Abstract
Purpose: The purpose of this study was to research the use of near-infrared spectroscopy (NIRS) on the neurocognitive functions in the patients undergoing coronary artery bypass grafting (CABG) with asymptomatic carotid artery disease.
Methods: The study design was carried out with the participation of 79 patients in a prospective, randomized and double blind control method. The patients were separated into two groups as NIRS (n = 43) and no NIRS (n = 36). A neurocognitive test was applied preoperatively and postoperatively to all patients before discharge. Cognitive functions were evaluated by applying the Montreal Cognitive Assessment test (MoCA).
Results: The decrease in the postoperative score of mean MoCA in no NIRS group was statistically significant when compared to preoperatively (p <0.001). Postoperative mean MoCA score was found to be significantly higher in NIRS group (NIRS: 26.8 ± 1.9 vs. no NIRS: 23.6 ± 2.5, p <0.001). It has been determined that there was a moderately positive significant correlation between the increase in the NIRS used patients (%) and increase in the MoCA score of the patients (r = 0.59, p <0.001).
Conclusion: Intraoperative NIRS usage in the patients undergoing CABG with carotid artery disease might be useful due to its postoperative positive effects on the cognitive functions.
Keywords: near-infrared spectroscopy, mild cognitive impairment, coronary artery bypass, carotid atherosclerotic disease
Introduction
Over the years, operability criterias for cardiac surgery has been enhanced. Therefore, averege age of operated patients and co-morbidities have increased.1) Cerebral injury is one of the most important complications of cardiac surgery which may cause mortality, morbidity, increased hospital costs and impaired quality of life. Perioperative cerebral injury includes stroke that occurs in 1.5% to 5.2% of patients, encephalopathy affecting 8.4% to 32% of patients.2) Cognitive dysfunction has been reported in approximately 50% of patients at discharge, 36% at 6 weeks, 26%–33% at one year, and 42% at five years.3,4) Pre-exisiting atherosclerotic plaque, thrombogenesis from the foreign surfaces of cardiopulmonary bypass, air from the cardiopulmonary bypass circuit, and pericardial fat globules are tought to be primary predictors of cognitive decline by creating microemboli during cardiac surgery.5) Cognitive dysfunction may propound clinical manifestations such as deterioration in memory, attention, (psycho) motor speed, and visuospatial ability. The incidence of cognitive dysfunction varies considerably but may be as high as 50% to 70% at 1 week after surgery, declining to 30% to 50% after two months.6) Near-infrared spectroscopy (NIRS) is a system used for monitoring brain activity. NIRS is based on the absorption of infrared light by biological tissues in a fashion similar to arterial saturometry. NIRS has one transmitter and two receptors. One receptor takes the signals from extracerebral tissue while other one takes signals from the junction of anterior and middle cerebral artery.7)
The aim of the study was to examine usefulness of intraoperative cerebral oxymetry monitoring on the neurocognitive functions in the patients undergoing coronary artery bypass grafting with asymptomatic carotid artery disease.
Materials and Methods
After the ethical approval is taken, this study is started to be carried out as randomized, controlled and with a double blind working design in the cardiovascular surgery department in a tertiary healthcare center. Study has started with 88 consecutive patients who had coronary artery bypass grafting (CABG) operation with asymptomatic carotid artery disease for whom no intervention is intended (carotid artery stenosis is between ≥50% and <70% on Doppler ultrasonography (USG)) in our clinic between December 2013 and February 2015. Two of these patients were excluded because of the refussion to participate in the study, four of them were excluded for the reasons of having 2 and 3 degrees of atherosclerosis in the ascending aorta (high possibility of lifting the atherosclerosis plaque), three of them were excluded since additional procedures such as mitral ring annuloplasty and aortic valve replacement. Informed consent form was taken from all the patients attending the study. The patients were separated into two groups as the patients to whom intraoperative near-infrared spectroscopy is applied (NIRS group) and not applied (no NIRS group). For the 79 remaining patients after the excluded patients were randomized to one of the two groups as NIRS (n = 43) or no NIRS (n = 36) by using the block method, which featured two permutations. Randomization list has been generated by the clinic head nurse and the patients were sent to the surgery in accordance with such list and the randomization list was kept hidden until the study is concluded.
The patients who had an additional procedure other than CABG, who had a ascending aortic atherosclerosis degree of ≥2, carotid artery stenosis ≥70% lesions on carotid Doppler USG, who had a low level of literacy, who had a clinical history of cerebrovascular attack, fit and who had psychiatric disorders were not included in this study.
All the operations were carried out by the same surgery and anesthesia team by using the standard surgical methods and cardioplegia protocols by means of on-pump cardiopulmonary bypass (CPB). All the patients were applied intraoperative epiaortic ultrasonography (EAU) by the same radiologist and the level of atherosclerosis in their aortic walls were assessed. Atherosclerotic changes in the level of atherosclerosis in ascending aorta accordance with the Modified Wareing classification used by Goto et al.8) (the section between ascending aorta, aortic valve and innominate artery has been separated in 3 areas and evaluated with EAU): The classification is carried out as 0 (normal); 1 (mild, >3 mm intimal thickness); 2 (medium, ≥3 mm intimal thickness in the 1 segment of ascending aorta) and 3 (severe, ≥3 mm intimal thickness in two or three segments, frequently accompanying luminal protrusion, ulceration of the mobile structure and plaque surface).
Myocardial protection has been applied on all of the patients at 30°C–32°C body temperature under mild hypothermia by using the intermittent antegrade cold blood cardioplegia in every 15 min and by both intermittent antegrade and continuous retrograde method when necessary (such as major coronary lesion, critical proximal lesion, advanced left ventricular dysfunction). Distal anastomosis is carried out under cross-clamp and proximal anastomosis is carried out under side-clamp in all the cases with the double clamp method. Cardiopulmonary bypass standard flow speed was used 2.2–2.6 L/min/m2, partial carbon dioxide was 40 mm Hg and above with the alpha-stat method, average arterial pressure was between 50–80 mm Hg, hematocrit (Hct) was between 20%–25%.
Preoperative and postoperative cognitive test has been applied to all the patients by two perfusionists under the supervision of the neurologist in accordance with the randomization list of the head nurse and it has been evaluated by two observers by using double blind method. Cognitive functions were evaluated by applying the Montreal Cognitive Assessment test (MoCA).9) Neurologic evaluation contained the evaluation of visual and speech disorders, paralysis in the upper and/or lower extremities or weakness and mental state.
Aortic cross-clamp periods, total CPB periods, atherosclerosis in ascending aorta degrees (by EAU), intensive care and duration of hospital stay and rSO2 parameters of all the patients were recorded.
Montreal Cognitive Assessment Test
Montreal Cognitive Assessment (MoCA), has been developed as a fast scanning test for mild cognitive disorder. MoCA evaluates different cognitive functions. These are attention and concentration, coordinating functions, memory, language, visual structuring skills, abstract thought, calculation and orientation. The application of MoCA takes about 10 min. The maximum score to get from this test is 30. According to this, 26 points and above are evaluated as normal, between 19–25 points are evaluated as mild cognitive disorder and below 19 are evaluated as serious cognitive disorders.9,10)
Evaluation of Near-Infrared Spectroscopy and Cerebral Oxygen Saturation
Near infrared spectroscopy (NIRS), measures regional cerebral oxygenation (rSO2). It interprets the oxy and deoxy hemoglobin: rSO2 = oxyhemoglobin/total oxyhemoglobin. Hemoglobin signal is weighted 75%–85% venous and 15%–25% arterial. Due to this normal rSO2 values are above 60%. The function is calculated by the machine based on Optical Sampling Density (OSD) or the depth of the possibility of a light beam to encounter a hemoglobin molecule. There is a light source and two different light sensors on the prop placed in fronto-temporal region. Data is taken from extra cranial (skin and bones) tissue with the sensor which is 3 cm away and both from extra cranial and brain tissue with the sensor which is 4 cm away. INVOSR (Somanetics, Michigan) sample is obtained by calculating the difference between two sources.11–13)
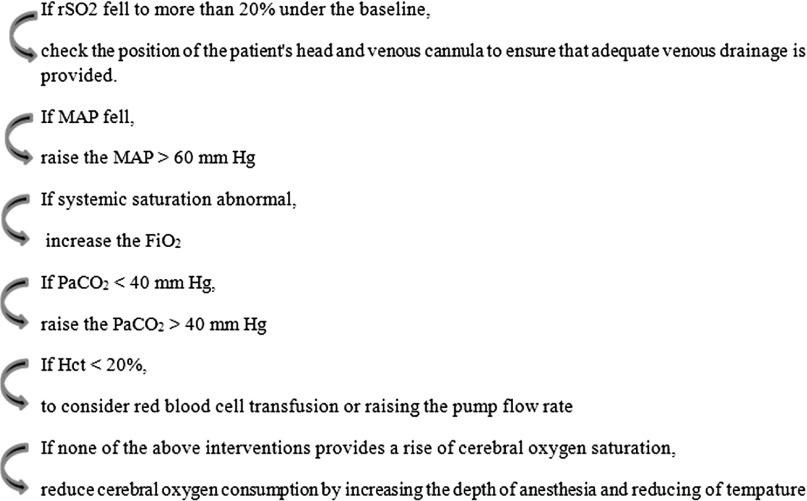
All the patients in NIRS group are monitored by using the INVOS system (INVOS 5100C; Somanetics Corp, Troy, MI, USA). INVOS is a system based on NIRS in the continuous and non-invasive measurement of the changes in the cerebral oxygen saturation. NIRS probes are placed in the fronto-temporal region on the brows of the patients from both sides. The distance between two probes is set as 4 cm. rSO2 values are recorded and some values are determined while the patients were awake before the induction of anesthesia. After cross-clamps are placed, rSO2 changes of the patients during cardiopulmonary bypass (CPB) have been recorded in excel format in computer environment by the perfusionist and were evaluated by two observers with double blind method. The algorithm used as standard12) which is suggested for the brain oxymetry use when there is a >20% decrease in the rSO2 values of the NIRS group patients during CPB when compared to their initial values (Fig. 1).
Fig. 1.
The algorithm for the treatment of cerebral desaturation. FiO2: fraction of inspired oxygen; Hct: hematocrit; MAP: mean arterial pressure; PaCO2: partial carbon dioxide; rSO2: regional cerebral oxygenation
Results
Preoperative demographic findings and risk factors are shown in Table 1. There were no statistical difference by means of preoperative data and risk factors between NIRS and no NIRS groups. Preoperative mean MoCA scores were similar in NIRS and no NIRS groups (p = 0.63).
Table 1.
Comparison between the groups based on demographic characteristics and clinical factors
| Factors | NIRS Group (n = 43) | No NIRS Group (n = 36) | p |
|---|---|---|---|
| Age, years | 59.1 ± 9.4 | 61.2 ± 10.3 | 0.34 |
| Gender, female, n (%) | 10 (23.3) | 7 (19.4) | |
| male, n (%) | 33 (76.7) | 29 (80.6) | 0.89 |
| Preoperative | |||
| Hypertension, n (%) | 31 (72.1) | 28 (77.8) | 0.74 |
| Diabetes, n (%) | 13 (30.2) | 11 (30.6) | 0.97 |
| COPD, n (%) | 7 (16.3) | 5 (13.9) | 0.76 |
| Chronic RI, n (%) | 1 (2.3) | 0 (0) | 1.00 |
| Smoking, n (%) | 33 (76.7) | 25 (69.4) | 0.63 |
| Family history of CVD, n (%) | 8 (18.6) | 2 (5.6) | 0.11 |
| Atrial fibrillation, n (%) | 1 (2.3) | 2 (5.6) | 0.58 |
| Left ventricle EF, % | 52.9 ± 5.8 | 55.4 ± 6.3 | 0.07 |
| Intraoperative | |||
| CPB time, minutes | 77.7 ± 28.3 | 78.6 ± 26.9 | 0.88 |
| ACC time, minutes | 48.8 ± 23.1 | 56.3 ± 25.8 | 0.17 |
| Mean no. of bypass graft | 2.65 ± 0.78 | 2.72 ± 0.65 | 0.67 |
| Postoperative | |||
| ICU length of stay, days | 1.74 ± 0.81 | 2.12 ± 1.05 | 0.09 |
| Hospital length of stay, days | 7.15 ± 1.39 | 7.67 ± 1.14 | 0.08 |
ACC: aortic cross-clamp; CPB: cardiopulmonary bypass; COPD: chronic obstructive pulmonary disease; CVD: cerebrovascular diseases; EF: ejection fraction; NIRS: near infrared spectroscopy; RI: renal insufficiency; ICU: intensive care unit
In NIRS group there was a postoperative decrease in the mean MoCA score when compared to preoperative but this was not statistically (p = 0.44). In no NIRS group, postoperative decrease in the mean MoCA score was statistically significant when compared to preoperative (p <0.001).
Before postoperative discharge the cognitive functions of the patients were re-evaluated again with MoCA test. When the postoperative mean MoCA scores of both groups were evaluated, it was 26.8 ± 1.9 in NIRS group and 23.6 ± 2.5 in no NIRS group. Postoperative mean MoCA score was found to be significantly higher in NIRS group (NIRS: 26.8 ± 1.9 vs no NIRS: 23.6 ± 2.5, p <0.001). MoCA items mean scores and MoCA score range of groups after the surgery can be seen in Table 2.
Table 2.
MoCA items mean scores and MoCA score range of groups after the surgery
| MoCA items | NIRS Group (n = 43) | no NIRS Group (n = 36) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Alternating trail making | 0.74 | 0.43 | 0.52 | 0.49 |
| Visuoconstructional skills (cylinder) | 0.88 | 0.32 | 0.66 | 0.47 |
| Visuoconstructional skills (clock) | 2.59 | 0.49 | 2.25 | 0.59 |
| Naming | 2.73 | 0.47 | 2.52 | 0.68 |
| Memory | 3.98 | 1.25 | 1.39 | 0.72 |
| Attention | 1.99 | 0.77 | 1.92 | 0.87 |
| Vigilance | 0.83 | 0.37 | 0.80 | 0.39 |
| Serial 7s | 2.52 | 0.62 | 2.81 | 0.46 |
| Sentence repetition | 1.86 | 1.05 | 1.75 | 1.13 |
| Verbal fluency | 0.71 | 0.48 | 0.76 | 0.41 |
| Abstraction | 1.97 | 0.81 | 1.80 | 0.76 |
| Delayed recall | 5.53 | 0.60 | 5.45 | 0.64 |
| Mean MoCA scores | 26.8 | 1.9 | 23.8 | 2.5 |
| MoCA score range | 21–30 | 17–30 | ||
MoCA: Montreal Cognitive Assessment; NIRS: near infrared spectroscopy; SD: standard deviation
In the postoperative period, severe cognitive disorder was not determined in any of the NIRS patients (0%). Together with this mild cognitive disorder was determined in seven patients (16.3%) in NIRS group. In no NIRS group three patients (8.3%) were determined to have severe and 16 patients (44.4%) were determined to have mild cognitive function disorder. Postoperative mild cognitive function disorder was significantly higher in no NIRS group when compared to NIRS group (p = 0.01). Although severe cognitive disorder is determined to be higher in no NIRS group, there was not a major difference when compared to the NIRS group (p = 0.09) (Table 3). No meaningful disorders in neurologic evaluation (visual and speech disorders, paralysis in the upper and/or lower extremities or weakness and mental state) for both groups.
Table 3.
Comparison between the groups of cognitive function impairment before and after the surgery
| Cognitive function | Preoperative | Postoperative | ||||
|---|---|---|---|---|---|---|
| NIRS (n = 43) | No NIRS (n = 36) | p | NIRS (n = 43) | No NIRS (n = 36) | p | |
| Mild impairment, n (%) | 3 (6.9) | 5 (13.8) | 0.46 | 7 (16.3) | 16 (44.4) | 0.01 |
| Serious impairment, n (%) | 0 (0) | 0 (0) | 1.00 | 0 | 3 (8.3) | 0.09 |
| MoCA mean score, mean ± SD | 27.1 ± 1.8 | 26.9 ± 1.9 | 0.63 | 26.8 ± 1.9 | 23.7 ± 2.5 | <0.001 |
MoCA: Montreal Cognitive Assessment; NIRS: near infrared spectroscopy; SD: standard deviation
The duration of intensive care unit staying was not statistically different between groups (p = 0.09). The hospital length of stay after the surgery was higher in no NIRS group (7.15 ± 1.39 vs. 7.67 ± 1.14) but this was not statistically significant (p = 0.08).
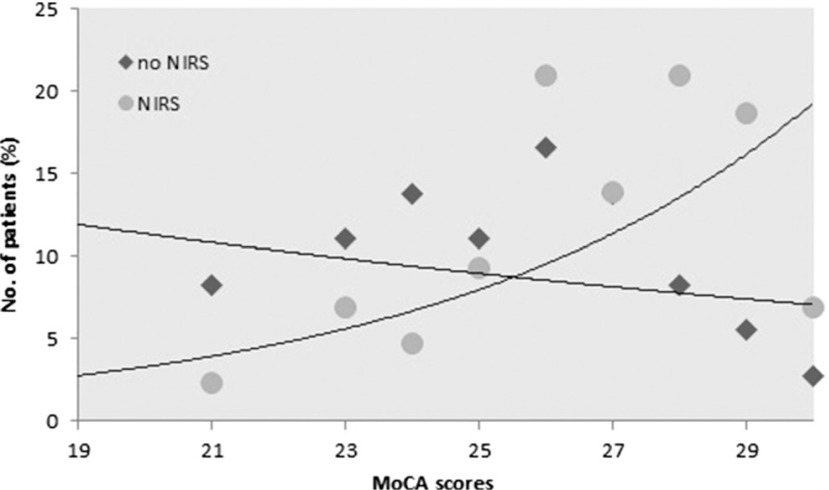
The relationship between intraoperative NIRS usage and postoperative mild cognitive disorder has been evaluated with correlation test. It has been determined that there was a moderately positive significant correlation between the increase in the MoCA score of the patients and the increase in the number of the patients (%) to whom NIRS is applied (r = 0.59, p <0.001). On the contrary, it has been seen that there is a weak and meaningless correlation between the number of the patients to whom NIRS was not applied and the increase in the MoCA score (r = – 0.12, p = 0.49) (Fig. 2).
Fig. 2.
The correlation between the number of the patients (%) in NIRS and no NIRS groups and MoCA scores. MoCA: Montreal Cognitive Assessment; NIRS: near-infrared spectroscopy
Discussion
In our study, standardized cerebral desaturation algorithm has been applied when rSO2 basal value is decreased more than 20% in the patients for whom cerebral oxygenation follow-up is being made with intraoperative NIRS method. It has been determined that the mild cognitive disorder was statistically lower in NIRS group than no NIRS group (16.3% vs. 44.4%) and severe cognitive impairment was not seen.
One of the most important things which affect the quality of life after open heart surgeries are the neurological results. The frequency of observing neurological damage after CABG changes between 1%–5% clinically and 50%–70% sub clinically.14) When this rate is evaluated as a cognitive disorder it is presented as 60% in the early period and 25%–30% in the late period.15) Of course, lots of patient-specific factors such as cranial system or atherosclerosis in ascending aorta affects neurologic damage.16)
Even though the exact relationship between coronary and carotid artery disease has been shown, the incidence rate could not be determined exactly because of the presence of many asymptomatic patients. Hemodynamically rate of significant stenosis (70% or more stenosis) in patients scheduled for myocardial revascularization has been reported between 2.8%–11.8% in various publications.17,18) Coronary artery diseases has been identified in half of patients with carotid artery diseases.19) While coronary artery surgery is a individual risk factor for cognitive damage, its association with the carotid artery becomes an important factor contributing to such risk.20,21) Thus, even if there is no indication of intervention, in the presence of carotid artery disease, the need arises for more effective and advanced monitoring when compared to standard monitoring of the brain in the patients who had CABG. NIRS method which is developed for such purposes, is easy to use, effective, non-invasive and offers a timely intervention and it is used for the purposes of measuring the saturation of regional brain tissue.22,23) NIRS monitoring is used routinely in our clinic in open heart surgeries.
Mahanna et al.24) reported 1%–35% impaired cognitive functions 6 weeks after the surgery and Slater et al.23) reported this rate as 60% in the early postoperative period. It has been reported that early term cognitive disorder improvement ratio and duration of hospital stay is longer in the patients who had a longer than 50 min of cerebral saturation period (decrease of rSO2 more than 20% than basal value) in the cerebral oxygenation follow-up via intraoperative NIRS method. Some researchers showed that even for a short period in which rSO2 value would be under the level of 50%, this increases the duration of hospital stay, neurologic damage and impairment of cognitive functions significantly.25–27)
In a study regarding the use of NIRS, the patients were randomized during CABG and NIRS monitoring is applied to one group as double blind method and actively to the other group. It has been determined that the group to whom Active NIRS monitoring is applied and intervention is made as standardized, had less extended desaturations and shorter hospital stay durations and decreased vital organ mortality and morbidity.28) In our study, while the NIRS group had a cognitive function impairment of 16.3%, it has been found significantly higher with 44.4% in no NIRS group. While severe cognitive disorder is not observed in NIRS group, it is observed in three patients in no NIRS group. It has also been determined that postoperative mean MoCA score is statistically lower in no NIRS group than NIRS group.
Conclusion
As a result, effective monitoring of the oxygenation of the cerebral tissue of the patients who had CABG in the presence of a risk factor such as carotid artery disease which requires no intervention, could significantly affect postoperative cognitive functions. Based on the positive effects of the NIRS method which is reflected on the results of our study, it could be preferred in the possible conditions as a result of its ease of use, the fact that it provides continuous cerebral monitoring and intervention and due to its beneficial effects over the postoperative cognitive functions.
Disclosure Statement
Any instution and organisation did not help us and our institution for this study. There is no conflict of interest related to the article.
References
- 1).Arrowsmith JE, Grocott HP, Reves JG, et al. Central nervous system complications of cardiac surgery. Br J Anaesth 2000; 84: 378-93. [DOI] [PubMed] [Google Scholar]
- 2).Hogue CW, Gottesman RF, Stearns J. Mechanisms of cerebral injury from cardiac surgery. Crit Care Clin 2008; 24: 83-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med 2001; 344: 395-402. [DOI] [PubMed] [Google Scholar]
- 4).Van Dijk D, Jansen EW, Hijman R, et al. Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA 2002; 287: 1405-12. [DOI] [PubMed] [Google Scholar]
- 5).Blauth CI. Macroemboli and microemboli during cardiopulmonary bypass. Ann Thorac Surg 1995; 59: 1300-3. [DOI] [PubMed] [Google Scholar]
- 6).Newman MF, Mathew JP, Grocott HP, et al. Central nervous system injury associated with cardiac surgery. Lancet 2006; 368: 694-703. [DOI] [PubMed] [Google Scholar]
- 7).Taillefer MC, Denault AY. Cerebral near-infrared spectroscopy in adult heart surgery: systematic review of its clinical efficacy. Can J Anaesth 2005; 52: 79-87. [DOI] [PubMed] [Google Scholar]
- 8).Goto T, Baba T, Matsuyama K, et al. Aortic atherosclerosis and postoperative neurological dysfunction in elderly coronary surgical patients. Ann Thorac Surg 2003; 75: 1912-8. [DOI] [PubMed] [Google Scholar]
- 9).McLennan SN, Mathias JL, Brennan LC, et al. Validity of the montreal cognitive assessment (MoCA) as a screening test for mild cognitive impairment (MCI) in a cardiovascular population. J Geriatr Psychiatry Neurol 2011; 24: 33-8. [DOI] [PubMed] [Google Scholar]
- 10).Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695-9. [DOI] [PubMed] [Google Scholar]
- 11).Colak Z, Borojević M, Ivancan V, et al. The relationship between prolonged cerebral oxygen desaturation and postoperative outcome in patients undergoing coronary artery bypass grafting. Coll Antropol 2012; 36: 381-8. [PubMed] [Google Scholar]
- 12).Akpek EA. Cerebral monitoring in cardiac surgery. J Anesth-JARSS 2008; 16: 117-24. [Google Scholar]
- 13).Casati A, Spreafico E, Putzu M, et al. New technology for noninvasive brain monitoring: continuous cerebral oximetry. Minerva Anestesiol 2006; 72: 605-25. [PubMed] [Google Scholar]
- 14).Lozano S, Mossad E. Cerebral function monitors during pediatric cardiac surgery: can they make a difference? J Cardiothorac Vasc Anesth 2004; 18: 645-56. [DOI] [PubMed] [Google Scholar]
- 15).Ahonen J, Salmenperä M. Brain injury after adult cardiac surgery. Acta Anaesthesiol Scand 2004; 48: 4-19. [DOI] [PubMed] [Google Scholar]
- 16).Yoon BW, Bae HJ, Kang DW, et al. Intracranial cerebral artery disease as a risk factor for central nervous system complications of coronary artery bypass graft surgery. Stroke 2001; 32: 94-9. [DOI] [PubMed] [Google Scholar]
- 17).Akins CW, Moncure AC, Daggett WM, et al. Safety and efficacy of concomitant carotid and coronary artery operations. Ann Thorac Surg 1995; 60: 311-8. [DOI] [PubMed] [Google Scholar]
- 18).Faggioli GL, Curl GR, Ricotta JJ. The role of carotid screening before coronary artery bypass. J Vasc Surg 1990; 12: 724-31. [DOI] [PubMed] [Google Scholar]
- 19).Hertzer NR, Loop FD, Taylor PC, et al. Combined myocardial revascularization and carotid endarterectomy. Operative and late results in 331 patients. J Thorac Cardiovasc Surg 1983; 85: 577-89. [PubMed] [Google Scholar]
- 20).Ricotta JJ, Faggioli GL, Castilone A, et al. Risk factors for stroke after cardiac surgery: Buffalo Cardiac-Cerebral Study Group. J Vasc Surg 1995; 21: 359-63. [DOI] [PubMed] [Google Scholar]
- 21).Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 1996; 335: 1857-63. [DOI] [PubMed] [Google Scholar]
- 22).Tan ST. Cerebral oximetry in cardiac surgery. Hong Kong Med J 2008; 14: 220-5. [PubMed] [Google Scholar]
- 23).Slater JP, Guarino T, Stack J, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009; 87: 36-44. [DOI] [PubMed] [Google Scholar]
- 24).Mahanna EP, Blumenthal JA, White WD, et al. Defining neuropsychological dysfunction after coronary artery bypass grafting. Ann Thorac Surg 1996; 61: 1342-7. [DOI] [PubMed] [Google Scholar]
- 25).Yao FS, Tseng CC, Ho CY, et al. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 2004; 18: 552-8. [DOI] [PubMed] [Google Scholar]
- 26).Monk TG, Reno KA, Olsen BS. Postoperative cognitive dysfunction is associated with cerebral oxigen desaturation. Anesthesiology 2000; 93: A167. [Google Scholar]
- 27).BhaskerRao B, VanHimbergen D, Edmonds HL, et al. Evidence for improved cerebral function after minimally invasive bypass surgery. J Card Surg 1998; 13: 27-31. [DOI] [PubMed] [Google Scholar]
- 28).Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 2007; 104: 51-8. [DOI] [PubMed] [Google Scholar]