Abstract
Objectives
Our aim was to identify the factors influencing the selection of a model of acute stroke service centralization to create fewer high-volume specialist units in two metropolitan areas of England (London and Greater Manchester). It considers the reasons why services were more fully centralized in London than in Greater Manchester.
Methods
In both areas, we analysed 316 documents and conducted 45 interviews with people leading transformation, service user organizations, providers and commissioners. Inductive and deductive analyses were used to compare the processes underpinning change in each area, with reference to propositions for achieving major system change taken from a realist review of the existing literature (the Best framework), which we critique and develop further.
Results
In London, system leadership was used to overcome resistance to centralization and align stakeholders to implement a centralized service model. In Greater Manchester, programme leaders relied on achieving change by consensus and, lacking decision-making authority over providers, accommodated rather than challenged resistance by implementing a less radical transformation of services.
Conclusions
A combination of system (top-down) and distributed (bottom-up) leadership is important in enabling change. System leadership provides the political authority required to coordinate stakeholders and to capitalize on clinical leadership by aligning it with transformation goals. Policy makers should examine how the structures of system authority, with performance management and financial levers, can be employed to coordinate transformation by aligning the disparate interests of providers and commissioners.
Keywords: major system change, stroke care, centralization, service transformation
Introduction
Major system change in healthcare involves ‘interventions aimed at coordinated, system wide change affecting multiple organizations and care providers’.1 There is interest internationally in this approach for improving outcomes and reducing costs but limited evidence on achieving it.2 A realist review of the literature (the Best framework) identified five rules for enhancing implementation.1 These link success to social processes (collective actions of human actors) enabling multiple forms of leadership, learning from history, improvement through feedback, physician engagement and service user involvement. By applying the Best framework, we aimed to understand the processes of planning and implementing two cases of major system change and, in so doing, critique and develop the framework.
We draw on a mixed methods evaluation of the centralization of acute stroke services to create fewer high-volume specialist services in two English metropolitan areas,3 London (population 8.17 million) and Greater Manchester (hereafter referred to as Manchester) (population 2.68 million).4 To give an indication of the scale of the changes, within two years of their implementation, over 8000 stroke patients were admitted to acute services in Manchester and 15,000 in London.5 However, the outcomes of centralizing services differed. Difference-in-differences analysis showed that centralizing stroke services in London reduced mortality and length of stay, while in Manchester length of stay in hospital fell but there was no impact on mortality beyond that which occurred in the rest of England.5 Through qualitative analysis of stakeholder interviews and documentary evidence, our aim was to explain why different models were implemented in two areas and in doing so, enhance the Best framework for future use.
Major system change of stroke services
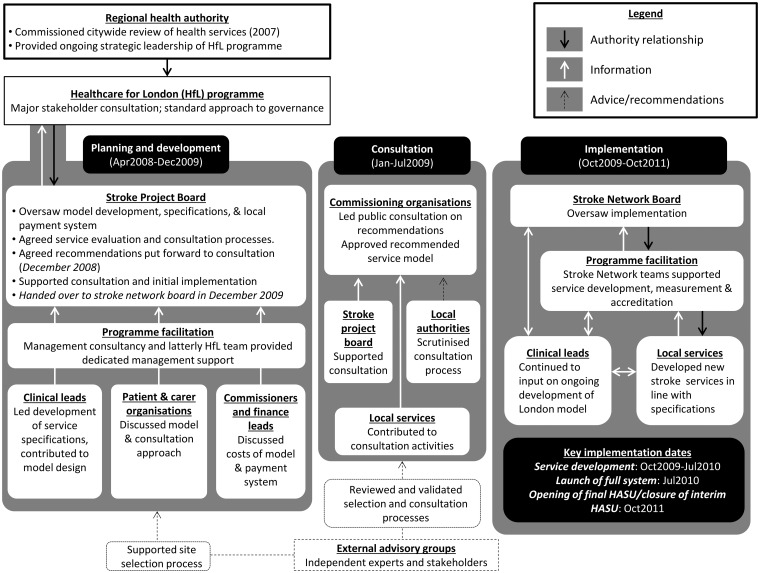
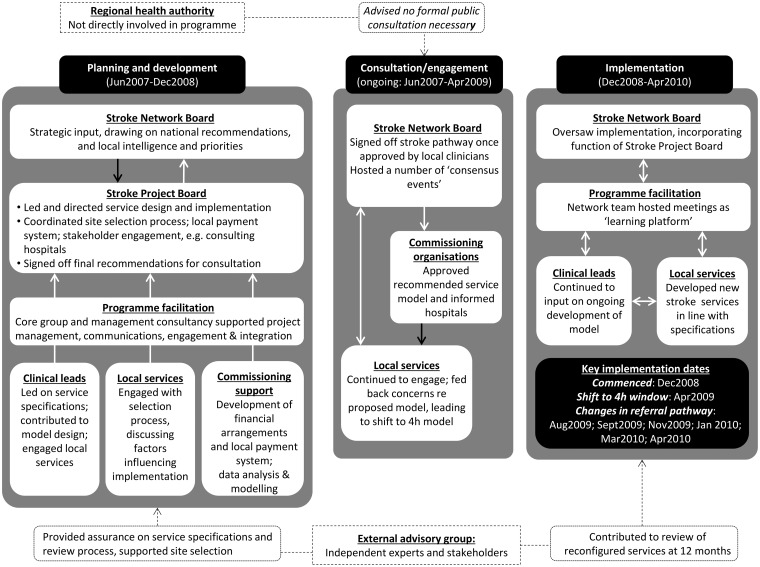
Proposals to transform acute stroke services in London and Manchester were based on evidence that people with suspected stroke should be admitted to a specialist acute stroke unit to get rapid access to brain imaging and anticoagulant drugs,6 and were informed by examples of specialist units in Australia7 and coordinated services in Canada.8 A national stroke strategy recommended ‘hub-and-spoke’ service models for large metropolitan areas, with specialist ‘hubs’ providing urgent care and ‘spoke’ units providing further care closer to patients’ homes.9 In Manchester, the case for centralizing services was made locally by health professionals to commissioning and provider leads. In London, centralizing acute stroke services was recommended as part of a review of services.10 In both areas, the process of centralization was characterized by overlapping phases of planning and development, consultation and implementation (Figures 1 and 2).
Figure 1.
Governance arrangements for centralizing acute stroke services in London.
Figure 2.
Governance arrangements for centralizing acute stroke services in Greater Manchester.
In London, the previous system for delivering acute stroke services involved 32 providers and the local ambulance service. In Manchester, nine providers and the ambulance service were involved. In both areas, a stroke project board (including providers, commissioners and patient representatives) was established to develop new service models and manage implementation. Change was governed using a ‘top-down’ approach in London, led by the pan-regional health authority (Figure 1), while a more ‘bottom-up’ network-based approach was used in Manchester, led by local providers and commissioners (Figure 2).
Informed by the external advisory group’s recommendations, commissioners in Manchester initially chose a service model in which all patients presenting at hospital within 24 h of onset of stroke symptoms would be treated in one of three Hyper Acute Stroke Units (HASUs); post hyper-acute care would be delivered by ten local Stroke Units (SUs). Shortly before implementation, some hospitals raised concerns about the impact of centralization on hospital resources and patient safety such as repatriation of frail and elderly patients. Consequently, the model was revised: only patients presenting at hospital within four hours of stroke symptoms appearing would be admitted to a HASU; all others would be taken as before to the nearest SU. Acute stroke services were not entirely withdrawn from any hospital. In London, the project board’s clinical subgroup recommended 10–12 HASUs but the project board proposed 8, reflecting the earlier review’s recommendations. Subsequently, 24 providers became SUs and stroke services were withdrawn from five hospitals.
Our aim in this paper is to determine why different models for centralizing services were chosen in London and Manchester and assess how the two different approaches contributed to different centralization models being implemented.
Methods
To analyse change in both areas, we conducted 45 semi-structured stakeholder interviews and analysed 316 documents. Using documentary evidence and snowball sampling, we identified stakeholders involved in governing the transformations (Table 1). The interviews lasted approximately 45 min and were audio-recorded. Interview topic guides covered governance approaches, proposal development, model agreement and implementation. Documentary evidence was used to develop narratives of the transformations, such as public consultation arrangements. The changes to services were implemented in 2010, and the interviews were conducted during 2012 and 2013. They represent a retrospective account when respondents were aware of how the services were performing. This use of different types of evidence,11 mitigated the risk of bias due to length of time since interviews.
Table 1.
Profile of interviewees in London and Manchester.
| Interviewees | London | Manchester | National | Total |
|---|---|---|---|---|
| Stroke network board | 5 | 6 | – | 11 |
| Pan-regional health authority | 7 | – | – | 7 |
| Service commissioners | 3 | 1 | – | 4 |
| Service users or representatives | 3 | 3 | – | 6 |
| Programme facilitation | 2 | 1 | – | 3 |
| Clinical leads | 2 | 1 | – | 3 |
| Provider organizations | 2 | 1 | – | 3 |
| Stroke services’ staff | – | 3 | – | 3 |
| Ambulance service | 1 | 1 | – | 2 |
| Politicians | 1 | – | 2 | 3 |
| Total | 26 | 17 | 2 | 45 |
Analysis of the interviews and documents was inductive and deductive,12 as coding was informed by themes emerging from the empirical data and a realist review of major system change literature.1 Data relating to London and Manchester were initially coded separately to produce narratives of transformation. Change across the two areas was compared using cross-cutting themes from the narratives, including receptivity to change, stakeholder involvement and experiences of service transformation. Finally, the coded data were analysed using Best’s five rules to compare mechanisms influencing major system change. The research team met regularly to discuss and agree interpretations of the data and identify questions for further exploration. To enhance validity, emerging findings were shared with relevant stakeholders from the two study areas, including professionals and service user representatives.
Results
The approaches to change are assessed by applying the five rules from the Best framework, including analysis of where the rules need to be adapted based on our findings (Table 2).
Table 2.
Summary analysis of Best et al.’s1 framework applied to major system change (MSC) of acute stroke services in London and Greater Manchester.
| London | Greater Manchester | Adapted rule | |
|---|---|---|---|
| Combine designated and distributed leadership | Centralizing services, and opportunity for investment, endorsed by clinical leaders, despite risk of losing services. Pan-regional authority oversaw change and helped to align stakeholders. | Impetus for centralizing services came from senior stroke physicians and public health staff; encouraged others to support change. Change led by local stroke network which did not have formal authority over providers. | Interplay between bottom-up and top-down leadership in achieving MSC; system-wide authority is needed to align multiple stakeholders over a large scale and encourage clinical commitment to system-wide improvement goals. |
| Feedback loops | Clinicians involved in developing quality standards for new services, as well as commissioners and providers’ finance teams. Providers received financial incentive for meeting standards. Stroke network advised providers on meeting standards. | Providers compensated for collecting and sharing national audit data, but no financial incentive for meeting clinical standards. Clinicians and managers from different providers along patient pathway met regularly to review performance. | Feedback may need to be combined with other tools to encourage behaviour change, e.g. financial incentives. |
| Attend to history | Awareness from previous attempts to transform services across London that implementing change is challenging. Legal firm consulted to avoid subsequent challenges. | Drew on experience from members of stroke network involved in an earlier reorganization of acute cardiac services. | Contextual factors can be a barrier to implementing lessons learned; political authority may be needed to challenge the existing context and enable more radical forms of transformation. |
| Engage physicians | Engaging variety of health professionals important in planning new services, especially ambulance service. Need to engage stakeholders outside health service; resistance from local politicians to closure of services. | Many stroke physicians supported change; some resistance from providers set to lose services. Need to engage other stakeholders, e.g. hospital managers as model had to be viable as ‘business proposal’. | Need to involve a range of stakeholders in planning MSC and have a system-wide governance structure to align their interests. |
| Involve patients and families | Proposal for centralizing stroke care put to public consultation. Quantified support for proposal used to legitimize centralization of services. | Perceived perspective of patients used to steer negotiations among providers and commissioners towards consensus. Some suggested that views of public and patients had limited influence on model of services. | Awareness that the drivers of MSC (e.g. clinical, political, social, financial) influence how different stakeholders’ views come to count during implementation; potential tension between patients’ and others’ perspectives. |
Rule 1: Combining designated and distributed leadership
This highlights the importance of combining designated leadership with distributed responsibility for improvement. In Manchester, the leadership of change was mainly distributed, while in London distributed and designated leadership were combined. This meant that when there was resistance to centralizing services from some stakeholders in both areas, there was a lack of system leadership in Manchester to challenge resistance and align stakeholders. As Figure 2 shows, the pan-regional health authority was not directly involved in the programme resulting in a less radical transformation of services in Manchester relative to London.
Distributed leadership
In both areas, reorganizing stroke services was supported by many clinicians because it was an opportunity for service investment and to gain further recognition as a profession distinct from geriatric medicine: ‘[clinicians] felt that stroke was a sort of a Cinderella service, that very little investment had been made in stroke. They saw that additional money was coming’ (Stroke network board member). Local clinical leaders’ endorsement of centralization generated wider support. In Manchester, change leaders used distributed leadership in relying on stroke physicians convincing others that centralization was necessary: ‘a lot of it was around peer support and, whether they liked it or not, those antagonists respected some of the lead stroke clinicians that were there around the table’ (Stroke network board member). While clinical leadership was visible in both areas, there were differences in designated leadership and how this was used to capitalize on distributed leadership.
Designated leadership
In London, designated leadership was easier to exercise than in Manchester because programme leaders possessed greater political authority to manage stakeholders’ resistance to change. Programme leaders were members of the pan-regional authority which oversaw changes to stroke services as part of a wider review of health services (Figure 1). This structure ensured that the model proposed by the project board for centralizing services was implemented: ‘you are the priesthood if you like of the model, so you keep the fidelity to the model that’s being described and only with your ‘say so’ can people deviate from it’ (pan-regional health authority member).
Planning was shaped by the pan-regional health authority because change was informed by a wider review10 of stroke and other services that had political influence because it was clinically led and demonstrated public support. Selection criteria for HASUs included strategic coherence13 with wider plans to develop major acute hospitals in London with other specialist services (major trauma care) and to ensure patients could reach a HASU by ambulance within 30 min. As clinical recommendations concerning designation were considered alongside hospitals’ fit with these broader criteria, some perceived that a ‘top-down’ approach to decision-making was taken: ‘giving them the model, saying this is what we want to do, and then there was a discussion about it, rather than it coming from the grass roots up’ (stroke network board member).
In Manchester, transformation was led by the stroke network board (Figure 2). As programme leaders lacked formal authority over providers and commissioners, changes were planned by consensus. As described earlier, a late challenge to the 24-h model came from some hospitals that were set to lose activity in the proposed changes to stroke services. In order to maintain unanimity, programme leaders implemented a 4-h model: ‘the minute it felt like unanimity was being compromised on that clinical discussion on the 24 versus the 4-hour pathway I think we were always going to be minded then to tilt towards holding unanimity’ (service commissioner).
Interplay between designated and distributed leadership
Designated leadership encouraged further distributed leadership of the changes proposed. In London, designated leadership was used to encourage stakeholders to associate with a wider geography of improvement:
My key mantra at the moment is to remind people constantly that this is the London model. So when an organisation says that they’d like to change something […] we say you can’t do that without it impacting on the whole of London (Stroke network member).
Further support for centralization was garnered through pan-London events during the public consultation, the second phase of the programme shown in Figure 1. Instead of a formal public consultation, Manchester held two consensus-building events involving providers, commissioners and the public where proposals for transformation were discussed (Figure 2).
Reflecting on the comparative difficulty of centralizing services in Manchester, one programme leader suggested that greater authority would have been useful in ensuring different stakeholders prioritized the wider metropolitan area’s interests: ‘one of the things that we would do now that we didn’t do then would be probably not proceed on the base of unanimity’ and instead ensure ‘people wear a kind of “Greater Manchester population” hat’ (service commissioner).
In London, while change was more ‘top-down’ than in Manchester, this approach encouraged distributed leadership by engendering recognition that meeting the centralization programme’s goals, and those of the stroke community, required a pan-London perspective. For instance, two clinical leaders in London performed a visible symbolic role in supporting the proposals, despite this meaning that their own services would not become HASUs. In Manchester, programme leaders’ weaker authority made encouraging distributed leadership more difficult, despite ‘support from the most senior and most respected clinicians’ (stroke network board member).
Rule 2: Establish feedback loops
This rule refers to the importance of measuring outcomes that are trusted by stakeholders and incentivizing improvement. Performance data were collected in both areas. In London, the designation process for hospitals was linked to achieving standards, such as minimum staff numbers, meaning that providers had to comply in order to be accredited. Providers also received a financial incentive for performing well, as performance data were monitored by the stroke networks, and payments were only made if quality standards were met. In Manchester, a local payment system was required to split the costs of providing services between HASUs and SUs, although payments were based on patients treated by each form of provider not by achieving standards. Thus, financial incentives were stronger in London than Manchester for improving clinical standards (in Manchester financial penalties were considered punitive by planners and not used).
Rule 3: Attend to history
The Best framework suggests the importance of learning from previous transformation attempts, including ‘failures’. In London, past failures to achieve major system change meant programme leaders focused on implementing ‘a small number of absolute priorities’. Change leaders were aware that dealing with stakeholders’ differences was critical during planning meetings: ‘not letting people go out the room if I thought actually they were disagreeing but they weren’t disagreeing in the room’ (service commissioner).
In Manchester, decision-making based on unanimity was preferred as historically collective decisions were made by consensus among commissioners and providers. One programme leader believed that the approach taken ‘introduced an awful lot of risk that we needn’t have played into it’ (service commissioner).
In both areas, stroke network members’ experiences of an earlier reorganization of acute cardiac services was utilized. This highlighted a need to encourage dialogue between the ambulance service and other stakeholders. In London, insistence by the ambulance service informed the decision to take a big bang approach to transformation whereby centralized services went live on a single date. Manchester’s ambulance service expressed a similar preference, but a decision was made to implement changes to services in stages instead. A barrier to addressing the ambulance service’s preference was the need to accommodate providers’ concerns about transferring patients in the new system: ‘The worry was that if you suddenly changed the system, the whole system, you could become completely overwhelmed’ (clinical lead).
Programme leaders attended to history by recognizing that the existing system was unlikely to be receptive to change. In Manchester, programme leaders attempted to overcome resistance by making decisions through consensus. This involved bowing to resistance from some providers and resulted in less radical transformation. Conversely, the political authority with which London’s programme leaders acted was critical in being able to challenge resistance.
Rule 4: Engage physicians
This rule highlights the need to engage physicians as they have historically had the power to influence major system change.14 However, in practice, the involvement of a wide range of stakeholders was required. Ambulance services who assessed and transported the majority of patients with suspected stroke, were critical: ‘it wouldn’t have happened if the ambulance service hadn’t been fully on board with it’ (stroke network board member).
Obtaining the agreement of hospitals’ senior management was necessary as changes to stroke provision would affect hospital income and other departments. In Manchester, one hospital did not bid to become a HASU, despite physician support, due to A&E pressure: ‘senior management had told [the consultant] not to, that the bid shouldn’t go in’ (clinical lead). The wider financial impact of full centralization was understood by programme leaders. To meet both physicians’ and hospital managers’ expectations, the model for centralizing services needed to achieve ‘clinical consensus’ and be a viable ‘business proposal’ (stroke network board member).
As well as affecting stakeholders within health services, change was affected by local politics. In London, the programme included establishing a committee of local politicians to scrutinize the proposal’s public interest. The implications of services being discontinued in some areas caused resistance from local government representatives: ‘issues which caused the most angst was the removal of facilities from a certain local authority area. Every elected councillor wants to protect their area’ (local politician).
While stroke physicians were a key stakeholder, the geographic scale and public interest in the changes proposed meant that other stakeholders, both within and outside the health service, needed to be engaged to avoid derailment of change. Champions included senior stroke physicians, who exerted social influence over other clinicians as the Best framework suggests. Rather than relying on physician engagement, success was enabled through dialogue between, and the alignment of, different stakeholders.
Rule 5: Involve patients and families
This rule suggests that change processes should include service users’ perspectives and priorities. Attempts were made to represent their views in both areas. For example, patient organizations sat on committees for governing changes. Patients’ perceived priorities informed other stakeholders’ decision-making. In London, the initial pan-London proposal to centralize stroke care underwent public consultation. As the majority of respondents (67% of 3464) agreed with introducing specialist centres,15 this was seen to justify implementing a centralized model: ‘Our mandate for doing what we were doing came from that public consultation in which “about seven” had been supported, and there were going to be about seven’ (pan-regional health authority member).
In Manchester, patients’ perceived needs were used to reach consensus during decision-making about centralizing services. However, some interviewees doubted whether service users’ views, while sought through consultation on proposed service models, influenced transformation: ‘I don’t think it really changed anything… but at least people felt that they had a voice’ (service user representative).
Patient and public views were used instrumentally by leaders to lend support to the implementation of well-defined models of care. In London, as public support for about seven specialist centres had been quantified, this aided agreement to implement more fully centralized services. Public involvement had a political dimension as engagement was structured by programme leaders’ framing the options for consultation and the choice of the outcomes to legitimize changes to services. In Manchester, there was no equivalent process to establish service users’ priorities.
Discussion
While services were more fully centralized in London, a less radical transformation of services took place in Manchester because programme leaders did not have the political authority to challenge resistance from some stakeholders. In Manchester, the original model in which patients would be eligible for HASU care within 24 h from onset of symptoms was revised so as to maintain consensus, such that only patients presenting within 4 h of developing symptoms were eligible for treatment in a HASU and no provider lost their stroke services. This contrasted with the model in London, in which all patients with suspected stroke were eligible for HASU treatment and stroke services were closed in five providers.
The Best framework was useful for identifying key processes in the transformation of stroke services, yet produced an incomplete account of change. A need exists for greater acknowledgement of: potential barriers to implementing each rule; potential conflict between rules in service planning; and, as others have shown,16,17 the importance of politics in decision-making concerning healthcare reorganization. Our suggested changes to the rules are summarized in Table 2.
Distributed leadership by stroke physicians and other stakeholders was apparent in both transformations, but system leadership was necessary to capitalize on distributed leadership by aligning it with transformation goals. This system designated leadership in London encouraged distributed leadership by aligning actors with a pan-London approach to improvement. This eschewed commitment to sustaining a given hospital’s acute stroke service, even those recognized as providing high-quality care at the time. Managing disparate stakeholder interests was easier in London than in Manchester because designated leaders exercised greater political authority through pan-regional bodies and committees. This suggests that system leadership with authority is necessary to align multiple organizations across a large scale. However, encouraging leadership throughout the system is equally important; evidence from Denmark has shown that implementing stroke service centralization ‘top-down’ restricted the involvement of front-line staff and undermined ownership.18
Differences in the use of feedback loops in London and Manchester highlight the importance of analysing the social and political context in which performance metrics are developed. Variation in responses to feedback can be explained partly by differences in how resources were used to support transformation (e.g. local quality standards were linked to financial incentives to a greater extent in London). As feedback loops include social and financial components, the expectations of policy makers relying on social influence alone to change behaviour may be blunted in some contexts (e.g. where resources are already strained and subject to competing demands).
In relation to attending to history, Best et al. showed the difficulties associated with implementing such lessons. Analysis of political factors in the current study shows that a potential barrier to applying lessons is the involvement of multiple stakeholder interests in change; accommodating these may thwart transformation. In Manchester, the ambulance service provided advice on the timing of implementation, but a barrier to executing their recommendations was the need to accommodate other stakeholders’ perspectives. Proceeding on the basis of consensus may lessen resistance to transformation but this approach produced less radical change. The rule of attending to history, which involves recognizing potential barriers to change, is insufficient for improving implementation. As demonstrated in London, system leadership combined with political authority that includes levers to finance and performance manage major system change is needed to challenge the existing context and enable transformation.
The importance of involving a range of stakeholders beyond physicians in major system change was illustrated. These changes necessitated engagement with a range of clinical and managerial groups as planning change involved clinical, financial, logistical and public interest considerations. In this case, privileging the interests of one stakeholder was inappropriate, as other groups could impede change, including ambulance services, hospital managers and local authorities.
Public and patient involvement was used instrumentally by programme leaders to demonstrate support for the proposals being developed rather than to fulfil the loftier aspiration of co-designed services, which is often absent from major system change.1 One reason for this is political; in both areas, a vision for transformed services was already well defined and programme leaders focused more on gaining public support for the service models stemming from this vision than on obtaining patients’ input into service design (such as identifying performance metrics from patients’ perspectives). This resonates with previous research showing that patient and public involvement is often guided by health professionals, especially where technical knowledge is deemed necessary to participate.19 Only considering involvement in relation to fulfilling a change programme’s needs neglects the reasons for, and impact of, involvement from the perspective of service users.20 Furthermore, rules may conflict with one another in this context. Engaging clinicians to pursue a clinical case for change may have implications for involving the public in service design, as their views may not coincide.
Analysis of politics and power explains how different forms of leadership are combined in major system change. In both areas, providers and commissioners were consulted extensively on the new model for stroke care proposed. In London, change leaders had the political authority to maintain their position in response to providers’ concerns. In Manchester, leaders had less political authority and focused on maintaining consensus among stakeholders but in so doing implemented a less radical transformation. The two models were later found to have significantly different impact on stroke mortality and the provision of evidence-based clinical interventions.5,21 The more radical transformation of services in London involved system authority structures (the pan-regional health authority) combined with senior clinical leadership who used persuasive arguments. Although change in Manchester also involved clinical leadership, weaker authority structures existed for aligning stakeholders.
Conclusion
The combination of bottom-up leadership and top-down coordination of major system change is vital in navigating the complex process of its implementation. Engaging local stakeholders in planning is important to ensure that change builds on their experiences, is relevant to their needs, and motivates staff.22 However, as multiple stakeholders are often involved, a coordinating body with political authority to bring together those different interests is needed. System leadership – underpinned with the political authority to align stakeholders – should assume a leading role in supporting innovation by coordinating change.
Since the transformations of stroke care were implemented, pan-regional health authorities have been abolished and many purchasing and performance management duties in England have been transferred to local commissioning consortia.23 Policy makers should reflect critically on the collective capacity these organizations, and the providers from which they purchase services, have to pursue major system change. More recently, proposals have been announced to devolve budgets and decision-making authority back up to regions, notably Manchester.24 In relation to these different approaches to decision-making, policy makers should consider how system structures can be used to enable the joint planning and implementation of major system change. Finally, against a background of austerity, where many health systems face financial pressure, some ‘rules’ may need to be prioritized over others. Formative research could explore the feasibility of using an explicit framework of rules to inform programme leaders’ decision-making about allocating resources to the activities signified by each ‘rule’ and highlight perceived barriers and enablers to their use in change.
Acknowledgements
The study was granted ethical approval by the London East NHS research ethics committee (Reference 11/LO/1396). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Declaration of conflicting interests
A.G. Rudd is National Clinical Director of Stroke, NHS England, and London Stroke Clinical Director. P.J. Tyrrell was Stroke Clinical Lead for Greater Manchester to 2013 and led the Greater Manchester stroke service centralization from 2007.
Funding
This paper presents independent research funded by the National Institute for Health Research Health Services and Delivery Research Programme (Study Reference 10/1009/09). ST, SM and NJF were supported by the NIHR Collaboration for Leadership in Applied Health Research and Care North Thames at Bart’s Health NHS Trust. CDAW was supported by the NIHR Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London and also by the NIHR Collaboration for Leadership in Applied Health Research and Care South London.
References
- 1.Best A, Greenhalgh, Lewis S, et al. Large-system transformation in health care: a realist review. Milbank Q 2012; 90: 421–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenhalgh T, Humphrey C, Hughes J, et al. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009; 87: 391–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fulop N, Boaden R, Hunter R, et al. Innovations in major system reconfiguration in England: a study of the effectiveness, acceptability and processes of implementation of two models of stroke care. Implement Sci 2013; 8: 5–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of National Statistics. 2011 Census: usual resident population, local authorities in England and Wales. ONS: 2012.
- 5.Morris S, Hunter RM, Ramsay AI, et al. Impact of centralizing acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014; 349: g4757. [DOI] [PMC free article] [PubMed]
- 6.National Institute for Health and Clinical Excellence. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA)(NICE Clinical Guidelines, no 68). London: Royal College of Physicians, 2008. [PubMed]
- 7.NAO. Reducing brain damage: faster access to stroke care, London: The Stationery Office, 2005. [Google Scholar]
- 8.Buchan A. Best practice in Stroke Care 2007. In:Healthcare for London conference, London, UK, 19 February 2007.
- 9.DH. National stroke strategy. London: Crown, 2007.
- 10.Healthcare for London. A framework for action, London: NHS London, 2007. [Google Scholar]
- 11.Eisenhardt KM, Graebner ME. Theory building from cases: opportunities and challenges. Acad Manage J 2007; 50: 25–32. [Google Scholar]
- 12.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007; 42: 1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Healthcare for London. The shape of things to come, London: NHS London, 2009. [Google Scholar]
- 14.Timmermans S, Oh H. The continued social transformation of the medical profession. J Health Soc Behav 2010; 51(Suppl 1): S94–S106. [DOI] [PubMed] [Google Scholar]
- 15.Healthcare for London. Consulting the capital, London: NHS London, 2008. [Google Scholar]
- 16.Barratt H, Raine R. Hospital service reconfiguration: the battle for hearts and minds. BMJ 2012; 344: e953–e953. [DOI] [PubMed] [Google Scholar]
- 17.Tuohy CJ. Accidental logics: the dynamics of change in the health care arena in the United States, Britain, and Canada, New York, NY: Oxford University Press, 1999. [Google Scholar]
- 18.Douw K, Nielsen CP, Pedersen CR. Centralizing acute stroke care and moving care to the community in a Danish health region: challenges in implementing a stroke care reform. Health Policy 2015; 119: 1005–1010. [DOI] [PubMed] [Google Scholar]
- 19.Fudge N, Wolfe CD, McKevitt C. Assessing the promise of user involvement in health service development: ethnographic study. BMJ 2008; 336: 313–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson JP, Bissell CL, Cooper CJ, et al. Exploring the impact of patient and public involvement in a cancer research setting. Qual Health Res 2014; 24: 46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramsay AI, Morris S, Hoffman A, et al. Effects of centralizing acute stroke services on stroke care provision in two large metropolitan areas in England. Stroke 2015; 46: 2244–2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sørensen T, Dyb K, Rygh E, et al. A qualitative description of telemedicine for acute stroke care in Norway: technology is not the issue. BMC Health Serv Res 2014; 14: 643–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DH. The functions of GP commissioning consortia: a working document, London, UK: Department of Health, 2011. [Google Scholar]
- 24.HM Treasury/greater Manchester Combined Authority. Greater Manchester agreement: devolution to the GMCA & transition to a directly elected mayor,www.gov.uk/government/uploads/system/uploads/attachment_data/file/369858/Greater_Manchester_Agreement_i.pdf (accessed 27 October 2015).