Abstract
A 12-year-old male with status asthmaticus developed subcutaneous emphysema and pneumomediastinum. He was transferred to our unit, where he received noninvasive ventilation (NIV). This respiratory support technique is not an absolute contraindication in these cases. After 2 h on NIV, he worsened sharply and the subcutaneous emphysema got bigger suddenly. He needed invasive ventilation for 5 days. Final outcome was satisfactory. This case illustrates that it is mandatory to keep a high level of vigilance when using NIV in patients with air leaks.
Keywords: Asthma, noninvasive ventilation, pneumomediastinum, subcutaneous emphysema
Introduction
Subcutaneous emphysema is caused by increased intraaveolar or intrabronchiolar pressure with an extrapleural outflow of air. Pneumomediastinum is also due to increased intra-alveolar pressure, which can occur with barotrauma, coughing, or asthma exacerbation.[1] It is more common in children under 7 years.[2,3] During an asthma attack, the incidence is estimated at one in 20,000 patients.[4] There is some controversy about the application of NIV in cases of air leak. We describe the case of a patient with asthma and associated pneumomediastinum and subcutaneous emphysema who showed an abrupt worsening after starting with NIV.
Case Report
Male patient, 12-year-old, with a history of asthma from the age of 2 years. He was treated with inhaled corticosteroids and long-acting beta agonists, without maintenance therapy during the previous year. He was diagnosed with idiopathic thrombocytopenic purpura at the age of 11. He was admitted to a district hospital with moderate respiratory distress. He was treated with intravenous corticosteroids and nebulized salbutamol and ipratropium bromide. Respiratory distress worsened sharply; he had swelling and crepitus at his neck. Chest X-ray confirmed the presence of subcutaneous emphysema and pneumomediastinum [Figure 1]. He was admitted in the Pediatric Intensive Care Unit (PICU) and connected to NIV. Two hours after NIV initiation his clinical condition worsened abruptly; physical examination revealed neck enlargement of up to two inches thick which compromised airway patency, on auscultation he had a silent chest. Blood gas analysis showed very severe respiratory acidosis (pH 7.10, pCO2 98.8 mmHg). Thorax X-ray and computed tomography (CT) scan showed the presence of subcutaneous emphysema dissecting the muscle compartments of cervical regions, supraclavicular, and costal wall and also showed a pneumomediastinum toward the minor fissure and around the bronchial structures [Figure 2]. The patient required invasive mechanical ventilation (IMV) for 5 days. At the beginning of IMV, he presented air-trapping, showing and intrinsic positive-end expiratory pressure of 5 mmHg. Volume-controlled ventilation was used for the first 4 days with a tidal volume of 6 ml/kg. The 5th day ventilation mode was changed to pressure support. Subcutaneous emphysema extended along his chest, abdominal wall and groins. After he was extubated, the outcome was satisfactory, but the signs of subcutaneous emphysema persisted a week after admission, with subsequent resolution.
Figure 1.

Chest X-ray examination showed pneumomediastinum and subcutaneous emphysema
Figure 2.
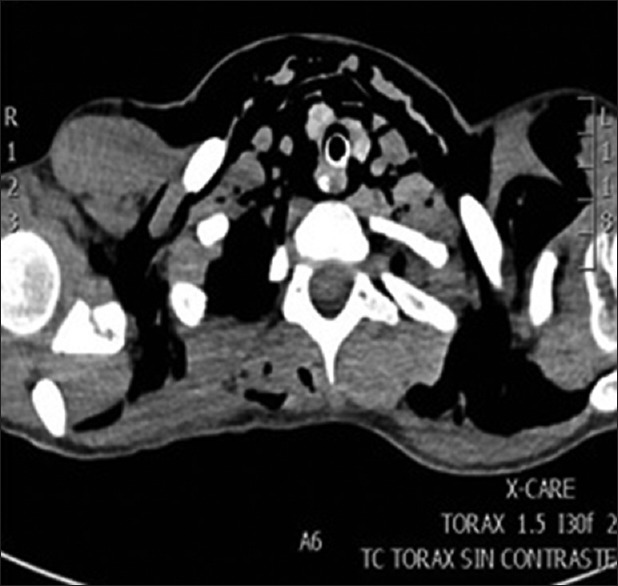
Computed tomography thorax of this patient demonstrating pneumomediastinum and subcutaneous emphysema blowing out of muscles and pneumomediastinum. The chest X-ray of Figure 1 is before the intubation, and the computed tomography scan is after the intubation
Discussion
Subcutaneous emphysema and pneumomediastinum are rare complications of status asthmaticus. If they are present, we have to foresee a sharp deterioration of the patient as it happened in our case. The use of IMV in the asthmatic patient is very uncommon nowadays due to the frequent use of NIV. At present, <2% of patients who were admitted to intensive care for asthma exacerbation require IMV.[5] Our patient required IMV because the air leak compromised airway patency. Risk factors for barotrauma in this patient were acute respiratory distress, emphysema, severe asthma exacerbation, young age, and air-trapping. NIV could exacerbate air leak resulting in intense cervical subcutaneous emphysema which almost impeded ventilation (silent chest) probably due to compromised airway. It is mandatory to monitor closely patients with air leak (pneumomediastinum in our case) and NIV;[6] especially if it is associated with clinical deterioration or CO2 retention. Literature to date describes an estimated incidence between 5% and 7% of pneumothorax or pneumomediastinum using NIV.[7,8,9] Controversy exists within the consideration of pneumomediastinum as an absolute contraindication in NIV.[10,11,12,13,14] Some authors[10,11,12,13,14] consider NIV as an absolute contraindication whereas others establish that it is a relative contraindication. Therefore, as our case illustrated it is essential to keep a high level of vigilance when using NIV in patients with air leak syndrome. It is necessary to detect changes in mental status or inability to maintain adequate ventilation and oxygenation as soon as possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
The authors gratefully acknowledge the assistance of the PICU medical and nursing staff of Hospital Universitario Central de Asturias.
Footnotes
Financial support and sponsorship Nil.
Conflicts of interest There are no conflicts of interest.
References
- 1.Zhang XY, Zhang WX, Sheng AQ, Zhang HL, Li CC. Diagnosis and prognosis of spontaneous pneumomediastinum in eighteen children. Zhonghua Er Ke Za Zhi. 2013;51:849–51. [PubMed] [Google Scholar]
- 2.Meireles J, Neves S, Castro A, França M. Spontaneous pneumomediastinum revisited. Respir Med CME. 2011;4:181–8. [Google Scholar]
- 3.Reed JA, Larson KE, Hsu BS. Spontaneous pneumomediastinum with subcutaneous emphysema: Report of two pediatric cases. S D Med. 2013;66:89, 91–3. [PubMed] [Google Scholar]
- 4.Giuliani S, Franklin A, Pierce J, Ford H, Grikscheit TC. Massive subcutaneous emphysema, pneumomediastinum, and pneumopericardium in children. J Pediatr Surg. 2010;45:647–9. doi: 10.1016/j.jpedsurg.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 5.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in admissions for pediatric status asthmaticus in New Jersey over a 15-year period. Pediatrics. 2010;126:e904–11. doi: 10.1542/peds.2009-3239. [DOI] [PubMed] [Google Scholar]
- 6.Carroll CL, Zucker AR. Barotrauma not related to type of positive pressure ventilation during severe asthma exacerbations in children. J Asthma. 2008;45:421–4. doi: 10.1080/02770900802085451. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs H, Schoss J, Mendler MR, Lindner W, Hopfner R, Schulz A, et al. The cause of acute respiratory failure predicts the outcome of noninvasive ventilation in immunocompromised children. Klin Padiatr. 2015;227:322–8. doi: 10.1055/s-0034-1395692. [DOI] [PubMed] [Google Scholar]
- 8.Ruggeri P, Girbino G. Fatal pneumomediastinum associated with use of noninvasive mechanical ventilation. Respirol Case Rep. 2014;2:126–8. doi: 10.1002/rcr2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–9. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Francisco PA, Pamela SF, Gustavo PT, Carolina CO, Daniel ZA. Asistencia ventilatoria no invasiva en pediatría. Rev Chil Pediatr. 2008;79:580–92. [Google Scholar]
- 11.Medina A, Pons-Òdena M, Martinón-Torres F, editors. Noninvasive ventilation in pediatrics. 3rd ed. Madrid: Ergon; 2015. [Google Scholar]
- 12.Akingbola OA, Hopkins RL. Pediatric noninvasive positive pressure ventilation. Pediatr Crit Care Med. 2001;2:164–9. doi: 10.1097/00130478-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Caples SM, Gay PC. Noninvasive positive pressure ventilation in the intensive care unit: A concise review. Crit Care Med. 2005;33:2651–8. doi: 10.1097/01.ccm.0000186768.61570.69. [DOI] [PubMed] [Google Scholar]
- 14.Essouri S, Chevret L, Durand P, Haas V, Fauroux B, Devictor D. Noninvasive positive pressure ventilation: Five years of experience in a pediatric intensive care unit. Pediatr Crit Care Med. 2006;7:329–34. doi: 10.1097/01.PCC.0000225089.21176.0B. [DOI] [PubMed] [Google Scholar]


