Abstract
Background
Middle-Aged and older African American women experience disproportionate rates of functional limitations and disability from osteoarthritis (OA) compared to other racial ethnic groups; however, little is known about what factors contribute to this disparity within African American women.
Objective
To examine factors associated with physical function and disability among African American women ages 50–80 with OA using the disablement process model.
Methods
This descriptive study included 120 African American women with OA from the Southwestern region of the United States. Regression techniques were used to model the correlates of physical function and disability and to test a mediation model.
Results
BMI and pain severity were significantly related to functional limitations. Depressive symptoms mediated the relationship between racial discrimination and disability.
Conclusion
Biological, intra individual, and extra individual factors are related to disablement outcomes in this sample of African American women, which is consistent with theory suggesting the need for treatment coupled with environmental modifications. This study can inform the development of future bio-behavioral interventions.
Keywords: older African Americans, functional limitations, disability, osteoarthritis
Osteoarthritis (OA) is a serious condition that can lead to mobility impairment, functional limitations and disabilities in older adults 1, 2, 3, and affects 33% (12.4 million) of all adults over the age of 65. 1 Approximately 80% of adults who have OA experience some level of mobility impairment, and 25% have disabilities. 1 Osteoarthritis can be particularly disabling in older minorities.
Middle-aged and older African American women in particular experience disproportionate rates of functional limitations and disabilities from OA in comparison to other older racial/ethnic groups. 4–9 Specifically, African American women with arthritis experience disability at almost twice the rate of their non-Hispanic White counterparts. 10 Although researchers have suggested that these disproportionate rates of functional limitations in African American women may be due to biological factors such as age, BMI, and pain, 8, 11, 12 it remains unclear what other factors may be related to disability in these women. 13, 14
Researchers examining factors related to functional limitations and disability in African Americans have examined between-group differences in African Americans and non-Hispanic Whites; however, little has been done examining these outcomes within samples of African American women. The researchers reported mixed findings in these studies. For example, after controlling for body mass index (BMI) and depressive symptoms, researchers reported no significant differences in functional limitations between African Americans and non-Hispanic Whites with knee OA.4 Yet in another study, African Americans were more likely to have activity and functional limitations than non-Hispanic Whites, after controlling for age and BMI. 13 Researchers have also reported that African Americans with OA have more pain and disability than non-Hispanic Whites with OA; however, these differences were no longer present after controlling for age and education. 15 Knee pain has been significantly associated with difficulty in performing functional tasks among African Americans and non-Hispanic Whites with OA. 16 When looking at depressive symptoms among African Americans researchers have reported both non-significant15 and significant relationships between more depressive symptoms and disability. 17, 18
In addition to looking at factors that have a relationship with physical function and disability outcomes, we have chosen three variables that are not routinely examined to explain these outcomes in African American women with OA. These include perceived racial discrimination, number of physician visits, and trust in healthcare providers. These three variables are both intra individual and extra individual factors and have used to explain health outcomes among this population; 19–27 however, little work has examined if these factors are related to functional limitations and disability outcomes among African American women with OA. Previous work examining different stages of the disablement process among African American women has not focused on intra and extra individual factors that might explain the within-group differences.
The disablement process model was used as a theoretical framework for this study. 28 The disablement process represents a four stage pathway that begins with pathology, followed by impairments, functional limitations, and ends with disability. A functional limitation is defined as an alteration in the use of the body that restricts engaging in specific activities. Disability is the inability to perform social roles or engage in activities of daily life (i.e. household activities, work, socialize). According to the disablement model, 28 both of these outcomes can be affected by biological (age, BMI), intra-individual (pain, depressive symptoms, trust in health care providers, number of physician visits), and/or extra-individual factors (racial discrimination). 28
The purpose of this study was to examine factors associated with physical function and disability among African American women ages 50–80 with OA using the disablement process model. We specifically sought to determine if pain severity, and/or depressive symptoms were correlates of functional limitations within a group of African American women. We also sought to determine if trust in health care providers was related to functional limitations and if this relationship was mediated by the number of physician visits, and lastly if racial discrimination was related to disability in the women and if the relationship was mediated by depressive symptoms.
Methods
Participants
The participants for this study were a convenience sample of 120 African American women ages 50–80 years of age with a diagnosis of OA and functional limitations. The inclusion criteria for this study included women who reported having 2 of 4 functional limitations derived from the National Health Interview Survey (unable to stand for 20 min, bend from a standing position, walk a quarter of a mile, or walk 10 steps without resting; CDC, 2009). 29
Measures
Age, BMI
Self-reported age was used as both a continuous variable in regression models and a dichotomous variable (middle-aged [50–65], and older [66–80]) in describing the sample. The women reported their weight and height. BMI was calculated using the following formula: BMI = weight (in pounds)/[height (in inches)]2 × 703.30
Functional Limitations
Functional limitations were measured with the revised version of the Health Assessment Questionnaire Disability Index (HAQ-DI), which assesses functional ability by addressing 8 activities including: dressing and grooming, arising, eating, walking, hygiene, reaching, gripping, and errands/chores. 31 The HAQ DI has previously been used to measure physical function limitations in people with arthritis and women aging with paralytic polio. 32, 33 Total scores on the HAQ-DI can range from 0–3, with 3 indicating severe limitations. Function was measured as a continuous variable and the Cronbach’s alpha for the HAQ-DI in this study was 0.93
Disability
Disability was measured using the Craig Handicap Assessment and Reporting Technique (CHART).34,35 The Chart contains 32 items across six dimensions including physical independence, mobility, occupation, social integration, economic self-sufficiency, and cognitive independence. The total index score could range from 0–600 and a total index score of less than 450 indicated the presence of disability. 35, 36 Researchers have reported the CHART to be a reliable instrument in samples that included African Americans and have reported a test–retest reliability of .93. 37
Number of Physician Visits
The number of physician visits was measured using the Stanford Health Care Utilization Survey (HCU). 38, 39 For the present study, the number of physician visits was measured using the number of physician visits in the last six months. Researchers have reported the HCU items to have strong test–retest reliabilities. The number of physician visits on the HCU has had a reported reliability of.76. 39
Pain Severity
Pain severity was measured using the short form of the McGill Pain Questionnaire (SF-MPQ). 40,41 For the present sample, Cronbach’s alpha for the total pain severity subscale was .87. The pain severity score could range from a 0–26 with higher scores indicating more pain severity.
Trust in Health Care Providers
Trust in providers was measured with the Trust in Physicians Scale (TPS). 42 The TPS measures three dimensions of trust in physicians: (1) dependability of physician, (2) confidence in physician’s skill set, and (3) reliability of information between patient and physician. The TPS has been adapted to measure trust in health care providers as opposed to just trust in physicians. 43 Higher scores indicate more trust in health care. Four items on the scale needed to be recoded. The TPS had a Cronbach’s alpha of .84 for this sample.
Depressive Symptoms
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D).44 The CES-D’s 20 items measure depression across nine domains: sadness, loss of interest, appetite, sleep, thinking/concentration, guilt, fatigue, movement, and suicidal ideations. The Cronbach’s alpha for the CES-D for this sample was 0.89. The CES-D scores can range from 0–60 with higher scores indicating more depressive symptoms.
Racial Discrimination
Racial discrimination was measured using the General Ethnic Discrimination Scale (GED), 45 an adaptation of the Schedule of Racist Events Scale. 46 The scale measured whether racist events were experienced over the last year using a Likert scale ranging from 1 indicating never to 6 indicating almost all of the time. In the present study, the recent discrimination subscale was used, which had a Cronbach’s alpha of 0.93
Procedures
Participants in this study were recruited through professional organizations (e.g. sororities and organizations for retired seniors) and churches in the Southwest region of the United States, including the states of Texas and New Mexico using fliers, research liaisons, and word of mouth. Participants who verbalized interest by calling the toll free number were screened for eligibility: diagnosis, age, sex, function, and race. The women who were eligible to be in the study were asked to complete a survey booklet. The booklet was administered via mail or in person depending on the request of the participant or if the participant was attending a health fair where data was collected in person. Participants were given $50 compensation upon completion and return of the booklet. All aspects of this study were reviewed and approved by The University of Texas at Austin Institutional Review Board. Verbal consent was obtained and then participants were mailed or handed a written consent form to complete.
Data Analysis
Descriptive statistics (means, standard deviations, and frequencies) were used to describe the sample. Pearson’s correlations were used to detect relationships between independent variables and outcome variables. Multiple regression was used to test specific correlates of functional limitations and/or disability. Variables that were not significantly related to function or disability were not included in the regression analyses. Mediation was tested using the method of Baron and Kenny (1986) and Preacher and Hayes (2004). 47, 48 A set of multiple regressions were completed and a Sobel test was conducted to test the indirect effects of racial discrimination on disability through depressive symptoms. SPSS version 22 and SPSS macro were used to analyze data. The CHART variable that was used to measure disability was missing 17% of the data; therefore, missing value imputations were conducted. When data is missing on the CHART instrument fewer subscales may be used to calculate total scores; however, we opted to maintain all subscales and impute missing data. Missing value imputations are a systematic way of estimating scores for missing values. 49 An imputation algorithm based on a Markov chain Monte Carlo simulation methods on SPSS 22 50 was used to conduct multiple imputations. Of note, patterns and percentages of missing values were analyzed for all the variables. Given that missing values were imputed for only those variables with more than 5% missing data, the only variable needing imputations was disability, e.g. the CHART. The level of statistical significance set for all research questions was p < 0.05.
Non-normality was detected so there were study variables that were transformed. In order to address positive skewness we transformed the number of physician visits, racial discrimination scores and depressive symptom scores. 49 After transformations of these variables, the variables showed normality and the regression assumptions were met before running further analyses.
Results
Sample
Nine percent of participants (n = 11) were from New Mexico; 91% (n = 109) were from Texas. The mean age for this sample was 63.04 (SD= 8.57). A total of 62% (n=74) of the sample was middle-aged and 38% (n-46) was older. A total of 63% of the participants (n = 76) were unemployed; 20% (n = 24) worked less than 40 hours a week; and 17% (n = 20) worked 40 hours a week or more. The average number of years of education was 14 (SD=2.9). This sample had a relatively high average education level in comparison to other studies of African Americans. 11. The average number of years with OA was 11.33 (SD= 10.46), ranging from 6 months to 64 years. The average BMI for this sample was 35.27 (SD=77.45). The mean BMI for this sample was slightly higher than the mean BMI in other samples of African American women. 12, 51 On average, middle-aged women reported significantly more pain severity (M=8.61, SE= 0.94) than older women (M=5.78, SE=0.94). ) (t (118) =2.12, p<.05). There was not a significant difference in education, disability, or function between middle-aged and older women. 12, 51 A detailed characterization of the sample is presented in Table 1.
Table 1.
Sample Characteristics of Middle-Aged and Older African American women with OA
| Mean | SD | Frequency | Percentage | |
|---|---|---|---|---|
| Age | 63.04 | 8.57 | ||
| Yearly Income | ||||
| Less than 10,000 | 27 | 23% | ||
| 10,001–15,000 | 22 | 18% | ||
| 15,001–20,000 | 5 | 4% | ||
| 20,001–25,000 | 12 | 10% | ||
| 25,001–35,000 | 14 | 12% | ||
| 35,001–50,000 | 14 | 12% | ||
| 50,001–75,000 | 17 | 14% | ||
| Greater than 75,000 | 6 | 5% | ||
| Missing | 3 | 2% | ||
| Employment | ||||
| Employed | 44 | 37% | ||
| Unemployed | 76 | 63% | ||
| Education in years | 14 | 2.9 | ||
| Marital Status | ||||
| Married | 36 | 30% | ||
| Divorced | 43 | 36% | ||
| Widowed | 27 | 23% | ||
| Never Married | 11 | 9% | ||
| Missing | 3 | 2% | ||
| Children in home | 41 | 35% | ||
| Had joint replacement | 25 | 21% | ||
Functional Limitations
We ran two models to test significant correlates of functional limitations among pain and depressive symptoms while controlling for covariates BMI, age, length of time with OA, and years of education in both models. In Model 1, pain severity was significantly associated with function (β = 0.50, p < .05). In Model 2, depressive symptoms were added. Pain severity remained significantly associated with function (β =0.48, p < .05); however, depressive symptoms were not significantly associated with function. See Table 2 for results of both models. BMI and age were significantly associated with function while length of time with OA was not.
Table 2.
Correlates of Function in Middle-Aged and Older African American Women
| Model/Variables | β | Adjusted R2 | t | p values |
|---|---|---|---|---|
| Model 1 | 0.29 | |||
| Pain Severity | 0.50 | 6.12 | 0.00 | |
| BMI | 0.23 | 2.80 | 0.01 | |
| Age | 0.20 | 2.28 | 0.02 | |
| How Long with OA | −0.06 | −0.68 | 0.50 | |
| Number of Years of Education | −0.12 | −1.32 | 0.19 | |
| Model 2 | 0.30 | |||
| Pain Severity | 0.48 | 5.75 | 0.00 | |
| Depressive Symptoms | 0.08 | 0.95 | 0.35 | |
| BMI | 0.23 | 2.74 | 0.01 | |
| Age | 0.21 | 2.42 | 0.02 | |
| How long with OA | −0.06 | −0.69 | 0.49 | |
| Number of Years of Education | −0.09 | −1.10 | 0.27 |
Number of Physician Visits as a Mediator
We tested if trust in health care providers was associated with function and if the relationship was mediated by number of physician visits. We found that trust in health care providers was not associated with function or number of physician visits; hence, it was determined that number of physician visits was not a significant mediator between trust in health care providers and function (results not shown).
Disability
We tested if pain severity was significantly related to disability while controlling for BMI, age, and length of time with OA, and years of education. Pain severity was significantly associated with disability (β = −0.24, p <0.05). However when we added function to this model, pain severity was no longer significantly associated with disability (β = −0.16, p> 0.05), whereas function was (β = −0.36, p <.05). The findings of these models are found in Table 3.
Table 3.
Correlates of Disability in Middle-Aged and Older African American Women
| Model/Variables | β | Adjusted R2 | t | p values |
|---|---|---|---|---|
| Model 1 | 0.13 | |||
| Pain Severity | −0.24 | −3.01 | 0.00 | |
| BMI | −0.06 | −0.73 | 0.47 | |
| Age | −0.05 | −0.84 | 0.40 | |
| How Long with OA | 0.01 | 0.01 | 0.99 | |
| Number of Years of Education | 0.26 | 3.01 | 0.00 | |
| Model 2 | 0.30 | |||
| Pain Severity | −0.16 | −0.96 | 0.34 | |
| Function | −0.36 | −3.38 | 0.00 | |
| BMI | 0.01 | 0.23 | 0.82 | |
| Age | −0.08 | −0.14 | 0.88 | |
| How long with OA | 0.00 | 0.01 | 0.81 | |
| Number of Years of Education | 0.30 | 2.70 | 0.01 |
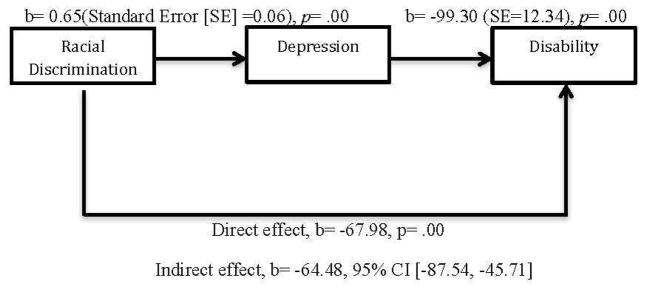
Depressive Symptoms as a Mediator
To test for the mediation effect of depressive symptoms on the relationship between racial discrimination and disability, the SPSS macros by Hayes was used to conduct a series of three regressions and the SOBEL test. This statistical application provided unstandardized b values, which are reported here. We controlled for BMI, age, length of time with OA, and years of education. First, disability was regressed on racial discrimination (b = −132.46, p <.05), which was significantly associated with disability. Second, depressive symptoms were regressed on racial discrimination (b=0.65, p<.05). Lastly, disability was regressed on depressive symptoms (b= −99.30, p <.05) while controlling for racial discrimination (b = −67.98, p < .05), Results show that the relationship between racial discrimination and disability was reduced and but still significant, suggesting that the relationship is partially mediated by depressive symptoms. This finding was further substantiated with the Sobel test, which more clearly delineates direct and indirect effects and allows for bootstrapping. The Sobel results supported that depressive symptoms significantly mediated the relationship between racial discrimination and disability (Z=−6.28, p<.05). The criteria for mediation were met and results suggest that depressive symptoms partially mediated the relationship between racial discrimination and disability. Please see Figure 1 for the direct effects and indirect effects of the SOBEL test.
Figure 1.
Mediation Model of Depression Mediating the Relationship between Racial Discrimination and Disability
Discussion
African American women often experience high rates of functional limitations and disability when they have a chronic condition such as OA. The primary intent of this study was to examine and understand what factors were related to the disablement outcomes (physical function and disability) in middle aged and older African American women with OA. We found that pain severity was associated with poorer function. The results of our analyses highlight factors related to disablement outcomes, which may be targeted to decrease the risk of functional limitations and disability. Pain severity, which is consistent with previous literature that pain is associated with function. 11, 52 Pain was still associated with function even after controlling for BMI. Pain may present difficulty when climbing stairs or walking. 53 Although weight may be an important health indicator our results show it may be pain that is more detrimental to function outcomes among older African American women. In addition, we explored if trust in health care providers was related to number of physician visits or function; our findings showed that trust in their health care providers was not related to their number of physician visits or their function.
We also determined that pain severity was associated with disability, which is consistent with previous findings in African Americans 14 and in older minority groups; 14, 54, 55 however, when we placed function in the model pain severity was no longer associated with disability but function was. In this study, women who had greater difficulty performing physical tasks such as climbing stairs or walking (function) were less able to engage in social roles (disability). The women’s social roles had a stronger relationship to physical function than pain severity. Further investigation may be needed to understand if function serves as a moderator between pain severity and disability.
Racial discrimination, which is related to self-report of worse physical and mental health, increased asthma risk, unhealthy behaviors, and higher blood pressures in African Americans, 24–27 was previously an unmeasured factor in the OA literature. In our study racial discrimination was associated with disability, as were depressive symptoms. Mediation was used to examine these relationships more closely. Depressive symptoms mediated the relationship between racial discrimination and disability. This indicates that although racial discrimination was associated with disability in African American women, this relationship may be related to the effect discrimination has on their ability to use their cognitive and emotional strength to overcome their functional limitations. In other words, discrimination is associated with poor mental health outcomes 56, which is related to the African American woman experiencing higher levels of disability. This is an area that needs to be explored further.
Overall, the findings of this study suggest that physical function and disability outcomes in African American women with OA does not occur in a social vacuum, but are influenced by factors in the women’s lives that may contribute to poorer function and greater disability. 57 Pain severity was associated with function suggesting that interventions targeting pain may be a path to improving function. Integrating holistic patient-centered care that includes an assessment of beliefs and experiences surrounding pain into a person’s pain treatment plan can lead to better outcomes.58 Further work focused on developing effective multidisciplinary pain programs tailored for African Americans is needed. 58 Researchers should develop interventions that address pain, and psychosocial coping from racial discrimination, and depressive symptoms in middle-aged and older African American women with OA. Effective interventions for depressive symptoms in African American women should stem from a holistic model that focuses on coping skills, social management skills, and health promotion.59 Coping skills that help African American women handle racial discrimination may also be needed. The results are consistent with those of previous studies in minority women that showed the pathway to disability was not necessarily a linear path from pathology to function to disability. The path to disability can be influenced by various, intra individual factors and extra individual factors. 57 Future studies should test factors associated with functional limitations and disability in African American women with conditions such as lupus or diabetes in order to obtain knowledge on function and disability outcomes in women with other chronic conditions. It is important that researchers work toward decreasing disability rates and improving function among older adults. 60
There were limitations to this study. First, the study was cross-sectional; causality cannot be assumed from such a design. Second, self-report was used, which can present limitations because participants might have difficulty remembering or might inaccurately report data. The women’s self-report of weight and height might not have been accurate. The third limitation is that the results of this study cannot be generalized beyond this sample of African American women with OA between the ages of 50 and 80 from Texas and New Mexico. A fourth limitation of this study was that this was a convenience sample, so there was the possibility of self-selection bias. The Sobel test uses asymptotic properties that are more appropriate for larger sample sizes. However, given paucity of tests for mediation, this is an often cited limitation of the Sobel test. Finally, comorbidities were not measured, so their effect on disability and function outcomes were not taken into account and we did not ask what type of OA the women had.
Despite the limitations, the current study was important because the findings show that the risk profile for functional limitations and disability in this sample of African American women with OA included other factors in addition to the biological factors, BMI and age. Further, a strength of this study is the variation in income levels of the women; their economic status did not fit into one category but were dispersed throughout the eight categories. This was a strength because we were able to examine function and disability outcomes in women from diverse income levels as opposed to a more homogenous sample that is majority low income or high income. The women’s health, environment, and reactions to their health and environment can all influence their disability outcomes and these women had a range of economic resources. This is also consistent with disability researchers who suggest that disability is a broader concept than health and impairment, and needs to be studied from a perspective of societal access.58
When within-group variability is known about a minority group, policies and interventions can be better tailored to meet the needs of that particular group.61 The knowledge gained from this study can provide a strong foundation leading to the development of appropriate interventions focused on improving function and decreasing disability rates in African American women with OA.
Conclusion
Our study adds to the scant literature on function and disability outcomes in African American women with OA by assessing the role pain, perceived racial discrimination, and depressive symptoms have on function and disability outcomes in older African American women with OA. Frequently, researchers examine function and disability outcomes using population-based studies in which they compare outcomes across various racial/ethnic groups and between sexes. 57 The results of this study, however, provide knowledge about functional limitations and disability using theoretical based variables, which might advance a more pragmatic approach to understanding African American women’s lives with OA. Although OA may be not life-threatening it is disabling, very prevalent, and often lacks uniform treatment. By gaining a better understanding of what biological, intra-individual and extra-individual factors lead to the disparities of functional limitations and disability in African American women with OA, researchers can begin to develop interventions to improve function, decrease disability rates, and improve quality of life that are tailored to African American women with OA.
Acknowledgments
This study was supported by the National Hartford Center of Gerontological Nursing Excellence Patricia G. Archbold Scholarship/MayDay Award, and NIH/NINR (1F131NR014399-01). The first author is supported by Johns Hopkins University Interdisciplinary Training Program in Bio-Behavioral Pain Research (NS070201).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Osteoarthritis Web site. Centers for Disease Control and Prevention; [Accessed January 29, 2015]. Osteoarthritis. http://www.cdc.gov/arthritis/basics/osteoarthritis.htm Published 2011, Updated May 14, 2014. [Google Scholar]
- 2.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: The role of catastrophizing. Pain. 2000;87:325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 3.Steinhilber B, Haupt G, Miller R, Grau S, Janssen P, Krauss I. Stiffness, pain and hip muscle strength are factors associated with self-reported physical disability in hip osteoarthritis. J Geriatric Phys Ther. 2014:99–105. doi: 10.1519/JPT.0b013e3182abe7b5. [DOI] [PubMed] [Google Scholar]
- 4.Allen KD, Helmick CG, Schwartz TA, DeVellis RF, Renner JB, Jordan JM. Racial differences in self-reported pain and function among individuals with radiographic hip and knee osteoarthritis: The Johnston County osteoarthritis project. Osteoarthritis Cartilage. 2009;17(9):1132–1136. doi: 10.1016/j.joca.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burns R, Graney MJ, Lummus AC, Nichols LO, Martindale-Adams J. Differences of self-reported osteoarthritis disability and race. JAMA. 2007;99(9):1046–1051. [PMC free article] [PubMed] [Google Scholar]
- 6.Elliott AL, Kraus VB, Fang F, Renner JB, Schwartz TA, Salazar A, … Jordan JM. Joint-specific hand symptoms and self-reported and performance-based functional status in African-Americans and Caucasians: The Johnston County Osteoarthritis Project. Ann Rheum Dis. 2007;66(12):1622–1626. doi: 10.1136/ard.2006.057422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andresen EM, Brownson RC. Disability and health status: ethnic differences among women in the United States. J Epidemiol Community Health. 2000;54(3):200–206. doi: 10.1136/jech.54.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colbert CJ, Almagor O, Chmiel JS, Song J, Dunlop D, Hayes KW, Sharma L. Excess body weight and four-year function outcomes: comparison of African Americans and whites in a prospective study of osteoarthritis. Arthritis Care Res (Hoboken) 2013;65(1):5–14. doi: 10.1002/acr.21811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sowers M, Jannausch ML, Gross M, Karvonen-Gutierrez CA, Palmieri RM, Crutchfield M, Richards-McCullough K. Performance-based Physical Functioning in African-American and Caucasian Women at Midlife: Considering Body Composition, Quadriceps Strength, and Knee Osteoarthritis. Am J Epidemiol. 2006;163(10):950–958. doi: 10.1093/aje/kwj109. [DOI] [PubMed] [Google Scholar]
- 10.Song J, Chang HJ, Tirodkar M, Chang RW, Manheim LM, Dunlop DD. Racial/ethnic differences in activities of daily living disability in older adults with arthritis: A longitudinal study. Arthritis Care Res. 2007;57(6):1058–1066. doi: 10.1002/art.22906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker TA, Whitfield KE. Physical functioning in older blacks: An exploratory study identifying psychosocial and clinical predictors. J Natl Med Assoc. 2006;98(7):1114–1120. [PMC free article] [PubMed] [Google Scholar]
- 12.Murrock CJ, Zauszniewski JA. Late life function and disability instrument in African American women: Function component. Women’s Health. 2011;51(5):482–496. doi: 10.1080/03630242.2011.589493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bolen J, Schieb L, Hootman JM, Helmick CG. Theis K., Murphy LB, Langmaid, G. Differences in the prevalence and severity of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis. 2010;7(3):A64. [PMC free article] [PubMed] [Google Scholar]
- 14.Cano A, Mayo A, Ventimiglia M. Coping, pain severity, interference, and disability: The potential mediating and moderating roles of race and education. J Pain. 2006;7(7):459–468. doi: 10.1016/j.jpain.2006.01.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parmelee PA, Harralson TL, McPherron JA, DeCoster J, Schumacher HR. Pain, disability, and depression in osteoarthritis: Effects of race and sex. J Aging Health. 2012;24(1):168–187. doi: 10.1177/0898264311410425. [DOI] [PubMed] [Google Scholar]
- 16.Jordan JM, Luta G, Renner JB, Dragomir A, Hochberg MC, Fryer JG. Knee pain and knee osteoarthritis severity in self-reported task-specific disability: The Johnston County Osteoarthritis Project. J Rheumatol. 1997;24(7):1344–1349. [PubMed] [Google Scholar]
- 17.Mendes de Leon CF, Rajan KB. Psychosocial influences in onset and progression of late life disability. J Gerontol A Biol Sci Med Sci. 2014;69(2):287–302. doi: 10.1093/geronb/gbt130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thorpe RJ, Jr, Clay OJ, Szanton SL, Allaire JC, Whitfield KE. Correlates of mobility limitation in African Americans. J Gerontol A Biol Sci Med Sci. 2011;66(11):1258–1263. doi: 10.1093/Gerona/glr122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greiner KA, James AS, Born W, Hall S, Engelman KK, Okuyemi KS, Ahluwalia JS. Predictors of fecal occult blood test (FOBT) completion among low-income adults. Prev Med. 2005;41(2):676–684. doi: 10.1016/j.ypmed.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99(7):1293–1299. doi: 10.2105/ajph.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheppard VB, Mays D, LaVeist T, Tercyak KP. Medical mistrust influences black women’s level of engagement in BRCA 1/2 genetic counseling and testing. J Natl Med Assoc. 2019;105(1):17–22. doi: 10.1016/s0027-9684(15)30081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saha S, Jacobs EA, Moore RD, Beach MC. Trust in physicians and racial disparities in HIV care. AIDS Patient Care STDs. 2019;24(7):415–420. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owsley C, McGwin G, Scilley K, Girkin CA, Phillips JM, Searcey K. Perceived barriers to care and attitudes about vision and eye care: focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006;47(7):2797–2802. doi: 10.1167/iovs.06-0107. [DOI] [PubMed] [Google Scholar]
- 24.Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc Sci Med. 2006;63(6):1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Coogan PF, Yu J, O’Connor GT, Brown TA, Cozier YC, Palmer JR, Rosenberg L. Experiences of racism and the incidence of adult-onset asthma in the Black Women’s Health Study. CHEST. 2014;145(3):480–485. doi: 10.1378/chest.13-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bull. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: Relationship to cardiovascular reactivity among African American and European American women. J Health Psychol. 2001;20(5):315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- 28.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 29.National Health Interview Survey on Disability. Centers for Disease Control and Prevention; [Accessed February 19, 2015]. Web site http://www.cdc.gov/nchs/nhis/nhis_disability.htm. Updated June 17, 2009. [Google Scholar]
- 30.About BMI for adults. Centers of Disease Control and Prevention; [Accessed February 19, 2015]. Web Site. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#Interpreted. Updated July 11, 2014. [Google Scholar]
- 31.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis & Rheum. 1980;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 32.Metsios GS, Stavropoulos-Kalinoglou A, Veldhuijzen van Zanten JJ, et al. Individualised exercise improves endothelial function in patients with rheumatoid arthritis. Ann Rheum Dis. 2014;73(4):748–751. doi: 10.1136/annrheumdis-2013-203291. [DOI] [PubMed] [Google Scholar]
- 33.Harrison T. Development of the activity effort scale for women aging with paralytic polio. J Neruosci Nurs. 2009;41(3):168–76. doi: 10.1097/jnn.0b013e3181a23e64. [DOI] [PubMed] [Google Scholar]
- 34.Mellick D, Walker N, Brooks CA, Whiteneck G. Incorporating the cognitive independence domain into CHART. Journal of Rehabilitation Outcomes Measurement. 1999;3:12–21. [Google Scholar]
- 35.Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. The Craig handicap assessment & reporting technique. Englewood, CO: Craig Hospital; 1988. [Google Scholar]
- 36.Whiteneck G, Brooks CA, Mellick D, Harrison-Felix C, Terrill MS, Noble K. Population-based estimates of outcomes after hospitalization for traumatic brain injury in Colorado. Arch Phys Med Rehabil. 2007;85:73–81. doi: 10.1016/j.apmr.2003.08.107. [DOI] [PubMed] [Google Scholar]
- 37.Meade MA, Lewis A, Jackson MN, Hess DW. Race, employment, and spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1782–1792. doi: 10.1016/j.apmr.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 38.Lorig K, Stewart A, Ritter P, Gonzalez VM, Laurent D, Lynch J. Outcome measures for health education and other health care interventions. Vol. 1996 Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- 39.Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. J Clin Epidemiol. 2001;54(2):136–141. doi: 10.1016/s0895-4356(00)00261-4. [DOI] [PubMed] [Google Scholar]
- 40.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 41.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 42.Anderson LA, Dedrick RF. Development of the Trust in Physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67:1091–1100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 43.Benkert R, Peters R, Tate N, Dinardo E. Trust of nurse practitioners and physicians among African Americans with hypertension. J Am Acad Nurse Pract. 2008;20(5):273–280. doi: 10.1111/j.1745-7599.2008.00317.x. [DOI] [PubMed] [Google Scholar]
- 44.Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for Epidemiologic studies depression scale: Review and revision (CESD and CESD-R) In: Maurish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 3. Mahwah, NJ: Erlbaum; 2004. pp. 363–377. [Google Scholar]
- 45.Landrine H, Klonoff EA. The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. J Black Psychol. 1996;22(2):144–168. doi: 10.1177/00957984960222002. [DOI] [Google Scholar]
- 46.Landrine H, Klonoff EA, Corral I, Fernandez S, Roesch S. Conceptualizing and measuring ethnic discrimination in health research. J Behav Med. 2006;29(1):79–94. doi: 10.1007/s10865-005-9029-0. [DOI] [PubMed] [Google Scholar]
- 47.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 48.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 49.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6. Boston, MA: Pearson; 2013. [Google Scholar]
- 50.IBM SPSS Missing Values 22. IBM; [Accessed February 19, 2015]. Web site. ftp://ftp.software.ibm.com/software/analytics/spss/documentation/statistics/22.0/en/client/Manuals/IBM_SPSS_Missing_Values.pdf Published 2013. [Google Scholar]
- 51.Newton RA, Cromwell RL. The relationship between physical performance and obesity in elderly African-American women. Phys Occup Ther Geriatr. 2009;27(6):423–440. [Google Scholar]
- 52.Cruz-Almeida Y, Sibille KT, Goodin BR, et al. Racial and ethnic differences in older adults with knee osteoarthritis. Arthritis Rheumatol. 2014;66(7):1800–1810. doi: 10.1002/art.38620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leveille SG, Bean J, Ngo L, McMullen W, Guralnik JM. The pathway from musculoskeletal pain to mobility difficulty in older disabled women. Pain. 2007;128(1):69–77. doi: 10.1016/j.pain.2006.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mangione KK, Craik RL, McCormick AA, et al. Detectable changes in physical performance measures in elderly African Americans. Phys Ther. 2010;90(6):921–927. doi: 10.2522/ptj.20090363. [DOI] [PubMed] [Google Scholar]
- 55.Ostir GV, Markides KS, Black SA, Goodwin JS. Lower body functioning as a predictor of subsequent disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 1998;53(6):491–495. doi: 10.1093/gerona/53a.6.m491. [DOI] [PubMed] [Google Scholar]
- 56.Hudson DL, Neighbors HW, Geronimus AT, Jackson JS. Racial Discrimination, John Henryism, and depression among African Americans. J Black Psychol. 2015:1–22. doi: 10.1177/0095798414567757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harrison T. Health disparities among Latinas aging with disabilities. Fam Community Health. 2009;32(1):1–12. doi: 10.1097/01.FCH.0000342838.05607.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hooten MW, Knight-Brown M, Townsend CO, Laures HJ. Clinical outcomes of multidisciplinary pain rehabilitation among African American compared with Caucasian patients with chronic pain. Pain Med. 2012;13:1499–1508. doi: 10.1111/j.1526-4637.2012.01489.x. [DOI] [PubMed] [Google Scholar]
- 59.Taylor J, Henderson D, Jackson BB. A holistic model for understanding and predicting depressive symptoms in African-American women. J Community Psychol. 1991;19(4):306–320. [Google Scholar]
- 60.Szanton SL, Thorpe RJ, Jr, Boyd C, et al. Community aging in place, advancing better living for elders: A bio-behavioral-environmental intervention to improve function and heath-related quality of life in disabled older adults. J AM Geriatr Soc. 2011;59(12):2314–2320. doi: 10.1111/j.1532-5415.2011.03698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Whitfield KE, Baker-Thomas T. Individual differences in aging minorities. Int J Aging Hum Dev. 1999;48(1):73–79. doi: 10.2190/YGAQ-0D95-M0V4-820M. [DOI] [PubMed] [Google Scholar]