Abstract
Hypopituitarism can present with psychiatric symptoms. We report a unique case of psychosis in clear consciousness in a case of hypopituitarism due to the secondary empty sella syndrome following a Russell's viper bite which was untreated and presented with psychotic symptoms for past 13 years following the snake bite. After the diagnosis of psychosis due to hypopituitarism was made, the patient was treated with levothyroxine and prednisolone supplements and his psychotic symptoms subsided without any psychotropic drugs. Vasculotoxic snake bites can cause hypopituitarism and can present with psychosis. Further research will be needed into the prevalence of this phenomenon.
Keywords: Empty sella syndrome, hypopituitarism, psychosis, Russell's viper
INTRODUCTION
India is a country, considered to have one of the highest numbers of snake bites and fatalities related to it.[1] The Russell's viper (Daboia russelii) is a known culprit and has been known to cause acute and chronic hypopituitarism.[2] Literature of psychosis in hypopituitarism has been limited to case reports and has been described in clear consciousness and vice versa.[3] In this context, we present a unique case encountered by us as follows.
CASE REPORT
Our patient, a 42-year-old married, premorbidly well-functioning male with no family history of mental illness being reported, recently visited the dermatology outpatient department along with his wife, for complaints of generalized hypopigmentation of the skin and truncal hair loss, which was gradual in onset of more than 12 years duration. During the examination, he was found to be gesturing and muttering, as if he was in conversation with an imaginary person. He was referred immediately to the psychiatry department where he was admitted for further evaluation.
His history revealed that he was apparently normal until 13 years back whereupon he had been admitted to the critical care unit for symptoms of sudden onset weakness, vomiting, dehydration, and melena following a Russell's viper snake bite. He was treated with supportive management. On discharge, our patient was diagnosed to have hypoadrenalism and was managed with oral prednisolone 2.5 mg twice in a day. Two months later, he was admitted again for hypoglycemic shock after complaining of the generalized weakness of the body. He was also diagnosed to have hypothyroidism during this time and was started on oral levothyroxine 50 mcg once in a day. Unfortunately, since the patient belonged to the low socioeconomic status, he dropped from further hormonal supplementation and follow-up after a month. Later over the years, his family gradually noticed personality changes in him. He would have low mood, anhedonia, increased religiosity, poor short-term memory, decreased social interaction, sleep, libido, and appetite. He would stop going for work citing he was being persecuted by the police and for the past 4 years he would be found muttering to himself and gesturing, as if he was in conversation with an invisible person. There was history suggestive of type 2 diabetes mellitus and hypertension in first and second degree relative but no history of other endocrine disorders in the family.
On mental status examination, he was conscious and oriented with poor eye contact, decreased psychomotor activity and talk, guarded about revealing the details of his persecutory ideas and described visual hallucinations of seeing ghosts to which he would converse, impaired attention, concentration, and immediate memory with Grade 3 insight. System examination showed generalized hypopigmentation, decreased body hair, 0 and bilateral pitting edema. The blood pressure was 110/80 mm of Hg with no postural hypotension. There were no neurological deficits on examination. His investigations revealed the thyroid stimulating hormone (TSH) levels of 3.73 mIU/L, T4 levels as 0.05 mcg/dl, T3 levels of 31 ng/dl, morning serum cortisol levels of 0.09 mcg/dl, and serum testosterone levels of 1.83 nmol/L. His routine blood examination, routine urine examination, routine blood sugar, serum sodium, calcium, bicarbonate and potassium, renal and liver function test, blood pH, and lipid profile were normal. Cosyntropin stimulation test, assays for growth hormone, follicular stimulating hormone, and luteinizing hormone were not available in our institution. Magnetic resonance imaging scan revealed an empty sella [Figure 1]. The diagnosis of organic delusional (schizophrenia-like) disorder was made as per 10th revision of International Statistical Classification of Diseases and health related problems.
Figure 1.
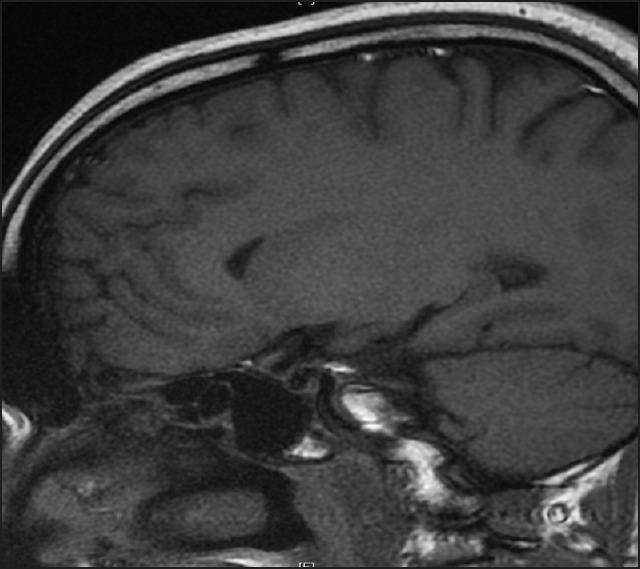
Saggital T1-weighted magnetic resonance imaging head showing an empty sella turcica
After the consultation with Department of General Medicine, the patient on the day 2 of admission, was started on oral levothyroxine 50 mcg/day and on day 5, after all investigation results had become available, oral prednisolone 5 mg in the morning and 2.5 mg in the evening was initiated. Patient's general condition improved subsequently, and his hallucinations and delusions subsided by day the 10 and discharged on the day 14 with the same medications along with vitamin supplements. He is on follow-up for the past one year, and the patient is maintaining the thyroid hormones and morning serum cortisol levels in the normal limits with the formerly mentioned medications.
DISCUSSION
Our case might be the first reported case of psychosis in clear consciousness following a secondary empty sella syndrome as the sequelae of a snake bite. Mortality from snake bites accounts for 0.47% of all deaths in India with the majority of estimated global burden of mortality from snake bites to be in South Asia.[1,4]
Golay, et al., in a recently published 2 year prospective study conducted in India, has found the prevalence of 9.37% of patients with snake bites having hypopituitarism.[5] Russell's viper venom is vasculotoxic in nature capable of causing damage to the pituitary and a possible Sheehan's syndrome like pathology has been described in the causation of pituitary damage following snake bites.[6] Paranoid psychosis in clear consciousness has been described in hypopituitarism with acute and chronic presentations.[7] However, psychosis in hypopituitarism could also be a manifestation of Addison's disease and hypothyroidism.[8,9] The temporal correlation between the onset of his symptoms after the snake bite and subsequent improvement on hormone replacement clearly shows hormonal deficiency as the cause of his psychosis which didn't need any antipsychotics for treatment. The finding of empty sella on radiological imaging clinched the diagnosis in our case along with the abnormal laboratory investigations. TSH was normal in our case in the presence of low T3 and T4 hormone level which can be seen in secondary hypothyroidism.[10] The importance of a good liaison between the clinical departments cannot be stressed enough in the management of this patient.
Follow-up studies of the patients will be needed to know the prevalence of psychosis in hypopituitarism following the vasculotoxic snake bites due its acute and chronic nature and also for better understanding of the phenomenon. Left unidentified, these symptoms might become attributed to a primary psychiatric disorder while missing the medical diagnosis that could be treated. Such cases can suffer from long-term morbidity as demonstrated in our case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tun-Pe, Phillips RE, Warrell DA, Moore RA, Tin-Nu-Swe, Myint-Lwin, et al. Acute and chronic pituitary failure resembling Sheehan's syndrome following bites by Russell's viper in Burma. Lancet. 1987;2:763–7. doi: 10.1016/s0140-6736(87)92500-1. [DOI] [PubMed] [Google Scholar]
- 3.Leo RJ, Burnett GJ, Hassett MJ. Psychosis associated with hypopituitarism. Gen Hosp Psychiatry. 1998;20:248–54. doi: 10.1016/s0163-8343(98)00028-0. [DOI] [PubMed] [Google Scholar]
- 4.Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, et al. Snakebite mortality in India: A nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018. doi: 10.1371/journal.pntd.0001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golay V, Roychowdhary A, Dasgupta S, Pandey R. Hypopituitarism in patients with vasculotoxic snake bite envenomation related acute kidney injury: A prospective study on the prevalence and outcomes of this complication. Pituitary. 2014;17:125–31. doi: 10.1007/s11102-013-0477-1. [DOI] [PubMed] [Google Scholar]
- 6.Antonypillai CN, Wass JA, Warrell DA, Rajaratnam HN. Hypopituitarism following envenoming by Russell's vipers (Daboia siamensis and D. russelii) resembling Sheehan's syndrome:First case report from Sri Lanka, a review of the literature and recommendations for endocrine management. QJM. 2011;104:97–108. doi: 10.1093/qjmed/hcq214. [DOI] [PubMed] [Google Scholar]
- 7.Dissanayake SA, Leiberman DM. Hypopituitarism with paranoid psychosis: A description of two cases. J Neurol Neurosurg Psychiatry. 1969;32:233–5. doi: 10.1136/jnnp.32.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anglin RE, Rosebush PI, Mazurek MF. The neuropsychiatric profile of Addison's disease: Revisiting a forgotten phenomenon. J Neuropsychiatry Clin Neurosci. 2006;18:450–9. doi: 10.1176/jnp.2006.18.4.450. [DOI] [PubMed] [Google Scholar]
- 9.Heinrich TW, Grahm G. Hypothyroidism presenting as psychosis: Myxedema madness revisited. Prim Care Companion J Clin Psychiatry. 2003;5:260–266. doi: 10.4088/pcc.v05n0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta V, Lee M. Central hypothyroidism. Indian J Endocrinol Metab. 2011;15(Suppl 2):S99–106. doi: 10.4103/2230-8210.83337. [DOI] [PMC free article] [PubMed] [Google Scholar]


