Summary
A 49-year-old diabetic man presented with a 2-day history of a painful right eye associated with a purulent discharge. Prior to becoming symptomatic, he reported that someone spat at him, resulting in direct contact between the saliva and his affected eye. Gram stain revealed numerous leucocytes with Gram-negative diplococci, and culture yielded Neisseria meningitidis (serogroup C). There was no evidence of any systemic infection, and blood cultures were negative for any growth. He was treated for primary meningococcal conjunctivitis (PMC) with intensive topical antibiotic eyedrops as well as systemic antibiotics. One week after commencing treatment he remained systemically well and his symptoms had fully resolved.
Introduction
Neisseria meningitidis is a rare cause of bacterial conjunctivitis. Previously reported cases of primary meningococcal conjunctivitis (PMC) suggest that children are more frequently affected than adults, with 95% of cases occurring in patients <25 years of age.1,2 Although PMC is a rare cause of bacterial conjunctivitis, it has the potential to develop into systemic and potentially life-threatening meningococcal infection in about 17.8% of patients.2 The current literature focuses on the importance of administering both topical and systemic treatment to prevent PMC developing into systemic meningococcal infection. We report an unusual case of unilateral PMC, in which saliva may represent direct mode of transmission for ocular infection.
Case Report
A 49-year-old man presented at Birmingham and Midland Eye Centre, United Kingdom, with a 2-day history of a painful right eye associated with copious purulent discharge. By the time he presented, he had difficulty opening his right eye because of swelling. He reported that approximately 10 days prior to the onset of symptoms someone had spat directly into his right eye while trying to separate a fight. His past medical history included hypercholesterolemia, vitamin B12 and D deficiency, and type 2 diabetes mellitus that was well controlled on gliclazide and metformin. He had no history of previous ocular problems and was not a contact lens wearer. Apart from the right eye conjunctivitis, his general health was good, with no history of fevers, photophobia, neck stiffness, or rash.
On examination, unaided Snellen visual acuity was 6/18 in the right eye and 6/5 in the left eye. The left eye appeared normal. Examination of the right eye revealed a closed eye, with purulent discharge, widespread chemosis, subconjunctival hemorrhage, and hyperemia. The right cornea had areas of subepithelial infiltration, stromal edema, and punctate epithelial erosions (Figure 1). Examination of the anterior chamber and posterior segment was unremarkable. There was no evidence of systemic infection. A right conjunctival swab was sent for Gram stain and culture before initial treatment was started with topical chloramphenicol 0.5%. The Gram stain revealed numerous leucocytes, with Gram-negative diplococci (Figure 2), and culture yielded Neisseria meningitidis (serogroup C). Peripheral blood cultures were negative for growth. Following sensitivity results the patient was admitted and treated with intensive topical chloramphenicol 0.5% and ofloxacin 0.3% eye drops. He was also administered 3 doses of intravenous ceftriaxone.
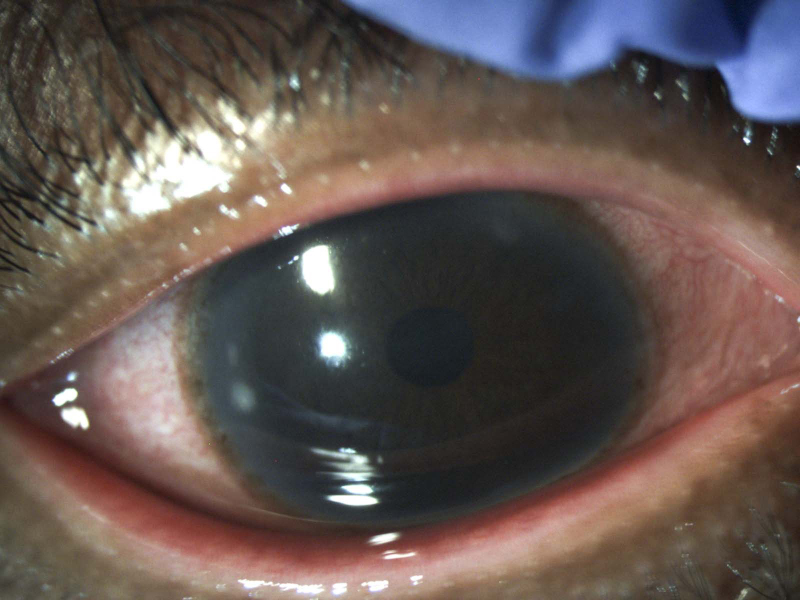
Figure 1.
Right eye showing conjunctival injection with subepithelial corneal infiltrates and stromal haze. Image taken after 72 hours of topical treatment.
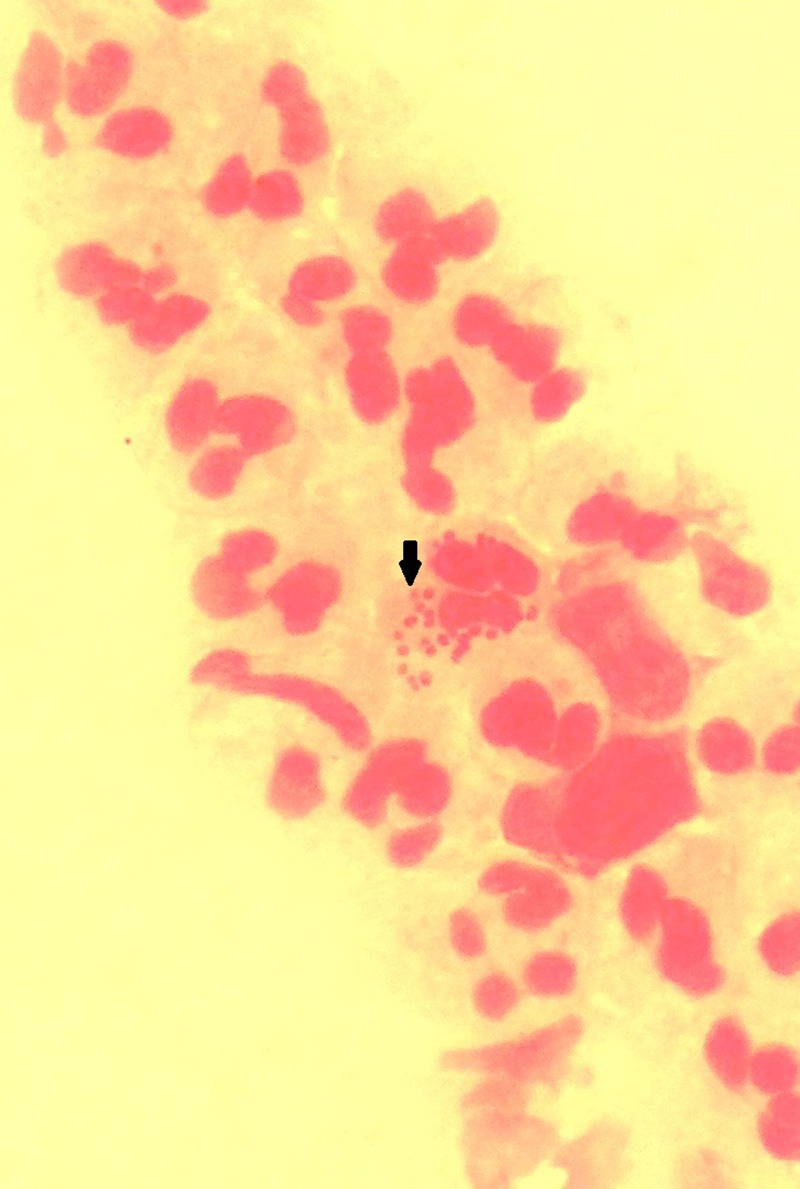
Figure 2.
Gram stain of conjunctival swab showing characteristic Gram negative diplococci and polymorphs.
By the third day of treatment, his symptoms had significantly improved, and he was discharged with topical chloramphenicol 0.5% and a course of oral ciprofloxacin. One week later, the hyperemia, chemosis, and purulent discharge had fully resolved (Figure 3). There was evidence of peripheral stromal scarring but no active infiltrates. Visual acuity in the right eye had improved to 20/16.7, and the patient remained well, with no evidence of secondary infection.
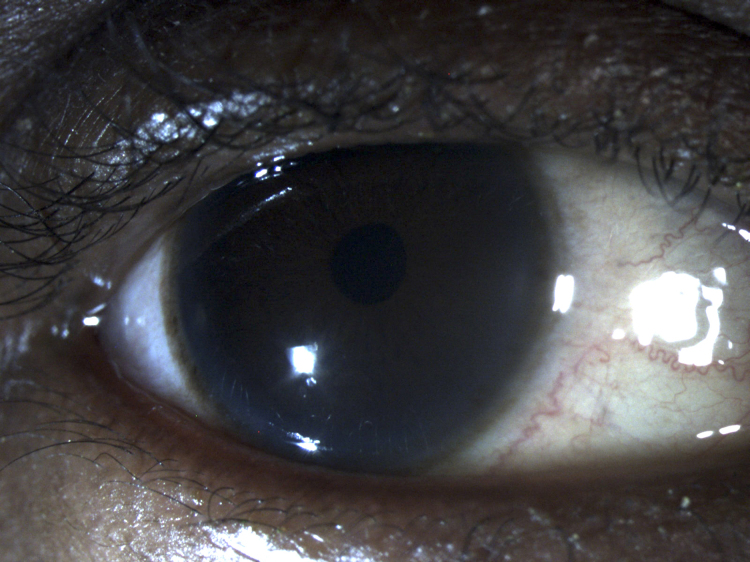
Figure 3.
Completely resolved infection with no signs of conjunctival congestion or corneal infiltrates.
Discussion
Previous reports have demonstrated the importance of treating PMC with both topical and systemic antibiotic treatment to prevent systemic meningococcal disease.2–4 Topical therapy alone is not sufficient to treat potential nasopharyngeal carriage, and the risk of developing invasive meningococcal disease is approximately 19 times greater for those receiving topical treatment alone compared to those also receiving systemic antibiotic treatment.2
However, there is little published literature reporting on potential sources of PMC infection. Meningococcal conjunctivitis is a rare cause of conjunctivitis that is most commonly associated with invasive meningococcal disease and rarely occurs in isolation. The present case is unusual because there is a very strong history to suggest that the mode of transmission in this case was from direct ocular contact with saliva. To our knowledge, PMC infection through direct contact with saliva has been reported only once before, in a nondiabetic individual.5 The human pharyngeal mucosa is commonly colonized with Neisseria meningitidis, and asymptomatic carriage is common, with a carriage prevalence of up to 35% in some populations.6–8 The pathogenesis of meningococcal disease is not fully understood; it remains unclear as to why this commensal bacterium can colonize the nasopharynx of a large proportion of the population without any ill effects but cause potentially life-threatening invasive disease in a very small minority. While the exact incidence of PMC is not known, it is thought to be <2% of all cases of conjunctivitis, despite the high prevalence of meningococcal carriage.9
Patients with diabetes are at increased risk of common infections.10 Further studies must be conducted to investigate this subject, but it could be that our patient was more susceptible to developing PMC because he was diabetic. We cannot know for certain whether our patient was colonized with Neisseria meningitidis prior to his PMC infection or whether the meningococcal infection was transmitted by direct contact with saliva. Unfortunately, a throat culture from the individual who spat in the patient’s eye could not be performed because his identity was unknown. This would have been helpful in confirming the mode of transmission by establishing whether the serogroup of Neisseria meningitidis was the same as that cultured from the affected eye. A study conducted by Orr et al8 found the prevalence of meningococcal carriage in saliva to be extremely low (0.4%) compared to carriage prevalence in the nasopharynx (32%) or tonsils (19%). They suggested that that low levels of salivary contact are unlikely to transmit meningococci. It is noteworthy that saliva from spitting is likely to contain not only saliva but also nasopharyngeal secretions, which Orr et al8 have shown to have a much higher prevalence of meningococcal carriage than pure saliva. While it is possible that our patient may have already been an asymptomatic carrier of Neisseria meningitidis and developed a spontaneous PMC, the history in this case suggests that the mode of transmission was from direct ocular contact with saliva.
To our knowledge, there is only one previously reported case in the literature of PMC transmitted by saliva, with this case being the first reported in a diabetic patient. It may be that individuals with diabetes have a relatively higher chance of developing PMC infections.
PMC can be difficult for clinicians to distinguish from other forms of conjunctivitis because the clinical picture can be very similar to more common conjunctival infections.11 Early diagnosis of PMC and timely treatment is essential to reduce ocular complications and minimize the risk of invasive systemic meningococcal disease. Once confirmed by Gram stain and culture, it is important that treatment includes both focused topical and systemic antibiotics in order to treat nasopharyngeal colonization as well as ocular disease.
Literature Search
The authors searched the PubMed database in January 2015, without language restriction, using the following search terms: meningococcal conjunctivitis, Neisseria meningitidis, saliva AND transmission, bacterial conjunctivitis.
Acknowledgments
The authors thank the Medical Illustration Department at Sandwell & West Birmingham Hospitals NHS Trust for Figures 2 and 3.
References
- 1.Anderson J, Lind I. Characterization of Neisseria meningitidis isolates and clinical features of meningococcal conjunctivitis in ten patients. Eur J clinical Microbiol Infect Dis. 1994 May;13:388–93. doi: 10.1007/BF01971995. [DOI] [PubMed] [Google Scholar]
- 2.Barquet N, Gasser I, Domingo P, Moraga FA, Macaya A, Elcuaz R. Primary meningococcal conjunctivitis: report of 21 patients and review. Rev Infect Dis. 1990;12:838–47. doi: 10.1093/clinids/12.5.838. [DOI] [PubMed] [Google Scholar]
- 3.Stansfield RE, Masterton RG, Dale BAS, Fallon RJ. Primary meningococcal conjunctivitis and the need for prophylaxis in close contacts. J Infect. 1994;29:211–4. doi: 10.1016/s0163-4453(94)90842-7. [DOI] [PubMed] [Google Scholar]
- 4.Hagelskjaer LH, Schonheyder HC, Blichfeld LP. Primary meningococcal conjunctivitis—more than meets the eye! Acta Paediatr. 1993;82:979–80. doi: 10.1111/j.1651-2227.1993.tb12614.x. [DOI] [PubMed] [Google Scholar]
- 5.Holdsworth, Jackson H, Kaczmarski E. Meningococcal infection from saliva. Lancet. 1996;348:1443. doi: 10.1016/S0140-6736(96)24047-4. [DOI] [PubMed] [Google Scholar]
- 6.European Centre for Disease Prevention and Control . Public health management of sporadic cases of invasive meningococcal disease and their contacts. Stockholm: ECDC; 2010. http://www.ecdc.europa.eu/en/publications/Publications/1010_GUI_Meningococcal_guidance.pdf. Accessed October 29, 2014. [Google Scholar]
- 7.Cartwright KAV, Stuart JM, Jones DM, Noah ND. The Stonehouse survey: nasopharyngeal carriage of meningococci and Neisseria lactamica. Epidemiol Infect. 1987;99:591–601. doi: 10.1017/s0950268800066449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orr HJ, Gray SJ, Macdonald M, Stuart JM. Saliva and meningococcal transmission. Emerg Infect Dis. 2003 Oct;9:1314–5. doi: 10.3201/eid0910.030444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neoh C, Agious-Fernandez A, Kaye SB, Molyneux EM, Hart CA. Primary meningococcal conjunctivitis in children. Br J Clin Pract. 1994;48:27–8. [PubMed] [Google Scholar]
- 10.Muller LM, Gorter KJ, Hak E, et al. Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis. 2005;41:281–8. doi: 10.1086/431587. [DOI] [PubMed] [Google Scholar]
- 11.Andreoli CM, Wiley HE, Durand ML, Watkins LM. Primary meningococcal conjunctivitis in an adult. Cornea. 2004;23:738–9. doi: 10.1097/01.ico.0000126316.82648.56. [DOI] [PubMed] [Google Scholar]