Abstract
Traditional approaches to unbundling hearing aid services often take existing bundled charges and then separate the charges across all potential services associated with dispensing the devices. However, this method results in every patient being charged the same amount even though the complexity of the service varies across patients. We describe a model of charging for hearing aid services that takes into account three elements associated with patient services (i.e., assessing hearing status, audiologic decision making and interpretation, and counseling and treatment options) and two levels of complexity (straightforward and complex). Using this approach, there is negligible long-term financial impact on a practice however patients will perceive a lower overall cost for amplification. Additionally, this approach provides a payment structure more representative of the professional value of each visit.
Keywords: Value, audiologist expertise, patient complexity, reimbursement, unbundling
Learning Outcomes: As a result of this activity, the participant will be able to (1) differentiate between bundling, unbundling, and itemization as it applies to charges associated with hearing aid delivery; (2) identify the breadth of audiologic considerations and decisions associated with the delivery of amplification devices; (3) determine the applicability of initiating a charge system based on patient complexity in their own practice.
Hearing care, particularly the hearing health care delivery system, is in a continuous state of evolution. Over the past decade, factors such as the Affordable Care Act, emergence of big box retailers, expansion of technology-based health care delivery systems (i.e., telehealth), and consolidation of the hearing aid distribution system through manufacturer owned practices have all contributed to this evolution.1 In the future, transformational changes to hearing care are likely, including the development of new technologies for the assessment of the auditory system (e.g., functional imaging), pharmacologic treatments for hearing loss, genetic manipulations to improve auditory function, and regeneration of hair cells.
The hearing care delivery system, as well as reimbursement, will likely continue to evolve in the near future.2 The recent shift of focus to an outcomes-based model for both delivery and reimbursement is an example of the evolutionary changes in the health care delivery system. The traditional fee-for-service, procedure-based model will give way to models that promote wellness, focus on coordinated care, and result in outcomes that are measurable and positive. Testing of these models is underway (http://innovation.cms.gov/initiatives/bundled-payments/).
Currently, reimbursement for hearing care services can be thought of as two distinctive, yet parallel processes. The first is the traditional procedure-based process whereby reimbursements are derived by submitting bills to third-party payers, for example, insurance companies. This is often referred to as fee-for-service methodology. The overall value of the service is typically decided by the payers, and the hearing care providers have the option of contracting for the offered rates, or not. Once contracted, payments are most commonly based on the Current Procedural Terminology (CPT) (Copyright American Medical Association) code submitted. The CPT code chosen is directly related to the procedure performed by the provider. That is, the provider submits charges based on defined procedures, and payers reimburse the audiologist based on the agreed payment per procedure.
In the procedure-based charge and reimbursement process, payment is based on the procedure performed, regardless of the time, intensity, and/or complexity of the encounter. For example, the CPT code 92552 represents pure tone air conduction testing. Whether the test involves 6 frequencies, 12, or even 25 different frequencies, or takes 10 minutes or 30 minutes to complete, the code is the same, as is the reimbursement. There are a few exceptions to this payment methodology in audiology. For example, the charges for an auditory processing evaluation (92620 and 92621) are based specifically on the time it takes to conduct the evaluation, and not on the individual tests performed.
The second common method for reimbursement of audiology services is what is referred to as direct payment, self-pay, or out-of-pocket expenses, wherein the patient, as opposed to a third party, pays for the services and/or product at the time services are rendered. This is the process most commonly associated with hearing aid dispensing or other such services that are traditionally not covered by insurance plans. The direct payment process most often uses an up-front bundled charge, which includes all professional services and/or products provided to a patient, due in full at the time of initial purchase.3
In the realm of hearing aid delivery, the bundled charge generally includes the audiological evaluation (billed to insurance when possible); the selection, fitting, and verification of the devices; follow-up services; the devices themselves; and any associated products (e.g., earmolds, batteries, and so on). The charges typically vary based on the number of devices dispensed and their level of technology, relative to the invoiced cost from the manufacturer.
All health care providers who bill insurance companies use the fee-for-service, procedure-based process to levy charges. The bundled or direct payment system is typically reserved for elective services (i.e., cosmetic surgery) and product sales (i.e., glasses, walkers, crutches, and so on).3 Thus, for hearing aids and other amplification devices, the patient's perspective is that the charge rendered is for the product. The patient does not typically understand that the service element of the process is included in the charge.4 The cost of the knowledge, skill, and time of the audiologist somehow gets lost in the process. For example, under the typical bundled model where all payment is tied into the hearing aid purchase amount, a patient may return for as many postfitting visits as they like, regardless of whether their concerns are tied to the device. From the audiologist's viewpoint, reports of practice productivity are often tied to the number of units sold, rather than the number of patients served or beneficial outcomes.5
To add to the confusion, many times the patient is not charged when they are seen for a hearing aid evaluation but do not purchase a device.6 It may be that the patient does not understand the cost of service versus the cost of the device, or perhaps the general hearing aid market has promoted this approach for so long that the expectation of patients and providers is such that there is no cost unless a device is purchased. Ironically, by not charging for the evaluation, it is hard to make the argument to the public, or third-party payers, that audiologic services have a value.
These concerns operate in an environment where the costs of hearing aids continue to rise every year. The costs of the hearing aid have long been important factors to patients,4 7 even though the perceived benefit is not be tied to the cost of the product.8 Rather, it is the service element that is a better predictor of positive outcomes.9
There is a difference between the cost of a device/service, the charge for a device/service, and the value of a device/service (see Amlani, this issue). For many patients, the cost of a hearing aid and the charge for a hearing aid are synonymous. They will perceive the terms of cost and charge as interchangeable. In the audiology world, the cost of the device more commonly refers to the price paid by the practice to purchase the hearing aid from a company. The charge is the amount billed to the patient. The concept of value incorporates the judged quality of the device/service in combination with the charge.
The desire to address the issue of the value of audiologic services versus the cost/charge of the devices led us to consider alternative models of charging for services, particularly those associated with the hearing aid delivery process. Initial consideration was given to unbundling the charges for hearing aids. Guidance for separating the charges of the product from the evaluation, dispensing, and follow-up services was sought. In particular, the American Academy of Audiology's (AAA) A Guide to Itemizing Your Professional Services was utilized to develop a separate charge for each service component in the hearing aid delivery process.10 In this model, the patient charge for the device would be linked to the cost of the device to the practice and not to the associated services.
In the AAA guide, charges for each aspect of service delivery are calculated by first identifying the expenses and desired profitability of the practice and dividing that total by the number of hours dedicated to the practice. This establishes an hourly rate for services. This rate is then applied to appointment types to derive specific charges for each service (see Sjoblad and Abel, this issue). For example, if the rate was determined to be $150/h, and a hearing aid evaluation appointment was scheduled for 1 hour, then the charge for a hearing aid evaluation would be $150. Similarly, a follow-up visit scheduled for 30 minutes would have a charge of $75. Important in this regard is that the charges for services, based on the AAA itemization process, are based on appointment times. That is, an appointment that is 1 hour long will get a specific charge, regardless of how much time is actually spent with the patient, or the complexity of the case.
In the course of establishing the itemized charges for our services, the question was raised as to why all patients would be charged the same fee, regardless of the time or complexity of the case. Fig. 1 shows the audiograms for two patients. Patient A is a 64-year-old retired school teacher who is very interested in getting assistance to hear better when communicating with family and friends. She is active and social and sees value in amplification. Patient B is also 64 years old, with an asymmetric loss that is due to noise exposure. He continues to work as a salesman. He is trying hearing aids at the insistence of his wife but does not feel he has a hearing loss. He has limited resources so cost is a factor. He feels hearing aids will make him look old. As can be surmised, these two patients will require very different approaches for evaluation, treatment, and counseling; however, they potentially could be charged the same fees at each step in the process. They both would be charged the same amount for the hearing aid evaluation, the same amount for the fitting, and the same for follow-up services. The only difference might be in the level of technology or that one patient would require more appointments than the other. The actual complexity of care, including all the audiologic decision-making, is not considered in this model.
Figure 1.
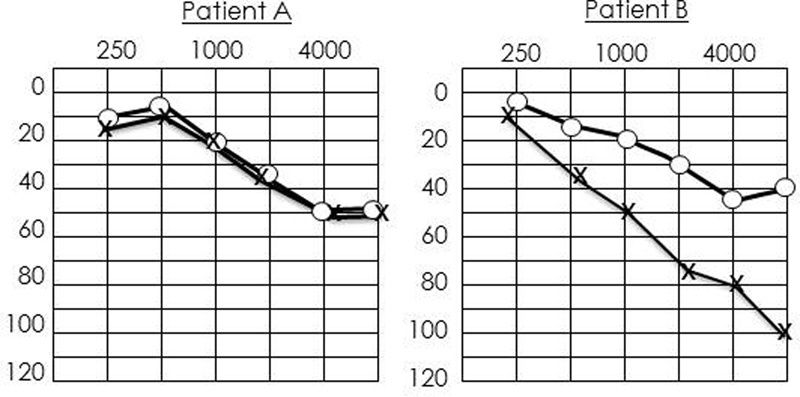
Audiograms of two different patients requiring different levels of engagement by the audiologist.
The question then became: Is appointment time the primary determinate of charges, or are there other factors such as the actual time spent with a patient or the audiologist's knowledge, skills, and decision-making that should be considered? Stated differently, could a charge system be developed that varies by the complexity of the case? Although time is one variable, the utilization of the knowledge, skills, and decision-making of the audiologist, which varies directly with the complexity of the case, could also be a factor in decisions regarding the charges levied on patients.
A good example of this type of system can be seen in the Evaluation and Management (E&M) codes used by physicians for office and hospital visits. The E&M codes are a subset of the CPT code system that was developed to allow the physician to select codes that represent the services furnished during the visit. They also were developed to ensure the medical necessity and appropriateness of the diagnostic or treatment services provided and to ensure that the documentation supports the services performed.
The charges for E&M codes vary based on three factors: patient type, setting in which the service is provided, and the level of service provided. Patient type refers to whether an individual is new to a practice (or presents with a new complaint) or has been seen in the past for the medical condition being addressed (i.e., established patient). Setting refers to the place the service is provided (e.g., outpatient, hospital, skilled nursing facility, and so on). The level of service is based on the history, physical examination, and the medical decision-making involved. This last factor accounts for a significant aspect of the knowledge and skills of the physician and/or the complexity of the patient.
Each element under the level-of-service factor varies by the complexity of the patient. First, the history taken by the provider can be problem focused, where the provider focuses on the presenting complaint, or can be comprehensive, where the provider not only reviews the present illness but also includes a review of past family, social, or medical history, along with a review of multiple body systems. Second, the examination component of the level-of-service category varies from problems focused to comprehensive, based on the number of systems assessed during the provider visit. There are very explicit guidelines for determining which level to use within each category. The third element under the level-of-service factor is medical decision-making. This element varies between straightforward, where the number of diagnostic or treatment options is limited, the amount of data to be reviewed is minimal, and the risk to the patient for complications is low, up to high complexity, where an extensive number of diagnostic or treatment options exist, the data to be reviewed are substantial, and/or the risk to the patient for complications or mortality is high. One might consider the difference in services between a patient who presents with a sprained wrist and a patient who presents with severe abdominal pain. One patient might receive a very focused but straightforward provider visit, whereas the other might require extensive testing and treatment options. A complete review of the E&M codes can be found at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/eval_mgmt_serv_guide-ICN006764.pdf.
As audiologists cannot be reimbursed by Medicare for E&M codes, most audiologists have not incorporated these codes into their billing process, although nongovernmental payers may recognize these codes if submitted by nonphysicians. Although certain factors and elements of the E&M codes, such as the location of the service provided, are not applicable to audiology services, the E&M codes can provide an analogous model for an audiology charge system. We used the E&M model in an initial attempt to develop a charge system for patient-care services based on the complexity of the patient, rather than simple unbundled charges or time-based charges. Moreover, the factors and categories of the framework were developed (1) to use terminology that was consistent with current E&M codes or third-party payer terms and (2) could be applied across a wide range of audiology services, including diagnostic services. Initially, our goal was to establish a framework for our amplification services to test the model in an area where third-party payers are typically not involved.
Framework
Table 1 displays the basic framework for the charge system developed. It includes two levels of service (straightforward and complex) and three factors (assessment of hearing status or hearing handicap, audiologic decision-making, and counseling and treatment.) The levels of service refer to the extent to which the audiologist is involved or engaged with the patient. Straightforward represents engagement at a level that is uncomplicated. Complex refers to patient engagement that may take more knowledge or skills to address patient complaints, to assess the patient condition, and/or to consider the multiple treatment options available.
Table 1. Matrix for Professional Services for New Patients.
| Assessment of Hearing Status and Hearing Handicap: Evaluating, Assessing, Diagnosing | Audiologic Decision-Making: Interpreting, Reviewing | Counseling and Treatment: Assisting, Instructing, Counseling | |
|---|---|---|---|
| New patient—straightforward | Assess chief complaint and history of chief complaint (quality, quantity, severity, duration, etc.) | Interpretation and review of limited number of problems (i.e., hearing loss only) and limited data sets (i.e., primarily audiologic procedures); uncomplicated medical history | Counseling on review of test results, handicap measures, and presentation of conclusions |
| Review of primary audiologic test results | Review of typical lifestyle concerns | Presentation of treatment options | |
| Assess with patient the psychological, educational, emotional, social, and/or vocational impact of chief complaint, using subjective measures of hearing handicap and impact on lifestyle | Decision for single product or straightforward treatment (traditional hearing aids) | Basic instruction or information dissemination and counseling regarding limited number of psychological, educational, emotional, social, and/or vocational impacts | |
| New patient—complex | Assess expanded history with review of other systems, drug and medication review, surgical/medical history, etc. | Interpretation and review of multiple issues/pathologies (i.e., tinnitus and hyperacusis) and/or multiple sets of data (multiple comorbidities); complicated medical history | Counseling on review of multiple test results, handicap measures, and presentation of conclusions |
| Review primary audiologic results (from other centers) and/or evaluate with secondary procedures to measure the extent of presenting complaint or additional complaints, such as basic tinnitus evaluation, speech-in-noise testing, etc. | Decisions for multiple treatment options | Advanced or extensive instruction or information dissemination and counseling regarding multiple aspects of psychological, educational, emotional, social, and/or vocational impact | |
| Evaluation using objective measures to assess hearing handicap and lifestyle impact | Review of multiple/unique lifestyle concerns | Presentation of multiple treatment options |
Note: See Table 2 for additional factors for established patients.
The three factors of the matrix were designed around the three aspects of audiologic care—assessment, treatment, and clinical decision-making. The assessment component is not just performing the tests, but it is about choosing which tests to perform, when, and for what reason. This requires the audiologist to use their extensive training and knowledge of the anatomical and physiological systems, possible effects of comorbid conditions, possible drug interactions, and other potential complexities. It involves both understanding the patient complaints and evaluating those complaints while ruling out the need for further testing or referrals to other medical specialties for underlying conditions that may be medically treatable. Audiologic decision-making refers to the responsibility for developing the correct conclusions, determining the appropriate treatment options, and for determining the process for presenting this information to the patient. Counseling and treatment involve not only the presentation of the treatment options, but also addressing any associated factors such as the psychological, emotional or vocational needs of the patient. Additionally, it addresses the degree to which a patient may need extra time or effort to fully understand the treatment plan.
Within each factor and level, there are multiple descriptors of services. As can be seen, assessment can revolve around the primary audiologic procedures (straightforward) or involve more procedures beyond that, typically performed in an audiologic evaluation (e.g., tinnitus matching, speech-in-noise, ultrahigh frequencies, and so on). When the assessment process evolves to these more involved procedures, then the charge process evolves to the complex level. Similarly, the audiologic decision-making and counseling and treatment categories move from simple to more involved depending on the complexity of the patient.
It is important to use the matrix consistently in determining the straightforward or complex level of service for each category. There needs to be consistency, both across patients and across clinicians, as to the level of service charged. Initially we decided that to move from the straightforward to the complex level at least two of the bullet points in the complex level need to be met. If only one element in the complex level was met, this was insufficient to categorize the service as complex. Similar to E&M codes, the associated documentation would have to support this decision.
The three factors of the audiologic process are not mutually exclusive. The provider is constantly making decisions, as well as continually altering assessment or treatment options, over the course of a patient interaction. However, the delivery process for audiology services generally can be considered to have three distinct parts—assessment, decision-making, and treatment—and therefore the matrix is designed to follow this process to the extent possible. Conversely, not all factors may be used within a single appointment with a patient. The audiologist seeing a patient for an audiologic evaluation who is determined to be essentially normal (no treatment necessary) may only utilize assessment and decision skills, and therefore no elements within the treatment and counseling columns will be applicable.
The factors and elements in Table 1 are for patients who are new to our practice. For established patients, additional elements are added (Table 2). Typically, established patients do not need the testing, decision-making, or treatment considerations that new patients require. Therefore, established patients are typically more straightforward, provided they are being seen as part of the process that relates to their initial reason to seek audiologic services. New patient elements are used whenever any of the following three criteria are met: (1) the patient is new to the practice, (2) it has been more than 1 year since the patient was last seen in the office, or (3) the patient presents with a new complaint, unrelated to the initial reason for being seen. Otherwise, the established patient elements are used for any follow-up visits.
Table 2. Additional Factors for Service Matrix When Patient Is an Established Patient.
| Assessment of Hearing Status and Hearing Handicap: Evaluating, Assessing, Diagnosing | Audiologic Decision-Making: Interpreting, Reviewing | Counseling and Treatment: Assisting, Instructing, Counseling | |
|---|---|---|---|
| Established patient—straightforward | Assessment of limited amount of data related to original complaint or a change in complaint | Perform basic reprogramming of hearing aid(s) | Basic counseling/instructions on adjustments made to hearing aids |
| Review of hearing recheck results | Perform listening checks | ||
| Assess the patient with new/changed psychological, educational, emotional, social and/or vocational impact of original complaints/change in complaints | Perform routine laboratory troubleshooting procedures such as retubing, replacing microphone covers, cleaning, etc. | ||
| Established patient—complex | Assessment of extensive amount of new complaints/change in complaints | Perform extensive reprogramming of devices | Extensive counseling/instruction on adjustments made to hearing aids and/or additional assistive devices |
| Review hearing recheck test results and/or evaluate with secondary procedure to measure extent of new complaints/change in complaints, such as tinnitus evaluation, speech-in-noise testing, ultrahigh frequencies, etc. | Perform hearing instrument test box measures and/or measurements | ||
| Evaluation using objective measures to assess change in hearing handicap and lifestyle complaints | Add additional assistive devices, such as streamers, remote products, etc. |
Following determination of the level of service within each category, the audiologist then references the charge structure displayed in Table 3. Please note that the charges displayed are not realistic but are used to provide examples of the differences across charge levels and patient type. As can be seen from the left-hand column, a combination of levels and categories is used to identify the patient charge for the service.
Table 3. Charges Associated with the Matrix of Audiology Services.
| Charge ($) | |||
|---|---|---|---|
| Level of Service | Rules | New Patient | Established Patient |
| 1 | Service in only one column, either level | 2.00 | 1.00 |
| 2 | Services in at least two columns, one at the straightforward level | 4.00 | 3.00 |
| 3 | Services in two columns, both are complex; or services in three columns, with only one complex | 6.00 | 4.00 |
| 4 | Services in all three columns, at least two are complex | 8.00 | 6.00 |
Note: Charges displayed are to provide examples of the relative charges for the patient status (new or established), and the complexity of the service. Actual charges are not provided.
Financial Considerations
Within our model, patients receive charges at almost every appointment. The initial evaluation may include the office visit charge as well as any charges for diagnostic procedures. In our model, the charges for any procedures continue to be billed to third parties while the office charges for the assessment; decision-making and/or treatments are expected to be paid at checkout. If a patient moves to a trial with a hearing aid, they are charged a flat rate for the process that includes the selection, fitting, and verification process and 60 days of follow-up from the fitting date. This is similar to the global period for surgical procedures whereby follow-up visits from the surgery are included in the surgical charge. The charge for the selection, fitting, and verification, as with all office visit charges, are not refundable. Only the separate product cost is refundable within the 60-day global period.
The charges for the devices are based, in part, on the cost of the products to the practice, as well as any costs that the practice incurs for overhead, maintaining inventory, shipping, or processing the devices. Similarly, any associated components, such as earmolds, streaming systems, or other devices also incur charges. The cost for the devices is refundable and in line with applicable state laws, but as the service charges have been separated, these are not refundable. Importantly, the charges for the devices are separated from the charges for professional audiology services. At the very least, the patient should perceive that the charges for the devices are significantly less than expected.
As noted previously, no charges are levied for follow-up visits that occur within the first 60 days following the initial fitting. The audiologist does have the discretion to expand this window for unusual circumstances. For visits that occur after the first 60 days, office visit charges apply with the amount charged based on the services provided as per the matrix. At this time, patients become established with the expectation that the services provided at follow-up appointments are directly related to the original reason the patient was seen in the office.
In this model, all new patients will receive an office visit charge for the consultation and, if appropriate, the corresponding CPT code charges for evaluation procedures. Even if a patient elects not to pursue amplification, there will be a charge. These patients utilized the knowledge, skill, and time of the audiologist. This skill set is unique to the audiology profession and occurs after years of college education and clinical experiences. Therefore, patients are tapping into a stream of expertise that requires compensation.
It should be noted that this model does not restrict the judgment of the audiologist from determining the appropriate level of charges, if any, for any given visit. Clearly there must be appropriate documentation to support the decision regarding the complexity of the case and the resulting charge, just like the E&M code guidelines require. However, the audiologist must also recognize that in some cases a second visit is necessary to resolve an issue. For example, if a part would need to be ordered for a hearing aid, then a second visit to complete a repair might be necessary. In this case, the audiologist has the latitude to not charge for one of the visits.
Long-Term Economics
One of the important questions is whether this model provides the same, or better, economic return to a practice as the traditional bundled model. The economic impact of the bundled model can be predicted based on the average or range of charges for hearing aid sales multiplied by the number of expected patients. This assumes that the charges rendered for products and services have been well thought out and account for overhead expenses and desired profitability. The number of patients purchasing products from preceding months can be used to predict anticipated patient flow over future months. For example, if the average charge per product/service with a bundled model is $1,000 per product, and one expects 15 patients per month to purchase products, then the revenue to the practice will be approximately $30,000 per month ($1,000 × 2 ears × 15 patients = $30,000).
In our model, as with many unbundled models, anticipated revenue is more complicated to predict. More assumptions about patient visits must be considered. First, the total number of patients visiting the practice must be considered as all patients will incur an office visit charge, regardless of whether they purchase a product or not. Second, patients undergoing a hearing aid trial but not purchasing a product must be accounted for, as the charges for these services must be considered in revenue projections. Finally, the number of return visits outside the 60-day window must be estimated. All of these factors have inherent variability that cannot be easily predicted. Thus, a true understanding of the economic impact of the model cannot be known until several years have passed.
Nonetheless, assumptions can be made and the economics of the model can be hypothetically predicted. For our predictions, we assumed 30 new patients per month, of whom 50% did not proceed beyond the initial evaluation stage. Of the 50% who proceeded to try hearing aids, two-thirds of the patients purchased two hearing aids. This means that of the 30 new patients per month, 20 hearing aids were dispensed. We did not account for returns. We also assumed that the number of follow-up visits was variable with 25% of the patients not returning for any follow-up visits after the global period in the first year, 25% returning for one visit, 25% requiring two follow-up visits, and 25% requiring three follow-up visits. For the initial and follow-up visits outside the 60-day window, we used the average office visit charge in our model.
When applying these assumptions, we found that our monthly revenues from the hearing aid dispensing business were nearly exactly the monthly revenues from our historical business model. Of course, the actual financial implications will not be known for several years as the services for all patients in the first year will not occur until at least 2 years out. This model does not account for services provided beyond the first year, which will naturally incur an office visit charge. Overall, the predicted revenues are in line with expectations from our historical model.
Advantages and Disadvantages
There are several advantages to this model. First, the up-front cost to patients may be reduced as product prices no longer need to include unlimited follow-up visits. This perception of pay as you go promotes fairness as patients are only paying for the services they actually use. For example, patient A returns for multiple follow-ups in the years following his hearing aid purchase and should not pay the same amount as patient B, who only requires follow-up within the global period. Revenues are distributed based on utilization. That is, the more a patient utilizes the services, the greater the number of charges they will incur. This may be a disadvantage if it discourages some people from utilizing services when they truly need them, but can be an advantage if it discourages people from overutilizing services when not necessary.
Small cost advantages are also gained as the tax paid on the products is lowered. Under the bundled model, state tax may be required on the entire charge if it appears the charge is for the device and not the services. Most unbundled models gain in this regard as the overall tax is lowered. This is a direct advantage to the patient as taxes are pass-through costs and have no impact on practice revenues.
Another important advantage to this model is that it assigns value to the expertise of the audiologist, rather than the time or appointment type. On an ongoing basis, the audiologist has to recognize the value of the effort in providing services and that all patient encounters have value. On a daily basis, the actual value of services provided can be calculated for an individual or a practice. Conversely, in a bundled model it may be more challenging to accurately value the productivity of the providers.
Like the general unbundling concept, one goal is to allow the patient to differentiate between the cost of the product and the cost for the services. Stated differently, the value of the services will begin to emerge from the cost of the product. The perception of the cost of the product will be lowered, even if the long-term costs are the same for some patients. In this regard, the opportunity to spread costs over time, rather than the large up-front costs, may be a perceived advantage to the patient. In fact, the more proficient the audiologist is at providing successful amplification initially, the real overall cost to the patient will be significantly lowered. In this regard, the value of amplification, a combination of the cost and the quality of the associated services, may increase as well (see Amlani, this issue).
There is also the opportunity for the audiologist or the audiology practice to emerge from a dependence on dispensing products as a primary economic focus. In this model, it does not matter where a patient purchases the product. Services are based on the expertise of the audiologist so the patients can purchase products online or can bring in products they purchased at other practices. Conversely, it does open the door for patients to choose products independent of the judgment or recommendations of the audiologist. Factors such as the level of technology, added features, or even style of the device are typically not well understood by patients, and therefore the devices purchased are inappropriate given the patient's hearing loss and lifestyle needs. It also requires that the audiologist have access to software for many manufacturers, including those that are typically available only to restricted distribution systems (e.g., Beltone products; Beltone, Chicago, IL).
Although we are testing this model in our hearing aid dispensing practice, the expectation is that the model could apply to almost any other aspect of audiologic practice. This charge model could be used for auditory processing evaluations, tinnitus evaluations, and even diagnostic evaluations. Although CPT-type charges account for performing and interpreting the procedure, the overarching process, including taking the patient history, decisions regarding which tests to perform, the complexity of combining test results into a single diagnosis, and the counseling that occurs beyond the reporting of the results of a test, is not currently charged in the third-party reimbursement process.
Next Steps
Feedback from patients is an important measure of the success of the model. We are collecting feedback after patient visits to identify their perception of the charge system. For many new patients, particularly those who have no experience in the acquisition of hearing aid products, there may not be a reference point (i.e., a bundled model) for comparison. In addition, their perceptions may change over time as they accumulate charges for visits over the 1 to 2 years postfitting.
The perception of the audiologists to this model is equally important. Many audiologists have worked in the bundled system for years, and thus the transition to charging for patient visits also can be unsettling. It requires a change in perspective, along with a change in the system for billing and charging. In some regards, the transition to this type of model requires a rethinking of all aspects of a patient encounter, from the initial phone call to scheduling an appointment through to the payment collection stage. Therefore engagement of the office and support staff is deemed critical to assist in the transition to this model.
Another important step in the process of transitioning to this model is addressing the charge structure associated with existing patients, particularly those who have come to expect visits with no charge. Collectively it was decided to honor a minimum of 1 year of continued free services, but to begin to inform patients that office visit charges will be implemented in the future. As we have not been using this model for a year at this point, the impact of this decision on patient satisfaction has not yet been determined.
As previously noted, the true results associated with this model will not be known for several years. For example, charges for new patients entering the system in month 11 will not have accumulated for 12 months after their first visit, at least. The transition of existing patients will take more than a year, depending on when they have future office visits. Moreover, the marketing effort that accompanies this model also will have an impact. Therefore the overall economic impact will take several years to discern.
The goal of differentially charging for expertise and knowledge of the audiologist is one method to describe the value of the audiologist to patient care. The model described herein is just that, a model. It is expected that elements, categories, or levels of the system might be added, deleted, changed, or debated. The system may have to be adjusted based on changes in reimbursement, coverage for hearing aids by third parties, or transformation to systems associated with the Affordable Care Act. However, the necessity to demonstrate the value of the service will be important in all these circumstances.
References
- 1.Sable-Antry S. Creating value in a changing health-care landscape. Audiol Today. 2015;27(1):40–45. [Google Scholar]
- 2.Messersmith J J, Jorgensen L. Beyond the individual practice: ACA impact on state insurance mandates for audiological care. Audiol Today. 2015;27(1):55–57. [Google Scholar]
- 3.Freeman B A. Itemized value pricing: responding to changes in the health-care system. Audiol Today. 2012;24(2):48–54. [Google Scholar]
- 4.Cropp I Why do hearing aids cost so much? AARP 2014. Available at: www.aarp.org/health/conditions-treatments/info-05-2011/hearing-aids-cost.2.html. Available July 10, 2015
- 5.Timm E. Napierville, IL: Phonak; 2011. Hearing Industry Benchmark Study Outcomes. [Google Scholar]
- 6.Freeman B A. The future of hearing care: what survival lessons can we learn from other professions? Audiol Today. 2014;26(2):31–36. [Google Scholar]
- 7.Franks J R, Beckmann N J. Rejection of hearing aids: attitudes of a geriatric sample. Ear Hear. 1985;6(3):161–166. doi: 10.1097/00003446-198505000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Newman C W, Hug G A, Wharton J A, Jacobson G P. The influence of hearing aid cost on perceived benefit in older adults. Ear Hear. 1993;14(4):285–289. doi: 10.1097/00003446-199308000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Stika C J, Ross M. Hearing aid services and satisfaction: the consumer viewpoint. ADA Feedback. 2006;17(2):26–31. [Google Scholar]
- 10.American Academy of Audiology A guide to itemizing your professional services. Available at: http//www.audiology.org/sites/default/files/20141001_AAA_Guide2ItemizingUrProfeServices.pdf. Accessed March 1, 2016


