Abstract
Background
Measles, a vaccine-preventable disease that can cause severe complications, was declared eliminated from the U.S. in 2000. The last published summary of U.S. measles epidemiology was during 2001−2008. We summarized U.S. measles epidemiology during 2009−2014.
Methods
We compared demographic, vaccination, and virologic data on confirmed measles cases reported to the Centers for Disease Control and Prevention during 1/1/2009—12/31/2014 and 1/1/2001—12/31/2008.
Results
During 2009−2014, 1264 confirmed measles cases were reported in the U.S., including 275 importations from 58 countries and 66 outbreaks. The annual median number of cases and outbreaks during this period was 130 (range: 55–667 cases) and 10 (range: 4–23 outbreaks), respectively, compared with an annual median of 56 cases (p=0.08) and 4 outbreaks during 2001−2008 (p=0.04). Among U.S.-resident case-patients during 2009−2014, children aged 12–15 months had the highest measles incidence (65 cases; 8.3 cases/million person-years), and infants aged 6–11 months had the second highest incidence (86 cases; 7.3 cases/million person-years). During 2009−2014, 865 (74%) of 1173 U.S.-resident case-patients were unvaccinated and 188 (16%) had unknown vaccination status; of 917 vaccine-eligible U.S.-resident case-patients, 600 (65%) were reported as having philosophical or religious objections to vaccination.
Conclusions
Although the U.S. has maintained measles elimination since 2000, measles outbreaks continue to occur globally resulting in imported cases and potential spread. The annual median number of cases and outbreaks more than doubled during 2009−2014 compared to the earlier post-elimination years. To maintain elimination, it will be necessary to maintain high two-dose vaccination coverage, continue case-based surveillance, and monitor the patterns and rates of vaccine exemption.
Keywords: measles, epidemiology, measles mumps rubella (MMR) vaccine, measles elimination
Background
Measles is a highly infectious, acute viral disease that causes a characteristic maculopapular rash, respiratory symptoms, and fever. Measles-related complications include diarrhea (affecting 8% of case-patients), otitis media (7−9%), pneumonia (1−6%), and encephalitis (1−2 per 1000 case-patients) [1]. Death occurs in 1−3 per 1000 cases [1]. In the pre-vaccine era, an estimated 3−4 million people in the U.S. became infected with measles annually, of whom 500,000 were reported. Of the reported cases, 500 persons died, 48,000 were hospitalized, and 4000 reported measles encephalitis annually [1].
High population immunity is the most effective way to prevent measles. The national measles vaccine program launched in 1963. Today, the U.S. recommends 2 doses of measles-mumps-rubella (MMR) vaccine for all school-aged children and high-risk adults born during or after 1957 (i.e., healthcare personnel, international travelers, and students at post-high school educational institutions) [2]. State laws require age-appropriate vaccination of children enrolled in childcare facilities and documentation of evidence of measles immunity upon entry into kindergarten or first grade [3]. For non-high risk adults born during or after 1957 and preschool-aged children who lack evidence of measles immunity, one dose of MMR vaccine is recommended [2].
The national measles vaccination program has achieved and maintained high one- and two-dose MMR vaccine coverage in pre-school and school-aged children. That success, coupled with improved control of measles throughout the Americas, resulted in the declaration of measles elimination in the U.S. in 2000 [4]. Elimination is the absence of endemic disease transmission (i.e., no epidemiological or virological evidence that measles virus transmission is continuously occurring for ≥12 months in a defined geographical area that has adequate surveillance) [4]. In December 2011, an external expert panel verified that the U.S. sustained elimination of measles from 2001−2011 [5].
However, as of 2012, there were still an estimated 20 million cases of measles globally [6] and 145,700 measles-related deaths annually [7], with extensive outbreaks in 2013 and 2014 occurring in the World Health Organization’s (WHO) European and Western Pacific Regions [8, 9]. As a result of importations of measles virus from abroad and subsequent spread into large unvaccinated communities, in 2014, the U.S. experienced the most measles cases and the largest measles outbreak in 20 years.
We previously reported on measles epidemiology in the U.S. from 2001−2008 [10]. In this report, we summarize measles epidemiology in the U.S. during the post-elimination years 2009−2014 and compared the findings with earlier post-elimination years.
Methods
All states legally mandate that healthcare personnel and clinical laboratories report measles cases to their respective local health departments. Measles surveillance is a passive reporting system that is activated when a suspected measles case is reported. This triggers a search for additional case-patients that might have had contact with the suspect case-patient. The sensitivity of the system is increased through reporting and a thorough investigation of all suspected case-patients.
Measles cases were identified and classified using standard case definitions and case classification [11]. A confirmed case of measles was either laboratory-confirmed or had a direct epidemiologically linkage to a patient with laboratory-confirmed measles infection [11]. State health departments reported confirmed cases of measles to the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC) via telephone or email [12] and electronically to the National Notifiable Diseases Surveillance System [13].
An outbreak of measles in the U.S. was defined as a chain of transmission with ≥3 confirmed cases. We analyzed all cases and outbreaks of measles reported in the U.S. during 2009–2014. Comparisons were made with epidemiological data from 2001–2008. Differences in medians were calculated by Wilcoxon rank sums and differences in proportions were calculated by Mantel-Haenszel chi-square in SAS 9.3 (Cary, NC).
Cases were classified either as internationally imported (i.e., exposure to measles virus occurred outside the U.S. 7–21 days before rash onset and rash developed within 21 days of entrance into the U.S., with no known exposure to measles occurring in the U.S. during that time) or U.S.-acquired (i.e., case-patients either had not been outside the U.S. during the 21 days before rash onset or were known to have been exposed to measles within the U.S.). U.S.-acquired cases were sub-classified into 4 mutually exclusive groups: (1) import-linked (i.e., any case in a chain of transmission that was epidemiologically linked to an internationally imported case), (2) imported-virus (i.e., cases in which an epidemiologic link to an internationally imported case was not identified but viral genetic evidence indicated an imported measles genotype within the chain of transmission), (3) endemic (i.e., cases in which transmission of measles virus was continuous for ≥12 months within the U.S.), and (4) unknown source (i.e., cases in which an epidemiological or virological link to importation or to endemic transmission within the U.S. could not be established after a thorough investigation) [13, 14].
Measles genotyping was performed at CDC by the Vaccine Preventable Disease Reference Laboratories [15] using standard methods [16]. Sequence data were submitted to the WHO Global Measles Sequence Database (MeaNS) [17, 18]. Genotyped viral isolates were categorized by the WHO region (i.e., African Region, Region of the Americas, South-East Asia Region, European Region, Eastern Mediterranean Region, or Western Pacific Region) from which the virus was imported, if known.
Index case-patients were defined as having the first rash onset in the 2-case chain or outbreak; co-index case-patients were defined as patients who had rash onset within 6 days of the index case-patient. We differentiated between U.S.-resident and foreign-visitor case-patients (i.e., foreign tourists, international students, new international adoptees, recent immigrants, refugees, and cruise ship employees) when we calculated incidence so that we could use U.S. Census data as the denominator [19], as well as when we reported vaccination status, because U.S. vaccination recommendations apply only to U.S. residents. This categorization allowed the differentiation of cases that would have been preventable had the recommended vaccination policy been implemented. Non-preventable cases were defined as measles cases that occurred among U.S. residents who either (1) had received ≥1 dose of measles-containing vaccine, (2) were vaccinated as recommended if traveling internationally, (3) were not vaccinated but had other evidence of immunity (i.e., were born before 1957 and, therefore, were presumed to be immune from natural disease in childhood, had laboratory evidence of immunity), or (4) belonged to a category (such as infants <1 year of age) for whom MMR vaccination is not recommended on a routine basis. “Philosophical or religious objectors” were defined as persons who were vaccine eligible, according to recommendations of the Advisory Committee on Immunization Practices (ACIP) [2] or the WHO [7], but remained unvaccinated because of personal or parental philosophical or religious beliefs.
We examined the rates of national 1-dose measles vaccination coverage among children 19–35 months of age and 2-dose measles vaccination coverage among adolescents from 2009 through 2014 using data from the National Immunization Survey, which supplies provider-verified, population based rates of immunization with 95% confidence intervals.
Results
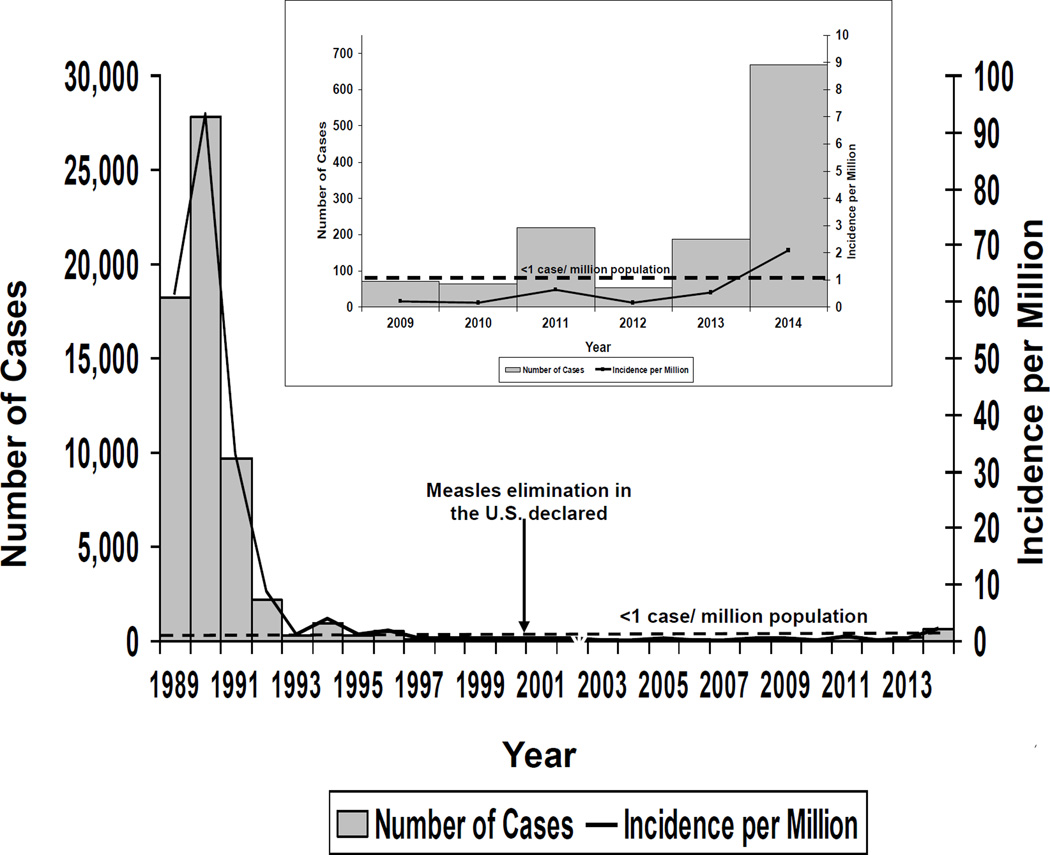
During 2009−2014, 1264 confirmed measles cases were reported in the United States from 42 states and the District of Columbia (annual median number of cases reported, 130 [range, 55 cases in 2012 to 667 reported in 2014]), representing an incidence of <1 case per million population every year, except in 2014 when the incidence was 2.08 per million population (Figure 1). Compared to earlier post-elimination years between 2001 and 2008, when the annual median number of cases reported was 56 cases/year (range, 37−140), the annual median number of cases during 2009−2014 was more than double [10], but the difference was not statistically significant (Table 1).
Figure 1.
Reported measles cases and incidence by year, United States, 1989−2014. Inset: Reported measles cases and incidence by year, United States from 2009−2014.
Gray shading: Reported number of measles cases
Black line: Measles incidence per million population
Table 1.
Comparison of key variables from the earlier post-elimination years (2001– 2008) with the later post-elimination years (2009– 2014)a
| 2001– 2008 | 2009– 2014 | p-value | |
|---|---|---|---|
| Reported case-patients annuallyb | 56 (37– 140) | 130 (55– 667) | 0.08 |
| Sex (male)c | 269/554 (49) | 682/1252 (55) | 0.02 |
| Median age (years)b | 15 (0– 89) | 14 (0– 84) | 0.53 |
| U.S. resident case-patientsc | 438/557 (79) | 1173/1263 (93) | <0.0001 |
| U.S. resident case-patients who were unvaccinated or had unknown vaccination statusc | 361/438f (83) | 1053/1173 (90) | <0.0001 |
| U.S. resident case-patients with philosophical or religious objections to vaccinationc,d | 110/162 (68) | 600/917 (65) | 0.54 |
| Preventable case-patientsce | 285/438 (65) | 917/1171 (78) | <0.01 |
| Complicationsc | 106/557 (19) | 109/1264 (9) | <0.0001 |
| Hospitalizationsc | 126/557 (23) | 211/1264 (17) | 0.003 |
| Imported cases annuallyb | 26 (18– 54) | 45 (21– 80) | 0.32 |
| Outbreaks annuallyb | 4 (2– 10) | 10 (4– 23) | 0.04 |
| Outbreak-related case-patientsb | 4 (3– 34)g | 5 (3– 383) | 0.71 |
| Outbreak durationb | 27 (3– 79) | 17 (3– 121) | 0.40 |
Data are median (range) for Wilcoxon rank sum results or n/N (%) for chi-squared results.
Differences in medians were calculated by Wilcoxon rank sums.
Differences in proportions were calculated by Mantel-Haenszel chi square.
Data on philosophical or religious objections were not routinely collected until 2004. Thus, for earlier post-elimination years, the numerator and denominator for this variable reflect data from 2004–2008. The denominator only includes vaccine-eligible U.S. resident case-patients.
Case-patients with preventable measles were case-patients for whom vaccination was recommended by the Advisory Committee on Immunization Practices but who had not received ≥1 dose of measles-containing vaccine.
In the previously published summary of measles epidemiological data from 2001– 2008 [10], the numerator was 358. In that paper, there were 3 individuals who were categorized as vaccinated, because they had a “yes” under the vaccinated variable, but they had an unknown number of doses. We re-categorized those individuals as having unknown vaccination status in this paper.
In the previously published summary of measles epidemiological data from 2001– 2008 [10], the annual median number of outbreak-related case-patients was 5. In that paper, there were 3 smaller outbreaks that were re-categorized as 1 larger outbreak by the health department after the paper was published. This resulted in a slight shift in the median number of outbreak-related case-patients.
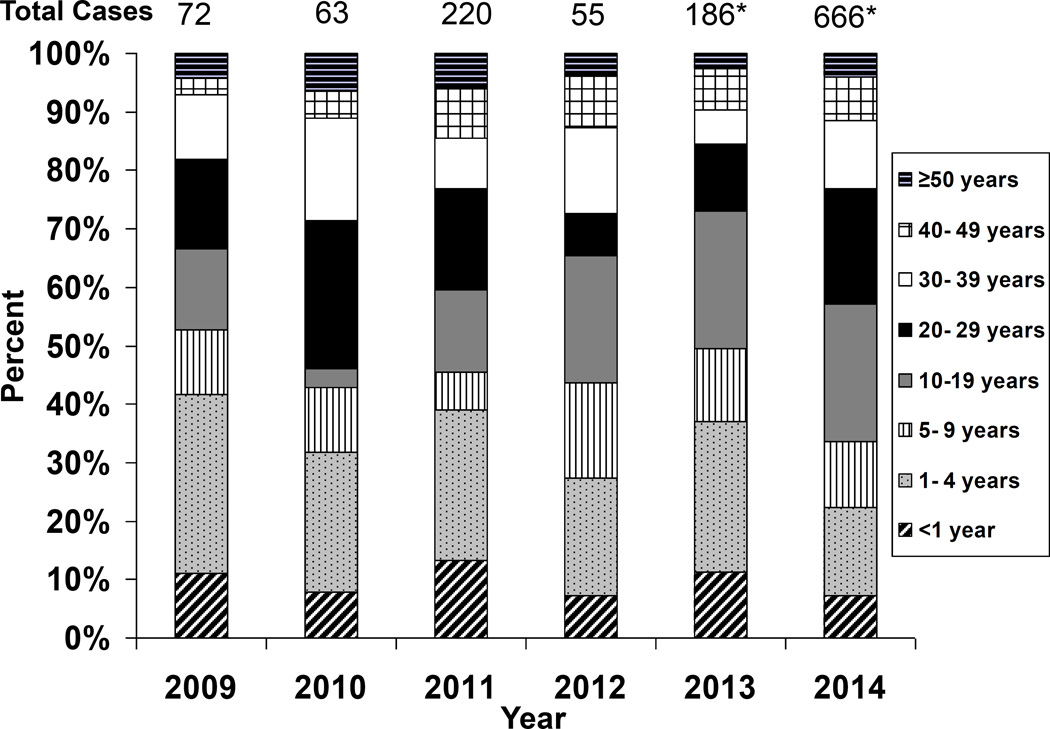
Of 1264 reported case-patients during 2009−2014, 682 (54%) were male. The median age of case-patients was 14 years (range, 1 day to 84 years). There were 115 (9%) case-patients <1 year, 254 (20%) 1−4 years, 136 (11%) 5−9 years, 255 (20%) 10−19 years, 222 (18%) 20−29 years, 135 (11%) 30–39 years, 91 (7%) 40–49 years, 54 (4%) were ≥50 years, and 2 (0.2%) were missing age information (Figure 2). Of those aged 1−4 years, 72 (28%) were aged 12−15 months. Among U.S. resident case-patients from 2009−2014, children aged 12−15 months had the highest incidence of measles of any age group (65 cases, or 8.3 cases/million person-years), and infants aged 6−11 months had the second highest incidence (86 cases, or 7.3 cases/million person-years). The incidence rate for children aged 12−15 months more than tripled compared with 2001−2008 when incidence rates were 2.6 cases/million person years, and for infants aged 6−11 months, incidence rates doubled compared with 2001−2008 when rates were 3.5 cases/million person-years.
Figure 2.
Percent of measles case-patients by age group (by year), United States, 2009−2014.
Diagonal striped bars: case-patients aged <1 year
Gray dotted bars: case-patients aged 1–4 years
Striped vertical bars: case-patients aged 5–9 years
Dark gray bars: case-patients aged 10–19 years
Black bars: case-patients aged 20–29 years
White bars: case-patients aged 30–39 years
Cross-hatched bars: case-patients aged 40–49 years
Horizontal striped bars: case-patients aged ≥50 years
*Missing data on 2 case-patients (1 in 2013 and 1 in 2014).
Complications were reported for 109 (9%) case-patients, including (in non-mutually exclusive categories): 41 (38%) with diarrhea, 36 (33%) with pneumonia, 27 (25%) with dehydration, 17 (16%) with otitis media, 11(10%) with thrombocytopenia, 3 (3%) with encephalitis, 1 with pancytopenia (1%), and 1 (1%) with hepatitis. Measles-related hospitalizations were reported for 211 (17%) case-patients (annual median number of hospitalized case-patients, 23 (range, 7−77 case-patients), whereas the annual median number of hospitalizations from 2001−2008 was 16 (range, 5–29) (p= 0.003) [10]. Of the 211 case-patients who were hospitalized during 2009−2014, only 71 (34%) reported measles-related complications. The remaining hospitalized case-patients were admitted for observation, work-up/diagnosis, or other/unknown reason. No deaths were reported during 2009−2014.
U.S. residents comprised 1173 (93%) case-patients, foreign visitors comprised 90 (7%) case-patients, and 1 (0.1%) had unknown residency status (Table 2). During 2009−2014, 865 (74%) U.S.-resident case patients were unvaccinated, 120 (10%) were vaccinated (of whom, 62 had ≥2 MMR doses), and 188 (16%) U.S.-resident case-patients had unknown vaccination status (of whom 155 [83%] patients with unknown vaccination status were adults), compared with 66% unvaccinated, 18% vaccinated, and 16% with unknown vaccination status during 2001−2008 (p<0.0001) [10].
Table 2.
Age group and vaccination status of reported measles case-patients, by U.S. residence status, United States, 2009–2014 (n= 1261)
| U.S. residents | Foreign visitors | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unvaccinated n (%) |
Vaccinated n (%) |
Unknown n (%) |
Total n (%) |
Incidence/ million population |
Unvaccinated n (%) |
Vaccinated n (%) |
Unknown n (%) |
Total n (%) |
n (%) | |
| Age group | ||||||||||
| <6 months | 22 (100) | 0 (0) | 0 (0) | 22 (2) | 1.86 | 1 (100) | 0 | 0 | 1 (1) | 23 (2) |
| 6–11 months | 85 (99) | 1 (1) | 0 (0) | 86 (7) | 7.25 | 5 (83) | 0 | 1 (17) | 6 (7) | 92 (7) |
| 12–15 months | 60 (92) | 4 (6) | 1 (2) | 65 (6) | 8.28 | 4 (67) | 1 (17) | 1 (17) | 6 (7) | 71 (6) |
| 16 months through 4 years | 130 (78) | 24 (14) | 12 (7) | 166 (14) | 1.88 | 15 (94) | 1 (6) | 0 (0) | 16 (18) | 182 (14) |
| 5–9 years | 114 (88) | 7 (5) | 8 (6) | 129 (11) | 1.05 | 5 (71) | 1 (14) | 1 (14) | 7 (8) | 136 (11) |
| 10–19 years | 215 (89) | 15 (6) | 13 (5) | 243 (21) | 0.97 | 9 (75) | 0 (0) | 3 (25) | 12 (13) | 255 (20) |
| 20–39 years | 193 (60) | 51 (16) | 79 (25) | 323 (28) | 0.63 | 10 (29) | 3 (9) | 21 (62) | 34 (38) | 357 (28) |
| 40–59 years | 42 (33) | 18 (14) | 68 (53) | 128 (11) | 0.25 | 6 (86) | 0 (0) | 1 (14) | 7 (8) | 135 (11) |
| ≥60 years | 3 (33) | 0 (0) | 6 (67) | 9 (1) | 0.02 | 0 (0) | 0(0) | 1 (100) | 1 (1) | 10 (1) |
| Total* | 864 (74) | 120 (10) | 187 (16) | 1171 (100) | 0.62 | 55 (61) | 6 (7) | 29 (32) | 90 (100) | 1261 (100) |
Note. Data are number of cases in age group (% of that age group constituted by that vaccination status) or total (% of total constituted by age group) or incidence per million population.
3 subjects were excluded because they were missing data on age or residency.
Among the 392 index and co-index case-patients during 2009−2014, 225 (57%) were unvaccinated, 61 (16%) were vaccinated, and 106 (27%) had an unknown vaccination status. Among the 872 non-index and non-co-index (i.e., spread) case-patients, 697 (80%) were unvaccinated, 65 (8%) were vaccinated, and 110 (13%) had an unknown vaccination status. The median age of the index and co-index case-patients was 20 years compared with 13 years among the spread case-patients.
Of 931 case-patients associated with measles outbreaks during 2009−2014, 744 (81%) were unvaccinated, 66 (7%) were vaccinated, and 121 (13%) had an unknown vaccination status, whereas of the 333 case-patients not associated with measles outbreaks, 178 (54%) were unvaccinated, 60 (18%) were vaccinated, and 95 (29%) had an unknown vaccination status. The proportion of case-patients associated with measles outbreaks who were unvaccinated or had unknown vaccination status (93%) was higher than the proportion unvaccinated or who had unknown vaccination status who were not associated with outbreaks (82%) (p <0.0001). On an annual basis, the proportion of case-patients who were unvaccinated or who had an unknown vaccination status ranged from 78% in 2012 to 92% in 2013.
National rates of 1-dose vaccination coverage among children 19–35 months of age ranged from 90% to 92% from 2009−2013, compared with rates of 91% to 93% for 2001−2008 [20]. Rates of 2-dose coverage among adolescents ranged from 89% to 92% from 2009−2014, compared with rates of 87% to 89% for 2006−2008 which are the only years for which 2-dose coverage data were available [21].
Of the 1171 measles cases that occurred among U.S. residents for whom we had data on age, 917 (78%) were considered preventable (Table 3), compared with 65% of U.S.-resident case-patients from 2001−2008 (p<0.01) [10]. Of the preventable cases during 2009−2014, 758 (83%) were acquired in the U.S. Of the 194 U.S.-resident case-patients who traveled internationally, 170 (88%) were unvaccinated or had an unknown vaccination status; of whom 159 (94%) were considered to have preventable measles, including 28 (18%) who were aged 6–11 months. A total of 600 (65%) of 917 vaccine-eligible U.S.-resident case-patients were reported as having a philosophical or religious objection to vaccination during 2009−2014, similar to 68% from 2004−2008, the only years data were available (p=0.54).
Table 3.
Number of preventablea and non-preventableb reported cases of measles among U.S. residents, by age, travel history, and measles vaccination status, United States, 2009–2014 (n=1171)
| International travel | No international travel | Total | |||
|---|---|---|---|---|---|
| Age group | Vaccinated | Not vaccinated or unknown vaccination status |
Vaccinated | Not vaccinated or unknown vaccination status |
|
| <6 months | 0 | 1 | 0 | 21 | 22 |
| 6–11 months | 0 | 28a | 1 | 57 | 86 |
| 12–15 months | 0 | 27a | 4 | 34 | 65 |
| 16 months– 4 years | 4 | 15a | 20 | 127a | 166 |
| 5–9 years | 3 | 2a | 4 | 120a | 129 |
| 10–19 years | 1 | 20a | 14 | 208a | 243 |
| 20–29 years | 8 | 32a | 21 | 140a | 201 |
| 30–39 years | 6 | 13a | 16 | 87d | 122 |
| ≥40 years | 2 | 32c | 16 | 87e | 137 |
| Total case-patients | 24 | 170 | 96 | 881 | 1171f |
| Total preventable | 0 | 159 | 0 | 758 | 917 |
| Total non-preventable | 24 | 11 | 96 | 123 | 254 |
Case-patients with preventable measles were case-patients for whom vaccination was recommended by the Advisory Committee on Immunization Practices but who had not received ≥1 dose of measles-containing vaccine.
Cases were defined as non-preventable if they occurred among US-resident case-patients who had received ≥1 dose of measles containing vaccine, were vaccinated as recommended if traveling internationally, or were not vaccinated but had other evidence of measles immunity (i.e., were born before 1957 and therefore were presumed to be immune from natural disease in childhood, had laboratory evidence of immunity, or laboratory confirmation of disease) or for whom vaccination is not recommended.
Of the 32 case-patients ≥40 years who were unvaccinated or had unknown vaccination status who traveled internationally, 22 were preventable. All 10 non-preventable case-patients were persons born before 1957 (measles-containing vaccine is not recommended for people in this age group, because they are presumed to be immune from natural disease in childhood).
Of the 87 case-patients aged 30–39 years who were unvaccinated or had unknown vaccination status who did not travel internationally, 86 were preventable. The non-preventable case-patient had a documented positive measles titer.
Of the 87 case-patients aged ≥40 years who were unvaccinated or had unknown vaccination status who did not travel internationally, 77 were preventable. Of the 10 non-preventable case-patients, 8 occurred in persons born before 1957 (measles-containing vaccine is not recommended for people in this age group, because they are presumed to be immune from natural disease in childhood) and 2 case-patients had documented positive measles titers.
Missing age data on 2 case-patients.
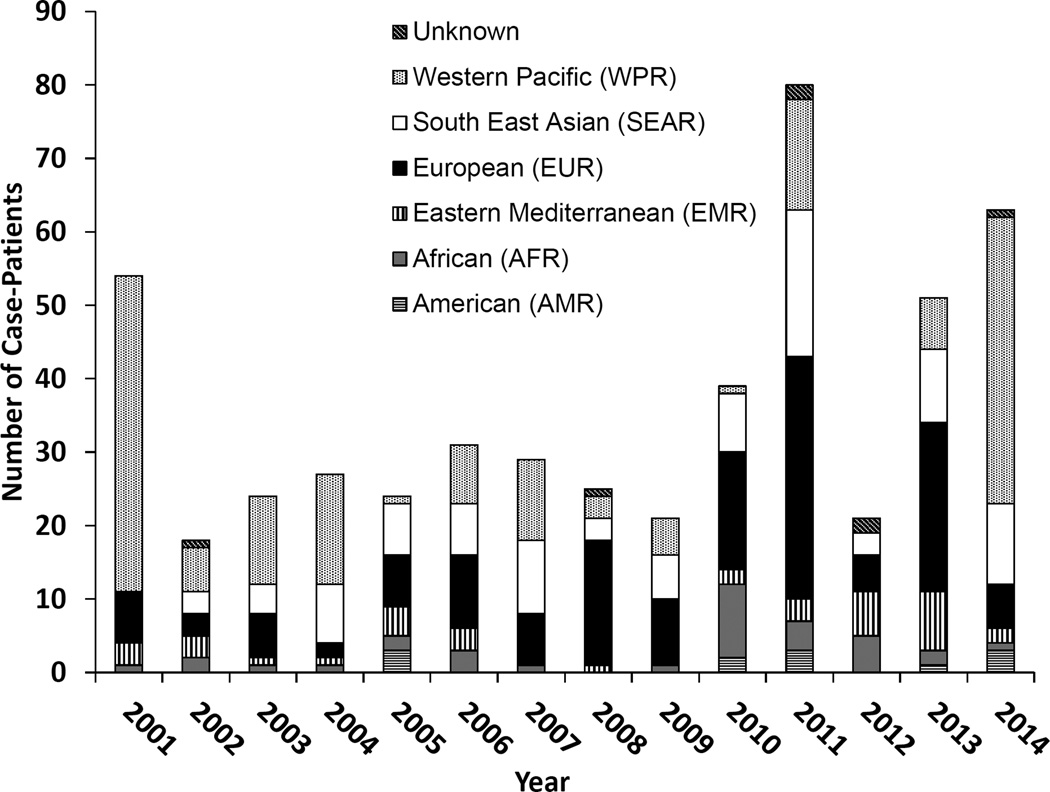
During 2009−2014, 275 (22%) cases were imported from 58 countries (annual median no. of cases imported, 45 [range, 21 to 80 cases]), compared with 232 (42%) cases imported from 44 countries during 2001−2008 (annual median number of cases imported, 26), p=0.32. During 2009−2014, U.S. residents comprised the majority of imported cases (194 imports, 71%). There was annual variation in the regional distribution from which the virus was imported during 2009−2014 (Figure 3). The highest number of imported cases were from the WHO European Region (92 [34%]), including 22 from the United Kingdom, 20 from France, 15 from Italy, and 12 from Germany. A median of 94 U.S.-acquired cases were reported annually (range, 24 to 604 cases). The 989 U.S.-acquired cases reported during 2009–2014 were classified as follows: 673 (68%) were import-linked cases, 256 (26%) were imported-virus or epidemiologically-linked to imported-virus cases, 0 were endemic cases, and 60 (6%) cases were of an unknown source. The transmission setting was known for 709 (72%) of the 989 U.S.-acquired cases. In non-mutually exclusive categories, transmission occurred in the home for 504 cases (71%), in the community for 295 (42%), in a healthcare facility for 55 (8%), at church for 49 (7%), at non-healthcare occupational settings for 19 (3%), at a childcare center for 14 (2%), at school for 6 (1%), and at other locations for 22 case-patients (3%).
Figure 3.
Measles importations to the U.S. by World Health Organization region, 2009−2014
White diagonal stripes on black background: importations of unknown origin
Black dots on white background: Western Pacific Region
White shading: South-East Asia Region
Black shading: European Region
Black and white vertical stripes: Eastern Mediterranean Region
Dark gray shading: African Region
Black and white horizontal stripes: Region of the Americas
During 2009–2014, a measles genotype was obtained from 143 (52%) of 275 imported cases and 61 (92%) of 66 outbreaks. Among genotypes obtained from imported and U.S.-acquired case-patients, B3 was the predominant measles genotype identified during 2009–2014 comprising 152 (35%) of the 434 genotypes reported. The other genotypes identified were D8 (101, 23%), D4 (89, 21%), D9 (64, 15%), H1 (18, 4%), and G3 (6, 1%). Final genotype results were missing on 4 (1%) specimens that were tested. These genotypes are associated with endemic transmission in many countries in Asia, Africa, and Europe.
During 2009–2014, there were 66 outbreaks (annual median number of outbreaks, 10 [range, 4–23 outbreaks]); this is more than double the annual median number of outbreaks that occurred in the earlier post-elimination years when the median was 4 outbreaks per year (range, 2–10 outbreaks), p=0.04 [10]. Of the 1264 case-patients reported during 2009–2014, 932 (74%) were outbreak-related. The median number of case-patients per outbreak was 5 (range, 3–383 case-patients) during 2009–2014 and 4 (range, 3–34 case-patients) during 2001–2008 (p=0.71) [10]. Outbreak duration (i.e., the time between the onset of rash in the first case and that in the last case) ranged from 3 to 121 days (median outbreak duration, 17 days) during 2009–2014 compared with a range of 3 to 79 days (median outbreak duration, 27 days) during 2001–2008 (p=0.40) [10]. The largest outbreaks during 2009–2014 are summarized in Table 4, with 4 (50%) of the outbreaks with ≥20 case-patients occurring primarily among philosophical or religious objectors.
Table 4.
Measles Outbreaks with ≥20 Case-Patients in the United States during 2009—2014
| Year | Cases, no. |
Primary state/ reporting district |
Primary setting of outbreak |
Median Age of case-patients |
Source Country (genotype) |
No. (%) unvaccinated |
No. (%) with unknown vaccination status |
Total number (%) of Philosophical or Religious Objectorsb |
No. (%) too young for being vaccinatedb |
No. (%) with other/unknown reasons for not being vaccinatedb,d |
|---|---|---|---|---|---|---|---|---|---|---|
| 2014 | 383 | OH | Household/Community | 15 years | Philippines (D9) | 340 (89) | 38 (10) | 281 (83) | 20 (6) | 39 (12) |
| 2013 | 59 | NYC | Household | 4 years | United Kingdom (D8) | 59 (100) | 0 (0) | 54 (92) | 4 (7) | 1 (2) |
| 2014 | 43 | KS/MO | Household | 21 years | Federated States of Micronesia (B3) | 29 (67) | 10 (23) | 2 (7) | 7 (24) | 20 (69) |
| 2014 | 34 | CAa+ 3 states | Community | 18 years | Unknown (B3) | 23 (68) | 5 (15) | 11 (48) | 2 (9) | 10 (44) |
| 2014 | 25 | NYC | Community | 22 years | Unknown (B3) | 9 (36) | 10 (40) | 2 (22) | 4 (44) | 3 (33) |
| 2013 | 23 | NC | Household/Community | 14 years | India (D8) | 18 (78) | 2 (9) | 18 (100)c | 0 (0) | 0 (0) |
| 2013 | 21 | TX | Church | 13 years | Indonesia (D9) | 18 (86) | 1 (5) | 17 (94) | 1 (6) | 0 (0) |
| 2011 | 21 | MN | Shelter | 23 months | Kenya (B3) | 17 (81) | 4 (19) | 7 (41) | 7 (41) | 3 (18) |
The 2014 California outbreak continued into 2015 (and was much larger and affected additional states than the total reported here). However, this report only included data through week 52 in 2014.
Denominators were the number unvaccinated.
An additional case-patient with unknown vaccination status was reported as having a philosophical or religious objection but was not included in this cell since the denominator only included unvaccinated case-patients (not those with unknown vaccination status).
Other reasons included: missed opportunity, invalid dose, on an alternative plan, hard to reach, just turned 12 months, and unknown.
Discussion
Although measles was declared eliminated in the U.S. in 2000 [4] and maintenance of elimination was verified in 2011 [5], measles cases and outbreaks have continued to occur. The proportion of U.S.-resident case-patients was higher during 2009−2014 compared to the earlier post-elimination years and there were twice as many outbreaks than during 2001−2008. Nonetheless, despite more U.S.-resident case-patients and outbreaks in recent years compared with earlier post-elimination years, there were still fewer outbreaks and fewer total cases reported annually during 2009−2014 than there were from 1994−1999, the 6 year period pre-elimination (a median of 10 outbreaks and 1264 total cases [median: 130 cases annually] during 2009−2014 vs. a median of 15 outbreaks and 2118 total cases [median: 224 cases annually] during 1994−1999) [22–26].
Globally, 20 million cases of measles occur annually [27]. In recent years, there have been numerous outbreaks with tens of thousands of cases reported on multiple continents, including countries that are traveled to frequently by U.S. residents [27]. From 2009−2014, the highest number of imported cases into the U.S. were from the WHO European Region, but all regions outside of the Americas are a continued source of importations. Measles importations reflected both the incidence of measles in countries around the world and travel patterns. Unvaccinated U.S. residents returning from trips abroad comprised the majority of imported measles cases in the U.S., as opposed to foreign visitors. Between 2012 and 2014, the United States experienced the arrival of an average of 12.2 million nonresidents from Western Europe annually [28–30], and 11.5 million U.S. citizens traveled to European countries annually [31, 32]; however, it experienced a much smaller number of travelers to and from Africa and Asia [28–32], where the incidence of measles is higher [27].
MMR vaccination coverage in the U.S. has remained stable with 90−92% 1-dose coverage among children aged 19–35 months from 2009−2013 [20] and 89−92% 2-dose coverage for adolescents during 2009−2014 [21]. Elimination was achieved with the current vaccination coverage levels and has not decreased on a national level since elimination was declared [4, 20]. Although 10% of case-patients during 2009−2014 were among vaccinated U.S. residents, this has not changed since elimination because of the effectiveness of the measles component of the MMR vaccine and the high MMR vaccination coverage of the population. It is also reassuring that although tens of thousands of people were likely exposed from the 1264 case-patients, relatively few exposed vaccinated individuals actually became infected due to high population immunity.
Measles outbreaks often began among unvaccinated individuals returning to the U.S. after being infected abroad and were subsequently sustained in pockets where unvaccinated people resided. Clustering among unvaccinated people is a common phenomenon and facilitates the spread of the virus [33]. Unvaccinated persons comprised the overwhelming majority of cases and outbreaks during 2009−2014, and over two-thirds of U.S. resident case-patients were reported as having a philosophical or religious objection. Case-patients who were reported as having personal or philosophical objections belonged to diverse sub-populations that spanned the spectrum on socioeconomic status, as well as political and religious ideologies [34–38].
The highest incidence of measles during 2009−2014 occurred among children aged 12−15 months, illustrating a risk for measles in young children around the recommended age for the first MMR dose. Recent data from 11,206 parents of children aged 24–35 months at the time of the 2009 National Immunization Survey has shown that 26% delayed, 8% refused, and 6% both delayed and refused vaccines [39]. Thus, it is important for healthcare personnel to follow measles vaccine policy recommendations for age-appropriate and timely vaccination and to engage parents who have concerns about vaccinating their children.
Healthcare personnel also have a role in rapidly identifying individuals who might be suspect measles cases. In recent measles outbreaks, measles was not considered in the differential diagnosis during the patient’s arrival at the healthcare facility [40, 41]. Thus, the implementation of airborne precautions was often either delayed or not done at all [42]. Additionally, late recognition of measles delays contact tracing and the implementation of appropriate quarantine measures, resulting in more exposures.
Although the overall percentage of hospitalizations was lower during 2009−2014 (17%) compared with 2001−2008 (23%), the annual median number of hospitalized case-patients was higher during 2009−2014 compared with the earlier post-elimination years (23 vs. 16 case-patients annually, respectively). This is despite the fact that specific groups who were affected by measles during 2009−2014 were less likely to seek medical care (e.g., Amish), even when they reported complications. Nonetheless, measles patients are often sick enough that at least half seek medical evaluation [42].
Two of the larger outbreaks during 2009−2014 had unknown source cases, but the genotype of the imported virus was identified. Molecular epidemiology has been particularly useful when there are unknown source cases by identifying genotypes that are circulating in countries that have not yet eliminated measles. This has provided further assurance that these unknown source cases are the result of imported virus rather than by circulation of an endemic genotype in the U.S. The molecular epidemiology analyses are facilitated by the global measles sequence database, MeaNS, which now contains sequences from over 22,000 cases. This allows for timely tracking of transmission chains on a global scale [18].
Although the U.S. has maintained measles elimination since 2000, measles outbreaks continue to occur globally, and therefore, the U.S. remains at risk of imported measles and potential spread. Measles is highly contagious, and when the virus lands in communities with pockets of unvaccinated individuals, it can lead to outbreaks. While these outbreaks have been controlled and the overall population susceptibility to measles remains low in the U.S., they require resource-intensive public health responses to contain them, and they divert resources from other public health activities. Early recognition of cases is challenging given the overall low number of cases in the U.S., but is critical to limiting transmission. In the current environment where measles is ubiquitous outside the Western Hemisphere, it will be necessary to have a committed global response to eradicate measles, as well as ensure that the U.S. maintains high two-dose vaccination coverage, continues case-based surveillance, and monitors the patterns and rates of vaccine exemption in order to maintain measles elimination.
Key points.
Although the U.S. has maintained measles elimination since 2000, imported cases still occur. Infants and young children had the highest incidence of measles. Over two-thirds of cases occurred among unvaccinated individuals; a majority were reported as philosophical or religious objectors.
Acknowledgments
We would like to thank Raydel Anderson, Rebecca, McNall and Elena Lopareva at CDC and VPD Reference Centers for genotyping and reporting sequence data.
Funding: No external funding sources were used to gather the data, analyze the data, or write up the findings.
Footnotes
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest: None reported
References
- 1.Strebel PM, Papania MJ, Parker Fiebelkorn A, Halsey NA. Measles Vaccine. In: Plotkin SA, Orenstein WA, Offit P, editors. Vaccines. 6 ed. Elsevier Saunders; 2013. pp. 352–387. [Google Scholar]
- 2.McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2013;62(RR-04):1–34. [PubMed] [Google Scholar]
- 3.Centers for Disease C. School immunization requirements for measles--United States, 1982. MMWR Morb Mortal Wkly Rep. 1982;31(6):65–67. [PubMed] [Google Scholar]
- 4.Katz SL, Hinman AR. Summary and conclusions: measles elimination meeting, 16–17 March 2000. J Infect Dis. 2004;189(Suppl 1):S43–S47. doi: 10.1086/377696. [DOI] [PubMed] [Google Scholar]
- 5.Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA pediatrics. 2014;168(2):148–155. doi: 10.1001/jamapediatrics.2013.4342. [DOI] [PubMed] [Google Scholar]
- 6.Fiebelkorn AP, Goodson JL. Measles (Rubeola) In: Brunette G, Kozarsky PE, editors. CDC Health Information for International Travel (The Yellow Book) New York, NY: Oxford University Press; 2014. [Google Scholar]
- 7.World Health Organization. Fact Sheet N. 286. Measles. Available at: http://www.who.int/mediacentre/factsheets/fs286/en/.
- 8.World Health Organization. Measles-Rubella Bulletin. [Accessed November 25, 2014]; Available at: http://www.wpro.who.int/immunization/documents/mrbulletinvol8issue10pdf?ua=1.
- 9.World Health Organization. Measles- WHO European Region. [Accessed May 15, 2015]; Available at: http://www.who.int/csr/don/6-march-2015-measles/en/.
- 10.Parker Fiebelkorn A, Redd SB, Gallagher K, et al. Measles in the United States during the Postelimination Era. J Infect Dis. 2010;202(10):1520–1528. doi: 10.1086/656914. [DOI] [PubMed] [Google Scholar]
- 11.Council of State and Territorial Epidemiologists. Surveillance Case Definition for Measles. Position Description 12-ID-07. [Accessed November 26, 2014]; Available at: http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/12-ID-07FINAL.pdf. [Google Scholar]
- 12.Guris D, Harpaz R, Redd SB, Smith NJ, Papania MJ. Measles surveillance in the United States: an overview. J Infect Dis. 2004;189(Suppl 1):S177–S184. doi: 10.1086/374606. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Nationanl Notifiable Diseases Surveillance System (NNDSS) [Accessed November 26, 2014]; Available at: http://wwwn.cdc.gov/nndss/.
- 14.Papania MJ, Seward JF, Redd SB, Lievano F, Harpaz R, Wharton ME. Epidemiology of measles in the United States, 1997–2001. Journal of Infectious Diseases. 2004;189:S61-S8. doi: 10.1086/381557. [DOI] [PubMed] [Google Scholar]
- 15.Association of Public Health Laboratories. APHL/CDC Vaccine Preventable Disease (VPD) Reference Centers. [Accessed June 24, 2015]; Available at: http://www.aphl.org/AboutAPHL/publications/Documents/ID_VPDQuickReferenceGuide_92014.pdf. [Google Scholar]
- 16.Bankamp B, Byrd-Leotis LA, Lopareva EN, et al. Improving molecular tools for global surveillance of measles virus. J Clin Virol. 2013;58(1):176–182. doi: 10.1016/j.jcv.2013.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rota PA, Brown K, Mankertz A, et al. Global distribution of measles genotypes and measles molecular epidemiology. J Infect Dis. 2011;204(Suppl 1):S514–S523. doi: 10.1093/infdis/jir118. [DOI] [PubMed] [Google Scholar]
- 18.Rota PA, Brown KE, Hubschen JM, et al. Improving global virologic surveillance for measles and rubella. J Infect Dis. 2011;204(Suppl 1):S506–S513. doi: 10.1093/infdis/jir117. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau. Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2013. [Accessed December 4, 2014]; Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 20.Centers for Disease Control and Prevention. National Immunization Survey (NIS)- Children (19–35 months) [Accessed April 29, 2015]; Available at: http://www.cdc.gov/vaccines/imz-managers/coverage/nis/child/index.html.
- 21.Centers for Disease Control and Prevention. NIS- Teen Data- Adolescents/Teens (13– 17 years) [Accessed April 29, 2015]; Available at: http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/index.html.
- 22.Yip FY, Papania MJ, Redd SB. Measles outbreak epidemiology in the United States, 1993–2001. J Infect Dis. 2004;189(Suppl 1):S54–S60. doi: 10.1086/379377. [DOI] [PubMed] [Google Scholar]
- 23.Papania MJ, Seward JF, Redd SB, Lievano F, Harpaz R, Wharton ME. Epidemiology of measles in the United States, 1997–2001. J Infect Dis. 2004;189(Suppl 1):S61–S68. doi: 10.1086/381557. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease C, Prevention. Measles--United States, 1994. MMWR Morb Mortal Wkly Rep. 1995;44(26):486–487. 93–94. [PubMed] [Google Scholar]
- 25.Centers for Disease C, Prevention. Measles--United States, 1995. MMWR Morb Mortal Wkly Rep. 1996;45(15):305–307. [PubMed] [Google Scholar]
- 26.Centers for Disease C, Prevention. Measles--United States, 1996, and the interruption of indigenous transmission. MMWR Morb Mortal Wkly Rep. 1997;46(11):242–246. [PubMed] [Google Scholar]
- 27.World Health Organization. Measles & Rubella Initiative Annual Report. [Accessed 12 June 2015]; Available at: http://www.who.int/immunization/diseases/measles/mri_annual-report_2013.pdf.
- 28.Office of Travel & Tourism Industries; International Trade Administration; US Department of Commerce. I-94 Program: 2014 Monthly Arrivals Data. Non-Resident Arrivals to the United States: World Region of Residence. [Accessed 10 June 2015]; Available at: http://travel.trade.gov/view/m-2014-I-001/index.html.
- 29.Office of Travel & Tourism Industries; International Trade Administration; US Department of Commerce. 2013 Monthly Tourism Statistics: Table C- Section 1: Total Visitation, Canada, Mexico, Total Overseas, Western Europe Non-Resident Visitation to the U.S. By world region/country of residence 2013. [Accessed 10 June 2015]; Available at: http://travel.trade.gov/view/m-2013-I-001/table1.html.
- 30.Office of Travel & Tourism Industries; International Trade Administration; US Department of Commerce. 2012 Montly Tourism Statistics: Table C - Section 1: Total Visitation, Canada, Mexico, Total Overseas, Western Europe Non-Resident Visitation to the U.S. By world region/country of residence 2012. [Accessed 10 June 2015]; Available at: http://travel.trade.gov/view/m-2012-I-001/table1.html.
- 31.Office of Travel & Tourism Industries; International Trade Administration; US Department of Commerce. U.S. Citizen Travel to International Regions, 2014 and U.S. Citizen Travel to International Regions, 2013. [Accessed 10 June 2015]; Available at: http://travel.trade.gov/view/m-2014-O-001/index.html.
- 32.Office of Travel & Tourism Industries; International Trade Administration; US Department of Commerce. U.S. Citizen Travel to International Regions, 2013 and U.S. Citizen Travel to International Regions, 2012. [Accessed 10 June 2015]; Available at: http://travel.trade.gov/view/m-2013-O-001/index.html.
- 33.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics. 2004;114(1):187–195. doi: 10.1542/peds.114.1.187. [DOI] [PubMed] [Google Scholar]
- 34.North Carolina Department of Health and Human Services Division of Public Health. Measles Outbreak Associated with a Traveler to India, April–June, 2013. [Accessed 15 July 2015]; Available at: http://epi.publichealth.nc.gov/cd/rubeola/provider_memo_rubeola_08062013.pdf.
- 35.Centers for Disease C, Prevention. Measles - United States, January 1-August 24, 2013. MMWR Morb Mortal Wkly Rep. 2013;62(36):741–743. [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease C, Prevention. Notes from the field: Measles outbreak--Hennepin County, Minnesota, February–March 2011. MMWR Morb Mortal Wkly Rep. 2011;60(13):421. [PubMed] [Google Scholar]
- 37.Centers for Disease C, Prevention. Notes from the field: measles outbreak among members of a religious community - Brooklyn, New York, March–June 2013. MMWR Morb Mortal Wkly Rep. 2013;62(36):752–753. [PMC free article] [PubMed] [Google Scholar]
- 38.Gastanaduy PA, Redd SB, Fiebelkorn AP, et al. Measles - United States, January 1-May 23, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(22):496–499. [PMC free article] [PubMed] [Google Scholar]
- 39.Smith PJ, Humiston SG, Marcuse EK, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen SY, Anderson S, Kutty PK, et al. Health Care-Associated Measles Outbreak in the United States After an Importation: Challenges and Economic Impact. J Infect Dis. 2011 doi: 10.1093/infdis/jir115. [DOI] [PubMed] [Google Scholar]
- 41.Rota JS, Hickman CJ, Sowers SB, Rota PA, Mercader S, Bellini WJ. Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: high risk of infection but low risk of transmission. J Infect Dis. 2011;204(Suppl 1):S559–S563. doi: 10.1093/infdis/jir098. [DOI] [PubMed] [Google Scholar]
- 42.Fiebelkorn AP, Redd SB, Kuhar DT. Measles in Healthcare Facilities in the United States During the Postelimination Era, 2001–2014. Clin Infect Dis. 2015 doi: 10.1093/cid/civ387. [DOI] [PMC free article] [PubMed] [Google Scholar]