Abstract
Small bowel herniation underneath the iliac vessel after transperitoneal pelvic lymphadenectomy is a rare complication. This report describes the first case of bowel incarceration behind the external iliac artery after transperitoneal robotic-assisted radical prostatectomy with extended lymph node dissection in a patient with prostate cancer 1 year after surgery. After diagnosis on CT scan, an open resection of the ischemic bowel was performed. Because of thrombosis, the external iliac artery was opened, the clot was removed and the elongated artery was resected with end-to-end anastomosis. In case of a meandering iliac artery, a retroperitonealization after pelvic lymphadenectomy might be discussed.
Keywords: Internal hernia, Complication, Lymphadenectomy, Robotic-assisted radical prostatectomy
Introduction
Extended pelvic lymph node dissection (ePLND) is recommended during radical prostatectomy (RP) for prostate cancer (PCa), if the estimated risk for positive lymph nodes exceeds 5%.1 Usually, typical complications of this procedure include lymphocele with or without fever, pelvic hematoma or deep vein thrombosis.2 An internal hernia underneath the skeletonized pelvic blood vessel is a rare complication after ePLND. To our knowledge, only five cases had been described, none of which occurred after RP and ePLND.
Guba et al3 first described an internal hernia of the small bowel involving the external iliac artery in 1978 in a patient 4 month after pelvic lymphadenectomy and irradiation in testicular cancer. Kim et al4 reported a strangulated internal hernia of the small bowel underneath the external iliac artery 3 months after a laparoscopic pelvic lymphadenectomy in a patient with cervical cancer. A third case was reported by Dumont et al5 in 2013 about a strangulated internal hernia behind the external iliac artery of the small bowel 4 years after bilateral laparoscopic salpingo oophrectomy. Ardelt et al6 described an internal hernia through an orifice underneath the common iliac artery 2 years after Dargent's operation in cervical cancer and Pridjian et al described a strangulated internal hernia underneath the common iliac artery following robot-assisted lymph node dissection during radical cystectomy.7
Here we describe a case of internal herniation of the small bowel underneath the external iliac artery 1 year after robotic RP with ePLND in a patient with PCa. Beside bowel resection, the elongated artery was also resected and an end-to-end anastomosis was performed.
Case presentation
A 50-year-old male suffering from prostate cancer cT2c with Gleason score 4 + 4 = 8 underwent robot-assisted laparoscopic prostatectomy with ePLND. The histological examination showed a pT3b pN1 (4/25), Gleason 4 + 5 = 9 with an R1 situation of up 3 mm on the right prostate basis. The 4 positive lymph nodes were all found in the left obturator region. Because of an insufficient PSA-Nadir under androgen suppressing therapy, we performed a salvage radiotherapy with 72 Gy of the prostatic bed and the left iliacal axis 6 months after surgery with good PSA-response.
One year after surgery, the patient reported sudden appearance of increasing abdominal pain. The abdominal CT scan showed a small bowel obstruction (SBO) with possible herniation under an elongated left external iliac artery (Fig. 1).
Figure 1.
CT showing an internal hernia (arrow points) underneath the external iliac artery (arrow).
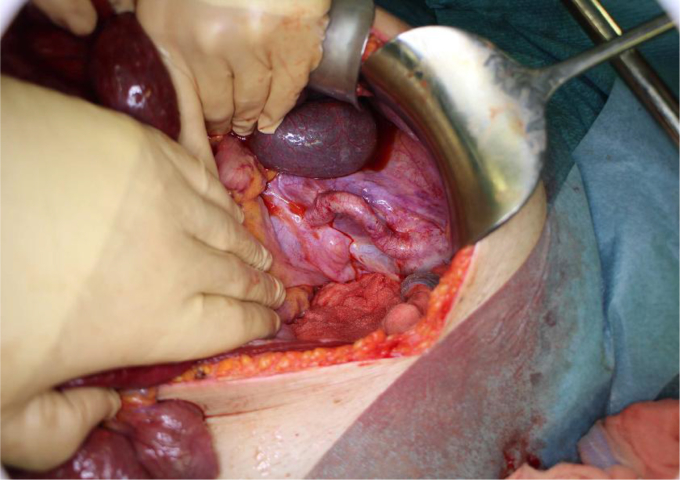
The patient underwent laparotomy with confirmation of the diagnosis of SBO (Fig. 2). A substantial part of the small bowel was found incarcerated through an orifice formed by the intraperitoneal, elongated left external iliac artery. The incarcerated small bowel was resected on a length of 1.6 m and an end-to-end anastomosis was performed.
Figure 2.
Incarcerated small bowel (arrow points) underneath the meandering external iliac artery (arrow).
Due to a lack of pulsation of the distal part of the external iliac artery, a lesion of the intima with consecutive thrombosis was suspected. Thus, an arteriotomy was performed and the thrombus has been removed. Performing a resection of 2 cm and end-to-end anastomosis of the elongated artery resulted in a shortening of the elongated artery. Additional for preventing recurrence of a herniation, the artery was fixed on the lateral peritoneum and secured by a fibrin sealant patch (TachoSil®, Takeda) (Figs. 3 and 4).
Figure 3.
Elongated external iliac artery after resection of the small bowel.
Figure 4.
Anastomosis of the external iliac artery after resection of the 2 cm elongated part.
The patient was discharged 13 days after the operation in good general condition. In a 14 months follow-up after surgery, the patient was in good health, had normal bowel activity and showed no evidence of cancer recurrence (PSA <0.01 ng/ml).
Discussion
When signs and symptoms of small bowel obstruction occur after surgery, the most common reason is adhesions.8 A much rarer reason, responsible for only around 6% for SBO are internal hernias with a total incidence of 0.2–0.9%. More than 90% of all internal hernias are caused by natural or artificial orifices built by the intestine, whereas 53% are paraduodenal hernias.9 An internal hernia caused by a vascular structure is a rarity.
Even pelvic and para-aortic lymph node dissection is a standard procedure in many operative treatments in cancer, such as prostate cancer, bladder cancer, ovarial cancer or cervical cancer, there are no clear recommendations for closure or nonclosure of the peritoneum. Franchi et al and Kadanali et al showed no difference for nonclosure of the peritoneum in postoperative morbidity after pelvic and para-aortic lymph node dissection in cervical and endometrial cancer.10, 11 However, data on meandering external iliac arteries were not given.
To our knowledge, this is the first case of an internal hernia underneath a meandering external artery after radical prostatectomy with ePLND. Several treatment options might be discussed. For instance, Guba et al closed the orifice, including the aorta, by a free peritoneal graft. Kim et al and Pridjian et al closed the orifice with peritoneum, while Ardelt et al closed it by gluing a collagen patch over the right common iliac artery. Dumont et al did not close the orifice at all. Since meandering iliac vessels seem to be a frequent anatomic variety,12 retroperitonealization after pelvic lymphadenectomy might be discussed.
Conclusion
Internal hernias underneath iliac vessels are a rare but momentous complication after ePLND and should be enclosed as a possible differential diagnosis in patient presenting with small bowel obstruction und meandering iliac vessels on CT scan.
Conflict of interest
None declared.
References
- 1.Heidenreich A., Bastian P.J., Bellmunt J. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65:124–137. doi: 10.1016/j.eururo.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 2.Briganti A., Chun F.K., Salonia A. Complications and other surgical outcomes associated with extended pelvic lymphadenectomy in men with localized prostate cancer. Eur Urol. 2006;50:1006–1013. doi: 10.1016/j.eururo.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Guba A.M., Lough F., Collins G.J. Iatrogenic internal hernia involving the iliac artery. Ann Surg. 1978;188:49–52. doi: 10.1097/00000658-197807000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim K.M., Kim C.H., Cho M.K. A strangulated internal hernia behind the external iliac artery after a laparoscopic pelvic lymphadenectomy. Surg Laparosc Endosc Percutan Tech. 2008;18:417–419. doi: 10.1097/SLE.0b013e318172fca2. [DOI] [PubMed] [Google Scholar]
- 5.Dumont K.A., Wexels J.C. Laparoscopic management of a strangulated internal hernia underneath the left external iliac artery. Int J Surg Case Rep. 2013;4:1041–1043. doi: 10.1016/j.ijscr.2013.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ardelt M., Dittmar Y., Scheuerlein H. Post-operative internal hernia through an orifice underneath the right common iliac artery after Dargent's operation. Hernia. 2014;18:907–909. doi: 10.1007/s10029-013-1129-0. [DOI] [PubMed] [Google Scholar]
- 7.Pridjian A., Myrick S., Zeltser I. Strangulated internal hernia behind the common iliac artery following pelvic lymph node dissection. Urology. 2015;86:e23–e24. doi: 10.1016/j.urology.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 8.van Oudheusden T.R., Aerts B.A., de Hingh I.H., Luyer M.D. Challenges in diagnosing adhesive small bowel obstruction. World J Gastroenterol. 2013;19:7489–7493. doi: 10.3748/wjg.v19.i43.7489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martin L.C., Merkle E.M., Thompson W.M. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186:703–717. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 10.Franchi M., Ghezzi F., Zanaboni F. Nonclosure of peritoneum at radical abdominal hysterectomy and pelvic node dissection: a randomized study. Obstet Gynecol. 1997;90:622–627. doi: 10.1016/s0029-7844(97)00359-1. [DOI] [PubMed] [Google Scholar]
- 11.Kadanali S., Erten O., Kucukozkan T. Pelvic and periaortic pertioneal closure or non-closure at lymphadenectomy in ovarian cancer: effects on morbidity and adhesion formation. Eur J Surg Oncol. 1996;22:282–285. doi: 10.1016/s0748-7983(96)80019-9. [DOI] [PubMed] [Google Scholar]
- 12.Yun W.S., Park K. Iliac anatomy and the incidence of adjunctive maneuvers during endovascular abdominal aortic aneurysm repair. Ann Surg Treat Res. 2015;88:334–340. doi: 10.4174/astr.2015.88.6.334. [DOI] [PMC free article] [PubMed] [Google Scholar]