Abstract
The spectrum of psychotic disorder represents a multifactorial and heterogeneous condition and is thought to result from a complex interplay between genetic and environmental factors. In the current paper, we analyze this interplay using network analysis, which has been recently proposed as a novel psychometric framework for the study of mental disorders. Using general population data, we construct network models for the relation between 3 environmental risk factors (cannabis use, developmental trauma, and urban environment), dimensional measures of psychopathology (anxiety, depression, interpersonal sensitivity, obsessive-compulsive disorder, phobic anxiety, somatizations, and hostility), and a composite measure of psychosis expression. Results indicate the existence of specific paths between environmental factors and symptoms. These paths most often involve cannabis use. In addition, the analyses suggest that symptom networks are more strongly connected for people exposed to environmental risk factors, implying that environmental exposure may lead to less resilient symptom networks.
Key words: psychosis, environmental exposure, risk factors, network analysis
Introduction
Disorders in the psychosis spectrum represent one of the leading causes of long-term disability worldwide.1 In spite of extensive efforts, their etiology remains poorly understood, hampering progress in treatment and prognosis.2
While collaborative efforts have confirmed the impact of genetic factors, an important role in the onset and progression of psychotic disorders is thought to be attributable to several environmental risk factors. Specifically, meta-analytical reviews have shown that psychosis expression is associated with developmental trauma, cannabis use, growing up in an urban environment, and minority group position.3 These findings have resulted in extensive research—using a broad range of methodological approaches—concerned with mapping and understanding the relations between environmental factors and schizophrenia.
In the current note, we propose and describe a novel psychometric framework for the study of disorders in the psychosis spectrum and show how it can be used to augment these research efforts. The framework is based on the general idea that mental disorders arise from the interaction between affective, cognitive, and behavioral components that make up its psychopathology and is known as the network approach.4
Psychotic Disorder—Standard Approaches and A Network Alternative
Standard approaches to psychosis spectrum diagnoses such as schizophrenia conceptualize the construct as a latent condition that acts as a common cause of its symptoms.5 In the psychometric representation of this conceptualization, the diagnosis of schizophrenia is represented as a latent variable (or set of latent variables), and its symptoms—such as hallucinations and delusions—are modeled as effects of this latent variable. As a result, symptoms of the disorder are interpreted as passive psychometric indicators, and interactions between symptoms do not form a central research interest. In accordance, this framework typically assumes that environmental factors affect symptoms via the latent disorder (ie, the disorder mediates the relation between environment and symptoms). However, recent studies show this assumption to be problematic, as individual symptoms of a disorder are influenced by different risk factors. For example, childhood trauma is associated with hallucinations and delusions, but not associated with negative symptoms.6 This suggests that alternative modeling options should be considered.
One such modeling option lies in the network approach: a novel psychometric framework based on a dynamical systems perspective. In network models, mental disorders such as schizophrenia are not conceptualized as common causes of symptoms, but as conditions that arise from the interaction between symptoms. Specifically, if symptoms engage in patterns of mutual reinforcement and feedback, the system as a whole can get “locked” in a state of extended (or even permanent) symptom activation: a mental disorder. Individual differences in vulnerability are naturally represented as differences in the connectivity of the network model: in more strongly connected networks, symptoms feature a higher level of interaction, which means that they will more easily activate each other7 to render the system as a whole less resilient.
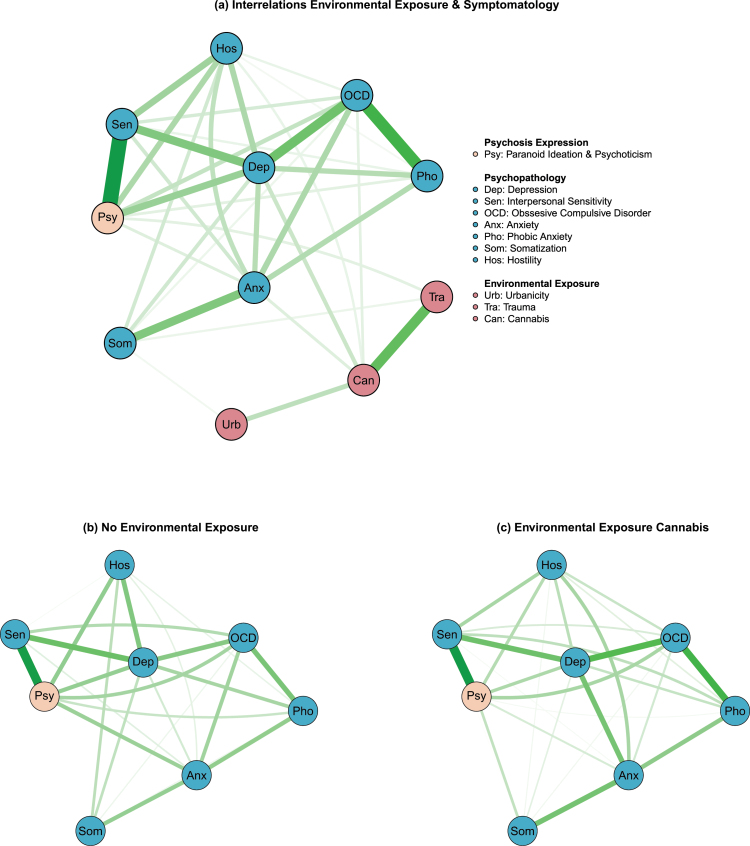
The relevant patterns of interaction can be visualized in a network structure4 (see figure 1), in which variables (here: risk factors and measures of psychopathology) are represented as nodes. The presence of an edge between any 2 nodes implies the existence of a statistical association, which does not vanish upon controlling for all of the other nodes in the network (eg, a partial correlation). Thus, the presence of an edge is suggestive of the existence of a causal relation, although it does not specify the nature or direction of such a relation. In standard visualizations, green edges indicate positive connections, while red edges indicate negative connections.4
Fig. 1.
(a) Network visualization of interrelations between environmental factors and schizophrenia symptomatology. (b and c) Network visualization of differences in psychopathology symptoms connectivity between a group not exposed to any of the three environmental factors and a group exposed to cannabis use. See the online article for a color version of this figure.
Network Analysis of General Population Psychopathology Data
In order to provide an example of how network models can be used to investigate the association between schizophrenia and environmental exposure, we constructed 3 networks of baseline data from the Early Developmental Stages of Psychopathology (EDSP)8 study, a 10-year prospective follow-up study investigating vulnerability and risk factors for onset and progression of psychopathological syndromes (detailed information about the sample is available elsewhere8,9).
First, we determine the network structure pertaining to 3 environmental risk factors (cannabis use, developmental trauma, and urban environment), 7 dimensional measures of psychopathology (anxiety, depression, interpersonal sensitivity, obsessive-compulsive disorder, phobic anxiety, somatizations, and hostility), and 1 composite dimensional measure of psychosis expression. We estimate this network using the mgm R-package10; details about the method, and a step-by-step tutorial on how to execute this type of analysis, are available elsewhere.10,11
The resulting network (figure 1a) shows a dense pattern of connections between dimensions of psychopathology and suggests that the 3 environmental risk factors are differentially related to specific symptoms in this network. For example, developmental trauma is linked to psychosis expression and somatization, while cannabis use is much more strongly related to other domains of psychopathology such as depression, anxiety, obsessive-compulsive disorder, and hostility. In addition, there is a strong positive link between trauma and cannabis use. Urbanicity has the least strong direct impact on psychopathology symptoms, featuring only one (weak) positive connection to somatization (ie, people coming from urban areas may be more prone to expressing symptoms of somatization). In fact, the network suggests that the effect of urbanicity may be largely mediated by cannabis use—people in urban areas may be more likely to use cannabis, which may in turn lead to the development of, eg, anxiety.
In recent research, environmental factors were shown to increase the likelihood of psychosis expression via an increase in general psychopathology.9 One mechanism consistent with this finding is that environmental exposure results in a more strongly connected and thus more vulnerable psychopathology network. To evaluate this hypothesis, we computed separate psychopathology networks for (a) participants who had not been exposed to any of the 3 aforementioned environmental factors (figure 1b) and (b) participants who had been exposed to cannabis use as an environmental risk factor (figure 1c). Even though the 2 networks show a high degree of similarity in terms of their structure, the network of exposed individuals is more strongly connected, and a permutation test7 shows the connectivity difference to be statistically significant (P = .04). The difference appears primarily due to increased connectivity of the node hostility, stronger connectivity between depression and anxiety, and connections between interpersonal sensitivity and phobic anxiety.
Concluding Comments
Network models can serve to disentangle the mechanisms that underlie the relation between environmental risk factors and disorders in the psychosis spectrum. The present note has evaluated 2 network mechanisms by which this may occur. First, environmental factors may exert main effects on specific (sets of) symptoms (eg, cannabis-anxiety) that subsequently spread through the symptom network. Second, environmental factors may increase the strength of interactions between symptoms, leading to a more strongly connected and less resilient network structure. The current examples are consistent with both of these processes.
Future research should aim to replicate these results and can be extended to unravel the precise mechanisms that underlie these statistical associations. In addition, such research should consider the role of genes in modifying the symptom network structure. In particular, it seems likely that genetic vulnerability may be expressed as increased connectivity of symptom interactions, which would serve to increase the impact of environmental factors on the network structure and/or to amplify the increase in connectivity that arises from environmental factors themselves.
Acknowledgment
We would like to express our gratitude to all participants of the Early Developmental Stages of Psychopathology study. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Miyamoto S, Miyake N, Jarskog LF, Fleischhacker WW, Lieberman JA. Pharmacological treatment of schizophrenia: a critical review of the pharmacology and clinical effects of current and future therapeutic agents. Mol Psychiatry. 2012;17:1206–1227. [DOI] [PubMed] [Google Scholar]
- 3. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. 2010;468:203–212. [DOI] [PubMed] [Google Scholar]
- 4. Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. [DOI] [PubMed] [Google Scholar]
- 5. Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol. 2013;31:43–53. [Google Scholar]
- 6. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of longitudinal depression. JAMA Psychiatry. 2015;72:1219–1226. [DOI] [PubMed] [Google Scholar]
- 8. Wittchen HU, Perkonigg A, Lachner G, Nelson CB. Early developmental stages of psychopathology study (EDSP): objectives and design. Eur Addict Res. 1998;4:18–27. [DOI] [PubMed] [Google Scholar]
- 9. Guloksuz S, van Nierop M, Lieb R, van Winkel R, Wittchen HU, van Os J. Evidence that the presence of psychosis in non-psychotic disorder is environment-dependent and mediated by severity of non-psychotic psychopathology. Psychol Med. 2015;45:2389–2401. [DOI] [PubMed] [Google Scholar]
- 10. Haslbeck JMB, Waldorp LJ. mgm: Structure Estimation for Time-Varying Mixed Graphical Models in high-dimensional Data. 2016. arXiv preprint 1510.06871. https://arxiv.org/abs/1510.06871. Accessed April 28, 2016.
- 11. Costantini G, Epskamp S, Borsboom D, et al. State of the art personality research: a tutorial on network analysis of personality data in R. J Res Pers. 2015;54:13–29. [Google Scholar]