Abstract
Purpose: To assess the short-term efficacy and quality of life (QOL) of patients with achalasia after peroral endoscopic myotomy (POEM).
Methods: Thirty-five achalasia patients underwent POEM from May 2013 to December 2013. The data on clinical evaluation and QOL before therapy, at 1 month and 6 months postoperation were collected and analyzed.
Results: All the thirty-five patients underwent POEM successfully. By comparing the data of the preoperative with that of 1 month and 6 months after POEM respectively, we found that: mean Eckardt score decreased (6.83 vs 0.51, 6.83 vs 0.46, all P <0.05), esophagus diameter reduced (47.97 mm vs 32.00 mm, 47.97 mm vs 28.50 mm, all P <0.05), and esophageal manometry declined (29.5 mmHg vs 11.5 mmHg, 29.5 mmHg vs 10.3 mmHg, all P <0.05). Complications occurred in 14.3% (5/35) of the cases, and no recurrence was observed. At each time point, postoperative QOL scores were higher than those of preoperative (P <0.05).
Conclusions: POEM is safe and effective for treating achalasia in the short-term, it can relieve clinic symptoms as well as improve patients’ QOL.
Keywords: achalasia, peroral endoscopic myotomy (POEM), short-form 36 (SF-36), quality of life
Introduction
Achalasia (AC) is a rare esophageal motility disorder characterized by aperistalsis of the esophageal body and impaired lower esophageal sphincter (LES) relaxation. Clinical manifestations include dysphagia, regurgitation, chest pain, weight loss, etc. Current treatment modalities of achalasia include pharmacologic agents, endoscopic methods (such as intrasphincteric injection of botulinum toxin, pneumatic dilatation, and endoscopic retrievable stent placement), and surgery.1) Pharmacological management such as calcium antagonists or nitrates has little effect.2) Though endoscopic methods can relieve the symptoms and improve the life quality of AC patients, the long-term efficacy is disappointing.3) Laparoscopic Heller Myotomy (LHM) is a standard surgical method for treating achalasia, and has demonstrated good long-term efficacy and life quality improvement.4,5) However, this procedure is more invasive with longer hospital stay and greater cost compared with endoscopic methods.6,7)
Peroral endoscopic myotomy (POEM) is a novel treatment for achalasia, and has shown exciting results in limited studies.8,9) However, little is known about the quality of life (QOL) outcomes after POEM. We aim to report the efficacy of POEM, investigate the QOL before and after POEM.
Materials and Methods
Study population
During May 2013 to December 2013, a total of 35 consecutive AC patients were included, and they all underwent a POEM procedure. Achalasia was diagnosed by established methods, on the basis of symptoms, esophageal manometry, esophagogastroduodenoscopy (EGD), and barium esophagram. AC patients who were evaluated not tolerable to anesthesia and those with severe cardiopulmonary disease or blood coagulation disorders (international normalized ratio >2.0, platelet count <100000/mm3) were excluded from the candidates of POEM. The study was approved by the Ethics Committee of Second Xiangya Hospital, Central South University. Informed consent was obtained from all patients before the procedure was performed. All patients were informed of possible complications and other possible treatment options.
POEM procedures
Prophylactic intravenous antibiotics and proton pump inhibitors (PPI) were introduced before the procedure. POEM was performed under general anesthesia via tracheal intubation by managing a standard single-channel endoscopy (GIF-Q260Z; Olympus, Tokyo, Japan) with a transparent cap (D-201-11802, Olympus) to the front. Carbon dioxide insufflator (UCR, Olympus) was used. Other accessories and equipment such as an argon plasma coagulation unit (APC300; ERBE), an injection needle (NM-4L-1; Olympus), a high-frequency generator (ICC 200; ERBE, Tübingen, Germany), a hybrid knife (ERBE, Tübingen, Germany), a dual knife (KD-650L; Olympus) and hemostatic clips (HX-600-135; Olympus) were also included. The POEM procedure was performed as follows: (1) A submucosal injection (a mix solution of 100 ml saline + 2 ml indigo carmine + 1 ml epinephrine) was made into the right posterior esophageal wall at about 10 cm above esophagogastric junction (EGJ). (2) A 2–3 cm longitudinal mucosal incision was made to create tunnel entry, and a bilaterally transverse dissection along submucosal layer was made to reduce the tension between mucosal entry and endoscope. (3) A submucosal tunnel was created, passing over the EGJ, and about 3 cm into the proximal stomach. The width of the submucosal tunnel was ≥3 cm. (4) Myotomy was started from 2–3 cm below tunnel entry, full-thickness myotomy at 6 cm around EGJ. (5) After careful hemostasis, several metal clips were applied to close mucosal entry.
Postoperative management
Patients were kept nil per os (NPO) for the first 24 h, a liquid diet for 3 days, and returned gradually to a soft diet within 2 weeks. Intravenous PPI and antibiotics were used for 3 days. At Day 2 post-operation, thoracoabdominal X-ray, or sometimes a chest CT were performed to check for the occurrence of emphysema, pneumothorax, pneumoperitoneum, and pleural effusion, etc.
Acquisition of data
Before POEM, a clinical evaluation was conducted and QOL was measured by Short Form-36 Health Survey (SF-36). 1 month and 6 months after therapy, clinical evaluation and QOL evaluation were performed again by outpatient service or telephone follow-up. And esophageal manometry and esophageal barium were also carried out before and after therapy.
The QOL was measured by the generic health related quality of life scale (SF-36) in its Chinese version. The SF-36 comprises 36 items divided into eight dimensions: Physical Functioning (PF), Role Physical (RP), Bodily Pain (BP), General Health (GH), Vitality (VT), Social Functioning (SF), Role Emotional (RE), and Mental Health (MH). Higher score of the health aspect imply higher QOL.
Eckardt criteria10) was used to evaluate the symptoms severity and patients were classified to four grades: grade 0, I, II, and III. Esophageal dilation was evaluated as Henderson11) reported, with grading I, II, and III.
Statistical analysis
Statistical analysis was performed with SPSS 21.0 software (Chicago, USA). Continuous variables were expressed as mean ± standard deviation, and limit or as media; and compared by paired-samples t test, or non-parametric tests. Significant differences were considered for P<0.05.
Results
Table 1 describes characteristics of the thirty-five patients with achalasia. All the thirty-five patients underwent POEM successfully, with a surgery success rate of 100%. The operation duration was from 38 min to 120 min with an average of 56.0 min. The mean follow-up time post-operation was 11.4 (6–15) months. Mean preoperative Eckardt score was (6.83 ± 1.81) and decreased to (0.51 ± 0.89) and (0.46 ± 0.56) at 1 month and 6 months postoperatively (Table 2 is a performance of each patient’s Eckardt scores before and after POEM), diameter of esophagus reduced from (47.97 ± 16.56) mm to (32.00 ± 8.08) and (28.50 ± 3.32) respectively, and preoperative resting LES also declined from (29.5 ± 12.6) mmHg to (11.5 ± 13.2) mmHg at 1 month and (10.3 ± 11.7) mmHg at 6 months postoperatively. There were significant differences in the above four parameter pre- and postoperatively (P<0.05). And there was no recurrence during the follow-up period (recurrence was defined as an Eckardt score ≥4 over 6 months post-operation).
Table 1.
Describes the characteristics of our 35 patients who underwent POEM
| Sex | |
| Male | 11 |
| Female | 24 |
| Age (years) | 40.2 (15–63) |
| Process of disease (months) | 101.6 (2–360) |
| Sigmoid-type esophagus | 2 |
| Previous therapy | |
| Calcium antagonists or nitrates | 2 |
| Balloon dilatation | 2 |
| Eckardt score class | |
| Grade 0 | 0 |
| Grade I | 1 |
| Grade II | 13 |
| Grade III | 21 |
| Esophageal dilatation degree class | |
| Grade I | 9 |
| Grade II | 21 |
| Grade III | 5 |
| Resting LES Manometry (mmHg) | 29.5 ± 12.6 |
POEM: peroral endoscopic myotomy; LES: lower esophageal sphincter
Table 2.
Eckardt scores of each patient before and after POEM
| Sequence number | Preoperatively | 1 month postoperatively | 6 months postoperatively |
|---|---|---|---|
| 1 | 10 | 1 | 1 |
| 2 | 6 | 0 | 1 |
| 3 | 5 | 0 | 0 |
| 4 | 7 | 0 | 0 |
| 5 | 10 | 2 | 1 |
| 6 | 4 | 0 | 0 |
| 7 | 7 | 0 | 0 |
| 8 | 7 | 0 | 1 |
| 9 | 5 | 0 | 0 |
| 10 | 8 | 1 | 1 |
| 11 | 9 | 0 | 0 |
| 12 | 5 | 0 | 0 |
| 13 | 5 | 0 | 0 |
| 14 | 9 | 1 | 1 |
| 15 | 7 | 0 | 0 |
| 16 | 9 | 0 | 0 |
| 17 | 4 | 1 | 0 |
| 18 | 8 | 0 | 0 |
| 19 | 8 | 1 | 1 |
| 20 | 9 | 1 | 1 |
| 21 | 3 | 0 | 0 |
| 22 | 7 | 1 | 1 |
| 23 | 5 | 0 | 0 |
| 24 | 6 | 0 | 1 |
| 25 | 4 | 0 | 0 |
| 26 | 8 | 4 | 2 |
| 27 | 6 | 0 | 0 |
| 28 | 6 | 0 | 0 |
| 29 | 7 | 0 | 1 |
| 30 | 8 | 0 | 0 |
| 31 | 9 | 2 | 1 |
| 32 | 8 | 0 | 0 |
| 33 | 7 | 0 | 0 |
| 34 | 7 | 1 | 1 |
| 35 | 6 | 2 | 1 |
| Mean ± SD | 6.83 ± 1.81 | 0.51 ± 0.89* | 0.46 ± 0.56*# |
*P <0.05 Eckardt scores of the preoperative vs those of the postoperative. #P <0.05 Eckardt scores of 1 month postoperatively vs those of 6 months postoperatively. POEM: peroral endoscopic myotomy; SD: standard deviation
Of all the thirty-five cases, five cases (14.3%) had complications. Three cases encountered neck/chest subcutaneous emphysema, and all of them were absorbed spontaneously within 3–5 days without any special intervention. One patient suffered from intractable hiccup and chest pain, which was relieved by analgesic therapy. Another patient suffered from heartburn and reflux 2 months after POEM, and EGD revealed reflux esophagitis. His symptom relieved after administration of PPI and mucosal protective agents.
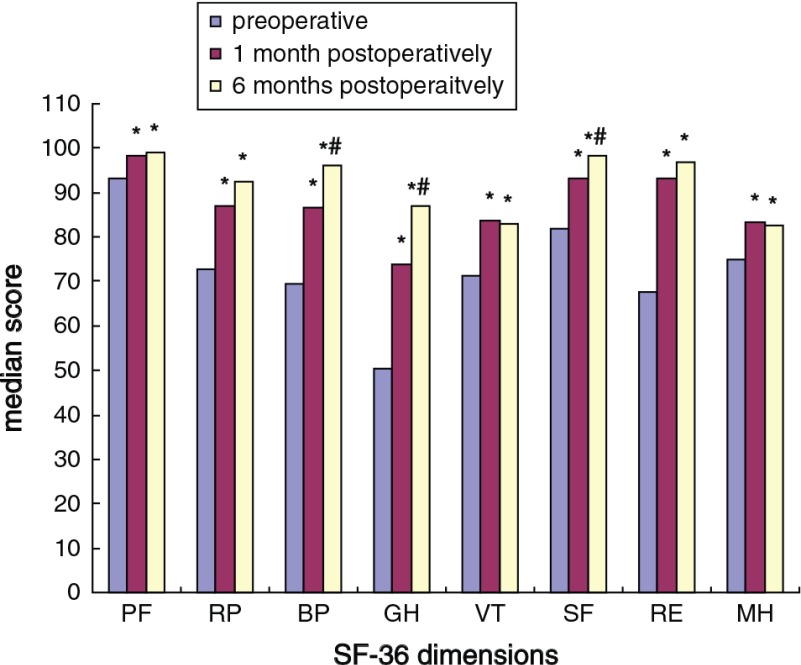
Table 3 shows QOL scores of preoperative, 1 month and 6 months postoperatively, and paired comparison results among them. After POEM, the QOL scores were improved obviously (P<0.05); compared with QOL scores at 1 month postoperatively, dimensions of bodily pain, general health, and social functioning at 6 months postoperatively were further improved. Figure 1 is a bar graph for Table 3.
Table 3.
AC patients’ QOL scores before and after POEM
| Dimensions | Preoperative | 1 month postoperatively | 6 months postoperatively |
|---|---|---|---|
| PF | 93.29 ± 9.54 | 98.14 ± 5.16* | 99.16 ± 2.45* |
| RP | 72.86 ± 40.39 | 87.14 ± 32.86* | 92.50 ± 23.6* |
| BP | 69.45 ± 25.21 | 86.74 ± 18.04* | 96.00 ± 8.66*# |
| GH | 50.29 ± 19.56 | 73.83 ± 15.73* | 86.97 ± 13.89*# |
| VT | 71.14 ± 16.14 | 83.57 ± 8.88* | 83.00 ± 3.56* |
| SF | 81.90 ± 23.97 | 93.33 ± 14.05* | 98.15 ± 6.08*# |
| RE | 67.62 ± 40.00 | 93.33 ± 23.98* | 96.76 ± 16.86* |
| MH | 74.86 ± 15.02 | 83.20 ± 8.50* | 82.67 ± 4.15* |
*P <0.05 QOL scores of the preoperative vs those of the postoperative. #P <0.05 QOL scores of 1 month postoperatively vs those of 6 months postoperatively. AC: achalasia; QOL: quality of life; POEM: peroral endoscopic myotomy; PF: physical functioning; RP: role physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role emotional; MH: mental health
Fig. 1.
The scores are performed as mean scores given in Table 3. *P <0.05 QOL scores of the preoperative vs those of the postoperative. #P <0.05 QOL scores of 1 month postoperatively vs those of 6 months postoperatively. QOL: quality of life
Discussion
AC is a chronic and progressive disease, affected patients often suffer from recurrent dysphagia and vomiting, which severely impair consumption of adequate amount of food and lower health status.12) Moreover, the disease may increase economic and healthcare burdens, and decrease work productivity, which greatly impair patients’ QOL.13) Some studies13,14) have demonstrated that QOL scores for AC patients were lower than that of general population. Among treatment methods for AC, POEM is a novel therapy, some studies have shown exciting short-term clinical efficacy.15,16) In the present study, we found that after POEM, the diameter of patients’ esophagus reduced, the Eckardt score decreased, and EGD showed no retention in the esophageal lumen and a unobstructed cardiac orifice. All these findings demonstrated that POEM could relieve obstruction of the LES. All the symptoms of the thirty-five cases relieved after POEM and no recurrence was observed during periodical follow-up. Only five cases had complications, and all the complications were treated by conservative methods successfully. So our results had also tested the safety and efficacy of POEM.
Meanwhile, we found POEM can obviously promote the AC patients’ QOL at preoperative level. The investigation represented that every concept of postoperative QOL scores was significantly higher than preoperative at 1 month and 6 months postoperatively which showed that POEM can improve the patients’ QOL in every dimensions, and the improvement persists with follow-up time extending. These is a little different from results of a recent published paper,17) which reported POEM can only promote QOL of several concepts: emotinonal well-being at postoperative at 3 weeks; emotional well-being, social functioning and general health at postoperative 6 months; and role limitation and social functioning at postoperative 1 year. We both performed the evaluation at early postoperative time, but our results showed POEM can improve patients’ QOL scores in all dimensions but not just in one or two.
Moreover, we compared QOL scores of 1month to 6 months postoperatively, and found that health aspect scores of bodily pain, general health and social functioning were significantly higher at 6 postoperative months. This indicated that the improvement effect became more prominent at 6 months after POEM. POEM could relieve obstruction of LES, and the operation wound is healing with time. These two elements both reduce pain and improved QOL of bodily pain. Increase of nutrition intake after POEM can promote patients’ general health and self-confidence, and the patients will make good performance in their personal relationship and improve the social functioning.
Most of the researchers focus on the promising clinical efficacy on relieving symptoms, however, both good clinical efficacy and improvement of QOL of patients after therapy are very important criteria to evaluate the medical treatment.18) Our investigation has testified that POEM is a suitable method for AC patients which could relieve the symptoms and wholely promote the postoperatively physical and psychological QOL level of the patients.
One limitation of our study is the small sample size, with only thirty-five cases included. The other is the relatively short-term follow-up time with a mean of just 11.4 months. Thus, a large-scale, randomized study between LHM and POEM, and long-term follow-up would be required to more accurately evaluate the long-term efficacy and improvement of QOL. In summary, our study showed that POEM is safe and effective for treating achalasia in the short-term as it can relieve the symptoms as well as improve the QOL. The improvement of QOL appears early after POEM, and its effect persists or becomes more prominent after 6 months without long term complication.
Conflict of Interest
All authors stated that there is no conflict of interest.
Acknowledgements
Thanks to numerous individuals participated in this study, and we acknowledge the editors and the anonymous reviewers for insightful suggestions on this work.
References
- 1).Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 2011; 8: 311-9. [DOI] [PubMed] [Google Scholar]
- 2).Chuah SK, Hsu PI, Wu KL, et al. 2011 update on esophageal achalasia. World J Gastroenterol 2012; 18: 1573-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Chuah SK, Hu TH, Wu KL, et al. Clinical remission in endoscope-guided pneumatic dilation for the treatment of esophageal achalasia: 7-year follow-up results of a prospective investigation. J Gastrointest Surg 2009; 13: 862-7. [DOI] [PubMed] [Google Scholar]
- 4).Gockel I, Junginger T, Eckardt VF. Long-term results of conventional myotomy in patients with achalasia: a prospective 20-year analysis. J Gastrointest Surg 2006; 10: 1400-8. [DOI] [PubMed] [Google Scholar]
- 5).Chen Z, Bessell JR, Chew A, et al. Laparoscopic cardiomyotomy for achalasia: clinical outcomes beyond 5 years. J Gastrointest Surg 2010; 14: 594-600. [DOI] [PubMed] [Google Scholar]
- 6).Nhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, long-term outcomes of surgical Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2012; 259: 1098-103. [DOI] [PubMed] [Google Scholar]
- 7).Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 2013; 154: 893-7; discussion 897-900. [DOI] [PubMed] [Google Scholar]
- 8).Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42: 265-71. [DOI] [PubMed] [Google Scholar]
- 9).Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 2013; 145: 309-11. [DOI] [PubMed] [Google Scholar]
- 10).Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 2004; 53: 629-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Henderson RD. Esophageal motor disorders. Surg Clin North Am 1987; 67: 455-74. [DOI] [PubMed] [Google Scholar]
- 12).Decker G, Borie F, Bouamrirene D, et al. Gastrointestinal quality of life before and after laparoscopic Heller myotomy with partial posterior fundoplication. Ann Surg 2002; 236: 750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Nenshi R, Takata J, Stegienko S, et al. The cost of achalasia: quantifying the effect of symptomatic disease on patient cost burden, treatment time, and work productivity. Surg Innov 2010; 17: 291-4. [DOI] [PubMed] [Google Scholar]
- 14).Ben-Meir A, Urbach DR, Khajanchee YS, et al. Quality of life before and after laparoscopic Heller myotomy for achalasia. Am J Surg 2001; 181: 471-4. [DOI] [PubMed] [Google Scholar]
- 15).Swanstrom LL. Peroral endoscopic myotomy for treatment of achalasia. Gastroenterol Hepatol (NY) 2012; 8: 613-5. [PMC free article] [PubMed] [Google Scholar]
- 16).Sharata A, Kurian AA, Dunst CM, et al. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 2013; 17: 1188-92. [DOI] [PubMed] [Google Scholar]
- 17).Vigneswaran Y, Tanaka R, Gitelis M, et al. Quality of life assessment after peroral endoscopic myotomy. Surg Endosc 2015; 29: 1198-202. [DOI] [PubMed] [Google Scholar]
- 18).Cox DR, Fitzpatrick R, Fletcher AE, et al. Quality-of-life assessment: can we keep it simple? J R Statist Soc A 1992; 155: 353-93. [Google Scholar]