Abstract
BACKGROUND & AIMS
Serotonin (5-hydroxytryptamine [5-HT]) has an important role in gastrointestinal function. LX1031 is an oral, locally acting, small molecule inhibitor of tryptophan hydroxylase (TPH). Local inhibition of TPH in the gastrointestinal tract might reduce mucosal production of serotonin (5-HT) and be used to treat patients with nonconstipating irritable bowel syndrome (IBS).
METHODS
We evaluated 2 dose levels of LX1031 (250 mg or 1000 mg, given 4 times/day) in a 28-day, multicenter, randomized, double-blind, placebo-controlled study of 155 patients with nonconstipating IBS. 5-hydroxyindoleacetic acid (5-HIAA), a biomarker of pharmacodynamic activity, was measured in urine samples at baseline (24 hours after LX1031 administration), and at weeks 4 and 6 (n = 76).
RESULTS
Each dose of LX1031 was safe and well-tolerated. The primary efficacy end point, relief of IBS pain and discomfort, improved significantly in patients given 1000 mg LX1031 (25.5%), compared with those given placebo, at week 1 (P = .018); with nonsignificant improvements at weeks 2, 3, and 4 (17.9%, 16.3%, and 11.6%, respectively). Symptom improvement correlated with a dose-dependent reduction in 5-HIAA, a marker for TPH inhibition, from baseline until week 4. This suggests the efficacy of LX1031 is related to the extent of inhibition of 5-HT biosynthesis. Stool consistency significantly improved, compared with the group given placebo, at weeks 1 and 4 (P < .01) and at week 2 (P < .001).
CONCLUSIONS
In a phase 2 study, LX1031 was well tolerated, relieving symptoms and increasing stool consistency in patients with nonconstipating IBS. Symptom relief was associated with reduced levels of 5-HIAA in urine samples. This marker might be used to identify patients with nonconstipating IBS who respond to inhibitors of 5-HT synthesis.
Keywords: Clinical Trial, Drug, Constipation, Inflammation
Irritable bowel syndrome (IBS) is a highly prevalent functional bowel disorder that currently is not fully understood or adequately treated.1,2 The negative impact of IBS on quality of life is severe; moreover, IBS is associated with direct and indirect medical costs that are surprisingly large.3–6 IBS is defined as a symptom complex, which means that a clinical diagnosis of IBS may identify a population of patients with a heterogeneous underlying pathophysiology.7 The Rome III criteria were developed to standardize the diagnostic criteria for IBS and emphasize altered bowel habits with recurrent pain and/or discomfort.8 IBS may be associated predominantly with diarrhea (IBS-D), constipation, or a mixed pattern of each.9,10
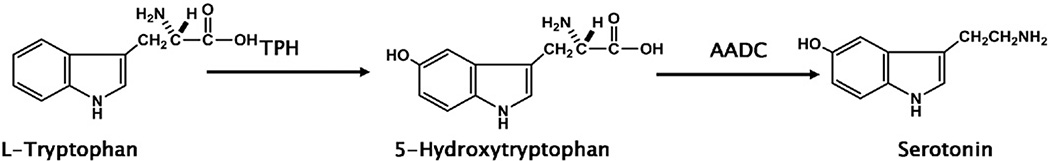
Gastrointestinal (GI) serotonin (5-hydroxytryptamine [5-HT]) may play an important role in the pathophysiology of nonconstipating IBS.2,11,12 Although 5-HT also is produced by neurons in the brain and in the pineal gland,13 the GI tract contains, by far, the largest depot of 5-HT in the body.14 This 5-HT is found both in mucosal enterochromaffin (EC) cells15 and in myenteric interneurons.11,16,17 The biosynthesis of 5-HT occurs in 2 steps: a rate-limiting enzyme, tryptophan hydroxylase (TPH), first converts L-tryptophan to 5-hydroxytryptophan, which then is converted to 5-HT by aromatic L-amino acid decarboxylase18 (Figure 1).
Figure 1.
Biosynthetic pathway of 5-HT production.
There are 2 isoforms of TPH, which are the products of separate genes, TPH1 and TPH2. TPH1 is found in EC cells, mast cells, and pinealocytes,19–21 whereas TPH2 is restricted to central and enteric neurons.16,22,23 The TPH1-dependent 5-HT of EC cells is released in response to a variety of signals, including increased intraluminal pressure and acid, which initiate peristaltic and secretory reflexes.24–27 Release of 5-HT from EC cells activates the mucosal projections of intrinsic primary afferent neurons, which in turn activate the microcircuits responsible for secretory as well as peristaltic reflexes.28–33 5-HT also stimulates extrinsic primary afferent neurons to convey noxious signals, including pain and nausea, to the central nervous system.34–38 Within the enteric nervous system, TPH2-dependent 5-HT is a neurotransmitter that mediates excitatory pathways regulating motility and secretion.11,12,39
Reports of gene polymorphisms abnormalities in EC cell number, 5-HT secretion, TPH1, serotonin transporter, and 5-HT receptors in subsets of patients with IBS suggest that abnormalities of 5-HT production, secretion, or action within the gut may have a role in the disordered motility and the discomfort characteristic of IBS.40–49 Drugs such as alosetron50,51 and cilansetron,52 which target 5-HT3 receptors, have been found to be effective in the treatment of IBS-D, whereas those that target 5-HT4 receptors are effective in the treatment of IBS-C.53–57 Although these compounds are not in wide use because of safety concerns,58 clinical benefit associated with treatment supports the concept that drugs that modify actions of 5-HT provide symptomatic relief for at least a subset of IBS patients. Given that 5-HT signaling is associated with increased GI activity, we developed LX1031, a locally acting inhibitor of TPH and 5-HT biosynthesis as a potential new therapy for nonconstipating IBS.59 This phase 2 study was designed to test the hypothesis that treatment with LX1031 would produce clinical improvements in symptoms of nonconstipating IBS and these improvements would be associated with a reduction in mucosal 5-HT production.
Materials and Methods
Study Design
This phase 2 clinical trial was conducted as a multicenter, randomized, double-blind, placebo-controlled, proof-of-concept study. Male and female patients 18 to 70 years of age with an established history of nonconstipating IBS (IBS-D and mixed-subtype IBS) based on ROME III criteria were recruited across 36 centers in the United States. Diagnostic criteria for nonconstipating IBS included symptom onset 6 months or more before study enrollment, with presence of abdominal pain or discomfort in the 3 months before enrollment. All patients were required to have a normal colonoscopy. In addition, patients were required to have no history of alarm signs or symptoms including fever, GI bleeding, weight loss, anemia, or abdominal mass. With the exception of bulking agents, medications used in the management of nonconstipating IBS symptoms (eg, antidiarrheal agents such as loperamide, diphenoxylate, bismuth subsalicylate, paregoric and anticholinergic antidepressants, opioid analgesic drugs, or other drugs that specifically affect bowel motility [prescription, over-the-counter, or herbal]), were to be discontinued 30 days before enrollment. There were no dietary restrictions during the study period. Patients who had received any investigational agent within 3 months of the start of the study also were excluded. The institutional review board at each participating center approved the research and all patients who participated in the study provided written informed consent. This study was registered with ClinicalTrials.gov (NCT00813098).
The clinical trial consisted of 4 study periods: screening, a 14-day run-in, a 28-day treatment, and a 14-day follow-up. During run-in, patients were required to complete daily diary records (10 of 14 days) to establish the extent of their baseline symptoms. Patients meeting the appropriate inclusion criteria were assigned randomly in a double-blind fashion to 1 of 2 doses of LX1031 (250 mg 4 times/day or 1000 mg 4 times/day) or placebo, taken daily during the 28-day treatment period; randomization was conducted centrally in blocks of 3. Separate written informed consent was obtained from patients willing to participate in evaluation of biomarkers directly associated with LX1031 mechanism of action: 24-hour urinary 5-hydroxyindoleacetic acid (5-HIAA) and whole-blood 5-HT. Urinary 5-HIAA samples were obtained at baseline and week 4 of the treatment period, and at the 2-week follow-up visit. Three samples of whole blood for assessment of 5-HT were obtained on the same days, with 1 sample being obtained while the patient was fasting and 2 samples postprandially, at 0.5 and 2.0 hours after a standardized, carbohydrate-rich meal.
Study Outcomes
Study outcomes were evaluated through the use of daily reporting into an interactive voice response system (IVRS), and visual analog scales (VAS). The prespecified primary efficacy end point was impact on global subjective assessment of pain and discomfort across the 4-week study treatment period (adequate relief assessment) based on a weekly response to the question, “In the past 7 days, have you had adequate relief of your IBS pain and discomfort?” In addition, secondary efficacy end point assessments included the following: IBS global assessment of improvement scale (7-point scale), urgency to defecate, Bristol Stool Form Scale (7-point scale), stool frequency, abdominal pain (4-point scale and VAS), and bloating (4-point scale and VAS).
Safety was evaluated weekly through a symptom-oriented physical examination, vital signs, review of concomitant medication(s), adverse event (AE) reports, hematology, and blood chemistry. In addition, electrocardiograms (ECGs) were obtained at baseline, at week 4 of the treatment period, and at completion of the week 2 follow-up period.
Statistical Analysis
Sample size calculations and power ranking equivalents were modeled using estimates of response rates, variability of study assessments, and differences between treatment and placebo arms with various placebo response rates. Based on simulated trial modeling estimates, in the presence of a 20% treatment difference, the probability of observing a greater than 0.05 difference (response rate to active drug minus response rate to placebo) approximated 90% with 45–50 subjects per arm.
Data were analyzed using descriptive summaries of the absolute and change from baseline for mean scores by week. The change from baseline in mean scores for each week was fitted using an analysis of covariance model, with baseline as the covariate. The safety analysis was conducted using the safety population, comprised of all patients who received at least 1 dose (or any portion thereof) of study drug or placebo; a predefined, per-protocol population was used in the analysis of efficacy variables. This population was required to be 80% or more compliant with the study medication, answer 75% or more of the IVRS questions concerning global subjective relief, and complete the study. Biochemical variables were summarized by measures of central tendency and the corresponding measures of variance. Relationships between biochemical markers and efficacy end points were evaluated using logistic regression models.
Results
Study Population
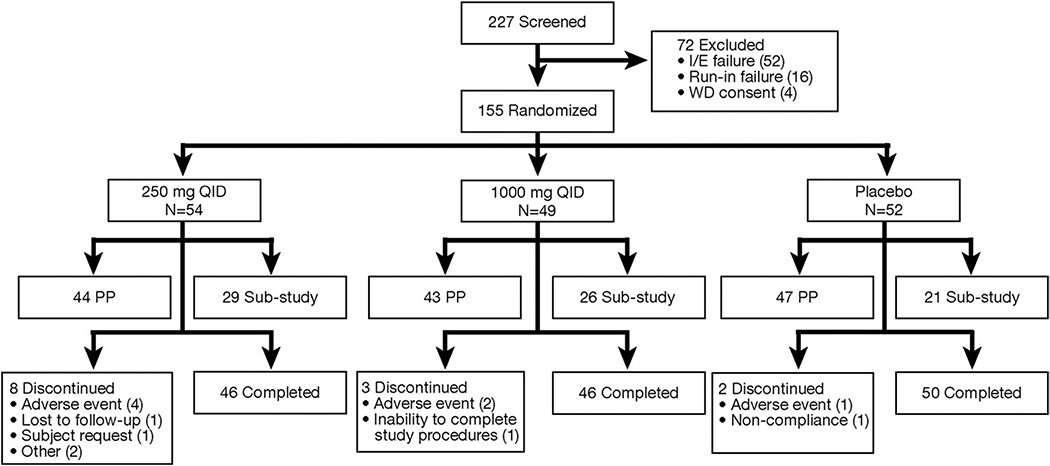
Between December 2008 and September 2009 a total of 227 patients were screened for inclusion in the protocol; 155 met enrollment criteria and were randomized to study medication. Of these, 142 completed the study with 134 meeting the predefined requirements for inclusion in the per-protocol population (Figure 2). All sites were given the opportunity to participate in the biomarker substudy; 76 patients at 19 of 34 sites participated. Patients enrolled in the biomarker substudy were demographically representative of the total patient population. The baseline characteristics of the 155 patients randomly assigned to the study groups are summarized in Table 1. Demographic variables between treatment and placebo groups were well balanced.
Figure 2.
Study disposition. QID, 4 times/day.
Table 1.
Baseline Characteristics of the Study Population
| Variable | Placebo (n = 52) | LX1031 250 mg QID (n = 54) | LX1031 1000 mg QID (n = 49) |
|---|---|---|---|
| Mean age ± SD, y | 48.0 ± 12.43 | 47.5 ± 12.93 | 48.7 ± 11.96 |
| Sex, n (%) | |||
| Male | 8 (15.4) | 8 (14.8) | 9 (18.4) |
| Female | 44 (84.6) | 46 (85.2) | 40 (81.6) |
| Race, n (%) | |||
| White | 47 (90.4) | 49 (90.7) | 43 (87.8) |
| Black | 2 (3.8) | 4 (7.4) | 6 (12.2) |
| Asian | 1 (1.9) | 0 (0) | 0 (0) |
| Other | 2 (3.8) | 1 (1.9) | 0 (0) |
| IBS type, n (%) | |||
| IBS-D | 37 (71.2) | 42 (77.8) | 39 (79.6) |
| Mixed-type IBS | 15 (28.8) | 12 (22.2) | 10 (20.4) |
| (n = 47) | (n = 44) | (n = 43)a | |
| Mean disease severity scores | |||
| Bloat VAS | 49.16 | 45.58 | 48.15 |
| Bloat 4-point scale | 1.82 | 1.67 | 1.74 |
| Pain VAS | 50.21 | 47.62 | 47.42 |
| Pain 4-point scale | 1.84 | 1.78 | 1.73 |
| Frequency | 2.92 | 3.35 | 3.3 |
| Urgency | 0.79 | 0.82 | 0.84 |
| Stool Form VAS | 4.24 | 4.09 | 4.26 |
QID, 4 times/day; VAS, visual analog scale.
n = 42 for bloat VAS and pain VAS.
Efficacy Outcomes
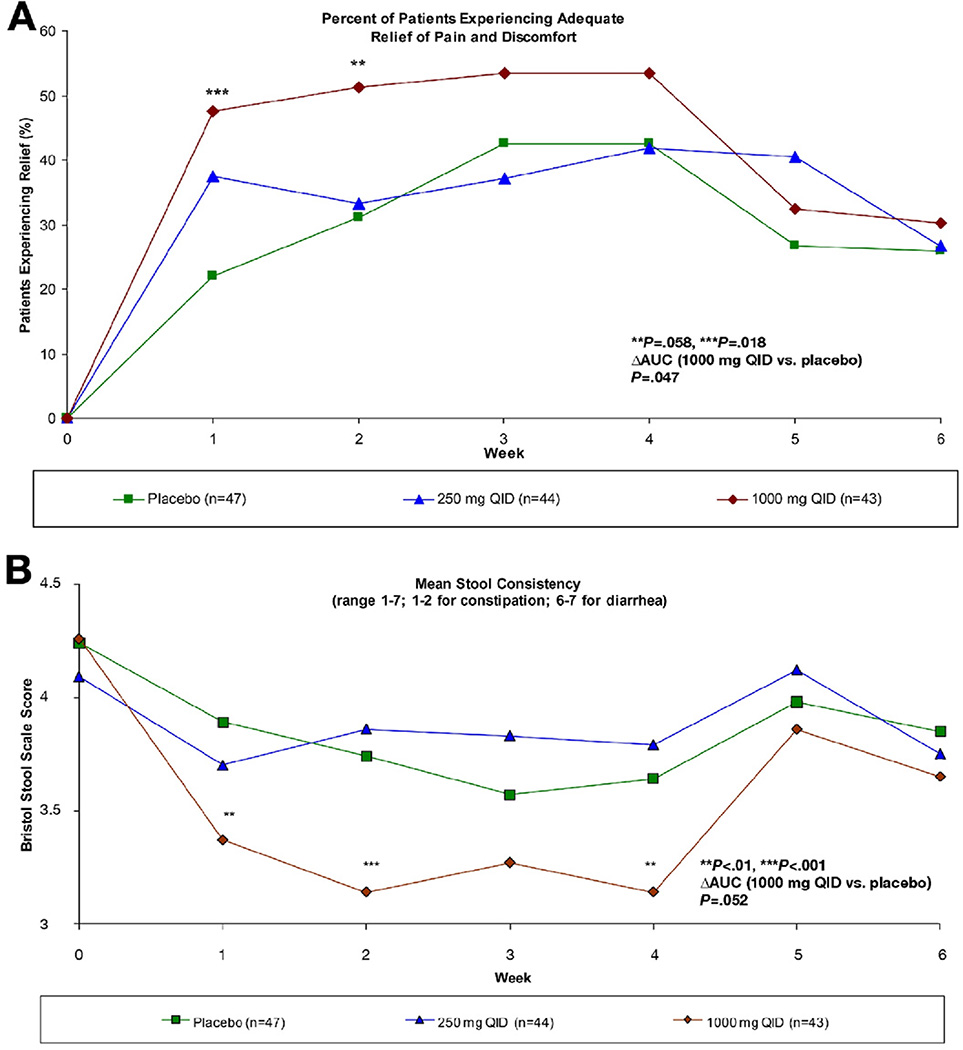
Evaluating the prespecified primary efficacy end point of global subjective adequate relief outcome, a statistically significant improvement of 25.5% was observed in the high-dose (HD) LX1031 group over placebo at week 1 (47.5% vs 22.0%; P = .018) with nonsignificant improvements of 17.9%, 16.3%, and 11.6% over placebo observed for weeks 2, 3, and 4, respectively (Figure 3A, and Table 2). Over time, patients receiving the placebo showed an improved response, reaching levels similar to that seen in the low-dose (LD) LX1031 arm. Stool consistency, a secondary end point measured by the Bristol Stool Form Scale, improved in the HD arm at weeks 1, 2, and 4 vs placebo (P < .01 weeks 1 and 4, P < .001 week 2) (Figure 3B, Table 2). In an effort to determine whether patients experienced a benefit as compared with placebo over the entire 4-week treatment period as a whole, a nonprespecified analysis of area under the curve was conducted that revealed that the HD group experienced a significant improvement (P = .047) in adequate relief from nonconstipating IBS pain and discomfort. After discontinuation of therapy, improvement observed in both adequate relief and stool consistency based on the daily Bristol Stool Form Scale disappeared rapidly, such that by 1 week after drug discontinuation, values were similar across both dose groups and placebo. There were no significant differences between the treatment groups and the placebo group for the other prespecified secondary efficacy variables at any time during the study.
Figure 3.
(A) Percentage of patients experiencing adequate relief on a weekly basis. (B) Weekly mean scores of daily Bristol Stool Form Scale (range, 1–7; 1–2 for constipation; 6–7 for diarrhea). ΔAUC, change in area under the curve; QID, 4 times/day.
Table 2.
Efficacy End Points
| Adequate relief of IBS pain and discomfort, % | Placebo (n = 47) | LX1031 250 mg QID (n = 44) | LX1031 1000 mg QID (n = 43) |
|---|---|---|---|
| Patients achieving adequate relief (primary efficacy end point), % |
|||
| Treatment week 1 | 22.0 | 37.5 | 47.5a |
| Treatment week 2 | 31.1 | 33.3 | 51.2 |
| Treatment week 3 | 42.6 | 37.2 | 53.5 |
| Treatment week 4 | 42.6 | 41.9 | 53.5 |
| Follow-up week 1 | 26.8 | 40.5 | 32.5 |
| Follow-up week 2 | 25.8 | 26.7 | 30.3 |
| Weekly mean scores of Daily Bristol Stool Form scale (±SD) |
|||
| Baseline | 4.24 (±1.05) | 4.09 (±0.99) | 4.26 (±1.039) |
| Treatment week 1 | 3.89 (±1.006) | 3.70 (±1.010) | 3.37b (±1.257) |
| Treatment week 2 | 3.74 (±0.972) | 3.86 (±1.005) | 3.14b (±1.338) |
| Treatment week 3 | 3.57 (±1.114) | 3.83 (±0.916) | 3.27 (±1.211) |
| Treatment week 4 | 3.64 (±1.118) | 3.79 (±0.915) | 3.14b (±1.04) |
| Follow-up week 1 | 3.98 (±1.232) | 4.12 (±0.837) | 3.86 (±1.170) |
| Follow-up week 2 | 3.85 (±1.185) | 3.75 (±1.061) | 3.65 (±1.098) |
| Biochemical evaluation of efficacy | |||
| (n = 21) | (n = 29) | (n = 26) | |
| Median 24-hour urinary 5-HIAA (mg/24 h) | |||
| Baseline | 3.35 | 3.20 | 2.80 |
| Treatment week 4 | 3.20 | 2.65 | 2.10 |
| Follow-up week 2 | 3.40 | 3.15 | 2.40 |
| Change (baseline vs week 4) | −4.48% | −17.19% | −25.00% |
QID, 4 times/day; SD, standard deviation.
P ≤ .05 vs placebo.
P ≤ .01 vs placebo.
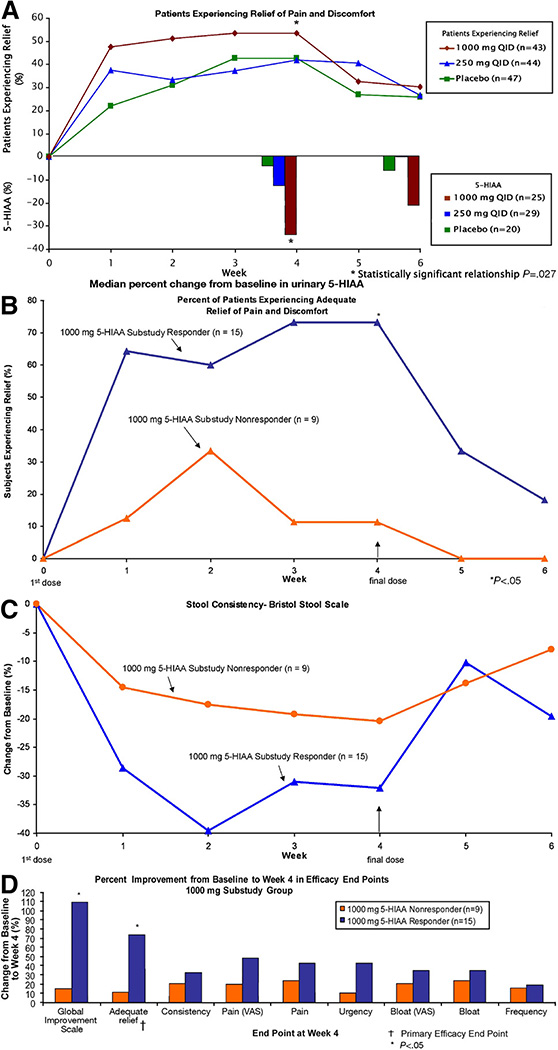
For patients who consented to participate in the biomarker substudy, a statistically significant relationship in the HD group was observed between the percentage decrease of urinary 5-HIAA and the improvement in the global subjective adequate relief from baseline to week 4 (P = .027, using the Wald statistic from logistic regression) (Figure 4A). Overall, a 25% change in median urinary 5-HIAA was observed after 4 weeks of treatment between the HD and placebo groups. A more modest reduction occurred in the LD group and minimal changes were seen in the placebo group (Table 2). No significant changes in whole-blood 5-HT were observed, which may be attributed to the limited turnover of platelets, a reservoir of 5-HT, during the 4-week treatment period.
Figure 4.
(A) Relationship between improvement in adequate relief and decline in 24-hour urinary 5-HIAA. (B) HD urinary 5-HIAA biomarker responders vs nonresponders achieving adequate relief on a weekly basis. (C) HD urinary 5-HIAA biomarker responders vs nonresponders Bristol Stool Form scale effects. (D) HD urinary 5-HIAA biomarker responders vs nonresponders across all efficacy outcomes. QID, 4 times/day.
Relationship of Clinical Improvement to Biochemical Markers of TPH Inhibition
To explore the potential use of the biomarker to distinguish those patients most responsive to LX1031 treatment, a retrospective analysis of those individuals who participated in the urinary 5-HIAA biomarker substudy was performed. Because the LD and placebo groups were not significantly distinguished with respect to the primary end point by week 4, treated patients were stratified based on urinary 5-HIAA: less than 15% reduction or 15% or greater reduction (a level that distinguished the HD group from both the placebo and LD groups). For the 24 individuals randomly assigned to HD LX1031 who participated in the substudy, 15 (63%) achieved a 15% or greater reduction in urinary 5-HIAA (5-HIAA biomarker responders), compared with 9 patients (37%) with a 5-HIAA reduction of less than 15% (5-HIAA biomarker nonresponders). Notably, 73% of patients in the HD 5-HIAA biomarker responder group reported achieving adequate relief of nonconstipating IBS pain and discomfort at week 4, whereas only 11% of the HD 5-HIAA biomarker nonresponders did so (P = .011; Figure 4B). The HD 5-HIAA biomarker responder group also experienced significantly greater improvements in stool consistency than did those in the HD group who did not reduce their 5-HIAA to a similar extent (Figure 4C).
Although there were no significant differences in the secondary efficacy assessments in the per-protocol population, the HD 5-HIAA biomarker responder group showed improvement in global measures and a number of additional GI symptoms (Figure 4D). By using the IBS global assessment of improvement 7-point scale, an overall subjective symptom improvement was observed compared with baseline (P = .026), whereas no differences had been observed in the per-protocol population with this instrument.
Adverse Effects
AEs reported were generally mild, self-limited, and evenly distributed across the placebo and both LX1031 treatment arms. In addition, there was no evidence of a dose response with respect to AEs. Thirteen patients discontinued therapy over the 4-week treatment period. Of these, 7 discontinued because of an AE (placebo, n = 1; 250 mg 4 times/day, n = 4; and 1000 mg 4 times/day, n = 2), including: insomnia, urinary tract infection, supraventricular tachycardia (pre-existing condition), gagging at pill ingestion, worsening of nonconstipating IBS symptoms, rash, and the only serious AE that was reported (transient ischemic attack unrelated to study drug). The remaining 6 discontinuations were due to the following: lost to follow-up evaluation (n = 1), withdrawn consent (n = 2), lack of compliance (n = 1), withdrawn by the principal investigator (n = 1), or inability to complete study procedures (n = 1). There were no clinically significant abnormalities observed in laboratory parameters, ECGs, or physical examinations. The most frequent AEs affected the GI system, as might be expected within this patient population (Table 3). Among the 5 patients with diarrhea in the HD group, most events were mild to moderate, fewer than 3 days in duration, and resolved without additional intervention. In addition, there was no temporal relationship to initiation of study drug dosing with the occurrence of these events. None of the patients who experienced events of diarrhea participated in the biomarker substudy.
Table 3.
Adverse Events
| Preferred term | Placebo (n = 52) n (%) | LX1031 250 mg QID (n = 54) n (%) | LX1031 1000 mg QID (n = 49) n (%) |
|---|---|---|---|
| Nausea | 4 (7.7) | 5 (9.3) | 4 (8.2) |
| Diarrhea | 2 (3.8) | 1 (1.9) | 5 (10.2) |
| Dyspepsia | 2 (3.8) | 3 (5.6) | 0 |
| Vomiting | 0 | 2 (3.7) | 2 (4.1) |
| Headache | 2 (3.8) | 3 (5.6) | 3 (6.1) |
| Somnolence | 1 (1.9) | 2 (3.7) | 1 (2.0) |
| Dizziness | 0 | 2 (3.7) | 0 |
| Dysgeusia | 0 | 2 (3.7) | 0 |
| Urinary tract infection | 1 (1.9) | 0 | 2 (4.1) |
| Blood amylase level increased | 0 | 2 (3.7) | 0 |
| White blood cell increased | 0 | 2 (3.7) | 0 |
| Back pain | 2 (3.8) | 0 | 2 (4.1) |
NOTE. AEs occurring in more than 1 patient at a rate greater than placebo by preferred term.
QID, 4 times/day
Discussion
LX1031 was developed as an oral TPH inhibitor that acts locally on the GI mucosa, gaining access primarily to TPH in the intestinal lining and thereby inhibiting 5-HT synthesis in the GI epithelium. The favorable safety profile observed in this study may be related, in part, to its local site of action in the GI tract, ability to inhibit 5-HT synthesis at the level of the EC cell, and low degree of oral bioavailability and systemic exposure. This exploratory phase 2 study shows that LX1031 may be effective in improving symptoms in patients with nonconstipating IBS with a significant number of patients reporting that they had experienced adequate symptom relief during the first week of therapy. Significant improvements also were observed in stool consistency at weeks 1, 2, and 4. These observations support the concept that nonconstipating IBS symptoms may be improved by inhibiting TPH.
Biomarker findings from this study are consistent with the idea that mucosal 5-HT dysregulation may influence nonconstipating IBS symptoms in a subset of patients. Indeed, the use of LX1031 also provides a pharmacologic probe that can further our understanding of the etiology of nonconstipating IBS by allowing the relationship between the change in a biomarker that reflects 5-HT biosynthesis (urinary 5-HIAA) and symptoms to be examined. The 5-HIAA biomarker also supports the linkage of clinical efficacy to the mechanism of action of LX1031: inhibition of TPH and reduction of serotonin synthesis. LX1031 has been shown consistently to reduce mucosal 5-HT production in preclinical models,59 in a phase 1 study of normal volunteers,60 and now in a phase 2 study of nonconstipating IBS patients.
Because EC cells contain the bulk of the 5-HT in the body, urinary measurements of 5-HIAA largely reflect the metabolism of GI mucosal 5-HT. If 5-HT release from EC cells or 5-HT hypersensitivity were to contribute to the etiology of nonconstipating IBS, then LX1031 would be expected to provide symptom relief to those patients who respond biochemically to LX1031, as shown by a decrease in urinary 5-HIAA. Conversely, patients who do not have a decrease in urinary 5-HIAA would be unlikely to show clinical improvement in response to therapy. The observation in this study, that relief of symptoms was associated with a decrease in urinary 5-HIAA, is consistent with these predictions.
The investigation of new drugs for the treatment of nonconstipating IBS is challenging because of a combination of factors including the heterogeneity of the patient population and variability in both subjective assessments and pharmacologic response. As such, there are inevitable and recognized limitations specific to the current study: (1) limited baseline disease severity data and IBS treatment history, (2) variability associated with treatment of patients with both mixed-subtype IBS and IBS-D; (3) limited sample size, duration of treatment, and follow-up periods, and (4) a high placebo effect (although not atypical for such trials).
Certain dimensions of nonconstipating IBS drug development and patient management could be improved through access to an objective biomarker that correlates with clinical response and pharmacologic action. The retrospective observation in this study that patients manifesting a reduction in urinary 5-HIAA excretion of 15% or more showed improvement in multiple efficacy parameters (Figure 4C) suggests that it may be possible to prospectively identify patients who are most likely to benefit from therapies designed to reduce serotonin synthesis in the GI tract. For example, it may be possible to use the biochemical response to LX1031, as measured by the reduction of urinary 5-HIAA over an initial dosing period, to identify those patients who are most likely to benefit from longer-term treatment. Therapy also could be individualized with respect to dose, based on the level of biomarker response to initial treatment followed by dose titration until a desired pharmacologic threshold effect is achieved in order to maximize the potential for clinical benefit. Although significant variability was observed in the biomarker parameters in this study, which in part may relate to differences in diet for foods rich in tryptophan, a dose-dependent effect was observed in the reduction of 24-hour urinary 5-HIAA. The lack of response to the compound in some patients may be due to increased GI transit time (limiting drug access to EC cells) or other factors limiting effective exposure of the compound to the epithelial surface of the GI tract. For such patients, a response might be obtained at higher doses of LX1031, or with an alternative compound or formulation with improved access to the mucosal epithelium.
Conclusions
LX1031, a locally acting TPH inhibitor, appeared safe and well tolerated in this exploratory phase 2 study over 4 weeks in patients with symptomatic, nonconstipating IBS. Results suggest that reduction of mucosally derived 5-HT may positively influence symptoms common to nonconstipating IBS. Importantly, a relationship was observed between improvement in symptoms and a reduction in 24-hour urinary 5-HIAA, a biomarker that corresponds to the rate of 5-HT synthesis and the mechanism of action of LX1031. The use of this biomarker may allow for identification of the subset of patients who have the best chance of experiencing an improvement in their nonconstipating IBS symptoms through therapy with a TPH inhibitor. Further studies with TPH inhibitors will be required to confirm these initial clinical findings and the related hypothesis that reduction of GI mucosal 5-HT correlates with symptom improvement in patients with nonconstipating IBS.
Acknowledgments
The authors thank Kristi A. Boehm, MS, from Lexicon Pharmaceuticals, Inc, for writing assistance.
Funding
Lexicon Pharmaceuticals, Inc, and Symphony Icon provided the funding for the LX1031 clinical studies. The statistical analysis of the entire data sets pertaining to efficacy (specifically primary and major secondary efficacy end points) and safety (specifically, serious adverse events as defined in federal guidelines) have been confirmed independently by a biostatistician who is not employed by the corporate entity.
The corresponding author had full access to all of the data and takes full responsibility for the veracity of the data and analysis.
Abbreviations used in this paper
- 5-HT
5-hydroxytryptamine, serotonin
- 5-HIAA
5-hydroxyindoleacetic acid
- AADC
aromatic L-amino acid decarboxylase
- AE
adverse event
- EC
enterochromaffin
- GI
gastrointestinal
- HD
high-dose
- IBS
irritable bowel syndrome
- IBS-D
irritable bowel syndrome-diarrhea predominate
- TPH
tryptophan hydroxylase
- TPH1
tryptophan hydroxylase type 1
- TPH2
tryptophan hydroxylase type 2.
Footnotes
Conflicts of interest
These authors disclose the following: Phil Brown was an employee and is a stockholder of Lexicon Pharmaceuticals, Inc. Doug Drossman is a consultant to Prometheus, Lexicon, Takeda, and Astra Zeneca. Alastair Wood is a partner, investor, and shareholder in Symphony Capital, LLC. Gary Cline is an independent contractor with the Department of Biostatistics at Icon Clinical Research and provided statistical analysis of the clinical data discussed in this article. Kenny Frazier, Jessica Jackson, Johanna Bronner, Joel Freiman, Brian Zambrowicz, and Arthur Sands are employees and stockholders of Lexicon Pharmaceuticals, Inc. Michael Gershon is a consultant to Lexicon Pharmaceuticals, Inc.
References
- 1.Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health-care practitioners. J Gastroenterol Hepatol. 2010;25:691–699. doi: 10.1111/j.1440-1746.2009.06120.x. [DOI] [PubMed] [Google Scholar]
- 2.Camilleri M. Evolving concepts of the pathogenesis of irritable bowel syndrome: to treat the brain or the gut? J Pediatr Gastroenterol Nutr. 2009;48(Suppl 2):S46–S48. doi: 10.1097/MPG.0b013e3181a1174b. [DOI] [PubMed] [Google Scholar]
- 3.Spiegel BM. The burden of IBS: looking at metrics. Curr Gastroenterol Rep. 2009;11:265–269. doi: 10.1007/s11894-009-0039-x. [DOI] [PubMed] [Google Scholar]
- 4.Maxion-Bergemann S, Thielecke F, Abel F, et al. Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics. 2006;24:21–37. doi: 10.2165/00019053-200624010-00002. [DOI] [PubMed] [Google Scholar]
- 5.Ten Berg MJ, Goettsch WG, van den Boom G, et al. Quality of life of subjects with irritable bowel syndrome is low compared to others with chronic diseases. Eur J Gastroenterol Hepatol. 2006;18:475–481. doi: 10.1097/00042737-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Drossman DA, Morris CB, Schneck S, et al. International survey of patients with IBS: symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol. 2009;43:541–550. doi: 10.1097/MCG.0b013e318189a7f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corazziari E, Delvaux M, Drossman DA. The functional gastrointestinal disorders and the Rome III process. In: Drossman DA, et al., editors. Rome III: the functional gastrointestinal disorders. 3rd. McLean, VA: Degnon Associates, Inc; 2006. pp. 1–29. [Google Scholar]
- 8.Drossman DA. Introduction. The Rome foundation and Rome III. Neurogastroenterol Motil. 2007;19:783–786. doi: 10.1111/j.1365-2982.2007.01001.x. [DOI] [PubMed] [Google Scholar]
- 9.Dorn SD, Morris CB, Hu Y, et al. Irritable bowel syndrome subtypes defined by Rome II and Rome III criteria are similar. J Clin Gastroenterol. 2009;43:214–220. doi: 10.1097/MCG.0b013e31815bd749. [DOI] [PubMed] [Google Scholar]
- 10.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 11.Gershon MD, Tack J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology. 2007;132:397–414. doi: 10.1053/j.gastro.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Galligan JJ, Parkman H. Recent advances in understanding the role of serotonin in gastrointestinal motility and functional bowel disorders. Neurogastroenterol Motil. 2007;19(Suppl 2):1–4. doi: 10.1111/j.1365-2982.2007.00970.x. [DOI] [PubMed] [Google Scholar]
- 13.Hasegawa H, Kobayashi T, Inoue F, et al. Intracellular metabolism of biogenic amines in paraneurons. Arch Histol Cytol. 1989;52:69–74. doi: 10.1679/aohc.52.suppl_69. [DOI] [PubMed] [Google Scholar]
- 14.Erspamer V. Occurrence of indolealkylamines in nature. In: Erspamer V, editor. Handbook of experimental pharmacology: 5-hydroxytryptamine and related indolealkylamines. Vol. 19. New York: Springer-Verlag; 1966. pp. 132–181. [Google Scholar]
- 15.Vialli M. Histology of the enterochromaffin cell system. In: Erspamer V, editor. Handbook of experimental pharmacology: 5-hydroxytryptamine and related indolealkylamines. Vol. 19. New York: Springer-Verlag; 1966. pp. 1–65. [Google Scholar]
- 16.Gershon MD. Enteric serotonergic neurones…finally! J Physiol. 2009;587:507. doi: 10.1113/jphysiol.2008.167676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neal KB, Parry LJ, Bornstein JC. Strain-specific genetics, anatomy and function of enteric neural serotonergic pathways in inbred mice. J Physiol. 2009;587:567–586. doi: 10.1113/jphysiol.2008.160416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koe BK, Weissman A. p-Chlorophenylalanine: a specific depletor of brain serotonin. J Pharmacol Exp Ther. 1966;154:499–516. [PubMed] [Google Scholar]
- 19.Cote F, Thevenot E, Fligny C, et al. Disruption of the nonneuronal tph1 gene demonstrates the importance of peripheral serotonin in cardiac function. Proc Natl Acad Sci U S A. 2003;100:13525–13530. doi: 10.1073/pnas.2233056100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cote F, Fligny C, Bayard E, et al. Maternal serotonin is crucial for murine embryonic development. Proc Natl Acad Sci U S A. 2007;104:329–334. doi: 10.1073/pnas.0606722104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walther DJ, Peter JU, Bashammakh S, et al. Synthesis of serotonin by a second tryptophan hydroxylase isoform. Science. 2003;299:76. doi: 10.1126/science.1078197. [DOI] [PubMed] [Google Scholar]
- 22.Gutknecht L, Waider J, Kraft S, et al. Deficiency of brain 5-HT synthesis but serotonergic neuron formation in Tph2 knockout mice. J Neural Transm. 2008;115:1127–1132. doi: 10.1007/s00702-008-0096-6. [DOI] [PubMed] [Google Scholar]
- 23.Gutknecht L, Kriegebaum C, Waider J, et al. Spatio-temporal expression of tryptophan hydroxylase isoforms in murine and human brain: convergent data from Tph2 knockout mice. Eur Neuropsychopharmacol. 2009;19:266–282. doi: 10.1016/j.euroneuro.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Bülbring E, Crema A. The action of 5-hydroxytryptamine, 5-hydroxytryptophan and reserpine on intestinal peristalsis in anaesthetized guinea-pigs. J Physiol (Lond) 1959;146:29–53. doi: 10.1113/jphysiol.1959.sp006176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bülbring E, Crema A. The release of 5-hydroxytryptamine in relation to pressure exerted on the intestinal mucosa. J Physiol (Lond) 1959;146:18–28. doi: 10.1113/jphysiol.1959.sp006175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bülbring E, Lin RCY, Schofield G. An investigation of the peristaltic reflex in relation to anatomical observations. Q J Exp Physiol. 1958;43:26–37. doi: 10.1113/expphysiol.1958.sp001305. [DOI] [PubMed] [Google Scholar]
- 27.Bülbring E, Lin RCY. The effect of intraluminal application of 5-hydroxytryptamine and 5-hydroxytryptophan on peristalsis, the local production of 5-hydroxytryptamine and its release in relation to intraluminal pressure and propulsive activity. J Physiol (Lond) 1958;140:381–407. [PMC free article] [PubMed] [Google Scholar]
- 28.Pan H, Gershon MD. Activation of intrinsic afferent pathways in submucosal ganglia of the guinea pig small intestine. J Neurosci. 2000;20:3295–3309. doi: 10.1523/JNEUROSCI.20-09-03295.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bertrand PP, Hu X, Mach J, et al. Serotonin (5-HT) release and uptake measured by real-time electrochemical techniques in the rat ileum. Am J Physiol Gastrointest Liver Physiol. 2008;295:G1228–G1236. doi: 10.1152/ajpgi.90375.2008. [DOI] [PubMed] [Google Scholar]
- 30.Bertrand PP. Real-time detection of serotonin release from enterochromaffin cells of the guinea-pig ileum. Neurogastroenterol Motil. 2004;16:511–514. doi: 10.1111/j.1365-2982.2004.00572.x. [DOI] [PubMed] [Google Scholar]
- 31.Bertrand PP, Kunze WAA, Furness JB, et al. The terminals of myenteric intrinsic primary afferent neurons of the guinea pig ileum are excited by 5-HT acting at 5-HT3 receptors. Neuroscience. 2000;101:459–469. doi: 10.1016/s0306-4522(00)00363-8. [DOI] [PubMed] [Google Scholar]
- 32.Patel BA, Bian X, Quaiserova-Mocko V, et al. In vitro continuous amperometric monitoring of 5-hydroxytryptamine release from enterochromaffin cells of the guinea pig ileum. Analyst. 2007;132:41–47. doi: 10.1039/b611920d. [DOI] [PubMed] [Google Scholar]
- 33.Bian X, Patel B, Dai X, et al. High mucosal serotonin availability in neonatal guinea pig ileum is associated with low serotonin transporter expression. Gastroenterology. 2007;132:2438–2447. doi: 10.1053/j.gastro.2007.03.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lang IM. Noxious stimulation of emesis. Dig Dis Sci. 1999;44:58S–63S. [PubMed] [Google Scholar]
- 35.Hillsley K, Kirkup AJ, Grundy D. Direct and indirect actions of 5-hydroxytryptamine on the discharge of mesenteric afferent fibers innervating the rat jejunum. J Physiol (Lond) 1998;506:551–561. doi: 10.1111/j.1469-7793.1998.551bw.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hillsley K, Grundy D. Sensitivity to 5-hydroxytryptamine in different afferent subpopulations within mesenteric nerves supplying the rat jejunum. J Physiol (Lond) 1998;509:717–727. doi: 10.1111/j.1469-7793.1998.717bm.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grundy D, Blackshaw LA, Hillsley K. Role of 5-hydroxytryptamine in gastrointestinal chemosensitivity. Dig Dis Sci. 1994;39(Suppl):44S–47S. doi: 10.1007/BF02300369. [DOI] [PubMed] [Google Scholar]
- 38.Blackshaw LA, Grundy D. Effects of 5-hydroxytryptamine on discharge of vagal mucosal afferent fibres from the upper gastrointestinal tract of the ferret. J Auton Nerv Syst. 1993;45:41–50. doi: 10.1016/0165-1838(93)90360-7. [DOI] [PubMed] [Google Scholar]
- 39.Neal KB, Bornstein JC. Mapping 5-HT inputs to enteric neurons of the guinea-pig small intestine. Neuroscience. 2007;145:556–575. doi: 10.1016/j.neuroscience.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 40.Spiller R, Garsed K. Infection, inflammation, and the irritable bowel syndrome. Dig Liver Dis. 2009;41:844–849. doi: 10.1016/j.dld.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 41.Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009;136:1979–1988. doi: 10.1053/j.gastro.2009.02.074. [DOI] [PubMed] [Google Scholar]
- 42.Wheatcroft J, Wakelin D, Smith A, et al. Enterochromaffin cell hyperplasia and decreased serotonin transporter in a mouse model of postinfectious bowel dysfunction. Neurogastroenterol Motil. 2005;17:863–870. doi: 10.1111/j.1365-2982.2005.00719.x. [DOI] [PubMed] [Google Scholar]
- 43.Spiller R. Serotonin and GI clinical disorders. Neuropharmacology. 2008;55:1072–1080. doi: 10.1016/j.neuropharm.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 44.Spiller R. Serotonin, inflammation, and IBS: fitting the jigsaw together? J Pediatr Gastroenterol Nutr. 2007;45(Suppl 2):S115–S119. doi: 10.1097/MPG.0b013e31812e66da. [DOI] [PubMed] [Google Scholar]
- 45.Dunlop SP, Coleman NS, Blackshaw E, et al. Abnormalities of 5-hydroxytryptamine metabolism in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2005;3:349–357. doi: 10.1016/s1542-3565(04)00726-8. [DOI] [PubMed] [Google Scholar]
- 46.Mawe GM, Coates MD, Moses PL. Review article: intestinal serotonin signalling in irritable bowel syndrome. Aliment Pharmacol Ther. 2006;23:1067–1076. doi: 10.1111/j.1365-2036.2006.02858.x. [DOI] [PubMed] [Google Scholar]
- 47.Coates MD, Mahoney CR, Linden DR, et al. Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and IBS. Gastroenterology. 2004;126:1657–1664. doi: 10.1053/j.gastro.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 48.Kapeller J, Houghton LA, Monnikes H, et al. First evidence for an association of a functional variant in the microRNA-510 target site of the serotonin receptor-type 3E gene with diarrhea predominant irritable bowel syndrome. Hum Mol Genet. 2008;17:2967–2977. doi: 10.1093/hmg/ddn195. [DOI] [PubMed] [Google Scholar]
- 49.Camilleri M, Andrews CN, Bharucha AE, et al. Alterations in expression of p11 and SERT in mucosal biopsy specimens of subjects with irritable bowel syndrome. Gastroenterology. 2007;132:17–25. doi: 10.1053/j.gastro.2006.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kerckhoffs AP, Ter Linde JJ, Akkermans LM, et al. Serotonin transporter transcript levels and serotonin content are increased in small intestine of irritable bowel syndrome subjects. Neurogastroenterol Motil. 2008;20:900–907. doi: 10.1111/j.1365-2982.2008.01100.x. [DOI] [PubMed] [Google Scholar]
- 51.Rahimi R, Nikfar S, Abdollahi M. Efficacy and tolerability of alosetron for the treatment of irritable bowel syndrome in women and men: a meta-analysis of eight randomized, placebo-controlled, 12-week trials. Clin Ther. 2008;30:884–901. doi: 10.1016/j.clinthera.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 52.Lembo T, Wright RA, Bagby B, et al. Alosetron controls bowel urgency and provides global symptom improvement in women with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2001;96:2662–2670. doi: 10.1111/j.1572-0241.2001.04128.x. [DOI] [PubMed] [Google Scholar]
- 53.Chey WD, Cash BD. Cilansetron: a new serotonergic agent for the irritable bowel syndrome with diarrhoea. Expert Opin Investig Drugs. 2005;14:185–193. doi: 10.1517/13543784.14.2.185. [DOI] [PubMed] [Google Scholar]
- 54.Chey WD, Pare P, Viegas A, et al. Tegaserod for female subjects suffering from IBS with mixed bowel habits or constipation: a randomized controlled trial. Am J Gastroenterol. 2008;103:1217–1225. doi: 10.1111/j.1572-0241.2008.01808.x. [DOI] [PubMed] [Google Scholar]
- 55.Kale-Pradhan PB, Wilhelm SM. Tegaserod for constipation-predominant irritable bowel syndrome. Pharmacotherapy. 2007;27:267–277. doi: 10.1592/phco.27.2.267. [DOI] [PubMed] [Google Scholar]
- 56.Greenwood-Van Meerveld B, Venkova K, Hicks G, et al. Activation of peripheral 5-HT receptors attenuates colonic sensitivity to intraluminal distension. Neurogastroenterol Motil. 2006;18:76–86. doi: 10.1111/j.1365-2982.2005.00723.x. [DOI] [PubMed] [Google Scholar]
- 57.Crowell MD, Mathis C, Schettler VA, et al. The effects of tegaserod, a 5-HT receptor agonist, on gastric emptying in a murine model of diabetes mellitus. Neurogastroenterol Motil. 2005;17:738–743. doi: 10.1111/j.1365-2982.2005.00681.x. [DOI] [PubMed] [Google Scholar]
- 58.Brandt LJ. The FDA’s decision-making process: isn’t it time to temper the principle of protective paternalism? Am J Gastroenterol. 2008;103:1226–1227. doi: 10.1111/j.1572-0241.2008.01815.x. [DOI] [PubMed] [Google Scholar]
- 59.Liu Q, Yang Q, Sun W, et al. Discovery and characterization of novel tryptophan hydroxylase inhibitors that selectively inhibit serotonin synthesis in the gastrointestinal tract. J Pharmacol Exp Ther. 2008;325:47–55. doi: 10.1124/jpet.107.132670. [DOI] [PubMed] [Google Scholar]
- 60.Freiman J, Jackson J, Frazier KS, et al. LX1031: inhibition of 5-HT synthesis as a new target in the management of irritable bowel syndrome (IBS) Neurogastroenterol Motil. 2009;21:250. [Google Scholar]