Abstract
Objectives:
Most older adults prefer to “age in place” and avoid formal long-term care. Yet demographic shifts, including population aging and an increasing prevalence of remarried and unmarried older adults, could undermine these goals, making it important to consider carefully how and why relationship status relates to long-term care risk.
Method:
We fit hazard models to a sample of adults aged 65 and older from eight waves (1998–2012) of the Health and Retirement Study (N = 21,564). We consider risk of any long-term care facility admission, as well as risk of long-duration stays.
Results:
Widowed, divorced, and never married adults have the highest risks of long-term care admission. Remarried and partnered adults have similar risks of long-term care admission as continuously married adults. Relationship status is more important for men than for women, especially when considering long-duration stays. Relationship status is also more significant for non-Hispanic White and Hispanic adults compared with non-Hispanic Black adults. Economic resources and, to some extent, social ties partially explain the association between relationship status and long-term care use.
Discussion:
By addressing the prohibitive costs of long-term care services which enable aging in place (e.g., home health care), relationship status disparities in long-term care may be reduced. Future studies should consider the link between long-term care facility use and relationship status in future cohorts as well as examine how relationship status structures access to a range of long-term care options.
Keywords: Family sociology, Gender, Health services use, Longitudinal methods, Long-term care, Minority aging (race and Hispanic ethnicity)
About 2.1 million Americans currently reside in long-term care facilities, defined as overnight facilities, including nursing homes and residential care communities, which provide a broad range of health care, personal care, and supportive services for adults who have limited self-care capabilities (Harris-Kojetin, Sengupta, Park-Lee, & Valverde, 2013). Fifty percent of male residents and 39% of female residents reside in long-term care facilities for longer than 3 months (Friedberg, Wenliang, Sun, Webb, & Li, 2014). Yet long-term care facilities are not the first choice for most older Americans; even in the event of poor health, almost all would prefer to remain at home and in their community (Feldman, Oberlink, Simantov, & Gursen, 2004; Sergeant, Ekerdt, & Chapin, 2010). Correspondingly, recent policy initiatives have begun to promote home- and community-based services that would reduce the need for long-term care facilities (Carlson, Foster, Dale, & Brown, 2007). To support these initiatives, research needs to identify factors that shape long-term care facility use, especially for long durations.
Relationship status is associated with long-term care facility use, as married adults are half as likely to enter long-term care facilities as unmarried adults (Freedman, 1996; Noël-Miller, 2010). Understandings of how relationship status influences entry into long-term care facilities are incomplete. Most previous studies on relationship status and long-term care facilities only compare currently married adults with currently unmarried adults, ignoring the heterogeneity within these two categories (Freedman, 1996; Himes, Wagner, Wolf, Aykan, & Dougherty, 2000). This approach is outdated given the new demographic reality that unmarried, remarried, and partnered older adult populations are growing in the United States (Lin & Brown, 2012). Twenty-nine percent of married adults are in second- or higher-order marriages (Kreider, 2006), and 4% of unmarried older adults are cohabiting (Brown, Lee, & Bulanda, 2006). Additionally, more older adults are divorced than in the past, and widowed and divorced adults are increasingly likely to remain single (Brown & Lin, 2012). The relative increase in remarriage and non-marital partnerships and overall decrease in marriage rates may undermine sources of support at older ages (Umberson & Montez, 2010). But as of yet, we do not fully know the implications of these relationship status trends on long-term care facility use. In this study, we move beyond binary comparisons of currently married adults and currently unmarried adults and provide a more nuanced examination of how long-term care risk varies across six relationship status categories: continuously married, remarried, partnered, widowed, divorced, and never married.
We also know little about the mechanisms linking relationship status to long-term care facility use. Three key predictors of long-term care admission are health and disability, economic resources, and social ties (Friedman, Steinwachs, Rathouz, Burton, & Mukamel, 2005). Further, relationship status is strongly associated with each of these predictors (Umberson & Montez, 2010). We propose as a conceptual model that differences between relationship status groups in these three predictors help explain differences in long-term care admission. Further, race/ethnicity and gender may moderate this association, as race/ethnicity and gender importantly shape relationship status experiences (Umberson et al., 2014) and risk of long-term care admission (Thomeer, Mudrazija, & Angel, 2015).
Conceptual Model of Diversity Across Relationship Statuses
Observed associations between relationship status and health, economic resources, and social ties reflect the complex interplay of marital benefits, dissolution strain, and selection factors throughout the life course. These likely translate into different risks of long-term care facility use across relationship status groups. Marriage is associated with better health, less disability, more financial resources, and more social integration, including a greater likelihood of children—an important source of support for older adults (Hughes & Waite, 2009; Wilmoth & Koso, 2002). The never married, who have never received benefits from marriage, report the lowest levels of household net worth and are the most likely to live alone and be childless (Pinquart, 2003; Wilmoth & Koso, 2002). Remarriage affords fewer benefits than first marriages, including lower marital quality, fewer health and financial benefits, and more strained relationships with children (Bulanda & Brown, 2007; Hughes & Waite, 2009; Kalmijn 2007; Wilmoth & Koso, 2002), reflecting remarriage’s status as an incomplete institution and the long-lasting influence of marital dissolution (Cherlin, 1978; Hughes & Waite, 2009).
Marriage benefits may extend to those in non-marital partnerships, including cohabitors and the living apart together (e.g., couples who have an intimate relationship but live at separate addresses; Levin, 2004). Partnered adults, like married adults, have an intimate partner committed to care for their health, share finances, and provide support (Musick & Bumpass, 2012). Partnered adults have fewer disabilities and chronic conditions and higher incomes and pensions than other unmarried adults (Brown et al., 2006; Zhang, 2006). At the same time, past research concludes that partnered adults report less relationship happiness, more psychological distress, more disabilities, and fewer caregiving benefits than married adults (Brown et al., 2006; Brown & Kawamura, 2010; Noël-Miller, 2011).
The perceived strain of marital dissolution, either through divorce or through spousal death, also shapes differential outcomes by relationship status. Marital dissolution contributes to worse health and disability, more financial hardship, and weaker social integration for remarried, divorced, widowed, and many partnered adults (Hughes & Waite, 2009; Kalmijn 2007; Wilmoth & Koso, 2002). The consequences of marital dissolution differ depending on whether the marital disruption is caused by divorce or spousal death (Liu & Umberson, 2008). In general, divorced adults are more economically disadvantaged than widowed adults (Kalmijn, 2007; Wilmoth & Koso, 2002), but widowed adults have worse health than divorced adults (Liu & Umberson, 2008). Remarried and divorced adults report less contact with their adult children than the continuously married, but widowhood, compared with divorce, increases adult children’s involvement and the likelihood of living with an adult child (Kalmijn, 2007; Lin & Brown, 2012). The never married have not experienced the strain of marital dissolution, and, in line with a marital strain hypothesis, some studies find similar health for never married adults and continuously married adults (Liu & Umberson, 2008; Williams & Umberson, 2004).
Health, social ties, and economic resources, in addition to being associated with different relationship statuses, also shape long-term care use. Poor health and disability often require specialized care and thus increase likelihood of long-term care facility use, especially for long durations (Mudrazija, Thomeer, & Angel, 2015). Economic disadvantage is also often associated with long-term care facility use, likely because those financially able to stay at home and receive alternative care choose to do so (Friedman et al., 2005). Social ties often serve as substitutes for formal care, reducing use of long-term care facilities (Charles & Sevak, 2005). We expect that health, social ties, and economic resources will help explain relationship status differences in long-term care facility use.
We further expect relationship status differences to be pronounced when considering longer durations of long-term care stays. People enter long-term care facilities for a variety of reasons, including short-duration rehabilitation following surgery and long-duration stays for daily medical and custodial care (Mudrazija et al., 2015). Short-duration stays may be less avoidable than long-duration stays because they more often involve specialized and intensive care which is difficult to provide in a home setting. Thus, we anticipate that relationship status will be more strongly associated with long-duration compared with short-duration stays.
Potential Differences by Gender and Race/Ethnicity
Long-term care facility use and relationship status are strongly patterned by gender and race/ethnicity. Women and non-Hispanic White adults are more likely to enter long-term care facilities than men and racial/ethnic minorities, such that 68% of long-term care facility residents are women and 79% are non-Hispanic White adults (Harris-Kojetin et al., 2013). These racial/ethnic differences persist despite non-Hispanic Black and Hispanic adults’ worse overall health and physical functioning (Thomeer et al., 2015). Regarding relationship status, among adults aged 65 and older, 73% of men are currently married compared with only 47% of women, and this gap increases with age (U.S. Census, 2015). Only 39% of non-Hispanic Black adults aged 65 and older, compared with 54% of Hispanic adults and 61% of non-Hispanic White adults, are currently married (U.S. Census, 2015). Just as long-term care facility use and relationship status vary by gender and race/ethnicity, we hypothesize that the association between long-term care use and relationship status as well as the mechanisms connecting relationship status to long-term care use will also vary by gender and race/ethnicity. Regarding gender, research using dichotomous measures of relationship status finds that marriage protects men from long-term care facility use more than women (Freedman, 1996; Noël-Miller, 2010). Regarding race/ethnicity, two recent studies conclude that marriage is protective for non-Hispanic White and Hispanic adults but not for non-Hispanic Black adults (Akamigbo & Wolinsky, 2007; Thomeer et al., 2015).
Method
We employ data from the Health and Retirement Study (HRS), a nationally representative biennial survey of persons aged 51 years and older, first interviewed in 1992 (Juster & Suzman, 1995). The HRS’s panel survey design allows us to examine risk of long-term care admission over an extended period of time in the midst of marital, health, economic, and social changes. For this study, we draw on eight waves of the HRS (1998–2012). In line with past studies (Freedman, 1996; Thomeer et al., 2015) and due to the lower rate of long-term care facility use among those younger than 65 years (Rogers & Komisar, 2003), we limit the analytic sample to age 65 and older. We exclude respondents who resided in a long-term care facility in the waves prior to 1998 or before age 65 (n = 553). The final sample size is 21,564.
Measurements
Long-term Care Facility Admission
We consider first long-term care facility admission as previous research suggests that the timing of first long-term care facility admission is important in marking the start of a person’s reliance on the formal long-term care system (Freedman, 1996). Respondents are asked whether, in the last 2 years, they have been a patient overnight in a nursing home, convalescent home, or other long-term health care facility. We construct a measure of age at first long-term care facility admission, subtracting the year and month of long-term care facility admission from the respondent’s birth year and month. We also construct a measure of length of stay, subtracting the year and month of long-term care facility admission from the year and month of long-term care facility discharge or death, and we separately examine risk of any long-term care facility admission and risk of long-term care facility use for 3 months or longer.
Intimate Relationship Status
The primary explanatory variable is relationship status, which is comprised of the following categories: continuously married, remarried, partnered, divorced/separated, widowed, and never married. Relationship status is measured at each wave. For partnered, respondents are asked, “Are you living with a partner as if married?” Thirteen percent of those who report being partnered are not currently living with someone else, indicating that some respondents do not interpret the question as meaning that they share a primary residence with their partner. Supplementary analysis reveals no significant differences in risk of long-term care admission between those who are partnered and living alone and those who live with their partner, so we consider them as one group. Because only 5% of partnered adults in both categories entered a long-term care facility, these results are only preliminary and future analysis should consider more carefully the differences between these two groups. Because a small number of partnered adults were in long-term care facilities for 3 months or longer, when examining only long-duration stays, we consider marital status (i.e., continuously married, remarried, divorced, widowed, and never married) but not partnership status.
Health and Disability
Health and disability measures include number of chronic conditions, number of reported difficulties with activities of daily living (ADL), and number of reported difficulties with instrumental activities of daily living (IADL). The number of chronic conditions is the sum of nine conditions, namely hypertension, diabetes, cancer, lung disease, heart disease, stroke, psychiatric problems, arthritis, and incontinence. The ADL difficulty score, ranging from 0 to 5, is the number of ADLs the respondent reports having some difficulties with (i.e., bathing, eating, dressing, walking across a room, and getting in or out of bed). The IADL score, ranging from 0 to 5, refers to the number of IADLs the respondent reports having some difficulties with (i.e., using a telephone, taking medication, handling money, shopping, and preparing meals).
Economic Resources
Economic resources include home ownership, Medicaid participation, and total nonhousing net worth. Homeownership and Medicaid coverage are coded as dichotomous variables. Total nonhousing net worth is the sum of household nonhousing asset amounts minus total debt, partitioned into four quartiles. We use the net worth imputations provided by the RAND HRS data file (RAND HRS Data, 2012).
Social Ties
Social ties include number of people in household, number of living children, any living siblings, nonspousal help and help availability, and contact with neighbors. Number of people in household and number of living children are count variables. Any living siblings is a dichotomous variable. For the nonspousal help variable, respondents are asked “Suppose in the future, you needed help with basic personal care activities like eating or dressing. Do you have relatives or friends (besides your husband/wife/ partner) who would be willing and able to help you over a long period of time?” Respondents currently receiving nonspousal help are not asked this question. We code three categories: no future nonspousal help (or don’t know), has future nonspousal help, or currently using nonspousal help. Contact with neighbors is a continuous variable, measured as how many times per month the respondent gets together with any neighbors for a social visit or chat.
Controls
Other variables include gender (man or woman), year of birth, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other, including American Indian, Alaskan Native, Asian, and Pacific Islander), and educational attainment (less than high school, high school degree or high school equivalency credential, some college or associate’s degree, and Bachelor’s degree or higher). We include year of birth rather than age, because age is the analysis time for the hazard models. Year of birth serves as a modest control for cohort.
Regarding missing data, 11.7% of respondents are missing information for one or more variables. We exclude respondents missing information on relationship status (n = 35), as this is our key variable of interest. For the remaining missing data, we use Imputation by Chained Equations (ICE) procedure for multiple imputation to generate five data sets (Royston, 2004). Respondents missing data on educational attainment, Medicaid participation, and number of chronic conditions are more likely to enter nursing homes and those missing information on future help availability are less likely. Respondents missing data on the other variables do not differ significantly in their risk of long-term care admission compared with those who do not have any missing data.
Analysis
To assess the risk of long-term care facility use, we begin with weighted descriptive statistics of individuals at baseline. We then use statistical difference tests to compare continuously married adults to other relationship statuses (remarried, partnered, widowed, divorced/separated, and never married) and women and men within each relationship status. We fit event history models—specifically Cox proportional hazard regression models—with time to first long-term care admission as the dependent variable. We repeat these models using time to first long-term care admission with a 3 month or longer stay as the dependent variable. The Cox regression models are appropriate to use when time dependence in the baseline hazard is unknown (Vuchinich, Teachman, & Crosby, 1991). Because risk of long-term care increases with age and relationship status is also linked to age (e.g., widowhood prevalence increases with age), we use age, rather than year, as our analytic unit of time. This allows us to focus on the likelihood of entering a long-term care facility at each age, which is more substantively significant than focusing on specific years. Respondents who do not enter a long-term care facility by the end of the study (n = 14,494) or die before the end of the study without entering a long-term care facility (n = 3,795) are right-censored. When considering only risk of long-duration stays, we also right-censor those with only short-duration stays (n = 1,473). We report hazard ratios which are exponentiated coefficients: A hazard ratio greater than one indicates an increasing risk of long-term care facility admission for a one-unit increase in the independent variable at any event time whereas less than one indicates a decreasing risk.
Relationship status and health and disability, economic resource, and social tie variables are time dependent, observed, and recorded at each age. These variables can change across time points, and the event history models take these changes into account. Transitions (e.g., from divorced to remarried, from two ADL difficulties to three ADL difficulties) that occur after entry into long-term care facilities are not included in these models but are only adjusted for if they occur before long-term care admission or to respondents who do not enter a long-term care facility during the study period. For birth year, gender, race/ethnicity, and educational attainment, we only include baseline values.
We estimate five models. Supplementary analysis reveals many statistically significant interactions between gender and other variables, including relationship status variables, so we stratify models by gender. Below we specifically detail which Relationship status * Gender two-way interactions are significant in the supplementary analysis. The coefficients for these statistically significant interaction terms range in size from 0.67 to 0.83, and tables including these interactions are available from the authors upon request. In the baseline model, we include relationship status, birth year, gender, race/ethnicity, and educational attainment. We add health and disability variables to the baseline model in the second model, economic resources to the baseline model in the third model, and social ties to the baseline model in the fourth model. In the fifth model, we include all variables. To test for moderation by race/ethnicity, we interact each relationship status variable with each race/ethnicity category. We test this using the full sample, not the sample stratified by gender nor the sample limited to long-duration stays, in order to maintain statistical power.
Results
Descriptive Statistics
In our sample, 3,275 respondents enter a long-term care facility during the study period (15.2%) and 1,802 enter a long-term care facility for 3 months or longer (8.4%). More women (18.8%) than men (11.9%) use long-term care facilities. As shown in Table 1, regarding any long-term care facility stay, a higher percentage of widowed women and men use long-term care facilities than any other group, with never married adults holding the second highest rate. Partnered adults have the lowest percentage entering the long-term care facility for both men and women. Long-term care facility stays 3 months or longer have similar rankings. Overall, these descriptive statistics suggest no statistical difference in long-term care facility use between partnered, continuously married, and remarried adults.
Table 1.
Descriptive Statistics at Baseline, Health and Retirement Study, 1998–2012 (N = 21,564)
| Continuously married | Remarried | Partnered | Divorced/separated | Widowed | Never married | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 4,870 men; 3,721 women) | (n = 2,125 men; 1,278 women) | (n = 252 men; 143 women) | (n = 731 men; 1,241 women) | (n = 1,271 men; 5,223 women) | (n = 309 men; 400 women) | |||||||
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| Entered nursing home | 0.07 | 0.08** | 0.06 | 0.07** | 0.05 | 0.05 | 0.10* | 0.14* | 0.18* | 0.23* | 0.12* | 0.16* |
| Nursing home stay > 3 monthsa | 0.02 | 0.03** | 0.02 | 0.03** | — | — | 0.06* | 0.05* | 0.10* | 0.14* | 0.07* | 0.10* |
| Sociodemographics | ||||||||||||
| Birth year | 1930 | 1931** | 1931* | 1932*,** | 1934* | 1935* | 1934* | 1933*,** | 1923* | 1924* | 1932* | 1929*,** |
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | 0.87 | 0.87 | 0.84* | 0.89** | 0.81* | 0.82* | 0.70* | 0.73* | 0.83* | 0.82* | 0.83 | 0.71*,** |
| Non-Hispanic Black | 0.05 | 0.05 | 0.08* | 0.06** | 0.10* | 0.08* | 0.17* | 0.16* | 0.11* | 0.11* | 0.12* | 0.16* |
| Hispanic | 0.06 | 0.06 | 0.05 | 0.03*,** | 0.07 | 0.08 | 0.11* | 0.09* | 0.04* | 0.05** | 0.04 | 0.09*,** |
| Other | 0.02 | 0.02 | 0.03 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.01 | 0.04*,** |
| Educational attainment | ||||||||||||
| Less than high school | 0.25 | 0.19** | 0.22 | 0.21 | 0.25 | 0.25 | 0.28 | 0.25* | 0.36* | 0.35* | 0.28 | 0.24* |
| High school | 0.38 | 0.49** | 0.39 | 0.49** | 0.35 | 0.45** | 0.41 | 0.44* | 0.39 | 0.44*,** | 0.33 | 0.38* |
| Some college or associate’s degree | 0.11 | 0.14** | 0.13* | 0.15 | 0.16* | 0.09*,** | 0.14 | 0.14 | 0.11 | 0.11* | 0.15 | 0.13 |
| Bachelor’s degree or more | 0.26 | 0.18** | 0.26 | 0.15*,** | 0.24 | 0.21** | 0.17* | 0.17 | 0.14* | 0.10*,** | 0.24 | 0.25* |
| Health and disability | ||||||||||||
| Number of chronic conditions | 2.23 | 2.25 | 2.31 | 2.48*,** | 2.26 | 2.74*,** | 2.33 | 2.76*,** | 2.48* | 2.63*,** | 2.29 | 2.42* |
| ADL difficulties | 0.28 | 0.29 | 0.30 | 0.33 | 0.24 | 0.30 | 0.42* | 0.50* | 0.60* | 0.69*,** | 0.35 | 0.49*,** |
| IADL difficulties | 0.27 | 0.27 | 0.27 | 0.28 | 0.16* | 0.24 | 0.37* | 0.42* | 0.58* | 0.71*,** | 0.37 | 0.46* |
| Economic resources | ||||||||||||
| Medicaid | 0.04 | 0.04 | 0.05 | 0.04 | 0.08* | 0.16*,** | 0.15* | 0.21*,** | 0.10* | 0.14*,** | 0.16* | 0.20* |
| Nonhousing net worth ($10,000s) | 42.57 | 44.05 | 37.75 | 37.79 | 35.60 | 34.70 | 27.84* | 13.04*,** | 22.71* | 14.09*,** | 35.08 | 14.77* |
| Own house | 0.91 | 0.91 | 0.89* | 0.89 | 0.81* | 0.84* | 0.56* | 0.57* | 0.67* | 0.65* | 0.64* | 0.54*,** |
| Social ties | ||||||||||||
| Number in household | 2.30 | 2.26** | 2.29 | 2.21*,** | 2.20* | 2.16* | 1.38* | 1.58*,** | 1.52* | 1.56* | 1.37* | 1.51* |
| Number of living children | 2.95 | 2.99 | 4.47* | 4.39* | 4.10* | 3.98* | 3.14* | 2.87** | 2.98 | 3.03 | 0.24 | 0.55** |
| No future help available or don’t know | 0.37 | 0.37 | 0.40* | 0.33*,** | 0.44* | 0.35** | 0.35 | 0.31* | 0.28* | 0.26* | 0.39 | 0.39 |
| Future help available | 0.51 | 0.51 | 0.47* | 0.55*,** | 0.46* | 0.51 | 0.52 | 0.52 | 0.49 | 0.46*,** | 0.48 | 0.43* |
| Currently using help | 0.12 | 0.12 | 0.13 | 0.12 | 0.10 | 0.14 | 0.13 | 0.17*,** | 0.23* | 0.28*,** | 0.13 | 0.18* |
| Any living siblings | 0.82 | 0.82 | 0.81 | 0.80 | 0.82 | 0.83 | 0.84 | 0.81 | 0.74* | 0.73* | 0.85 | 0.74*,** |
| Monthly contact with neighbors | 8.13 | 7.77** | 8.24 | 8.20 | 7.69 | 7.39 | 11.95* | 9.32*,** | 10.78* | 10.35* | 11.70* | 11.56* |
Notes: ADL = activities of daily living; IADL = instrumental activities of daily living.
aIn the analysis of nursing home stays 3 months or longer, partnered adults were categorized as either divorced, widowed, or never married. In this analysis, there were 811 divorced men, 1,267 divorced women, 1,410 widowed men, 5,332 widowed women, 342 never married men, and 408 never married women.
*Statistically different from continuously married (same gender): p < .05. ,**Statistically different from men: p < .05; Descriptive statistics are weighted.
Risk of Any Long-Term Care Use During Study Period
The baseline models are presented in Model 1 in Table 2 for men and in Table 3 for women. For both men and women, divorced, widowed, and never married adults have statistically significant higher hazards of long-term care admission compared with continuously married adults, whereas partnered and remarried adults report a similar level of risk of nursing home admission as continuously married adults. The difference between continuously married adults and unmarried adults appears larger for men than for women, although supplementary interaction analysis supports that these gender differences are only statistically significant for divorced adults. Among both men and women, the never married have the highest risk for any long-term care use, and divorced and never married men have more than twice the risk of long-term care admission as continuously married men.
Table 2.
Hazard Ratios for Entry Into Nursing Home, Health and Retirement Study 1998–2012 (Men only: N = 9,558)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| HR | HR | HR | HR | HR | |
| Union status | |||||
| Continuously married (ref) | |||||
| Remarried | 1.06 | 1.00 | 1.02 | 1.06 | 1.03 |
| Partnered | 1.00 | 1.17 | 0.88 | 1.13 | 1.17 |
| Divorced/separated | 2.26*** | 2.15*** | 1.47** | 2.01*** | 1.47** |
| Widowed | 1.83*** | 1.65*** | 1.46*** | 1.61*** | 1.29** |
| Never married | 2.54*** | 2.50*** | 1.74** | 2.26*** | 1.68** |
| Sociodemographics | |||||
| Birth year | 1.09*** | 1.07*** | 1.09*** | 1.07*** | 1.07*** |
| Race/ethnicity | |||||
| Non-Hispanic White (ref) | |||||
| Non-Hispanic Black | 1.00 | 0.85 | 0.73** | 0.98 | 0.88 |
| Hispanic | 0.74* | 0.61*** | 0.43*** | 0.74* | 0.63** |
| Other | 0.80 | 0.55* | 0.50** | 0.79 | 0.53* |
| Educational attainment | |||||
| Less than high school (ref) | |||||
| High school | 0.91 | 1.15 | 1.10 | 1.12 | 1.22* |
| Some college or associate’s degree | 0.94 | 1.34** | 1.17 | 1.28* | 1.47*** |
| Bachelor’s degree or more | 0.77** | 1.21* | 1.00 | 1.08 | 1.29* |
| Health and disability | |||||
| Number of chronic conditions | 1.17*** | 1.14*** | |||
| ADL difficulties | 1.43*** | 1.32*** | |||
| IADL difficulties | 1.30*** | 1.15*** | |||
| Economic resources | |||||
| Medicaid | 2.22*** | 1.44*** | |||
| Nonhousing net worth quartiles | |||||
| First (ref) | |||||
| Second | 0.74** | 1.07 | |||
| Third | 0.66*** | 1.03 | |||
| Fourth | 0.67*** | 1.13 | |||
| Own house | 0.58*** | 0.69*** | |||
| Social ties | |||||
| Number in household | 0.85*** | 0.82*** | |||
| Number of living children | 0.98 | 0.97 | |||
| No future help available or don’t know (ref) | |||||
| Future help available | 0.88 | 0.95 | |||
| Already using help | 7.44*** | 2.92*** | |||
| Any living siblings | 0.92 | 0.94 | |||
| Monthly contact with neighbors | 1.00 | 1.01* | |||
| Log likelihood | −7,690.73 | −7,063.07 | −7,532.51 | −7,077.78 | −6,859.88 |
Notes: ADL = activities of daily living; HR = hazard ratio; IADL = instrumental activities of daily living.
*p < .05. **p < .01. ***p < .001.
Table 3.
Hazard Ratios for Entry Into Nursing Home, Health and Retirement Study 1998–2012 (Women only; N = 12,006)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| HR | HR | HR | HR | HR | |
| Union status | |||||
| Continuously married (ref) | |||||
| Remarried | 0.96 | 0.97 | 0.95 | 1.05 | 1.01 |
| Partnered | 0.99 | 1.05 | 0.86 | 0.97 | 0.95 |
| Divorced/separated | 1.77*** | 1.62*** | 1.13 | 1.48*** | 1.09 |
| Widowed | 1.59*** | 1.45*** | 1.26*** | 1.36*** | 1.09 |
| Never married | 1.88*** | 1.83*** | 1.26 | 1.58*** | 1.19 |
| Sociodemographics | |||||
| Birth year | 1.09*** | 1.08*** | 1.09*** | 1.09*** | 1.08*** |
| Race/ethnicity | |||||
| Non-Hispanic White (ref) | |||||
| Non-Hispanic Black | 0.77*** | 0.62*** | 0.59*** | 0.70*** | 0.64*** |
| Hispanic | 0.56*** | 0.44*** | 0.35*** | 0.54*** | 0.45*** |
| Other | 0.78 | 0.72 | 0.56** | 0.69* | 0.70* |
| Educational attainment | |||||
| Less than high school (ref) | |||||
| High school | 0.84*** | 1.11* | 1.06 | 1.03 | 1.19** |
| Some college or associate’s degree | 0.79** | 1.09 | 1.10 | 1.03 | 1.23** |
| Bachelor’s degree or more | 0.85* | 1.20* | 1.24** | 1.10 | 1.36*** |
| Health and disability | |||||
| Number of chronic conditions | 1.15*** | 1.11*** | |||
| ADL difficulties | 1.31*** | 1.23*** | |||
| IADL difficulties | 1.36*** | 1.19*** | |||
| Economic resources | |||||
| Medicaid | 2.17*** | 1.31*** | |||
| Nonhousing net worth quartiles | |||||
| First (ref) | |||||
| Second | 0.76*** | 0.94 | |||
| Third | 0.79*** | 1.01 | |||
| Fourth | 0.73*** | 0.95 | |||
| Own house | 0.58*** | 0.73*** | |||
| Social ties | |||||
| Number in household | 0.81*** | 0.78*** | |||
| Number of living children | 0.97** | 0.96** | |||
| No future help available or don’t know (ref) | |||||
| Future help available | 0.81** | 0.88 | |||
| Already using help | 6.97*** | 2.79*** | |||
| Any living siblings | 0.92 | 0.95 | |||
| Monthly contact with neighbors | 1.01* | 1.01** | |||
| Log likelihood | −15,762.63 | −14,700.47 | −15,428.96 | −14,658.17 | −14,310.89 |
Notes: ADL = activities of daily living; HR = hazard ratio; IADL = instrumental activities of daily living.
*p < .05. **p < .01. ***p < .001.
In Model 2, we consider the health and disability variables. As in the baseline model, divorced, widowed, and never married adults are significantly more likely to enter long-term care facilities than continuously married adults. Adjusting for health and disability variables only modestly adjusts the differences in risk of long-term care admission for women or men. Supplementary interaction analysis indicates that the gap between continuously married adults and divorced and widowed adults is larger for men than for women.
Once economic resources are included in the models (Model 3), divorced and never married women have similar risks of long-term care admission as continuously married women, indicating that lower economic resources among divorced and never married women compared with continuously married women account for their greater long-term care risk. Widowed women have a 26% greater risk of long-term care use than continuously married women, even taking widowed women’s fewer economic resources into account. For men, including economic resources in the model contributes to widowed and divorced men exhibiting similar risks of long-term care admission, which is not the case in earlier models. Widowed, divorced, and never married men are still more likely to enter long-term care facilities than continuously married men, with never married men possessing the highest risk. Supplementary interaction analysis confirms that relationship status differences are statistically more pronounced for men than for women for all three unmarried groups.
Concerning social tie variables (Model 4), for women, but not for men, number of living children, having nonspousal help available, and monthly contact with neighbors decrease the risk of long-term care facility use. For both women and men, social ties partially explain the relationship between relationship status and risk of long-term care admission. Supplementary interaction analysis indicates that the gap between continuously married adults and divorced and widowed adults is significantly larger for men than for women. Finally, in the full model (Model 5), for men, relationship status differences are reduced after adjusting for health and disability, economic resources, and social ties, but never married, widowed, and divorced men still have a statistically higher risk of long-term care admission than continuously married men at 8%, 29%, and 47%, respectively. For women, controlling for health and disability, economic resources, and social ties reduces the differences between continuously married adults and divorced, widowed, and never married women adults to nonsignificance. Supplementary interaction analysis indicates that the gap between continuously married adults and divorced and widowed adults is larger for men than for women.
Risk of Long Duration of Stay in Long-Term Care Facility
Table 4 shows risk of long-term care use for 3 months or longer (i.e., long-duration stays). Supplementary interaction analysis demonstrates that men’s relationship status is statistically more strongly related to risk of long-duration stays than women’s relationship status for all relationship statuses with the exception of widowhood in Model 1. For both men and women across most models, the never married have the highest risk of long-duration stays. Across all models, divorced men have a higher risk of long-duration stays than widowed men. Divorced and widowed women have similar risks of long-duration stays in most models, and economic resources appear to be more important in explaining divorced women’s risk of long-duration stays than widowed women’s. In the full model (Model 5), relationship status differences for women are fully explained, but divorced and never married men still have a greater risk of long-duration stay risk than continuously married adults at 52% and 96% higher risks, respectively.
Table 4.
Hazard Ratios for Entry Into Nursing Home for Greater Than 3 Months, Health and Retirement Study 1998–2012
| (Men and Women; N = 21,564) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
| Baseline | Health and disability | Socioeconomic resources | Family and social ties | Full | ||||||
| HR | HR | HR | HR | HR | ||||||
| Union status | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women |
| Continuously married (ref) | ||||||||||
| Remarried | 1.07 | 1.00 | 1.02 | 1.00 | 1.03 | 0.98 | 1.06 | 1.11 | 1.04 | 1.04 |
| Divorced/separated | 3.29*** | 1.62*** | 3.16*** | 1.51** | 1.94*** | 0.92 | 2.20*** | 1.18 | 1.52* | 0.85 |
| Widowed | 2.27*** | 1.66*** | 2.09*** | 1.53*** | 1.66*** | 1.21* | 1.51** | 1.25* | 1.18 | 0.96 |
| Never married | 4.01*** | 2.32*** | 3.86*** | 2.21*** | 2.25*** | 1.38 | 2.92*** | 1.68** | 1.96** | 1.19 |
| Log likelihood | −3,833.42 | −8,562.51 | −3,327.46 | −7,669.12 | −3,668.02 | −8,241.34 | −3,249.04 | −7,566.06 | −3,094.26 | −7,262.10 |
Notes: ADL = activities of daily living; HR = hazard ratio; IADL = instrumental activities of daily living.
* p < .05. ** p < .01. ***p < .001; adjusted for birth year, race/ethnicity, educational attainment, number of chronic conditions, ADL and IADL difficulties, Medicaid, nonhouse net worth, homeownership, number in household, number of living children, future help availability, any living siblings, and contact with neighbors.
Moderation by Race/Ethnicity
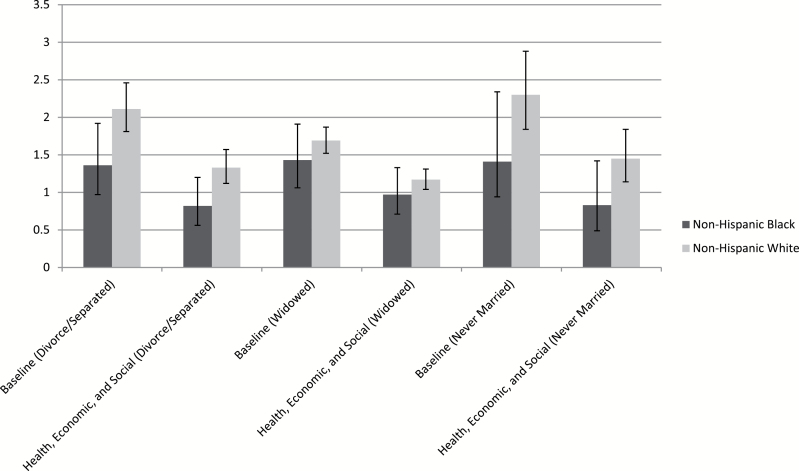
Moderation analysis for race/ethnicity differences indicate that relationship status is less important for non-Hispanic Black adults than for non-Hispanic White adults, but there are no significant differences between non-Hispanic White adults and Hispanic adults. Specifically, being never married or divorced does not increase the risk of long-term care use for non-Hispanic Black adults when compared with being continuously married, whereas these relationship statuses do increase the risk of long-term care use for non-Hispanic White adults. Additionally, the difference in risk of long-term care admission for widowed respondents compared with continuously married respondents is significantly smaller for non-Hispanic Black adults than for non-Hispanic White adults. The hazard ratios for divorced, widowed, and never married adults, relative to continuously married adults, are shown in Figure 1 for non-Hispanic Black adults and non-Hispanic White adults.
Figure 1.
Hazard ratio and confidence intervals for divorced/separated, widowed, and never married stratified by race (Non-Hispanic Black and Non-Hispanic White); Health and Retirement Study, 1998–2012 (n = 8,353; Reference is continuously married).
Discussion
As demonstrated in prior studies of intimate relationship status and health (Brown et al., 2006; Hughes & Waite, 2009; Kalmijn, 2007; Wilmoth & Koso, 2002), married adults and unmarried adults are heterogeneous groups. In the present study, we acknowledge this diversity to better predict and understand long-term care facility use, considering not only how relationship statuses differentially structure long-term care admission but also the risk factors that undergird these differences and how the importance of these risk factors differs by gender, race/ethnicity, and length of stay. This project is especially critical in light of the fact that most older adults prefer to “age in place” and avoid placement in long-term care facilities, an aim supported by governmental agencies concerned with the increasing cost of long-term care facilities (Feldman et al., 2004).
As in past research (Freedman, 1996; Himes et al., 2000), we confirm that continuously married adults are less likely than unmarried adults to enter long-term care facilities, demonstrating the salience of marriage in protecting against long-term care facility use. We extend prior research by offering three important caveats to this finding. First, we demonstrate that those in non-marital partnerships and remarriages have similar likelihoods as continuously married adults of entering long-term care facilities, suggesting that it is not continuous marriage per se but rather the presence of an intimate partner that is protective and supportive in later life. While studies of younger adults and non-marital partnerships find that partnered adults are generally disadvantaged compared with married adults (Brown, 2000; Horwitz & White, 1998), our study supports recent studies that find that partnership and marriage provide similar benefits and resources at older ages (Brown & Kawamura, 2010; Musick & Bumpass, 2012). Regarding remarriage, Cherlin (1978) proposed several decades ago that remarriage is an incomplete institution, offering fewer benefits such as lower social support and fewer economic resources than continuous marriage. Our findings show that this may no longer be the case, at least with respect to remarried adults’ long-term care facility use. One possible reason for these shifts is that as non-marital unions and remarriages become more common, there is comparatively less selection into these statuses than previously.
Second, by disaggregating unmarried adults into partnered, widowed, divorced, and never married adults, we are able to see that of these groups, the never married are at the greatest risk of being admitted into a long-term care facility, suggesting that never married adults face the most obstacles to aging in place. Contemporary studies of health and relationship status find that the never married do not experience a morbidity disadvantage compared with those who are currently married whereas there is a morbidity disadvantage for divorced and widowed adults (Liu & Umberson, 2008; Zhang & Hayward, 2006). Our results suggest that this advantage does not extend to long-term care facility use, either because the never married never received the health, economic, and social benefits of marriage—including the social protection of having children—or due to unobserved selection factors. Further, among men, widowed adults exhibit a lower risk of long-term care admission compared with divorced adults, indicating that divorce may be more disruptive than widowhood, perhaps particularly in regard to economic resources which, as we find in this analysis, are the most important factors in explaining long-term care use differences.
Third, the degree to which relationship status is related to long-term care use is importantly moderated by gender and race/ethnicity. Confirming previous studies (Freedman, 1996; Noël-Miller, 2010), being unmarried places men at greater risk for long-term care use than women. By looking specifically at subgroups of married and unmarried adults, we demonstrate that these gender differences also exist at this more nuanced level. The gender differences are even more exaggerated when considering only long-duration stays, suggesting that men rely heavily on their spouse or partner to be able to remain in their own homes and communities long term. Building further on these studies, we demonstrate that divorced, widowed, and never married men’s greater risk of long-term care facility use is not fully explained by the health, economic, or social variables, thus indicating the need for future research to identify these pathways specific to unmarried men. We find that being married does not advantage non-Hispanic Black respondents relative to being unmarried in terms of nursing home use. This supports claims that marriage is less protective for Black adults than for White adults (Akamigbo & Wolinsky, 2007; Thomeer et al., 2015). This also suggests that kin (i.e., friends and family) and perhaps even non-marital partners serve as functional substitutes for marriage among unmarried non-Hispanic Black adults, whereas other racial and ethnic groups receive more informal support from a spouse than from other kin (Angel & Settersten, 2015; Silverstein & Wang, 2015).
In addition to developing long-term care risk portraits for each group, we also test three pathways linking relationship status to long-term care admission. Our models indicate that economic resources are most responsible for explaining the disparity in long-term care use between continuously married adults and unmarried adults, particularly for women. Economically advantaged older adults often choose to age in place, rather than in long-term care facilities (Friedman et al., 2005), and our study indicates that this option is perhaps more available to married adults than to other groups, with never married adults most disadvantaged. Married and partnered adults are better able to age in place also because they have their spouse or partner to rely on for support, indicating that financial resources are a necessary but not sufficient condition. Interventions which seek to improve widowed, never married, and divorced adults’ financial well-being and to reduce the cost of remaining in the community will likely also reduce the risk of long-term care use and promote aging in place for unmarried and unpartnered adults. For example, the Cash and Counseling program provides older adults with a monetary allowance, which reduces incidences of unmet need, and the Community First Choice option in the Affordable Care Act encourages states to provide home- and community-based services and supports to eligible adults (Carlson et al., 2007). Relationship status disparities in long-term care use and institutional bias in Medicaid long-term care policies can be reduced through programs which seek to expand Medicaid community-based waiver programs for older unmarried adults who are eligible for a long-term care facility but prefer to remain in the community. An important next step for research is to evaluate the impact of Medicaid’s rules allowing special income and asset protections to married couples but requiring non-married couples and unmarried adults to be impoverished before they are eligible for long-term care assistance (U.S. Department of Health and Human Services, 2005).
Limitations
This study’s unique contributions to understanding relationship status and long-term care use should be considered within the context of study limitations. Our study indicates that relationship status is associated with risk of long-term care admission over time and that this difference in long-term care use is statistically explained by differences in economic resources and social ties; however, this is not necessarily a story of causation. The observed relationship between relationship status and long-term care risk may be due to selection or other unobserved factors.
Additionally, older adults have multiple care options, including informal care from friends and family members, paid home or community care, and formal institutional care, and each option exists within a continuum of care, differing by type of support, intensity of support, and duration. Within formal care institutions, which we examine in this study, nursing homes are functionally very different from other long-term care facilities, such as assisted living facilities, and each type has distinct payment structures, client eligibility rules, and financing models, which likely influence access to and use of various long-term care options. Due to data limitations within the HRS, we do not examine the whole spectrum of long-term care options or differentiate between institutions. Researchers identify significant disparities in access to different types of long-term care options, such that the least healthy and most socioeconomic disadvantaged have the fewest options and are most likely to use nursing homes (Zimmerman et al., 2003). We expect that our findings regarding relationship status differences would be more pronounced if only considering nursing homes as unmarried adults likely have fewer long-term care options than married adults. Future studies should consider how relationship status shapes both the availability and use of different types of long-term care, including nursing homes, assisted living facilities, and in-home care. This research agenda is particularly important as assisted living facilities and in-home care become more popular, rates of nursing home use decline, and new options for long-term care are introduced to meet the demands of a growing older adult population (Spillman, Liu, & McGilliard, 2008).
Conclusion
As family structures continue to change, with more adults entering and exiting marriages and other relationships multiple times over the life course (Cherlin, 2010), it is increasingly important to use multiple categories of relationship status and to place these indicators carefully within their health, economic, and social contexts. We demonstrate that non-marital relationships and remarriage may offer protection to older adults similar to those provided by marriage. Specifically, within the context of long-term care, remarried and partnered adults seem to be as able as continuously married adults to avoid long-term care facilities and age in the community. Researchers should continue to examine the importance of remarriage and non-marital partnerships on later-life outcomes, a topic largely understudied despite its demographic prevalence. Our study also draws attention to the vulnerability of divorced, widowed, and never married older adults whose economic disadvantages and, to a lesser extent, social isolation may decrease their ability to age in place.
The host of issues confronted here are critical as state and federal governments face the so-called “silver tsunami” being generated by aging Baby Boomers and will continue to be important with the aging of even newer cohorts. The Baby Boomer cohort has less access to traditional informal caregivers (e.g., children and spouses) than previous cohorts, and this retreat from marriage and declining fertility is even more pronounced among younger cohorts (Ryan, Smith, Antonucci, & Jackson, 2012). But as of yet, little is known how these demographic and societal changes, along with increased desires to age in place and avoid institutional care, will matter for long-term care use among newer cohorts. Clearly, understanding the many ways in which intimate relationships influence options in long-term care merits increased attention in research and policy to meet the growing needs of an aging population.
Funding
The research was supported by the National Institute of Minority Health and Health Disparities grant (R01 MD005894-01) and a center grant (R24 HD042849) from the National Institute of Child Health and Human Development to the Population Research Center at the University of Texas at Austin.
Acknowledgments
M. B. Thomeer originated the study, led data analysis and interpretation, and wrote the article. S. Mudrazija participated in the conceptualization of the study and contributed to statistical analysis, data interpretation, and manuscript writing. J. L. Angel participated in the conceptualization of the study, data interpretation, and manuscript writing.
References
- Akamigbo A., & Wolinsky F (2007). New evidence of racial differences in access and their effects on the use of nursing homes among older adults. Medical Care, 45, 672–679. doi:10.1377/hlthaff.27.2.393 [DOI] [PubMed] [Google Scholar]
- Angel J. L., & Settersten R. A (2015). What changing American families mean for aging policies. Public Policy Aging Report, 25, 78–82. doi:10.1093/ppar/prv011 [Google Scholar]
- Brown S. L. (2000). The effect of union type on psychological well-being: Depression among cohabitors versus marrieds. Journal of Health and Social Behavior, 41, 241. doi:10.1177/0022146515594631 [PubMed] [Google Scholar]
- Brown S. L., & Kawamura S (2010). Relationship quality among cohabitors and marrieds in older adulthood. Social Science Research, 39, 777–786. doi:10.1177/0022022111419030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S. L. Lee G. R., & Bulanda J. R (2006). Cohabitation among older adults: A national portrait. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61, S71–S79. doi:10.1093/geronb/61.2.S71 [DOI] [PubMed] [Google Scholar]
- Brown S. L., & Lin I.-F (2012). The gray divorce revolution: Rising divorce among middle-aged and older adults, 1990–2010. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 731–741. doi:10.1093/geronb/gbs089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulanda J. R., & Brown S. L (2007). Race-ethnic differences in marital quality and divorce. Social Science Research, 36, 945–967. doi:10.1016/j.ssresearch.2006.04.001 [Google Scholar]
- Carlson B. L., Foster L., Dale S. B., Brown R. (2007). Effects of cash and counseling on personal care and well-being. Health Services Research, 42, 467–487. doi:10.1111/j.1475-6773.2006.00673.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles K. K., Sevak P. (2005). Can family caregiving substitute for nursing home care? Journal of Health Economics, 24, 1174–1190. doi:10.1016/j.jhealeco.2005.05.001 [DOI] [PubMed] [Google Scholar]
- Cherlin A. (1978). Remarriage as an incomplete institution. American Journal of Sociology, 84, 634–650. [Google Scholar]
- Cherlin A. (2010). Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and the Family, 72, 403–419. doi:10.1111/j.1741-3737.2010.00710.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman P. H. Oberlink M. R. Simantov E., & Gursen M. D (2004). A tale of two older Americas: Community opportunities and challenges. New York, NY: Center for Home Care Policy and Research, Visiting Nurse Service of New York. [Google Scholar]
- Freedman V. A. (1996). Family structure and the risk of nursing home admission. TheJournals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51B, S61–S69. doi:10.1177/0898264315577779 [DOI] [PubMed] [Google Scholar]
- Friedberg L. Wenliang H. Sun W. Webb A., & Li Z (2014). New evidence on the risk of requiring long-term care. Working Paper: CRR WP 2014-12. Center for Retirement Research at Boston College. [Google Scholar]
- Friedman S. M. Steinwachs D. M. Rathouz P. J. Burton L. C., & Mukamel D. B (2005). Characteristics predicting nursing home admission in the program of all-inclusive care for elderly people. The Gerontologist, 45, 157–166. doi:10.1093/geront/45.2.157 [DOI] [PubMed] [Google Scholar]
- Harris-Kojetin L. Sengupta M. Park-Lee E., & Valverde R (2013). Long-term care services in the United States: 2013 overview. National Health Care Statistics Reports, no. 1. Hyattesville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Himes C. L. Wagner G. G. Wolf D. A. Aykan H., & Dougherty D. D (2000). Nursing home entry in Germany and the United States. Journal of Cross-Cultural Gerontology, 15, 99–118. doi:10.1023/A:1006797731500 [DOI] [PubMed] [Google Scholar]
- Horwitz A. V., & White H. R (1998). The relationship of cohabitation and mental health: A study of young adult cohort. Journal of Marriage and the Family, 60, 505–514. doi:10.2307/353865 [Google Scholar]
- Hughes M. E., & Waite L .J (2009). Marital biography and health at mid-life. Journal of Health and Social Behavior, 50, 344–358. doi:10.1177/002214650905000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster F. T., & Suzman R (1995). An overview of the Health and Retirement Study. The Journal of Human Resources, 30, S7–S56. doi:10.2307/146277 [Google Scholar]
- Kalmijn M. (2007). Gender differences in the effects of divorce, widowhood and remarriage on intergenerational support: Does marriage protect fathers? Social Forces, 85, 1079–1104. doi:10.1353/sof.2007.0043 [Google Scholar]
- Kreider R. M. (2006). Remarriage in the United States. Paper presented at the American Sociological Association, Montreal, Canada. [Google Scholar]
- Levin I. (2004). Living apart together: A new family form. Current Sociology, 52, 223–240. doi:10.1177/0011392104041809 [Google Scholar]
- Lin I.-F., & Brown S. L (2012). Unmarried boomers confront old age: A national portrait. The Gerontologist, 52, 153–165. doi:10.1093/geront/47.2.224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., & Umberson D. J (2008). The times they are a changin’: Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior, 49, 239–253. doi:10.1177/002214650804900301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudrazija S. Thomeer M. B., & Angel J (2015). Gender differences in institutional long-term care transitions. Women’s Health Issues, 25, 441–449. doi:10.1016/j.whi.2015.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musick K., Bumpass L. (2012). Re-examining the case for marriage: Union formation and changes in well-being. Journal of Marriage and the Family, 74, 1–18. doi:10.1111/j.1741-3737.2011.00873.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noël-Miller C. (2010). Spousal loss, children, and the risk of nursing home admission. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B, 370–380. doi:10.1093/geronb/gbq020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noël-Miller C. M. (2011). Partner caregiving in older cohabiting couples. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66B, 341–353. doi:10.1093/geronb/gbr027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M. (2003). Loneliness in married, widowed, divorced, and never-married older adults. Journal of Social and Personal Relationships, 20, 31–53. doi:10.1177/02654075030201002 [Google Scholar]
- RAND HRS Data. (2012). National Institute on Aging and the Social Security Administration. Rand Center for the Study of Aging, Version N; Santa Monica, CA. [Google Scholar]
- Rogers S., & Komisar H (2003). Who needs long-term care? Fact sheet, Long-term care financing project. Washington, DC: Georgetown University Press. [Google Scholar]
- Royston P. (2004). Multiple imputation of missing values. Stata Journal, 4, 227–241. [Google Scholar]
- Ryan L. H., Smith J., Antonucci T. C., Jackson J. S. (2012). Cohort differences in the availability of informal caregivers: Are the Boomers at risk? The Gerontologist, 52, 177–188. doi:10.1093/geront/gnr142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sergeant J. F., Ekerdt D. J., Chapin R. K. (2010). Older adults’ expectations to move: Do they predict actual community-based or nursing facility moves within 2 years? Journal of Aging and Health, 22, 1029–1053. doi:10.1177/0898264310368296 [DOI] [PubMed] [Google Scholar]
- Silverstein M., & Wang R (2015). Does familism inhibit demand for long-term care? Public policy implications of growing ethnic diversity in the United States. Public Policy Aging Report, 25, 83–87. doi:10.1093/ppar/prv016 [Google Scholar]
- Spillman B. C. Liu K., & McGilliard C (2008). Trends in residential long term care: Use of nursing homes and assisted living and characteristics of facilities and residents. Washington, DC: The Urban Institute. [Google Scholar]
- Thomeer M. B. Mudrazija S., & Angel J. L (2015). How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 628–638. doi:10.1093/geronb/gbu114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D., Montez J. K. (2010). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51(Suppl), S54–S66. doi:10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D., Williams K., Thomas P. A., Liu H., Thomeer M. B. (2014). Race, gender, and chains of disadvantage: Childhood adversity, social relationships, and health. Journal of Health and Social Behavior, 55, 20–38. doi:10.1177/0022146514521426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2015). America’s families and living arrangements: 2014. Washington, DC: Statistical Abstract of the United States. [Google Scholar]
- U.S. Department of Health and Human Services. (2005). Spouses of Medicaid long-term care recipient. http://aspe.hhs.gov/daltcp/reports/spouses.htm [Google Scholar]
- Vuchinich S. Teachman J., & Crosby L (1991). Families and hazard rates that change over time: Some methodological issues in analyzing transitions. Journal of Marriage and Family, 53, 898–912. doi:10.1023/A:1016001211182 [Google Scholar]
- Williams K., Umberson D. (2004). Marital status, marital transitions, and health: A gendered life course perspective. Journal of Health and Social Behavior, 45, 81–98. doi:10.1177/002214650404500106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth J., & Koso G. (2002). Does marital history matter? Marital status and wealth outcomes among preretirement adults. Journal of Marriage and Family, 64, 254–268. doi:10.1111/j.1741-3737.2002.00254.x [Google Scholar]
- Zhang Z. (2006). Marital history and the burden of cardiovascular disease in midlife. The Gerontologist, 46, 266–270. doi:10.1093/geront/46.2.266 [DOI] [PubMed] [Google Scholar]
- Zhang Z., & Hayward M. D (2006). Gender, the marital life course, and cardiovascular disease in late midlife. Journal of Marriage and Family, 68, 639–657. doi:10.1111/j.1741-3737.2006.00280.x [Google Scholar]
- Zimmerman S. Gruber-Baldini A. L. Sloane P. D. Eckert J. K. Hebel J. R. Morgan L. A., … Konrad T. R (2003). Assisted living and nursing homes: Apples and oranges? The Gerontologist, 43, 101. doi:10.1093/geront/43.suppl_2.107 [DOI] [PubMed] [Google Scholar]