Abstract
Objectives
A wide range of patient benefits have been attributed to single room hospital accommodation including a reduction in adverse patient safety events. However, studies have been limited to the US with limited evidence from elsewhere. The aim of this study was to assess the impact on safety outcomes of the move to a newly built all single room acute hospital.
Methods
A natural experiment investigating the move to 100% single room accommodation in acute assessment, surgical and older people’s wards. Move to 100% single room accommodation compared to ‘steady state’ and ‘new build’ control hospitals. Falls, pressure ulcer, medication error, meticillin-resistant Staphylococcus aureus and Clostridium difficile rates from routine data sources were measured over 36 months.
Results
Five of 15 time series in the wards that moved to single room accommodation revealed changes that coincided with the move to the new all single room hospital: specifically, increased fall, pressure ulcer and Clostridium difficile rates in the older people’s ward, and temporary increases in falls and medication errors in the acute assessment unit. However, because the case mix of the older people’s ward changed, and because the increase in falls and medication errors on the acute assessment ward did not last longer than six months, no clear effect of single rooms on the safety outcomes was demonstrated. There were no changes to safety events coinciding with the move at the new build control site.
Conclusion
For all changes in patient safety events that coincided with the move to single rooms, we found plausible alternative explanations such as case-mix change or disruption as a result of the re-organization of services after the move. The results provide no evidence of either benefit or harm from all single room accommodation in terms of safety-related outcomes, although there may be short-term risks associated with a move to single rooms.
Keywords: health facility moving, hospitals, patient safety, quality of health care
Introduction
In the UK, National Health Service providers are encouraged by Department of Health guidance to provide higher proportions of single room accommodation (an aim of 50%) in any new hospital builds. Although as yet, there are few wards or hospitals in the UK with all single room accommodation and the opportunities for evaluation have been limited, in recent years an increasing number of such hospitals have been built. Interest in the role of all single room accommodation has increased, with the Department of Health undertaking investigations into single room designs and ward layout. There is a wide range of potential advantages attributed to single room accommodation including fewer medication errors, and improved patient outcomes such as reduced infection rates and faster patient recovery rates.1,2 Although there are significant potential benefits claimed from providing single room accommodation, to date, little empirical work on single rooms has been undertaken in the UK, with most research emanating from the US and Scandinavia.
The mechanism hypothesized for fewer infections in single rooms is the reduction of person-to-person contacts as well as limiting the spread of infection by person-surface-person contacts.3 Two rigorous systematic reviews have been conducted on the association of single room accommodation with healthcare-associated infections. Dettenkofer et al.4 included 17 historic and prospective cohort studies between 1975 and 2001 in their systematic review. The majority of studies were conducted in intensive care units (ICU, n=9), followed by surgical wards (n=4), isolation units (n=2) and general hospitals (n=2). Three out of nine studies in ICUs reported a reduction in infections, while no reduction was found for postoperative wound infections in the four studies of surgical wards. No reduction in infections was documented for isolation wards, although increasing the number of beds per room led to an increased number of infections in acute medical wards. A later review by Whitehead et al.5 identified two additional studies in neonatal and paediatric intensive care settings between 2001 and 2006 showing a reduction of the mean number of infections in isolation or single rooms in comparison to multiple-bed bays. More recent studies, all conducted in ICUs6–9 have shown a reduction in several types of infections including meticillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile (C. diff). In summary, an association between single room accommodation and decreased infection rates has been shown in intensive care but not elsewhere, indicating the need for research outside intensive care.
Other adverse events such as falls or medication errors have been identified as being potentially affected by single rooms.3,10 However, the evidence is scant. In their systematic review, van de Glind et al.11 could only identify opinion articles which claimed a decreased rate of medication errors due to improved patient registration and reduced likelihood of misidentifying patients in single rooms. It is recognized that a number of environmental factors are associated with fall rates,2 and anecdotal evidence suggests a potential increased risk of falls in single rooms because nurses and fellow patients have less opportunity to see those at risk and keep them under surveillance leading to reduced opportunity to detect imminent falls. This was also confirmed in the qualitative part of our study.12,13 Two studies only available as an abstract or letter indicate an increase of falls after moving to single room accommodation. However, neither analysis considered case-mix differences or included control sites.14,15
The aims of the current study were to investigate the impact of moving to a new hospital building with 100% single room accommodation on infection rates and nurse-related patient safety outcomes.
Methods
Design
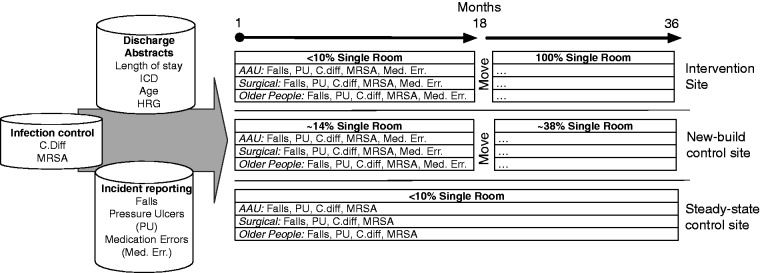
We conducted a before-and-after study with non-equivalent controls16 to isolate the effects of caring for patients in 100% single room accommodation on infection and safety outcomes. This ‘difference in difference’ approach is one of the recommended approaches according to the MRC guideline on natural experiments.12 The main risks of bias in this approach are changes to the composition of unmeasured characteristics over time, and between exposed and unexposed groups. To overcome this problem, not only safety event rates (e.g. falls or pressure ulcers) were scrutinized but also changes to underlying patient characteristics like length of stay and case mix (according to Healthcare Resource Groups (HRGs)). However, the data did not allow us to link safety events with individual patient discharge data, which would have provided the opportunity for patient-level risk adjustment. This analysis is part of a larger mixed-methods study, which also investigated the impact of 100% single room accommodation on staff and patient perceptions as well as associated costs.13,17 Figure 1 provides an overview of the study design, the different sites and data sources.
Figure 1.
Overview of data sources and design features.
C. diff: Clostridium difficile; MRSA: meticillin-resistant Staphylococcus aureus.
Setting
The study was undertaken in a large multisite NHS acute Trust in the South of England, with two NHS Trusts, also in the South of England, as controls. The study considered the effects of moving a number of services from existing hospitals with low provision of single rooms into a new hospital which provided 100% single room inpatient accommodation. In the overall project, four wards (acute assessment, older people, surgical and maternity) were selected for in-depth scrutiny and to represent a range of different patient populations and care settings. Of these, three (acute assessment, older people, surgical) were matched with wards in control hospitals for the present analysis. Because of the low incidence of pressure ulcers, falls and infections, maternity wards were excluded from further analyses. We looked for two different comparator sites with the following characteristics: steady state control, with no change, but planning to move in the future (indicating wards that were nearing the end of their expected useful life, to ensure comparability with the intervention site); and new build control, having moved to a new building with mixed accommodation with about 50% single rooms (as a control for changes associated with a move to a new facility versus 100% single rooms). After contacting several potential NHS trusts, one hospital (no move, planned move in 2014) and another hospital (new building, mixed accommodation, moved in 2011) agreed to participate in the study.
The intervention site had less than 10% of single rooms before the move to 100% single room accommodation. The wards at the new build control site before the move consisted of eight-bedded, three-bedded and single rooms. With the move, the proportion of single rooms increased from 14% to 38% in the included wards. The steady state control site had less than 10% single rooms.
Data collection
Trusts were asked to provide retrospective routine data on safety events (falls, medication administration errors, pressure ulcers) and hospital-acquired infections for a three-year period from January 2010 to December 2012. Outcome data were requested for wards at the old hospital site and their succeeding wards at the new 100% single room accommodation hospital. The chosen outcomes are all regarded as being sensitive to the quality and quantity of nursing care provided, with some (falls, infections, medication errors) reflecting specific challenges or hypothesized advantages attributed to single rooms.18 The same data were requested from wards of the same type at each of the control sites.
Routine data on safety events are captured in various ways by either incident reports, infection control monitoring or administrative sources like discharge abstracts. Data were received from several departments within each trust, including finance, infection control and nursing management. Definitions of the incidents recorded in these routine quality data were standardized. For example, pressure ulcers are classified using a grading system.
Handling missing data
Because of the range of data sources, conducting the analysis at the ward level and because of changes in the data infrastructure during the study period, not all data were available for all wards throughout the investigation period. Thirty-six-month periods of data for falls, pressure ulcers, medication error, C. diff and MRSA rates were available for a total of 15 time series at three wards (acute assessment, older people and surgical ward) at the 100% single room site. For the steady state control site, the reporting system for medication errors changed during the study period, so no monthly unit level data for medication errors were available. For the new build control site, only C. diff and MRSA data were available for the full study period, with 26–33-month data available for falls, pressure ulcers and medication errors. Also, only 32 months of administrative data were available, which was crucial to determine the denominator (bed days) thereby reducing the period that could be matched to outcome data. To impute the missing bed days, we calculated the mean and standard deviation of the previous five months (all post-move) and used these values assuming a normal distribution to randomly generate and impute four aggregate values. For missing outcome data, listwise deletion was used, which subsequently reduced the number of available time points.
Contextual data
Where possible trends were compared with either trust level or national trends data in order to assess if trends were potentially attributable to single rooms or part of a secular trend. For falls, we assessed changes in the underlying risk of the trust population at the 100% single room intervention site between April 2011 and September 2013. Patients at risk of a fall were defined as having either one of the Charlson comorbidity diagnoses19 or having a diagnosis associated with a high fall risk20 or being 70 years of age or older. The detailed international classification of diseases (ICD) codes used are described elsewhere.17 We also compared C. diff and MRSA standardized rates with the national mandatory reporting data from Public Health England.
Analytical approach
The comparison of trends in infections or safety events could be conducted at the individual, ward or hospital level. However, safety incidents like falls, as well as hospital-acquired infections, are usually recorded in dedicated reporting systems, which only contain information about the harmed patients thereby excluding information about the overall population of the ward or the trust. While individual-level data would allow risk adjustment, and therefore reduce selection bias in the comparison of trusts or wards, these data were not available at all three sites. A different way of addressing selection bias is based on risk stratification, which groups patients in strata with similar characteristics. Analysing data at the ward level by comparing wards of the same type (e.g. medical ward) partially achieves this goal since most wards have specific populations where patients share similar characteristics. We therefore analysed falls and pressure ulcer incidents and hospital-acquired infection rates at the ward level.
We used administrative data containing information on: patients’ age, length of stay, primary diagnoses based on the ICD, version 10,21 HRG codes and diagnoses used in the Charlson comorbidity index,22 to match wards with approximately similar characteristics between trusts and to identify changes in their patient populations over time.
As data were in the form of monthly rates, the analysis was conducted as an interrupted time-series analysis augmented by statistical process control charts (SPCCs) in order to analyse changes in safety events and hospital-acquired infections before and after the move or over the same period of time for the steady state control site. SPCCs plot the outcome of interest over time on a chart, which contains a centre line (representing the mean) and upper and lower confidence limits, which are defined as three standard deviations below or above the centre line. SPCCs allow differentiation between common cause variation, which refers to random error as opposed to special cause variation which arises from genuine changes in the level of the variable of interest.23 Several rules identify special cause variation, two of which are of particular interest to identify changes in safety events or infection rates after the move: one data point outside the confidence limits; and eight or more consecutive data points above the centre line.23
For all outcomes, U-charts with Cornish-Fisher expansion were used, which are appropriate to handle varying sample sizes and count data with a Poisson distribution.24 U-charts is a type of SPCC. All charts were plotted with the improved quality Control Charts (IQCC) package25 in R.26
Assessing trends before and after the move, or identifying differences between trusts and associating these trends with a single room effect, requires three conditions to be met: the outcomes of interest (safety events, hospital-acquired infections) change after the intervention (single room accommodation is introduced); the core characteristics of the patient population remain the same over time and any identified effect is strongest at the 100% single room site, weaker at the new build control site with mixed accommodation and not present at the steady state control site.
Based on these considerations, we first analysed the before-and-after data from the 100% single room site before comparing with the comparator sites to assess whether there was a ‘single room’ effect.
Results
Variation associated with the move to 100% single room accommodation hospital at the intervention site
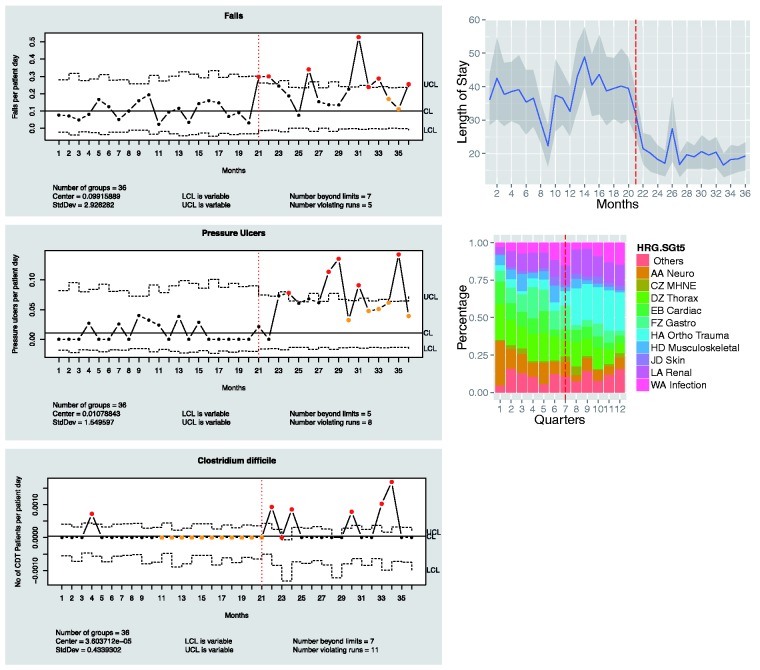
Five of the 15 time series revealed special cause variation that coincided with the move and could be associated with the new 100% single room site. In the older people’s ward, falls, pressure ulcers and C. diff rates increased. Two criteria for special cause variation were met: 12 measurement points above the upper control limits (indicated in red) and more than eight consecutive points above the centre line (indicated in yellow). However, the case mix of the older people ward also changed substantially in the same period: the length of stay decreased from 37 to 20 days and the proportion of orthopaedic trauma patients (orthopaedics/trauma HRG subgroup) increased from 4.6% to 24.8% (Figure 2).
Figure 2.
U-chart with CF-expansion for older people ward moving to move to 100% single room accommodation: falls, pressure ulcers and Clostridium difficile (left); length of stay and HRG subgroups (right). Dashed line at 21 months represents the time of the move.
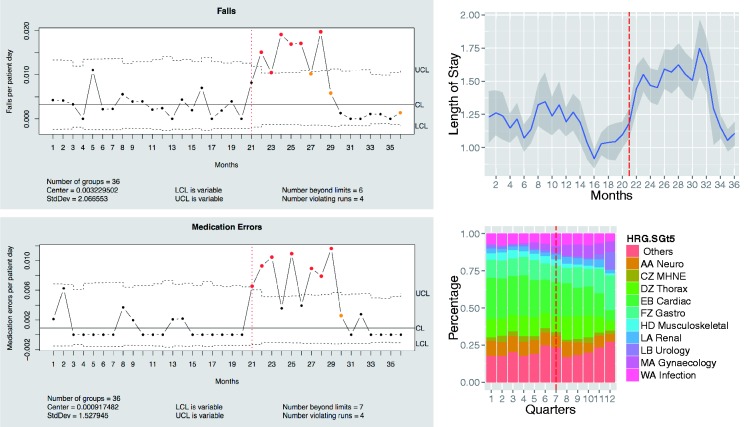
In the acute assessment ward at the 100% single room accommodation site, falls and medication errors increased temporarily but returned to pre-move levels after 7–9 months (Figure 3). In the same period, length of stay also increased from 1.2 to 1.4 days, and some changes in case mix could be observed such as a reduction by 7% in the cardiac HRG group.
Figure 3.
U-chart with CF-expansion for acute assessment ward moving to 100% single room accommodation hospital: falls and medication errors (left); length of stay and HRG subgroups (right). Dashed line at 21 months represents the time of move.
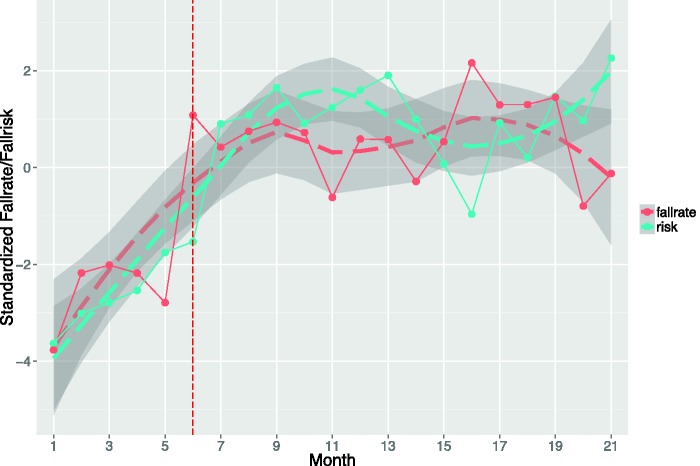
From April 2011 to December 2012, the fall risk for the intervention site increased in close proportion to the fall rate (see Figure 4). The fall risk and the fall rate were strongly positively associated (r = 0.68) indicating that although there had been a clear sustained increase in the rate of falls, it was not possible to attribute this clearly to single rooms given the overall increase in the proportion of patients at risk of falls.
Figure 4.
Trust level comparison between fall rate and fall risk at single room site.
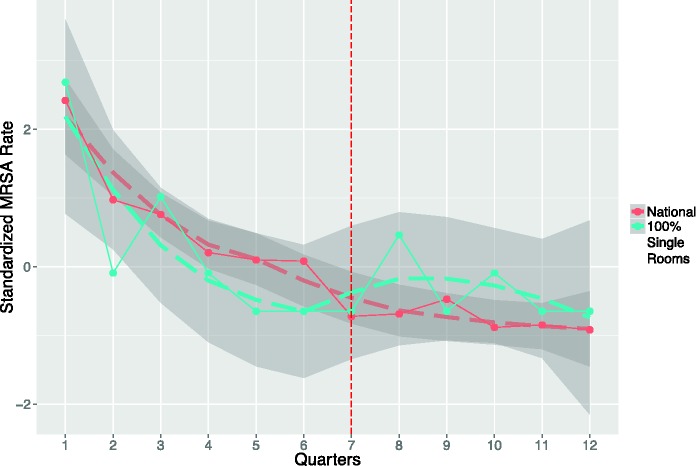
Figure 5 shows that MRSA infections decreased from 279 cases in the first quarter of 2010 to 92 in the fourth quarter of 2012 at the 100% single room intervention site. Trust-level data for C. diff are not publicly reported, but the overall national trend is similar: the trust apportioned number of infections decreased from 3489 (Q1, 2010) to 1525 (Q4, 2012), which represents a reduction of 56% in the three-year period.
Figure 5.
Comparison between national and trust-level MRSA rate at single room site.
Special cause variation at the new build control site
Fifteen time series were available across the three wards and five outcomes at the new build control site with lengths varying from 24 to 36 months (not presented). No special cause variation could be identified in any ward that could be attributed to the move to the new build (not displayed). Although there were special cause variation events, these were either single time points below or above the control limits or violating runs (seven consecutive runs below/above the centre line) did not coincide with the move. These special cause variation events were therefore discarded as they were not potentially attributable to the move or to an increase in the proportion of single rooms.
Special cause variation at the steady state comparator site
Twelve 36-month time series across the three wards for falls, pressure ulcers, MRSA and C. diff rates were available from the steady state control site. Various special cause variations were present in the older people’s ward and the acute assessment unit. For example, the fall rate on the older people’s ward declined while the pressure ulcer rate on the acute assessment ward increased. In both cases, the patient population changed (not displayed) to some extent, however, other factors might have played a role too.
Discussion
The analysis included 30 time series where the effect of an increasing proportion of single rooms could have been observed (three wards and five outcomes at the single room and the mixed accommodation site). Five time series showed special cause variation following a move to sites with more single room accommodation, all at the 100% single room site. Three time series showing an increase in falls, pressure ulcers and C. diff infections on the older people’s ward at the 100% single room site could be related to a change in case mix rather than the move to single rooms, and no similar changes were observed at the new build control site.
The only time series with special cause variation that coincided with the move where there was no substantial case-mix changes was at the acute assessment unit at the 100% single room site where there were increases in falls and medication errors. Although this could indicate an effect of single room accommodation, the increase was only temporary. Both fall and medication error rates decreased to their previous levels 6–9 months after the move. This temporary peak was not observed at the new build mixed accommodation site. The temporary nature of this increase and the lack of confirmation at the mixed accommodation control site support an alternative explanation. This increase in adverse safety events was probably more related to disruption in the workflow than to single rooms. This disruption is most likely to be associated with a move to any new environment and the need to adjust work patterns. While some of the disruptions and need for adaptation may be associated with the specific environment (i.e. single rooms), the fact that increases were temporary and no similar pattern was observed in the control wards which also experienced a move and an increase in single beds, suggests that it is not inevitable and/or that the increased risk is not intrinsically associated with single rooms. It may be avoidable and it certainly seems that, given time, adaptations were made to reduce it.
Our study adds to the literature in two ways: in common with a small number of other studies,4 we did not find a single room effect in surgical and general care settings; and we generated stronger evidence by adding comparison and comparison with national trends sites rather than the simple before-and-after designs of most studies in the field. In the absence of opportunities to undertake randomized controlled trials, a quasi-experimental approach combining time-trend analysis, individual-level risk adjustment, comparison sites and contextual data seems the most promising approach to critically analyse the issue of single room accommodation in future studies.
The patient safety and infection control outcomes provide only one perspective on the potential effects of single rooms. Other parts of our study indicate more pronounced differences, both positive and negative, in terms of patient and staff experience, but with little or no change in costs.13
Limitations
While more hospitals are moving to a greater proportion of single rooms in the UK, at the time of data collection, it was a challenge to recruit control hospitals and it was almost impossible to get the timing right to recruit those moving to a new build. It would have been desirable to include a larger sample of hospitals either those which had made similar moves or as control sites, but this was not possible. It was only possible to use aggregate data without individual risk adjustment because most of the safety events data (e.g. falls, pressure ulcers) could not be linked to individual patient characteristics. An alternative approach would have been to pool before-and-after data and test for differences. However, this would not have allowed us to identify and consider the implications of the patterns of change over time. A time series-based approach, using SPCCs, was the most appropriate given the data available.27 While definitions of ‘incidents’ in the routine quality data are standardized, the approaches to gathering data may not be. There is a risk of under-reporting of incidents. However, as the key aim was not to compare hospitals but to scrutinize (differences in) changes within trusts over time, this weakness was less important.
Conclusions
For all special cause variations in safety events that coincided with the move to single rooms, we found plausible alternative explanations such as case-mix changes or disruption through the re-organization of the services after the move. Therefore, we conclude that these results provide no evidence of either benefit or harm arising from use of 100% single room accommodation in terms of these safety-related outcomes. While the results of a single observational study with intrinsic limitations cannot conclusively demonstrate no safety effect, the results correspond with the wider literature, which shows a link between single rooms and reduced infection rates in intensive care but not in general medical or surgical populations.4 The transient rise in falls associated with the move to all single rooms suggests that there is a need to mitigate risk during any transition period. Further investigation is warranted to determine whether the increase in risk is associated with a temporary disruption of work patterns or with an ongoing need to alter work patterns to reduce risk in single rooms.
Data sharing
No additional data available.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval
Ethical approval was obtained from King’s College London Psychiatry, Nursing and Midwifery Research Ethics Sub-Committee (approval granted January 2010 and for Phase 2 in January 2012 ref. PNM/09/10-30).
Funding
This project was funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (project number 10/1013/42). The views and opinions expressed are those of the authors and do not necessarily reflect those of the Health Services and Delivery Research Programme, NIHR, the NHS or the Department of Health.
Competing interests
None declared
References
- 1.Phiri M. One patient one room – theory & practice: an evaluation of the leeds nuffield hospital, Sheffield, UK: NHS Estates, 2004. [Google Scholar]
- 2.Ulrich RS, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. Herd 2008; 1: 61–125. [DOI] [PubMed] [Google Scholar]
- 3.Zimring C, Joseph A, Choudhary R. The role of the physical environment in the hospital of the 21st century: a once-in-a-lifetime opportunity, Concord, CA: The Center for Health Design, 2004. [Google Scholar]
- 4.Dettenkofer M, Seegers S, Antes G, et al. Does the architecture of hospital facilities influence nosocomial infection rates? A systematic review. Infect Control Hosp Epidemiol 2004; 25: 21–25. [DOI] [PubMed] [Google Scholar]
- 5.Whitehead S, Bending M, Lowson K, et al. Cost-effectiveness of hospital design: options to improve patient safety and wellbeing, York, UK: Health Economics Consortium (YHEC), 2011. [Google Scholar]
- 6.Bracco D, Dubois M-J, Bouali R, et al. Single rooms may help to prevent nosocomial bloodstream infection and cross-transmission of methicillin-resistant Staphylococcus aureus in intensive care units. Intensive Care Med 2007; 33: 836–840. [DOI] [PubMed] [Google Scholar]
- 7.Cheng V, Tai J, Chan W, et al. Sequential introduction of single room isolation and hand hygiene campaign in the control of methicillin-resistant Staphylococcus aureus in intensive care unit. BMC Infect Dis 2010; 10: 263–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonizzoli M, Bigazzi E, Peduto C, et al. Microbiological survey following the conversion from a bay-room to single-room intensive care unit design. J Hosp Infect 2011; 77: 84–86. [DOI] [PubMed] [Google Scholar]
- 9.Teltsch DY, Hanley J, Loo V, et al. Infection acquisition following intensive care unit room privatization. Arch Intern Med 2011; 171: 32–32. [DOI] [PubMed] [Google Scholar]
- 10.Huisman ERCM, Morales E, van Hoof J, et al. Healing environment: a review of the impact of physical environmental factors on users. Build Environ 2012; 58: 70–80. [Google Scholar]
- 11.van de Glind I, de Roode S, Goossensen A. Do patients in hospitals benefit from single rooms? A literature review. Health Policy 2007; 84: 153–161. [DOI] [PubMed] [Google Scholar]
- 12.Craig P, Cooper C, Gunnell D. Using natural experiments to evaluate population health interventions, Glasgow, UK: Medical Research Council, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maben J, Griffiths P, Penfold C, et al. One size fits all? Mixed methods evaluation of the impact of 100% single room accommodation on staff and patient experience, safety and costs. BMJ Qual Saf 2015; DOI:10.1136/bmjqs-2015-004265. [DOI] [PMC free article] [PubMed]
- 14.Okeke J, Daniel J, Naseem A, et al. Impact of all single rooms with ensuite facility in an acute care hospital in Wales (UK). Age Ageing 2013; 42(Suppl 3): 1–11. [Google Scholar]
- 15.Ugboma I, Drahota AK, Higgins B, et al. Effect of bedroom size on falls in hospital: does one size fit all? J Am Geriatr Soc 2011; 59: 1153–1154. [DOI] [PubMed] [Google Scholar]
- 16.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference, Boston, MA: Houghton Mifflin, 2001. [Google Scholar]
- 17.Maben J, Griffiths P, Penfold C, et al. Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation. Health Serv Deliv Res 2015; 3: 254–254. [PubMed] [Google Scholar]
- 18.Griffiths P, Jones S, Maben J, et al. State of the Art Metrics for Nursing: a rapid appraisal, King's College London, UK: National Nursing Research Unit, 2008. [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 20.Brand CA, Sundararajan V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual Saf Health Care 2010; 19: e51–e51. [DOI] [PubMed] [Google Scholar]
- 21.Organization WH. ICD-10: international statistical classification of diseases and related health problems, Geneva, Switzerland: World Health Organization, 2004. [Google Scholar]
- 22.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130–1139. [DOI] [PubMed] [Google Scholar]
- 23.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care 2003; 12: 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan TP. Statistical methods for quality improvement, 3 ed Hoboken, NJ: Wiley, 2011. [Google Scholar]
- 25.Recchia DR, Barbosa EP and de Jesus Goncalves E.Improved quality control charts. R package version 0.5, Vienna, Austria: IQCC, 2010.
- 26.R Developement Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2013, www.R-project.org, 2005 (accessed 21 December 2015).
- 27.Simon M, Griffiths P. Choose your tool wisely: U charts are more informative than run charts with or without tests of significance. A comment on Unbeck et al. (2014), Unbeck et al. (2013) and Kottner (2014). Int J Nurs Stud 2015; 52: 481–486. [DOI] [PubMed] [Google Scholar]