Abstract
Delayed presentation of children with cancer is a significant barrier to improving the survival from children’s cancer in low- and middle-income countries (LMICs). Botswana, a country of approximately 2 million people in southern Africa, has only 1 pediatric cancer treatment program, based at Princess Marina Hospital (PMH) in the capital of Gaborone. A pediatric cancer recognition training program was developed that reached 50% of the government hospitals in Botswana teaching 362 health care workers how to recognize and refer children with cancer to PMH. Through evaluation of attendees, limitations in pediatric cancer training and general knowledge of pediatric cancer were identified. Attendees demonstrated improvement in their understanding of pediatric cancer and the referral process to PMH following the workshop.
Keywords: Africa, Botswana, cancer, training, education, pediatric cancer, pediatric oncology, delayed presentation
Introduction
Worldwide, 160 000 children are diagnosed with cancer each year. Approximately 29 000 of those children are in sub-Saharan Africa where resources for pediatric cancer are very limited.1 The overall cure rate is 80% for children with cancer in high-income settings like the United States and Europe. In low- and middle-income countries (LMICs), where children are often diagnosed too late or not diagnosed at all, the majority die from these curable cancers.2 One of the many barriers to survival of pediatric cancer in LMICs is late presentation.3-7
The only services for children with cancer in Botswana are offered at Princess Marina Hospital (PMH), the main government referral hospital in the capital of Gaborone. Since 2007, Baylor College of Medicine (BCM) and Texas Children’s Cancer and Hematology Centers (TXCH) have maintained a full-time pediatric hematologist-oncologist at PMH.8 To build local capacity, numerous pediatric cancer training programs have been offered at PMH through BCM/TXCH, including the development of a comprehensive pediatric hematology-oncology curriculum for a 5-day workshop at PMH to a multidisciplinary group of 30 health care workers in Botswana.9 Whereas most training focused on the care of a child with cancer and was based at PMH, training that focused on timely recognition and referral by primary health care workers throughout the country was necessary. Therefore, a pediatric cancer awareness training program was developed to reach health care workers at hospitals throughout Botswana.
Methods
Botswana is similar in size to the state of Texas, with a population of 2.2 million people.10 It has 25 government medical hospitals, including primary, district, and two of which are referral hospitals. There are also two faith-based mission and government partnership hospitals, and there is one psychiatric hospital. Hospitals are strategically located across the country, with district and referral hospitals in the population centers. Hospitals and clinics in rural Botswana have long relied on outreach from PMH and Gaborone for medical education and clinical assistance.11,12 The goal of the pediatric cancer recognition program was to visit at least 50% of the hospitals throughout Botswana to educate health care workers on warning signs of pediatric cancer and to inform health care workers of pediatric cancer services available at PMH.
Pediatric cancer recognition training workshops were organized with leadership at each hospital. The full-time BCM/TXCH pediatric hematologist-oncologist based at PMH developed and delivered the teaching. The teaching format was open-forum didactic sessions, with lectures using pictures of physical exam, radiographic, hematological, and/or pathological findings to illustrate presentations of pediatric cancers. The length of the workshops was determined by hospital leadership and varied from 2 hours to 1 day. All health care workers were welcome to attend with a focus on physicians and nurses who typically have the most patient contact and are the decision makers with respect to clinical care.
All attendees of the training sessions were asked to complete a pretest evaluation assessing their knowledge of the burden of cancer in children, survivability of pediatric cancer in ideal settings, and the most common types of cancer in children. Additionally, attendees were asked about any training in pediatric oncology either during their preservice and/or clinical training years. Finally, attendees were asked to indicate their comfort with caring for children with cancer and their understanding of the referral process to PMH. Following the presentations, they were asked to complete the same questions regarding pediatric cancer,their comfort level with pediatric cancer patients, and their ability to refer a child with suspected cancer to PMH as well as an evaluation of the speaker and the presentations. Statistical analysis of the questionnaires included expressing responses as percentages, evaluating ordinal data as means, and χ2 analyses of respondents’ responses by medical specialty. Statistical analyses were done using STATA, version 11 (StataCorp LP, College Station, TX).
Results
Pediatric cancer recognition training workshops were offered at 14 (53.8%) of the 26 government/mission hospitals in Botswana, excluding PMH, over a 10-month period (Figure 1). Of the 362 health care workers who attended a workshop, 279 (77.1%) completed the pretest, posttest, self-assessment, and evaluation. Nurses represented the majority of attendees who identified their profession, at 49.2% (178/362), whereas physicians represented 30.1% (109/362).
Figure 1.
Pediatric cancer recognition training sites in Botswana.
Only 7.4% (20/272) of attendees completing the evaluations indicated that they had some formal training in pediatric oncology, including a fellowship, clinical rotation, and/or workshops. Most of those who had some formal training were physicians (at 23.5% [12/51]), whereas only 1.8% were nurses (2/114; P ≤ .01). When asked if their clinical training program included a pediatric oncology component, 26.8% (64/239) confirmed that their training program had either clinical or didactic pediatric cancer components, with the most common group being physicians (63.8%, 30/47) when compared with nurses (15.8%, 16/101; P ≤ .01; Table 1).
Table 1.
Pediatric cancer training by profession
| Question | Nurses | Physicians | Others | Total | P Value |
|---|---|---|---|---|---|
| Formal training in pediatric oncology (fellowship, clinical rotations, workshops), yes (n = 272) | 2/114 (1.8%) | 12/51 (23.5%) | 6/107 (5.6%) | 20/272 (7.4%) | <.01 |
| Training included pediatric oncology component (clinical experience, formal lectures, readings), yes (n = 239) | 16/101 (15.8%) | 30/47 (63.8%) | 18/91 (19.8%) | 64/239 (26.8%) | <.01 |
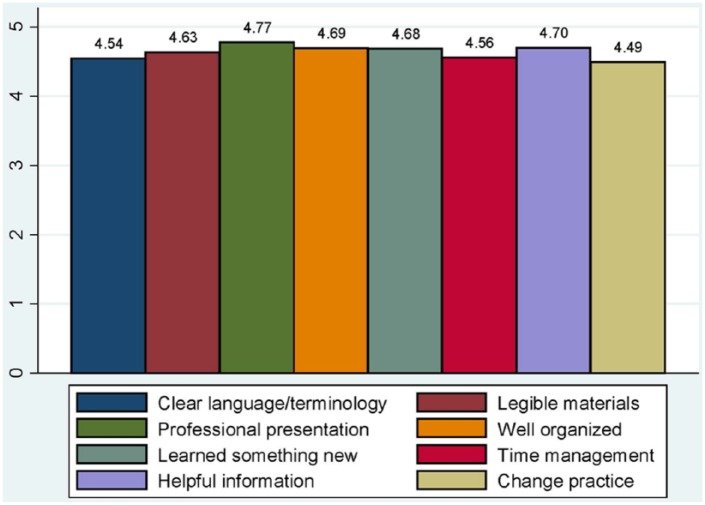
Before the workshop, the majority of attendees were not familiar with the worldwide incidence of pediatric cancer (42.0%, 107/255, answered correctly) or the survival percentage of pediatric cancer in an ideal setting (43.5%, 113/260, answered correctly). After the workshop, these percentages increased to 90.8% and 92.0%, respectively. When attendees were asked if they understood how to refer a child with suspected cancer to PMH, only 32.7% (84/257) answered positively (4-5 on a Likert scale of 1-5 where 1 = strongly disagree, 3 = neutral, 5 = strongly agree) prior to the seminar. Physicians were most aware of the process (at 54.9% 28/51) compared with nurses (25.9%, 28/108) and others/unidentified (28.6%, 28/98; P ≤ .01). After the workshop, 79.5% indicated that they understood how to refer a child with suspected cancer to PMH (Table 2). Attendees were asked to critically evaluate the workshop for clarity and content. On a 1 to 5 Likert scale, with 5 denoting strongly agree, all criteria had a mean of 4.49 or greater (Figure 2).
Table 2.
Pre- and post-test responses by profession
| Question | Pretest |
Posttest |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nurses | Physicians | Others | Total | P Value | Nurses | Physicians | Others | Total | P Value | |
| Incidence of pediatric cancer, correct response | 40/107 (37.4%) | 19/48 (39.6%) | 48/100 (48%) | 107/255 (42.0%) | .28 | 101/109 (92.7%) | 45/49 (91.8%) | 91/103 (88.4%) | 237/261 (90.8%) | .53 |
| Survival of pediatric cancer in ideal setting, correct response | 38/110 (34.6%) | 27/48 (56.3%) | 48/102 (47.1%) | 113/260 (43.5%) | .03 | 99/110 (90.0%) | 49/49 (100%) | 93/103 (90.3%) | 241/262 (92.0%) | .07 |
| Most common pediatric cancer, correct response | 72/102 (70.6%) | 43/49 (87.8%) | 87/102 (85.3%) | 202/253 (79.8%) | .01 | 104/111 (93.7%) | 49/49 (100%) | 100/108 (92.6%) | 253/268 (94.4%) | .16 |
| Most common solid tumor, correct response | 50/101 (49.5%) | 11/47 (23.4%) | 42/95 (44.2%) | 103/243 (42.4%) | .01 | 91/109 (83.5%) | 42/49 (85.7%) | 78/108 (72.2%) | 211/266 (79.3%) | .06 |
| Comfort managing a child with suspected cancer, positive response (4-5 on a 5-point scale) | 29/106 (27.4%) | 5/50 (10.0%) | 15/97 (15.5%) | 49/253 (19.4%) | .02 | 72/109 (66.1%) | 24/46 (52.2%) | 53/101 (52.5%) | 149/256 (58.2%) | .09 |
| Understanding the referral process of child with suspected cancer, positive response (4-5 on a 5-point scale) | 28/108 (25.9%) | 28/51 (54.9%) | 28/98 (28.6%) | 84/257 (32.7%) | <.01 | 84/107 (78.5%) | 41/46 (89.1%) | 76/100 (76%) | 201/253 (79.5%) | .18 |
Figure 2.
Evaluation of workshop by health care workers (mean scores on a 1-5 Likert scale where 1 = strongly disagree, 3 = neutral, 5 = strongly agree).
Discussion
In visiting 50% of government hospitals in Botswana, 362 health care workers were trained on how to recognize and refer children with suspected cancer to PMH, the only hospital in the country with pediatric oncology services. Assessment of attendees found that the majority of health care workers in Botswana had no prior training or clinical experience in pediatric oncology. Though treatment is available at PMH for children with cancer, recognition of suspected cancer and timely referral are essential to offer curative options for Batswana children.
Delayed presentation and diagnosis of pediatric cancer is a major issue in LMICs. The reasons for delay of diagnosis are multifactorial, including the malignancy type, patient/family demographics, and multiple factors within health care systems in LMICs.3-7 A South African study found that the median time of physician delay, the time from the child’s presentation to the health care system until diagnosis of cancer, was 20 days, contrasted with patient delay, the time lapse between onset of symptoms until the first health care encounter, which was 5 days.3 A Turkish study had similar results, with a median physician delay of 28 days versus 3 days for the patient/parent delay. This study also found that the physician delay was longer when the first patient contact was with a general practitioner instead of a pediatrician and even longer if the first contact physician was a nonpediatric specialist.6 Of the 109 workshop attendees in Botswana who identified as physicians, only 10 (9.2%) identified as a pediatrician.
Because of the late presentation of childhood cancers in South Africa, the Southern African Children’s Cancer Study Group (SACCSG) developed the Saint Siluan warning signs of childhood cancer.13 The warning signs were distributed throughout the Johannesburg area, with a catchment area population of 6 million, over a 6-month period, through lectures (610 attendees) and posters. Public awareness was also included through a multimedia campaign. Compared with the 12 years that preceded the awareness campaign, new referrals and new cancer diagnoses increased in the 6 years following the program from a mean of 78.4/year to 109.3/year.13 In Botswana, there are no organizations similar to the SACCSG. The pediatric hematology-oncology program at PMH has primarily relied on 1 BCM/TXCH pediatric hematologist-oncologist to serve the entire country, including a busy hematology service with the country’s only comprehensive hemophilia program for adults and children. Because of the addition of a second physician through the Baylor International Pediatric AIDS Initiative (BIPAI)/Texas Children’s Hospital Global Health Corps and a TXCH project manager/care coordinator based at PMH, the full-time pediatric hematologist-oncologist was able to engage in nationwide outreach for the first time since the program’s inception in 2007.14 With limited time and resources, more than 50% of government hospitals were reached, with 362 health care workers attending the training. The long-term impact on referral patterns and new cancer diagnoses remains to be seen, but the short-term impact can be seen in the respondents’ increased awareness of basic pediatric cancer knowledge and the services available at PMH for children with cancer.
Although this cancer recognition program met its goals, limitations of the program emerged that will inform future pediatric cancer education initiatives. Financial constraints are a routine limitation in LMICs. Expenses for this training program included travel costs for the physician, educational materials, and catering at some sites. The overall cost of the program was $4054.02 or $11.20 per health care worker trained. With limited full-time staffing in Botswana, it is not possible for the PMH oncologist to engage in prolonged educational initiatives while maintaining the quality of the clinical service. Future training models may involve intensively training representatives from hospitals and clinics throughout Botswana to serve as a local resource for their colleagues and as a direct link to the pediatric hematology-oncology service at PMH. TXCH is also currently developing a web-based didactic teaching model to include both physician and nurse education. With only 26.8% of attendees of the pediatric cancer recognition workshops indicating that their clinical training program had a pediatric oncology component, there is a tremendous need to incorporate pediatric cancer training into preservice training programs for physicians, nurses, and all health care workers in Botswana. Engaging the government and other stakeholders to promote pediatric cancer modules in training programs will be paramount.
There are many challenges to improving diagnosis and survival of pediatric cancer in LMICs. Even where programs exist to treat children with cancer, such as the program at PMH, successful treatment is dependent on children being appropriately recognized and urgently referred to advanced care by health care workers in the primary care setting. Despite significant deficiencies in human resources, a pediatric cancer recognition program was presented at half of all government/mission hospitals throughout Botswana. Sustained efforts are necessary to maximize the impact of such programs to lead to improved survival of pediatric cancer patients in LMICs.
Author Contribution
JSS contributed to the conception and design; contributed to acquisition, analysis, and interpretation of data; drafted the manuscript; critically revised the manuscript; gave final approval; and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
EI contributed to the conception and design; critically revised the manuscript; gave final approval; and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
PSM contributed to the conception and design; critically revised the manuscript; gave final approval; and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant through the Tapeats Fund.
References
- 1. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [DOI] [PubMed] [Google Scholar]
- 2. Ribeiro RC, Steliarova-Foucher E, Magrath I, et al. Baseline status of paediatric oncology care in ten low-income or mid-income countries receiving My Child Matters support: a descriptive study. Lancet Oncol. 2008;9:721-729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stefan DC, Siemonsma F. Delay and causes of delay in the diagnosis of childhood cancer in Africa. Pediatr Blood Cancer. 2011;56:80-85. [DOI] [PubMed] [Google Scholar]
- 4. Lins MM, Amorim M, Vilela P, et al. Delayed diagnosis of leukemia and association with morbid-mortality in children in Pernambuco, Brazil. J Pediatr Hematol/Oncol. 2012;34:e271-e276. [DOI] [PubMed] [Google Scholar]
- 5. Fajardo-Gutierrez A, Sandoval-Mex AM, Mejia-Arangure JM, Rendon-Macias ME, Martinez-Garcia Mdel C. Clinical and social factors that affect the time to diagnosis of Mexican children with cancer. Med Pediatr Oncol. 2002;39:25-31. [DOI] [PubMed] [Google Scholar]
- 6. Cecen E, Gunes D, Mutafoglu K, Sarialioglu F, Olgun N. The time to diagnosis in childhood lymphomas and other solid tumors. Pediatr Blood Cancer. 2011;57:392-397. [DOI] [PubMed] [Google Scholar]
- 7. Brown BJ, Adeleye AO, Ibeh JN. A prospective study on the causes of delayed diagnosis of childhood cancer in Ibadan, Nigeria. Pediatr Hematol/Oncol. 2015;32:365-373. [DOI] [PubMed] [Google Scholar]
- 8. Slone JS, Agrawal AK, Mehta PS, et al. Reply to “childhood cancer in Africa.” Pediatr Blood Cancer. 2014;61:1524. [DOI] [PubMed] [Google Scholar]
- 9. Kollar D, Hesselgrave J, Slone A, et al. Multidisciplinary Pediatric Oncology Training in Botswana. International Society of Paediatric Oncology; [Abstract P-207], Toronto, Canada: 2014. [Google Scholar]
- 10. Central Intelligence Agency. The World Factbook. Africa: Botswana. https://www.cia.gov/library/publications/the-world-factbook/geos/bc.html. Accessed August 17, 2015.
- 11. Workneh G, Scherzer L, Kirk B, et al. Evaluation of the effectiveness of an outreach clinical mentoring programme in support of paediatric HIV care scale-up in Botswana. AIDS Care. 2013;25:11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reid MJ, Haverkamp M, McAllister T, Miller J, Kirk BL. Airborne outreach: building HIV capacity and strengthening health care systems in rural Botswana. J Int Assoc Provid AIDS Care. 2014;13:106-109. [DOI] [PubMed] [Google Scholar]
- 13. Poyiadjis S, Wainwright L, Naidu G, Mackinnon D, Poole J. The Saint Siluan warning signs of cancer in children: impact of education in rural South Africa. Pediatr Blood Cancer. 2011;56:314-316. [DOI] [PubMed] [Google Scholar]
- 14. Slone JS, Slone AK, Mehta PS. Maximizing the impact of a pediatric hematology-oncology twinning program. Pediatr Blood Cancer. 2015;63:369. [DOI] [PubMed] [Google Scholar]