Summary
Cogan syndrome is a rare disease characterized by coexisting audiovestibular and ocular symptoms. Almost half of patients develop systemic manifestations. We report the case of a 38-year-old woman who presented with severe medium and large vessel vasculitis as a systemic manifestation of Cogan syndrome.
Introduction
Cogan syndrome was first defined as nonsyphilitic keratitis, coexisting with Meniere-like vestibuloauditory symptoms in 1945.1 In 1980 the definition was expanded to include attacks of vertigo, tinnitus, hearing loss, and ocular symptoms other than interstitial keratitis.2 Because the symptoms of Cogan syndrome are alleviated by corticosteroid treatment, many consider Cogan syndrome an immune-mediated disease. Interstitial keratitis is observed in 80% of the patients and is usually bilateral. Half of the patients experience sudden, fluctuating and progressive hearing loss, which is mostly bilateral. Hearing loss becomes permanent in 20% of patients.3 Cogan syndrome has a mortality rate of approximately 10%. Causes of death include systemic vasculitis, cardiac complications (ruptured aortic aneurysms, myocardial infarction, congestive cardiac failure), gastrointestinal bleeding, cerebrovascular accident, subarachnoid hemorrhage, and renal complications.4,5
There are two variants of Cogan syndrome: typical and atypical.2 Atypical Cogan syndrome manifests with eye involvement other than interstitial keratitits, including acute angle-closure glaucoma, retinal vasculitis, papillitis, central retinal vein occlusion, and vasculitic optic neuropathy. Audiovestibular symptoms of atypical Cogan syndrome also differ from the Meniere-like symptoms observed in typical Cogan syndrome. In typical Cogan syndrome, the interval between the onset of ocular and audiovestibular manifestations is <2 years. In atypical Cogan syndrome this interval widens. Systemic manifestations are more common with atypical Cogan syndrome. The most common systemic manifestations are headache, arthralgia, fever, arthritis, and myalgia. Some forms of vasculitis are observed in approximately 10% to 13 % of patients.2,3,6 The common vasculitis manifestations are recurrent upper extremity phlebitis and vasculitis, polyarteritis nodosa, diffuse vasculitis, and testicular artery and external iliac artery vasculitis, all of which are inflammation of medium-sized vessels.3 Aortitis has also been reported, but information regarding the potential severity of aortic involvement is lacking. We report a patient with Cogan syndrome who developed severe aortitis that required surgery.
Case Report
A 26-year-old woman with an unremarkable family history other than a father with coronary artery disease presented to her local otolaryngologist with sudden-onset vertigo and hearing loss eventually requiring cochlear implants in both ears. Within a year, she was diagnosed with Cogan syndrome after she developed interstitial keratitis. Her eye disease was controlled with a combination of prednisone and mycophenolate mofetil and was subsequently quiescent off all medications for 6 years.
Ten years after her initial Cogan syndrome diagnosis, she presented with lower extremity pain and claudication. Laboratory work-up to investigate other autoimmune diseases showed an elevated erythrocyte sedimentation rate but was otherwise unrevealing; results for rheumatoid factor and antinuclear antibodies were negative. Computerized tomography angiogram revealed a 5.6 cm (normal value, <2.6 cm) grade 4 thoracoabdominal aortic aneurysm with infrarenal aortic and total iliac system occlusion, and high-grade stenosis of the bilateral renal, celiac and superior mesenteric arteries (Figure 1). An echocardiogram showed an extensive mural thrombus of the abdominal aorta.
Figure 1.
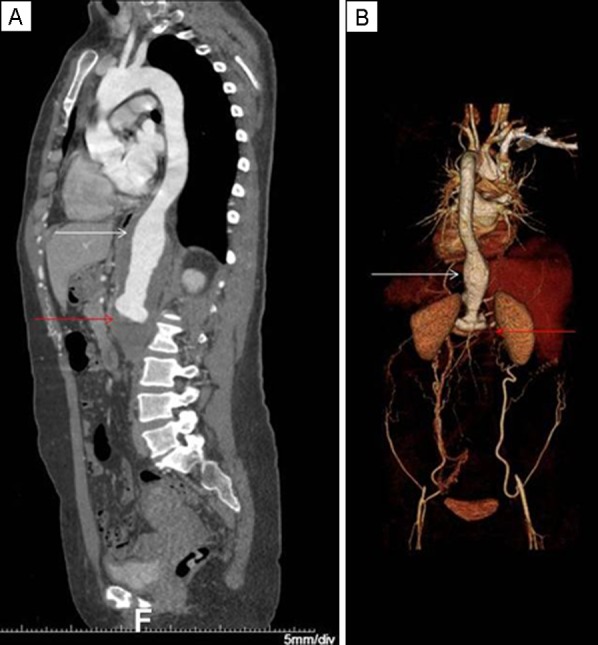
Computed tomography of the full aorta (A) and its 3D reconstruction (B) show a grade IV thoracoabdominal aortic aneurysm (white arrows) with infrarenal aortic and total iliac system occlusion (red arrows).
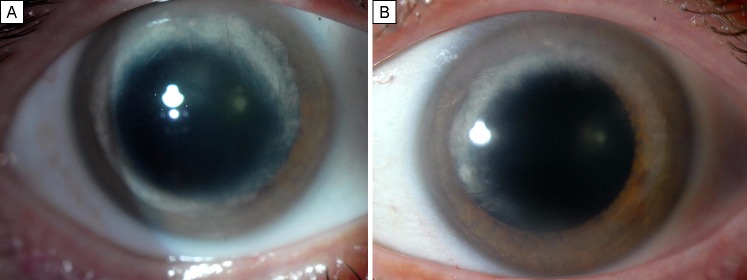
She underwent resection and grafting of the thoracoabdominal aortic aneurysm and bypass grafts were placed between the aorta and celiac, superior mesenteric, right and left renal, and bifemoral arteries. Following surgery, the patient was started on systemic prednisone and methotrexate, and systemic corticosteroid was tapered-off within 3 months. She had no active ocular inflammation at presentation and over the course of follow-up. On examination, she had old ghost vessels and posterior stromal opacification in a ring-like configuration in the paracentral cornea in both eyes consistent with her history of interstitial keratitis (Figure 2).
Figure 2.
Slit-lamp photographs showing corneal scarring secondary to interstitial keratitis in the patient’s right (A) and left (B) eyes.
Discussion
Cardiovascular manifestations are more commonly seen in patients with atypical Cogan syndrome and include aortitis with aortic insufficiency, Takayasu-like stenotic vascular lesions, and coronary artery involvement.2 It has been documented that aortitis, with an estimated prevalence of 10%, can occur from 2 weeks to 12 years after the initial diagnosis of Cogan syndrome.6,7 There are several reports of Cogan syndrome patients that have required vascular surgery.8–10 In these cases, the indications for surgery were problems in the ascending aorta, aortic root, mitral valve, and coronary arteries. There has only been one report of a thoracic aortic aneurysm with rapidly progressive aortic regurgitation and thrombosis of the common iliac artery in a Cogan syndrome patient with coronary involvement.11
The present case is unique because of the severity and involved areas of the vasculitis. The patient’s vascular manifestations included a thoracoabdominal aortic aneurysm with infrarenal aortic and total iliac system occlusion, and high-grade stenosis to bilateral renal, celiac and superior mesenteric arteries. Despite the severity of these manifestations, the root of aorta, which is one of the most frequently involved areas in Cogan syndrome, was spared. The cardiovascular manifestations of Cogan syndrome can often be treated with corticosteroids. In the present case, the patient required extensive surgery because of the consequences of severe vasulitis, demonstrating that cardiovascular manifestations of Cogan syndrome can be life-threatening in rare cases. Because this type of severe involvement is unusual, Cogan syndrome patients are not routinely referred for cardiovascular imaging. However, patients should be educated about the warning symptoms of such involvement.
In our case, the patient had severe cardiovascular involvement in the absence of any active ocular inflammation. She had been free of any ocular and audiovestibular symptoms for over 5 years off of immunosuppressive medication. Development of severe systemic vasculitis despite quiescence of the primary sites of inflammation in Cogan syndrome emphasizes the need for continued monitoring of all potential Cogan syndrome manifestations even after the ocular and audiovestibular symptoms subside.
The manifestations in this case, especially severe interstitial keratitis, sudden hearing loss, and an interval of a year between onset of these symptoms are more consistent with typical Cogan syndrome. Haynes et al reported that life-threatening aortic insufficiency develops only in 10% of typical Cogan syndrome patients and serious systemic necrotizing vasculitis is rarely observed in typical Cogan syndrome, whereas 21% of atypical Cogan syndrome is associated with vasculitis.2 In contrast, a study of 32 patients reported by Grasland et al showed no significant difference in frequency of aortitis manifestations between typical and atypical Cogan syndrome patients.12 Thus, significant cardiovascular disease can occur regardless of the ocular and audiovestibular manifestations. An ophthalmologist diagnosing a patient with Cogan syndrome should perform a focused review of systems and refer the patient to both an otolaryngologist and internist. The patient should be questioned for any hematuria, decrease in urine output, hemoptysis, breathlessness, chest pain, abdominal pain, gastrointestinal bleeding, myalgia, arthralgia, headache, visual changes, limb claudication, necrotic lesions, pain or coldness in extremities, and loss of pulse to identify any symptoms of systemic vasculitis and aortitis. Blood pressures should be obtained and pulses should be felt from all extremities. Any blood pressure difference, absence of pulse, arterial bruit, and abnormal heart sounds should alarm the physician. The ophthalmologist, internist, and patient should be aware of the potential systemic symptoms to monitor for them so as to promptly diagnose and treat potentially life-threatening cardiovascular disease related to Cogan syndrome.
Literature Search
PubMed was most recently searched on July 23, 2014, for reports in English, without date restriction, using the following terms: Cogan syndrome; Cogan syndrome AND cardiovascular manifestations; Cogan syndrome AND systemic manifestations.
References
- 1.Cogan DG. Syndrome of nonsyphilitic interstitial keratitis and vestibuloauditory symptoms. Arch Opthamol. 1945;33:144–9. doi: 10.1001/archopht.1959.00940090697004. [DOI] [PubMed] [Google Scholar]
- 2.Haynes BF, Kaiser-Kupfer MI, Mason P, Fausi AS. Cogan syndrome: studies in thirteen patients, long term follow-up, and a review of the literature. Medicine. 1980;59:426–41. [PubMed] [Google Scholar]
- 3.Gluth MB, Baratz KH, Matteson EL, Driscoll CLW. Cogan syndrome: a retrospective review of 60 patients throughout a half century. Mayo Clin Proc. 2006;81:483–8. doi: 10.4065/81.4.483. [DOI] [PubMed] [Google Scholar]
- 4.Cundiff J, Kansal S, Kumar A, Goldstein DA, Tessler HH. Cogan’s syndrome: a cause of progressive hearing deafness. American Journal of Otolaryngology. 2006;27:68–70. doi: 10.1016/j.amjoto.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Baumann A, Helbling A, Oertle S, Häusler R, Vibert D. Cogans syndrome: clinical evolution of deafness and vertigo in three patients. Eur Arch Otorhinolaryngol. 2004;262:45–9. doi: 10.1007/s00405-004-0738-8. [DOI] [PubMed] [Google Scholar]
- 6.Vollertsen RS, McDonald TJ, Younge BR, Banks PM, Stanson AW, Ilstrup DM. Cogan’s syndrome: 18 cases and a review of the literature. Mayo Clin Proc. 1986;61:344–617. doi: 10.1016/s0025-6196(12)61951-x. [DOI] [PubMed] [Google Scholar]
- 7.Slobodin G, Naschitz JE, Zuckerman E, et al. Aortic involvement in rheumatic diseases. Clin Exp Rheumatol. 2006;24(2 Suppl 41):S41–7. (2006). [PubMed] [Google Scholar]
- 8.Jansen M, Saleh S, Bolster M, et al. Thoracic vasculitis presenting as surgical problems. Virchows Arch. 2010;456:91–6. doi: 10.1007/s00428-009-0865-0. [DOI] [PubMed] [Google Scholar]
- 9.Weissen-Plenz Sezer O, Vahlhaus C, et al. Aortic dissection associated with Cogans’s syndrome:deleterious loss of vascular structural integrity is associated with GM-CSF overstimulation in macrophages and smooth muscle cells. J Cardiothorac Surg. 2010;5:66. doi: 10.1186/1749-8090-5-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cochrane AD, Tatoulis J. Cogan’s syndrome with aortitis, aortic regurgitation, and aortic arch vessel stenoses. Ann Thorac Surg. 1991;52:1166–7. doi: 10.1016/0003-4975(91)91304-e. [DOI] [PubMed] [Google Scholar]
- 11.Tseng JF, Cambria RP, Aretz HT, Brewster DC. Thoracoabdominal aortic aneurysm in Cogan’s syndrome. J Vasc Surg. 1999;30:565–8. doi: 10.1016/s0741-5214(99)70086-8. [DOI] [PubMed] [Google Scholar]
- 12.Grasland A, Pouchot J, Hachulla E, et al. Typical and atypical Cogan’s syndrome: 32 cases and review of the literature. Rheumatology. 2004;43:1007–15. doi: 10.1093/rheumatology/keh228. [DOI] [PubMed] [Google Scholar]