Abstract
Background
The increasing stroke burden in sub-Saharan Africa far outstrips the availability of skilled human resource to provide timely and efficient acute, rehabilitative and preventive services. The objective of this study was to examine the impact of a short-term task-shifting stroke training program on the stroke knowledge of a cohort of Nigerian non-neurologist health workers (NNHWs).
Methods
Utilizing a quasi-experimental design, NNHWs drawn from 53 local government areas of Ogun and Oyo states participated in an intensive, multicomponent one-day stroke workshop. Stroke knowledge was evaluated before and after the training using a self-administered questionnaire.
Results
Out of a total of 210 NNHWs who participated in the session, 116 (55.2%) completed the pre-workshop questionnaire survey of stroke knowledge while 191 (91.0%) completed the post-workshop questionnaire survey. There were no statistically significant differences in the distribution of the age, gender and professional categories of the two groups. The participants' knowledge was significantly increased at the end of the training about stroke risk factors (p < 0.001), stroke symptoms (p < 0.001) and how stroke develops (p=0.009). The proportion of respondents who understood the FAST mnemonic increased from10.3% before the training to 90.6% at the end of the training (p < 0.001). The professional category of participants was associated with knowledge gain about swallowing test and thrombolysis.
Conclusion
Our data support the effectiveness of stroke-specific task-shifting training for non-neurologist health workers in a low resource setting. Interim studies with intermediate outcomes are needed to show that improved knowledge results in better care despite resource limitation. Randomized controlled trials will be useful to confirm findings and translate knowledge improvement into practical intervention.
Keywords: Stroke, Task shifting, Non-neurologists, Health workers, Nigeria, Africa
1. Background
There is a burgeoning epidemic of cardiovascular risk factors and stroke in Nigeria and sub-Saharan Africa with stroke accounting for up to a quarter of medical admissions in elderly adults [1] and over three quarters of neurologic admissions [2]. However, with an average of 0.04 neurologists per 100,000 population in Africa, there is inadequate human resource of skilled professionals to effectively tackle this burden and provide timely and efficient preventive, restorative and rehabilitative services [3–5].
In an effort to enhance the quality of stroke care across the continuum of healthcare services in all regions of the world, the World Stroke Organization (WSO) recently rolled out a global stroke care guidelines and action plan [6]. This advocates a three-tier approach to stroke care, the first of which (minimal health services) is operationalized largely by non-physician healthcare workers (NPHW) with sufficient basic stroke knowledge to educate the public, evaluate at-risk subjects, recognize stroke warning signs and decide on appropriate line of action [6].
Task-shifting describes a situation where a task normally performed by a physician is transferred to a health professional with a different or lower level of education and training, or to a person specifically trained to perform a limited task only [7]. Task-shifting is a novel strategy of proven efficacy to build relevant competences in NPHW to bridge the human resource gap in the provision of services for non-communicable diseases [7–9] and HIV/AIDS [10] in low and middle income countries. By restructuring the workforce in this way, task shifting enables more efficient use of the available human resources. Although we have previously reported insufficient stroke knowledge among African health workers [11], there is no documented evidence of stroke-specific task-shifting training for non-neurologist health workers (NNHWs) in Africa [12].
The objective of this study was to examine the effect of a program of intensive short-term task-shifting stroke training on the stroke knowledge of a cohort of Nigerian African non-neurologist health workers [NNHWs]. We hypothesized that an intensive, multi-component short-term stroke training would significantly enhance the knowledge of NNHWs about critical stroke symptoms, warning signs, risk factors and appropriate course of action for acute stroke.
2. Methodology
2.1. Study setting
Nigeria operates a three-tier health care system stratified into primary, secondary and tertiary health care levels. Of the three levels, two federal tertiary healthcare centers in south-western Nigeria, Federal Medical Centre, Abeokuta and University College Hospital, Ibadan in Ogun and Oyo states respectively are located in this setting and served as sites for this study.
2.2. Study design
This study utilized a quasi-experimental (pre-test and a post-test) design.
2.3. Study participants
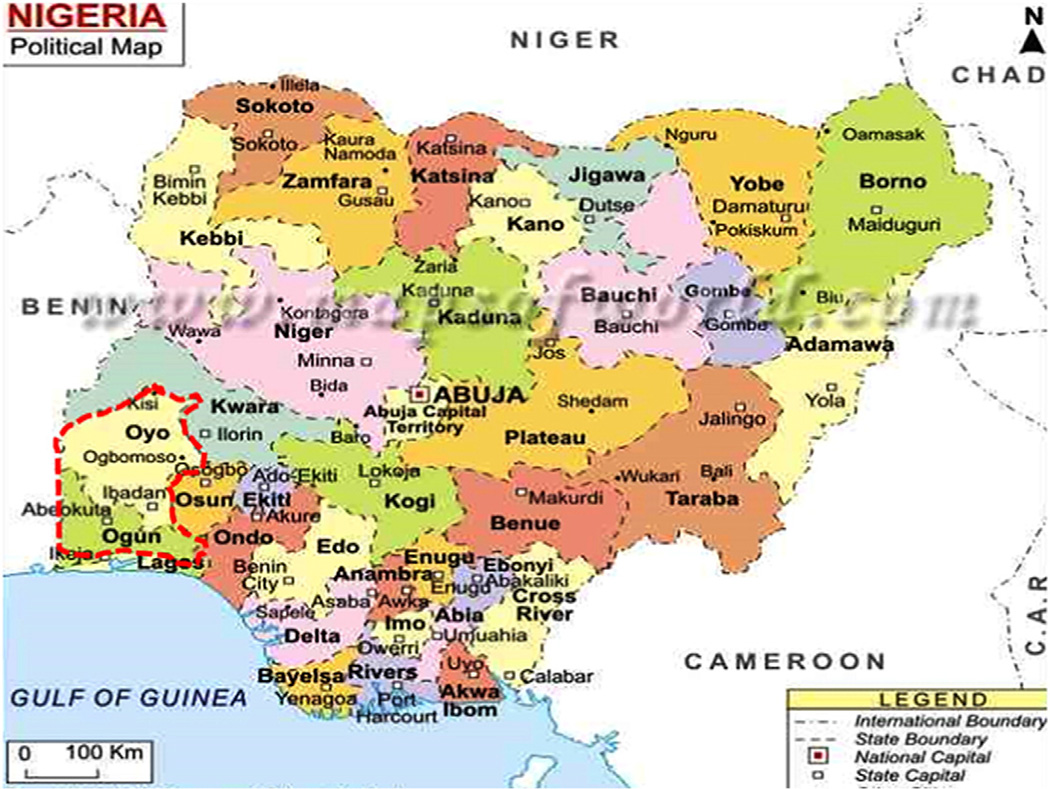
Two hundred and ten non-neurologist health workers [NNHWs] including medical officers, nurses and community health extension workers drawn from the combined 53 local government areas (LGAs) across Ogun and Oyo states (Fig. 1) participated in the study.
Fig. 1.
Map of Nigeria showing the two southwestern states of Ogun and Oyo with a total of 53 local government areas (LGAs) from which participants were drawn for the stroke task shifting training workshop.
2.4. Intervention activities
Participants were taken through a one-day 8 hour intensive basic stroke course having the sole aim of building their capacity for early recognition, resuscitation, appropriate and prompt referral of suspected stroke cases as well as preventive and basic rehabilitative care. The workshop curriculum covered topics including general introduction and burden of stroke in Nigeria, identification of stroke, stroke mimics, primary and secondary prevention of stroke, approach to early management of acute stroke and life after stroke. These elements of the education package aimed to empower the participants with the basic knowledge and competences to recognize potential cases of stroke and take appropriate quick decisions. To complement didactic presentations, an educational stroke documentary film developed by us and practical/interactive sessions on case vignettes were incorporated into the curriculum. Further incorporated into the curriculum was “FAST”, a mnemonic that represents stroke symptoms (“F” for “Face droop,” “A” for “Arm weakness,” “S” for Speech affected/slurred, and “T” for “Time to call 911”) and derived from the Cincinnati pre-hospital stroke scale [13] though other symptoms not part of the “FAST” mnemonic were also highlighted. These topics were facilitated by very experienced faculty members, senior neurologists and leaders of the Nigeria Stroke Society.
2.5. Evaluation activities
Participants' level of stroke knowledge was evaluated before and after the intervention, using a self-administered stroke literacy questionnaire previously developed by us [11]. The questionnaire was developed following a comprehensive review of previous studies on stroke knowledge and perception [11]. Potential items were identified and subsequently, a draft instrument was developed which included sociodemographic variables such as age, gender, marital status, highest educational qualification, professional category, as well as questions evaluating knowledge and perception of stroke cause, risk factors, how it occurs, treatment preference and some questions on management of stroke. The original draft instrument was pilot-tested on 40 health workers then in 2007 in another hospital followed by refinement of ambiguous or deletion of redundant questions before preparation of the final version of the questionnaire. For the current study, we added items on the FAST mnemonic as well as more items on stroke management such as neuroimaging as gold standard for stroke diagnosis, swallowing test, aspiration pneumonitis and the golden period of thrombolysis.
Administrative clearance to conduct and evaluate the training program was obtained from the Ogun and Oyo States Ministries of Health. At data acquisition and entry, records were handled confidentially and all processed data were anonymous.
2.6. Statistical analysis
To ascertain the comparability of the participants who partook of the pre-test and post-test, we compared their socio-demographic characteristics using the independent t test and chi square test for age and categorical variables respectively. We explored stroke knowledge responses relative to work category comparing pre- and post-performance within the strata. Because the questionnaires were completed anonymously, we did not undertake matched inferential statistical analyses restricted to those individuals who completed both pre-test and post-test.
3. Results
Out of a total of 210 NNHWs who participated in the session, 116 (55.2%) completed the pre-workshop questionnaire survey of stroke knowledge while 191 (91.0%) completed the post-workshop questionnaire survey. Table 1 shows the socio-demographic characteristics of the participants who completed the pre- and post-workshop surveys respectively, and these were similar with respect to age (p = 0.956), gender (p = 0.785) and work category (p = 0.859). Majority of the respondents (about 50%) consisted of nurses and community health extension workers (CHEWs).
Table 1.
Socio-demographic characteristics of training workshop participants.
| Variables | Pre-test (n = 116) |
Post-test (n = 191) |
Test-statistic | p-value |
|---|---|---|---|---|
| Age: mean (SD) years | 46.1 (8.2) | 46.2 (8.2) | 0.056a | 0.956 |
| Sex | 0.075 | 0.785 | ||
| Male | 50 (43.5) | 80 (41.9) | ||
| Female | 66(56.5) | 111 (58.1) | ||
| Religion | 1.396 | 0.237 | ||
| Christianity | 88 (76.5) | 156 (82.1) | ||
| Islam | 27 (23.5) | 35 (17.9) | ||
| Professional category | 2.582 | 0.859 | ||
| Nurse | 37 (33.0) | 76 (39.8) | ||
| CHEW | 18 (16.1) | 32 (16.8) | ||
| Medical officer | 9 (8.0) | 14 (7.3) | ||
| Snr medical officer | 17 (15.2) | 20 (10.5) | ||
| Chief medical officer | 7 (6.2) | 11 (5.8) | ||
| Consultant | 5 (4.5) | 6 (3.1) | ||
| Others | 19 (17.0) | 32 (16.8) |
Independent t-test; other comparisons were by chi square test.
Table 2 shows the effect of the training program on participants' knowledge of stroke risk factors, causes, symptoms, management principles and local epidemiology. Knowledge of participants about stroke risk factors (90.5% vs 99.0%, p < 0.001), stroke symptoms (79.3% vs 90.6%, p < 0.001) and how stroke develops (81.0% vs 95.3%, p=0.009)was significantly increased at the end of the training. Before the training, only 10.3% of respondents could identify the FAST mnemonic whereas at the end of the training, over 90% of respondents could identify the FAST mnemonic and its components and this represented a remarkable improvement (p < 0.001). There was also a significant improvement (89.8% vs 98.9%, p < 0.001) in the proportion of subjects who submitted that brain neuroimaging is gold standard for confirming a diagnosis of stroke.
Table 2.
Effect of the training program on participants' knowledge of stroke risk factors, causes, symptoms, management principles and local epidemiology.
| Variable | Pre-test | Post-test | χ2 test | ||
|---|---|---|---|---|---|
| No | % | No | % | p value | |
| No of risk factors correctly identified | 0.001 | ||||
| 0 | 2 | 1.7 | 1 | 0.5 | |
| 1–3 | 9 | 7.8 | 1 | 0.5 | |
| ≥4 | 105 | 90.5 | 189 | 99.0 | |
| Stroke develops througha | |||||
| Rupture of blood vessel | 94 | 81.0 | 173 | 90.6 | <0.001 |
| Blockage of blood vessel | 89 | 81.0 | 182 | 95.3 | <0.001 |
| Stroke symptoms correctly identified | 0.009 | ||||
| 0 | 2 | 1.7 | 0 | 0 | |
| 1–3 | 22 | 19.0 | 18 | 9.4 | |
| ≥4 | 92 | 79.3 | 173 | 90.6 | |
| Brain neuroimaging is gold standard for confirming a diagnosis of stroke |
<0.001 | ||||
| True | 97 | 89.8 | 187 | 98.9 | |
| False | 11 | 10.2 | 2 | 1.1 | |
| Knowledge of FAST mnemonic | |||||
| F | 13 | 11.2 | 177 | 92.7 | <0.001 |
| A | 14 | 12.1 | 174 | 91.1 | <0.001 |
| S | 21 | 18.1 | 176 | 92.1 | <0.001 |
| T | 13 | 11.2 | 174 | 91.1 | <0.001 |
| FAST | 12 | 10.3 | 173 | 90.6 | <0.001 |
| Aspiration is a common complication that may lead to death in stroke patients |
0.247 | ||||
| True | 99 | 85.3 | 171 | 89.5 | |
| False | 3 | 2.6 | 11 | 5.8 | |
| No response | 14 | 12.1 | 9 | 4.7 | |
| Swallowing test should be carried out before feeding a stroke patient |
<0.001 | ||||
| True | 71 | 61.2 | 166 | 86.9 | |
| False | 26 | 22.4 | 18 | 9.4 | |
| No response | 19 | 16.4 | 7 | 3.7 | |
| Cerebral decompression is appropriate after stroke event |
<0.001 | ||||
| True | 64 | 55.2 | 162 | 84.8 | |
| False | 19 | 16.4 | 12 | 6.3 | |
| No response | 33 | 28.4 | 17 | 8.9 | |
| Refer stroke patients for specialist care as soon as possible |
0.648 | ||||
| True | 108 | 93.1 | 184 | 96.3 | |
| False | 4 | 3.4 | 5 | 2.6 | |
| No response | 4 | 3.4 | 2 | 1.0 | |
| Blood clot in the brain can be lysed if patient presents within 4 h of stroke onset |
0.002 | ||||
| True | 73 | 62.9 | 164 | 85.9 | |
| False | 21 | 18.1 | 16 | 8.4 | |
| No response | 22 | 19.0 | 11 | 5.7 | |
| Stroke is the number 1 non-infectious cause of death in Nigeria |
0.739 | ||||
| True | 100 | 86.2 | 173 | 92.0 | |
| False | 10 | 8.6 | 15 | 15 | |
| No response | 6 | 5.2 | |||
| The number 1 risk factor for stroke in Nigeria is hypertension |
0.722 | ||||
| True | 111 | 95.7 | 183 | 99.5 | |
| False | 1 | 0.9 | 1 | 0.5 | |
| No response | 4 | 3.4 | – | ||
Multiple responses.
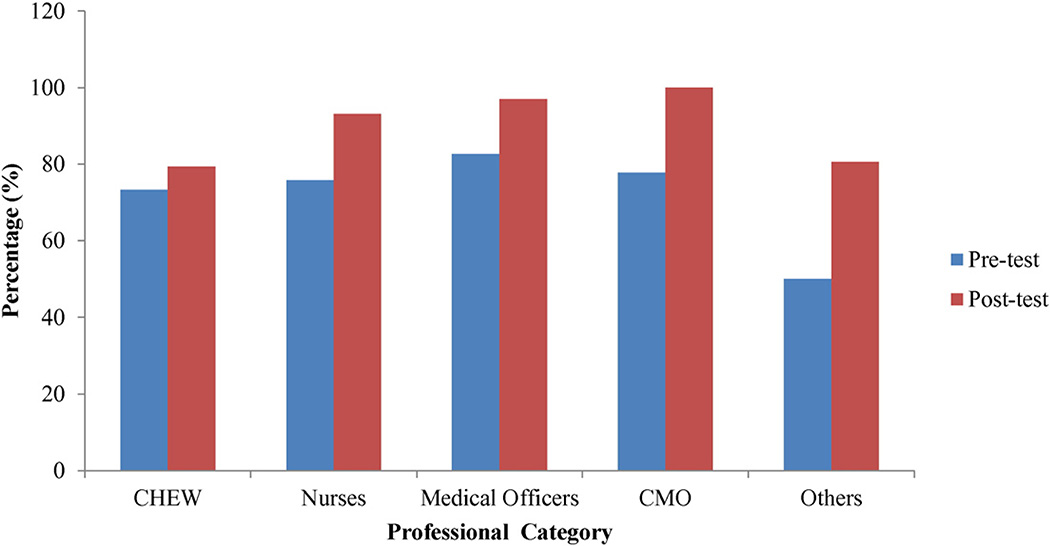
Although majority (87.4%) of respondents (85.3.%) before and (89.5%) after the training (p=0.247) identified aspiration as a common complication that may cause death in stroke patients, knowledge of the practice of swallowing test, a preventive approach, was significantly improved after the training (61.2% vs 86.9%, p < 0.001) (Fig. 2).
Fig. 2.
Association between respondents' professional category and knowledge of swallowing test before and after the training.
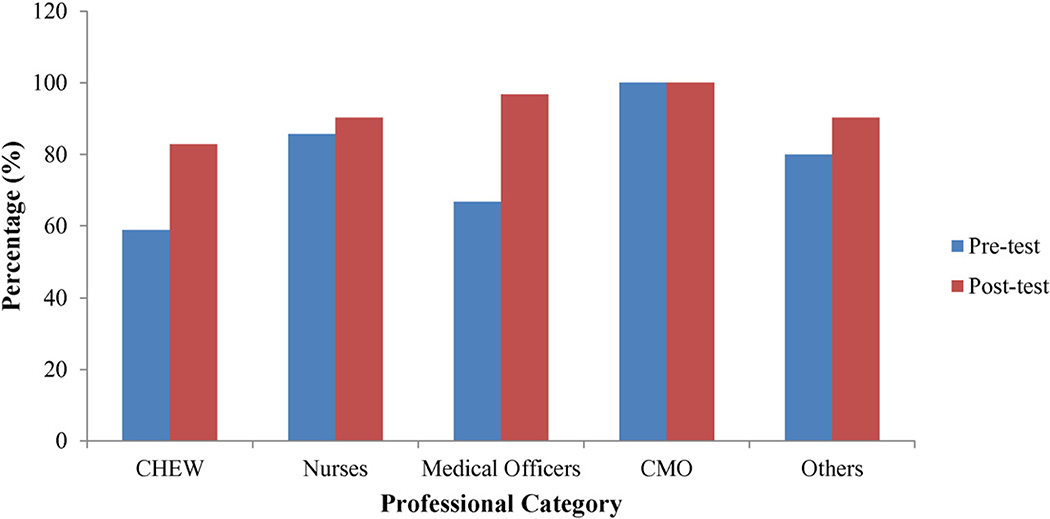
Majority of respondents (93.1%) before and (96.3%) after the training (p=0.648) submitted that stroke patients need to be referred for specialist care as soon as possible. However, there was remarkable improvement in their knowledge of cerebral decompression (55.2% vs 84.8%, p < 0.001) and thrombolysis (62.9% vs 85.9%, p = 0.002) (Fig. 3) as general and specific treatment approaches for stroke.
Fig. 3.
Association between respondents' professional category and knowledge of thrombolysis before and after the training.
Respondents demonstrated a high level of awareness of stroke being the number one non-communicable cause of death and of hypertension being the dominant risk factor for stroke among Nigerians, though this was not significantly influenced by the training (Table 2).
Figs. 2 and 3 show the relationship between respondents' work category and knowledge of swallowing test and thrombolysis before and after the workshop, demonstrating knowledge increment in both aspects of acute stroke management.
4. Discussion
In this study, we found that utilizing an intense short term multimodal task-shifting educational intervention, knowledge of risk factors and warning symptoms of stroke, how stroke develops, the FAST mnemonic and some approaches to stroke management was significantly improved in a cohort of non-neurologist health workers drawn from primary and secondary healthcare centers based in the 53 local government areas of two southwestern states of Nigeria (Fig. 1).
Improved stroke literacy among these health workers, majority of whom were nurses and community health extension workers empowers them in early detection of possible cases of stroke in their community-based clinics and health centers with minimal health services [6,14,15].
Improvement in the respondents' knowledge of acute management strategies including cerebral decompression and swallowing test could enhance their ability to institute appropriate early management steps (where necessary) in cases of suspected acute stroke with implications for the eventual outcome [6]. Furthermore, closing the stroke knowledge gap of health workers enhances their capacity to provide effective stroke education to members of the community [11,16].
A significant implication of the findings of this study is that an effective task-shifting stroke training of NNHWs constitutes a robust strategy to fill up the human resource gap for prompt stroke diagnosis and early care across the continuum of care as prescribed by the recent World Stroke Organization global stroke care guidelines and action plan [6,17]. This is particularly important for the first-tier of care, minimal health services, where non-physician health workers are often the dominant staff available. Task-shifting approaches have been successfully engaged in developing nurse-led diabetes and hypertension, epilepsy as well as HIV/AIDS care in several African countries including Cameroun, Ghana, Kenya [8,18,19]. Furthermore, the World Health Organization has recognized task shifting as an effective and pragmatic approach to tackling the chronic shortage of health workers, especially, in resource poor settings [20,21]. The World Federation of Neurology has also supported task shifting approaches as a measure to mitigate the overwhelming shortage of neurologists in Africa by supporting the publication of the educational material ‘Where there is no neurologist’ among other efforts [22,23]. The current study provides the first evidence for a stroke-specific task shifting capacity building in sub-Saharan Africa, a region currently witnessing a rapid expansion of the burden of NCDs including stroke despite scarce skilled human resources for health [24].
This study, nevertheless, has limitations. Although the demographic characteristics of participants who partook of the pre- and post-training evaluation of stroke literacy were similar, a lower proportion of respondents took part in the pre-test and this could have influenced the baseline parameters against which improvement was measured post-intervention. Furthermore, paired analysis of pre- and post-test respondents would have been ideal, but for the anonymous response of workshop participants in the two arms of the survey. The likelihood of the significant improvement in stroke knowledge recorded in the post-test being due to an inherently more knowledgeable post-test cohort is a possible confounder but the absence of any significant demographic differences in the pre- and post-test responders is reassuring. Long term retention of knowledge gained was not reported in the present study, although the cohort of NNHWs is now being followed up to assess the medium- and long-term impact of the training on their stroke care practices in their respective locations across the two states.
In summary, we have shown data that support the effectiveness of a stroke-specific task-shifting training for non-neurologist health workers in a low resource setting However, some interim studies with intermediate outcomes are needed to show that improved knowledge results in better care despite limitations of relevant resources. With this, randomized controlled trials may further be undertaken to confirm these findings and assess behaviors related to improved health workers' stroke literacy and translate knowledge improvement to action. Studies are also needed to evaluate the impact of longer multipronged stroke educational intervention on stroke care practices, including quality of care indicators as prescribed in the WSO guidelines.
Acknowledgments
This project was undertaken with a special educational grant from the World Federation of Neurology and the World Stroke Organization. We acknowledge the support of the staff of the Ogun and Oyo States Ministries of Health in mobilizing health workers for the Stroke Training Program. Our work is supported by U01 NS079179 (THRIVES) and U54 HG007479 (SIREN) grants from the National Institutes of Health (USA).
Footnotes
Authors' contributions
This study was conceptualized and designed by ROA, MOO and PBA. FTT, YO and AO contributed to the Stroke Training Program. Data was collected by EU, FMO, OA, OA and MA. JOA analyzed the data and contributed to data interpretation. ROA wrote the first draft of the manuscript while all authors revised and made intellectual contributions to subsequent versions. Final version of the manuscript was approved by all authors.
References
- 1.Akinyemi RO, et al. Contribution of noncommunicable diseases to medical admissions of elderly adults in Africa: a prospective, cross-sectional study in Nigeria, Sudan, and Tanzania. J. Am. Geriatr. Soc. 2014;62(8):1460–1466. doi: 10.1111/jgs.12940. [DOI] [PubMed] [Google Scholar]
- 2.Owolabi LF, et al. Pattern of neurological admissions in the tropics: experience at Kano, Northwestern Nigeria. Ann. Indian Acad. Neurol. 2010;13(3):167–170. doi: 10.4103/0972-2327.70875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owolabi MO, Bower JH, Ogunniyi A. Mapping Africa's way into prominence in the field of neurology. Arch. Neurol. 2007;64(12):1696–1700. doi: 10.1001/archneur.64.12.1696. [DOI] [PubMed] [Google Scholar]
- 4.Norrving B, Kissela B. The global burden of stroke and need for a continuum of care. Neurology. 2013;80(3 Suppl 2):S5–S12. doi: 10.1212/WNL.0b013e3182762397. [DOI] [PubMed] [Google Scholar]
- 5.Ward AB, et al. Evaluation of the Post Stroke Checklist: a pilot study in the United Kingdom and Singapore. Int. J. Stroke. 2014;9(Suppl A100):76–84. doi: 10.1111/ijs.12291. [DOI] [PubMed] [Google Scholar]
- 6.Lindsay P, et al. World Stroke Organization global stroke services guidelines and action plan. Int. J. Stroke. 2014;9(Suppl A100):4–13. doi: 10.1111/ijs.12371. [DOI] [PubMed] [Google Scholar]
- 7.Joshi R, et al. Task shifting for non-communicable disease management in low and middle income countries—a systematic review. PLoS One. 2014;9(8):e103754. doi: 10.1371/journal.pone.0103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Labhardt ND, et al. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv. Res. 2010;10:339. doi: 10.1186/1472-6963-10-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ogedegbe G, et al. A cluster-randomized trial of task shifting and blood pressure control in Ghana: study protocol. Implement. Sci. 2014;9:73. doi: 10.1186/1748-5908-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callaghan M, Ford N, Schneider H. A systematic review of task-shifting for HIV treatment and care in Africa. Hum. Resour. Health. 2010;8:8. doi: 10.1186/1478-4491-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akinyemi RO, et al. Knowledge and perception of stroke amongst hospital workers in an African community. Eur. J. Neurol. 2009;16(9):998–1003. doi: 10.1111/j.1468-1331.2009.02666.x. [DOI] [PubMed] [Google Scholar]
- 12.Ovbiagele B. Phone-based intervention under nurse guidance after stroke: concept for lowering blood pressure after stroke in Sub-Saharan Africa. J. Stroke Cerebrovasc. Dis. 2015;24(1):1–9. doi: 10.1016/j.jstrokecerebrovasdis.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams O, et al. Child-mediated stroke communication: findings from Hip Hop Stroke. Stroke. 2012;43(1):163–169. doi: 10.1161/STROKEAHA.111.621029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mosley I, et al. What is stroke symptom knowledge? Int. J. Stroke. 2014;9(1):48–52. doi: 10.1111/ijs.12024. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh HC, et al. Development of an educational program for staffs of emergency medical service to improve their awareness of stroke within 3 hours of symptom onset: a pilot study. Acta. Neurol. Taiwan. 2013;22(1):4–12. [PubMed] [Google Scholar]
- 16.Adelman EE, et al. Stroke awareness among inpatient nursing staff at an academic medical center. Stroke. 2014;45(1):271–273. doi: 10.1161/STROKEAHA.113.002905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lehmann U, et al. Task shifting: the answer to the human resources crisis in Africa? Hum. Resour. Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kredo T, et al. Task shifting from doctors to non-doctors for initiation and maintenance of antiretroviral therapy. Cochrane Database Syst. Rev. 2014;7:CD007331. doi: 10.1002/14651858.CD007331.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kengne AP, et al. Task shifting in the management of epilepsy in resource-poor settings. Epilepsia. 2010;51(5):931–932. doi: 10.1111/j.1528-1167.2009.02414.x. [DOI] [PubMed] [Google Scholar]
- 20.Campbell C, Scott K. Retreat from Alma Ata? The WHO's report on Task Shifting to community health workers for AIDS care in poor countries. Glob. Public Health. 2011;6(2):125–138. doi: 10.1080/17441690903334232. [DOI] [PubMed] [Google Scholar]
- 21.Geneva: World Health Organization; 2012. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions Through Task Shifting. [PubMed] [Google Scholar]
- 22.Birbeck GL, Munsat T. Neurologic services in sub-Saharan Africa: a case study among Zambian primary healthcare workers. J. Neurol. Sci. 2002;200(1–2):75–78. doi: 10.1016/s0022-510x(02)00132-6. [DOI] [PubMed] [Google Scholar]
- 23.Munsat T, et al. International issues: educational programs of the World Federation of Neurology. Neurology. 2009;72(10):e46–e49. doi: 10.1212/01.wnl.0000344183.62422.b2. [DOI] [PubMed] [Google Scholar]
- 24.Moran A, et al. The epidemiology of cardiovascular diseases in sub-Saharan Africa: the Global Burden of Diseases, Injuries and Risk Factors 2010 Study. Prog. Cardiovasc. Dis. 2013;56(3):234–239. doi: 10.1016/j.pcad.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]