05, **p < .01, ***p < .001.
Aside from partnership status and partner’s smoking, the other important predictor of smoking cessation is whether the respondent reports any new chronic condition (OR = 2.60). In addition, smoking cessation is more likely as age increases, among those with more education, Blacks and Hispanics compared with non-Hispanic whites, those with more existing health problems, and those who previously smoked slightly less. Table 3 presents the predicted probabilities of smoking cessation by partnership status and partner’s smoking holding the covariates at their mean values. Respondents with partners who relapse into smoking and those whose partners continuously smoke have the lowest probabilities of smoking cessation at .07 (95% CI 0.04–0.10) and 0.10 (0.09–0.11). Those who go through partnership transitions (widowed, separated/divorced, or gained partner) have a 0.11 probability of smoking cessation (0.07–0.15). The unpartnered are in the middle with a 0.13 probability of smoking cessation (0.12–0.14). Those partnered with a non-smoker are more likely than the unpartnered to stop smoking (0.16) and those whose partners quit smoking are the most likely by far with a 0.38 probability (0.34–0.42).
Table 3.
Predicted Probabilities (95% CI) of Smoking Cessation by Partnership/Partner Smoking, Health and Retirement Study 1992–2010 (N = 5,250)
| Partnership status and partner’s smoking | Predicted probability | 95% CI |
|---|---|---|
| Partnered in previous and current interview: partner relapses into smoking | 0.07 | (0.04–0.10) |
| Partnered in previous and current interview: partner smokes both interviews | 0.10 | (0.09–0.11) |
| Widowed since last interview: former partner smoker or non-smoker | 0.11 | (0.08–0.13) |
| Separated/Divorced since last interview: former partner smoker or non-smoker | 0.11 | (0.07–0.14) |
| Gained partner since last interview: new partner smoker or non-smoker | 0.11 | (0.07–0.15) |
| Unpartnered in previous and current interview | 0.13 | (0.12–0.14) |
| Missing partnership or partner smoking data in previous or current interview | 0.14 | (0.11–0.16) |
| Partnered in previous and current interview: partner non-smoker at both interviews | 0.16 | (0.15–0.17) |
| Partnered in previous and current interview: partner stops smoking | 0.38 | (0.34–0.42) |
Note: Predicted probabilities are calculated from multivariate model in Table 2, holding other covariates at mean levels.
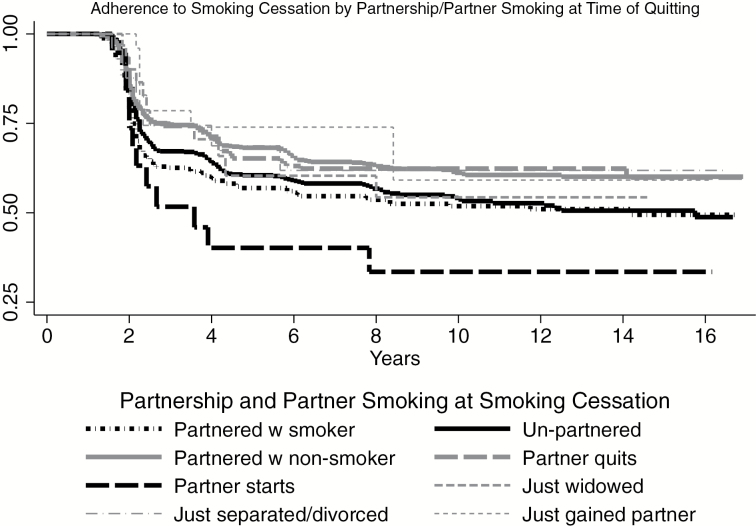
What are the patterns in adherence to smoking cessation by partnership status and partner’s smoking? Figure 1 presents the Kaplan–Meier survival curve for adherence to smoking cessation by partnership context. For this chart, partnership and partner’s smoking is time-invariant and refers to the time of smoking cessation because the method requires time-invariant categories. Overall, the patterns show that a few years after quitting smoking, about two-thirds of respondents remain non-smokers and that over the longer term, slightly more than half are still non-smokers. However, the patterns of adherence vary by partnership and partner’s behavior at the time of quitting. Those whose partners relapsed into smoking when they quit, start smoking again soon after quitting. Only 40% are still not smoking after 4 years and only about one-third adhere in the medium term. Those who are partnered with smokers when they quit smoking are the second group who take up smoking again. The unpartnered are in the middle, with about two-thirds adhering to smoking cessation after 2–4 years and about half at 8–12 years after quitting. Respondents with very high adherence to smoking cessation are those who are either partnered with non-smokers or those whose partners quit at the same time as them (shown in the thick solid and dashed gray lines). About three quarters remain non-smokers at 2–4 years and two-thirds at 6–12 years. Respondents who gain a partner at the time of smoking cessation also have very high adherence to smoking cessation, although this group is small.
Figure 1.
Adherence to smoking cessation by partnership/partner smoking at time of quitting.
Table 4 presents results from discrete-time event history models, examining adherence to smoking cessation in a multivariate framework. Respondents partnered with non-smokers (OR = 0.69) and those whose partners quit smoking (OR = 0.70) have significantly lower risk of reverting back to smoking than the unpartnered. There are no significant differences in adherence patterns for those partnered with smokers and the unpartnered. The small group of respondents with partners who relapsed into smoking have a higher risk of reverting back to smoking (OR = 2.11), but this is not statistically different from the unpartnered (p > .05). There are few other significant correlates of adherence to smoking cessation, highlighting the importance of partnership context.
Table 4.
Correlates of Adherence to Smoking Cessation: Odds Ratios from Discrete Time Event History Models for Reverting Back to Smoking After Smoking Cessation (N = 2,285)
| Bivariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE B | OR | B | SE B | OR | |||
| Partnership status and partner smoking (Unpartnered in previous and current interview) | ||||||||
| Partnered in previous and current interview: partner smokes at both interviews | 0.08 | .121 | 1.09 | −0.01 | .126 | 0.99 | ||
| Partnered in previous and current interview: partner non-smoker at both interviews | −0.34 | .095 | 0.71 | *** | −0.37 | .102 | 0.69 | *** |
| Partnered in previous and current interview: partner stops smoking | −0.31 | .154 | 0.73 | * | −0.36 | .159 | 0.70 | * |
| Partnered in previous and current interview: partner relapses into smoking | 0.90 | .392 | 2.45 | * | 0.75 | .399 | 2.11 | |
| Widowed since last interview: former partner smoker or non-smoker | −0.24 | .350 | 0.78 | −0.29 | .351 | 0.74 | ||
| Separated/Divorced since last interview: former partner smoker or non-smoker | −0.23 | .407 | 0.79 | −0.38 | .410 | 0.68 | ||
| Gained partner since last interview: new partner smoker or non-smoker | −0.51 | .424 | 0.60 | −0.47 | .429 | 0.62 | ||
| Missing partnership or partner smoking data in previous or current interview | 0.08 | .241 | 1.08 | 0.03 | .244 | 1.03 | ||
| Age | −0.03 | .006 | 0.97 | *** | −0.03 | .007 | 0.97 | *** |
| Female (male) | 0.12 | .078 | 1.12 | −0.01 | .084 | 1.01 | ||
| Education | −0.01 | .012 | 0.99 | −0.02 | .014 | 0.97 | ||
| Race (non-Hispanic White) | ||||||||
| Non-Hispanic Black | 0.14 | .101 | 1.15 | 0.05 | .106 | 1.06 | ||
| Hispanic or other | 0.06 | .124 | 1.06 | −0.04 | .136 | 0.96 | ||
| Any new smoking-related condition (none)a | −0.11 | .104 | 0.89 | −0.07 | .106 | 0.93 | ||
| Labor force status (not working)a | ||||||||
| Part-time | 0.23 | .115 | 1.26 | * | 0.17 | .120 | 1.18 | |
| Full-time | 0.24 | .093 | 1.25 | * | 0.06 | .104 | 1.06 | |
| Whether died during study period | −0.16 | .097 | 0.85 | −0.14 | .101 | 0.90 | ||
Notes: aNotes time-varying variable.
bAll models control for the number of months between interviews and dummies for years.
*p < .05, **p < .01, ***p < .001.
We performed multiple sensitivity analyses and the results of each of these were similar to those presented here. First, we ran the analyses separately for men and women because social control over health behaviors is often gendered (Umberson, 1992) and because partnered respondents in the same household are both included and not independent of each other. Results were remarkably similar and therefore we present the combined results. Second, we tested whether there was an interaction between partnership status or partner’s smoking and a new chronic illness, but found no significant interaction. Third, we tested whether the results differ if we included only the first smoking cessation for respondents among the set that quit smoking more than once during the period of observation. Fourth, we weighted our regression models and found similar results, but with much higher significance levels and chose to report the unweighted results. Fifth, the results were similar when excluding the cohabiting respondents, likely because this is a small group (<6% at first interview). Sixth, we used multiple imputation to estimate values for the missing control variables but found similar results to the ones presented. Last, the results are robust to coding choices of the control variables.
Discussion
Not all partners are beneficial for health, but few studies have examined the variation within the partnered group and the importance of a partner’s health behaviors in shaping one’s own behaviors and health outcomes relative to other factors. This study used a sample of 5,250 middle aged and older smokers from the Health and Retirement Study, a nationally representative longitudinal survey of older Americans. We examined how patterns of smoking cessation and adherence to smoking cessation differ by partnership status and partner’s smoking using self-reported smoking data. We focus on partnership because it is the most important relationship for health behaviors, due in part to direct and indirect social control within the couple (Umberson, 1987), behavior diffusion (Reczek, 2012), and shared environments.
We find that the unpartnered do not have the lowest likelihood of smoking cessation and adherence. Similar to other literature, we find that those partnered with smokers have a much lower likelihood of smoking cessation and those partnered with non-smokers have a much higher likelihood of smoking cessation (McBride et al., 1998; Monden et al., 2003). However, our nuanced results show some new patterns. The partner’s smoking dynamics are hugely important for respondents’ smoking changes. Those with partners who quit smoking at the same time that they did had by far the highest probabilities of smoking cessation (0.38), much higher than those whose partners were stable non-smokers (0.16). Those partnered with steady smokers and those whose partners relapsed into smoking during the study period have the lowest likelihoods of smoking cessation (0.10 and 0.07, respectively). The likelihood of smoking cessation among the unpartnered was 0.13, which fell between those partnered with smokers and those partnered with non-smokers (steady non-smokers and those who recently quit). The consistently unpartnered had similar probabilities of smoking cessation as those who experienced three types of partnership transitions—those who were widowed, separated/divorced, or re-partnered since last interview. All of these groups had similar probabilities of smoking cessation. This finding is new and future research should go into greater depth to explore more heterogeneity within these groups who experience partnership changes of different types. We did not have the sample size to do so in this article.
Similarly, large variability by partnership status and partner’s smoking was also found regarding adherence to smoking cessation. Of the middle aged and older Americans who quit smoking during the study period, those who were partnered with a smoker or whose partner began smoking during the study were the least successful in abstaining from smoking. This echoes previous work that found that partner’s smoking was associated with lower adherence to smoking cessation in the short term (Coppotelli & Orleans, 1985; Franks et al., 2002; Kahn et al., 2002; Mermelstein et al. 1986) but extends this comparison to a much longer time period. There are also, however, many more important patterns. Respondents who quit when partnered with a non-smoker or who had a partner who quit with them were the most successful at smoking cessation. Those who were unpartnered or who experienced changes in their partnership status had similar adherence patterns to those partnered with smokers, but worse than those partnered with non-smokers. The similar adherence patterns among those experiencing partnership transitions and the unpartnered may reflect variation within this group, for example getting divorced from a smoker might differ from getting divorced from a non-smoker. Variability in adherence patterns among those undergoing different types of partnership transitions to and from partners with different health behavior patterns should be the topic for other research with larger samples of respondents experiencing partnership transitions.
Our results join a growing body of literature suggesting a more nuanced understanding of how partners (or lack thereof) influence health (Meyler et al., 2007; Reczek, 2012). In terms of smoking specifically, being partnered does not always mean healthier behavior changes; the association between partnership and smoking changes depends greatly on the health behavior and health behavior changes of the partner. In fact, the unpartnered display healthier behaviors than those with partners who engage in unhealthy behaviors, regardless of gender.
There are several reasons why those whose partners quit smoking have higher rates of quitting and better adherence than others, even those partnered with non-smokers. One is that when a partner successfully quits, it takes away the smoking cues in the home environment, making it easier for a partner to quit (Franks et al., 2002; Mermelstein et al., 1986; Orleans, 2000). A second reason is that quitting together means that a partner will provide support for the behavior change (Franks et al., 2002). This support may be more effective coming from a former smoker than a non-smoker because former smokers will better understand the situation and provide more empathetic support (Coppotelli & Orleans, 1985; Mermelstein et al., 1986). A third possible reason why partners are more successful when quitting together is unique to older couples. Older smokers are likely addicted and have decided not to quit earlier in life, and factors that induce them to quit are going to be different from those that encourage younger smokers to quit (Clark, Rakowski, Kviz, & Hogan, 1997). A partner’s influence combined with increased concerns about health in later life may be more important among older smokers (Cross & Markus, 1991; Siegler, Kaplan, Von Dras, & Mark, 1999; Margolis, 2013b).
We ran our sensitivity analysis separately for men and women but found no differences. In their study of marriage and smoking cessation in middle age, Franks and colleagues (2002) did not find gender differences either; nor did Falba and Sindelar (2008) in their study of spousal concordance in health behavior changes. We hypothesize that social control, which is more often exercised by women to influence men’s behaviors (Reczek & Umberson, 2012; Umberson, 1992), may be less important in older age than in younger years. Convergence processes that happen over a long marriage may make gender less significant than in the early phases of relationships. Couples could become more similar over time because of shared environments, social networks, and accumulated understandings, making gender less significant in defining the ways in which they influence each other’s behaviors. Moreover, if the impetus to quit is tied to health shocks or worries about aging, then this is a more specific reason to quit than prevention and may be less gendered (Cross & Markus, 1991; Margolis, 2013b; Siegler et al., 1999).
This study has many strengths including its use of longitudinal and self-reported data from both partners, yet it does have some limitations. First, the data allow the examination of smoking changes between each interview, approximately every other year, but may not capture shorter-term changes and therefore may underestimate the amount of smoking change. Although the data may miss transient changes in smoking, they do capture longer-term changes that likely have greater effects on health. Second, this analysis focuses on smokers in middle and older age and does not capture whether respondents changed their behavior earlier in life. Prior research documents high rates of smoking cessation in the past for these cohorts (de Walque, 2010). Yet, this is the population at risk of smoking cessation in middle and older age and this behavior change is important for managing illness and promoting healthy aging. Third, we were not able to include information about relationship quality, which is likely an important factor in how partners’ health behaviors are related. The HRS asked questions that address relationship quality of a small pilot sample of 4,000 respondents in 2004. These questions have been posed to a rotating random 50% of respondents in subsequent waves. The 2010 wave is thus the first to provide longitudinal data from the 2006 participants (Smith et al., 2013). Future research should take advantage of these data to examine this aspect of the relationship context and its link to spousal health behavior changes. We expect that the health behaviors of partners in high-quality relationships would be even more sensitive to each other’s health behaviors and changes in these behaviors because these couples are likely to spend more time in a shared environment and to provide positive support and encouragement in attempts to quit smoking. Lastly, due to small subsamples we could not estimate precisely the risks of smoking changes among same-sex couples relative to heterosexual couples, or cohabiting relative to married couples but these topics can be explored with other data.
Our study makes four contributions to the research on partnership and health behaviors in older age. First, we provide further evidence that researchers should draw distinctions among partnered smokers based on their partner’s behavior. We show that the unpartnered display health behavior changes between those whose partners exhibit positive and negative behaviors. Past work that has found no differences between the partnered and unpartnered may be due to unmeasured differences in partnership characteristics. Data on partners are often unavailable which is one of the reasons why studies like ours are less common (Kravdal, 2008). An important advantage of having longitudinal data on the smoking behavior of both partners is that it allowed us to document the group with the highest odds of smoking cessation—those with partners who also quit. If this group had not been isolated, then it would bias upward the odds of cessation among the partnered group of smokers.
Second, we jointly examine health behavior changes by partnership status, health behaviors of the partnered by the partner’s behavior, and partnership transitions. Prior research has focused on one of these aspects at a time, but we show that there are meaningful comparisons to be made between the continuously unpartnered, those who experience a partnership change, and those who are partnered with different types of partners. A cross-sectional analysis would obscure all the differences between those who are partnered with smokers who quit, partners who relapse into smoking, those who are newly partnered, and those whose partners remain smokers or remain non-smokers. Grouping all those partnered at one point in time can lead to biased inferences about differences in health behaviors by partnership status. This study design can also be used to examine changes in other health behaviors, mental, or physical health.
Third, we focus on middle and older aged adults whereas other work has mostly focused on younger adults (Homish & Leonard, 2005; McBride et al., 1998; Pollak & Mullen, 1997; Woodby et al., 1999). The smoking behaviors of this age group are important because smoking cessation is recommended for treating many commonly diagnosed illnesses in older age (Lichtenstein et al., 2006) and because quitting smoking in older age can lead to living longer (Doll et al., 2004). Better understanding the correlates of smoking changes among this population will enhance health promotion programs.
Last, we examine smoking cessation and adherence controlling for demographic factors, health, and work, which are also associated with changes in smoking. Most past research has used smaller medical samples without many of these key controls. We are therefore able to compare the magnitude of differences by partnership and partner’s health behaviors with other factors that are important in middle and older age. Net of other factors, partnership context at the time of cessation strongly predicts longer term patterns of adherence and shapes health in older age.
Funding
This work was supported by the National Institutes of Health (NIA T32-AG000177, P30AG12836 and NICHD T32HD007242, R24HD044964); and the Social Sciences and Humanities Research Council of Canada.
Acknowledgments
We gratefully acknowledge Ingrid Connidis and the anonymous reviewers for valuable comments on a previous draft and the University of Michigan and RAND for making the HRS data accessible and clearly documented. R.M. planned the study, conducted the data analysis, and drafted the article. L.W. contributed to the writing and revising of the manuscript.
References
- Allison P. D. (1982). Discrete-time methods for the analysis of event histories. Sociological Methodology, 13, 61–98. http://dx.doi.org/10.2307/270718 [Google Scholar]
- Bove C. F., Sobal J., Rauschenbach B. S. (2003). Food choices among newly married couples: convergence, conflict, individualism, and projects. Appetite, 40, 25–41. doi:10.1016/S0195-6663(02)00147-2 [DOI] [PubMed] [Google Scholar]
- Carr D., & Springer K. W (2010). Advances in families and health research in the 21st century. Journal of Marriage and Family, 72, 743–761. DOI: 10.1111/j.1741-3737.2010.00728.x [Google Scholar]
- Carstensen L. L. (1992). Social and emotional patterns in adulthood: support for socioemotional selectivity theory. Psychology and Aging, 7, 331–338. http://dx.doi.org/10.1037//0882-7974.7.3.331 [DOI] [PubMed] [Google Scholar]
- Clark M. A. Rakowski W. Kviz F. J., & Hogan J.W (1997). Age and stage of readiness for smoking cessation. Journal of Gerontology: Social Sciences, 52B, S212–S221. http://dx.doi.org/10.1093/geronb/52b.4.s212 [DOI] [PubMed] [Google Scholar]
- Coppotelli H. C., Orleans C. T. (1985). Partner support and other determinants of smoking cessation maintenance among women. Journal of Consulting and Clinical Psychology, 53, 455–460. http://dx.doi.org/10.1037//0022-006x.53.4.455 [DOI] [PubMed] [Google Scholar]
- Cross S., & Markus H (1991). Possible selves across the life span. Human Development, 34, 230–255. http://dx.doi.org/10.1159/000277058 [Google Scholar]
- de Walque D. (2010). Education, information, and smoking decisions: Evidence from smoking histories in the United States, 1940–2000. Journal of Human Resources, 45, 682–717. http://dx.doi.org/10.1353/jhr.2010.0009 [Google Scholar]
- DeVault M. (1991). Feeding the family: The social construction of caring as gendered work. Chicago, IL: University of Chicago Press. [Google Scholar]
- Doll R. Peto R. Boreham J., & Sutherland I (2004). Mortality in relation to smoking: 50 years’ observations on male British doctors. British Medical Journal, 328, 1519 http://dx.doi.org/10.1136/bmj.38142.554479.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falba T. A., & Sindelar J. L (2008). Spousal concordance in health behavior change. Health Services Research, 43, 96–116. http://dx.doi.org/10.1111/j.1475-6773.2007.00754.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franks M. M., Pienta A. M., Wray L. A. (2002). It takes two: marriage and smoking cessation in the middle years. Journal of Aging and Health, 14, 336–354. http://dx.doi.org/10.1177/08964302014003002 [DOI] [PubMed] [Google Scholar]
- Fuller T. D. (2010). Relationship status, health, and health behavior: An examination of cohabiters and commuters. Sociological Perspectives, 53, 221–246. http://dx.doi.org/10.1525/sop.2010.53.2.221 [Google Scholar]
- Goldman N. (2001). Social inequalities in health disentangling the underlying mechanisms. Annals of the New York Academy of Sciences, 954, 118–139. http://dx.doi.org/10.1111/j.1749-6632.2001.tb02750.x [PubMed] [Google Scholar]
- Heeringa S. G., & Connor J. H (1995). Technical description of the health and retirement survey sample design. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf
- Homish G. G., Leonard K. E. (2005). Spousal influence on smoking behaviors in a US community sample of newly married couples. Social Science & Medicine, 61, 2557–2567. doi:10.1016/j.socscimed.2005.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L., Boulifard D. A., Contrada R. J. (2012). Mending broken hearts: marriage and survival following cardiac surgery. Journal of Health and Social Behavior, 53, 33–49. doi:10.1177/0022146511432342 [DOI] [PubMed] [Google Scholar]
- Kahn R. S., Certain L., Whitaker R. C. (2002). A reexamination of smoking before, during, and after pregnancy. American Journal of Public Health, 92, 1801–1808. http://dx.doi.org/10.2105/ajph.92.11.1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravdal O. (2008). A broader perspective on education and mortality: Are we influenced by other people’s education? Social Science & Medicine, 66, 620–636. http://dx.doi.org/10.1016/j.socscimed.2007.10.009 [DOI] [PubMed] [Google Scholar]
- Leonard K. E., & Mudar P (2003). Peer and partner drinking and the transition to marriage: a longitudinal examination of selection and influence processes. Psychology of Addictive Behaviors, 17, 115–125. http://dx.doi.org/10.1037/0893-164x.17.2.115 [DOI] [PubMed] [Google Scholar]
- Lichtenstein A. H. Appel L. J. Brands M. Carnethon M. Daniels S. Franch H. A., & Howard B (2006). Diet and lifestyle recommendations revision 2006. Circulation, 114, 82–96. http://dx.doi.org/10.1161/circulationaha.106.176158 [DOI] [PubMed] [Google Scholar]
- Liu H., & Umberson D. J (2008). The times they are a changin’: marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior, 49, 239–253. http://dx.doi.org/10.1177/002214650804900301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzoli L. Willari P. Pirone G. M., & Boccio A (2007). Marital status and mortality in the elderly: A systematic review and meta-analysis. Social Science & Medicine, 64, 77–94. http://dx.doi.org/10.1016/j.socscimed.2006.08.031 [DOI] [PubMed] [Google Scholar]
- Margolis R. (2013. a). Educational differences in healthy behavior changes and adherence among middle aged Americans. Journal of Health and Social Behavior, 54, 353–368. http://dx.doi.org/10.1177/0022146513489312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis R. (2013. b). Health shocks in the family: Gender differences in smoking changes. Journal of Aging and Health, 25, 882–903. http://dx.doi.org/10.1177/0898264313494411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride C. M., Curry S. J., Grothaus L. C., Nelson J. C., Lando H., Pirie P. L. (1998). Partner smoking status and pregnant smoker’s perceptions of support for and likelihood of smoking cessation. Health Psychology, 17, 63–69. http://dx.doi.org/10.1037//0278-6133.17.1.63 [DOI] [PubMed] [Google Scholar]
- Mermelstein R., Cohen S., Lichtenstein E., Baer J. S., Kamarck T. (1986). Social support and smoking cessation and maintenance. Journal of Consulting and Clinical Psychology, 54, 447–453. http://dx.doi.org/10.1037/0022-006x.54.4.447 [DOI] [PubMed] [Google Scholar]
- Meyler D. Stimpson J. P., & Peek M. K (2007). Health concordance within couples: A systematic review. Social Science & Medicine, 64, 2297–2310. http://dx.doi.org/10.1016/j.socscimed.2007.02.007 [DOI] [PubMed] [Google Scholar]
- Monden C. W., van Lenthe F., de Graaf N. D., Kraaykamp G. (2003). Partner’s and own education: does who you live with matter for self-assessed health, smoking and excessive alcohol consumption? Social Science & Medicine, 57, 1901–1912. http://dx.doi.org/10.1016/s0277-9536(03)00055-8 [DOI] [PubMed] [Google Scholar]
- Orleans T. C. (2000). Promoting the maintenance of behavior change: Recommendations for the next generation of research and practice. Health Psychology, 19, 76–83. http://dx.doi.org/10.1037/0278-6133.19.suppl1.76 [DOI] [PubMed] [Google Scholar]
- Pollak K. I., & Mullen P. D (1997). An exploration of the effects of partner smoking, type of social support, and stress on postpartum smoking in married women who stopped smoking during pregnancy. Psychology of Addictive Behaviors, 11, 182–189. http://dx.doi.org/10.1037//0893-164x.11.3.182 [Google Scholar]
- Reczek C. (2012). The promotion of unhealthy habits in gay, lesbian, and straight intimate partnerships. Social Science & Medicine, 75, 1114–1121. doi:10.1016/j.socscimed.2012.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek C., & Umberson D (2012). Gender, health behavior, and intimate relationships: lesbian, gay, and straight contexts. Social Science & Medicine, 74, 1783–1790. http://dx.doi.org/10.1016/j.socscimed.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler J. C. Kaplan B. H. Von Dras D. D., & Mark D. B (1999). Cardiovascular health: A challenge for midlife. In Willis S.L., Reid J.D. (Eds.), Life in the middle: Psychological and social development in middle age (pp.148–160). San Diego, CA: Academic Press; http://dx.doi.org/10.1016/b978-012757230-7/50026-2 [Google Scholar]
- Smith J. Fisher G. Ryan L. Clarke P. House J., & Weir D (2013). Psychosocial and lifestyle questionnaire 2006–2010 documentation report core section LB. Institute for Social Research.
- Umberson D. (1987). Family status and health behaviors: social control as a dimension of social integration. Journal of Health and Social Behavior, 28, 306–319. http://dx.doi.org/10.2307/2136848 [PubMed] [Google Scholar]
- Umberson D. (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine, 34, 907–917. http://dx.doi.org/10.1016/0277-9536(92)90259-s [DOI] [PubMed] [Google Scholar]
- Williams K., Umberson D. (2004). Marital status, marital transitions, and health: a gendered life course perspective. Journal of Health and Social Behavior, 45, 81–98. http://dx.doi.org/10.1177/002214650404500106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodby L. L. Windsor R. A. Snyder S. W. Kohler C. L., & Diclemente C. C (1999). Predictors of smoking cessation during pregnancy. Addiction, 94, 283–292. http://dx.doi.org/10.1046/j.1360-0443.1999.94228311.x [DOI] [PubMed] [Google Scholar]
- York Cornwell E., & Waite L. J (2012). Social network resources and management of hypertension. Journal of Health and Social Behavior, 53, 215–231. http://dx.doi.org/10.1177/0022146512446832 [DOI] [PMC free article] [PubMed] [Google Scholar]