Abstract
Acute fibrinous and organizing pneumonia (AFOP) is a rare disease characterized by bilateral basilar infiltrates and histological findings of organizing pneumonia and intra-alveolar fibrin in the form of “fibrin balls.” Here, we report a 43-year-old female with complaints of fever, dry cough, and shortness of breath with hypoxemia. High-resolution computed tomography thorax revealed diffuse confluent consolidation in bilateral lung zones. Bronchoscopy and transbronchial biopsy revealed features of AFOP. With prednisolone treatment, there was an improvement in her condition. AFOP is a rare disease and should be taken into consideration and differential diagnosis of severe acute pneumonias with no significant comorbidities.
Keywords: Acute fribinous, organizing pneumonia, nonresolving pneumonia, pneumonia
Introduction
Acute fibrinous and organizing pneumonia (AFOP) was first described by Beasley et al. in 2002 as a condition characterized by alveolar damage, eosinophilic pneumonia, and organizing pneumonia. Totally <120 cases have been published in literature, including this case. The features that distinguish it histologically are the presence of intra-alveolar fibrin balls, absence of usual hyaline membranes and eosinophils and many foci of fibroblastic activity.[1] Early diagnosis is important because it can be progressive and fatal. It has been described in almost all age groups with associations including autoimmune disease and connective tissue, drugs, occupational, and environmental exposures and other infectious agents. They are usually two forms of this illness, a severe form which leads to rapid respiratory failure and a subacute form which has a much better prognosis.[1] There is no specific treatment though immunosuppressant and steroids produce good results in patients with sub-acute AFOP. The chest radiograph findings of AFOP are almost identical to those seen in cryptogenic organizing pneumonia, consistent with migratory, patchy, diffuse, alveolar opacities with bilateral, and peripheral distributions.[1,2,3,4,5]
Case Report
A 42-year-old female was admitted with complaints of dry cough of 5 days, high-grade fever since 15 days, generalized malaise and progressive worsening shortness of breath since 5 days.
She was a nonsmoker with no history of any comorbid illness in the past. No known chemicals, fumes or occupational or allergen exposure. Upon examination, she was dyspneic, blood pressure of 110/70 mmHg and had fever of 103 F. She had a respiratory rate of 32/min, heart rate of 120 beats/min. She had no icterus, edema, clubbing, rash, skin lesions, cervical lymphadenopathy, or joint swelling. Her oxygen saturation was 74% on room air. Upon auscultation, there were fine inspiratory crepitations. Other system examinations were unremarkable.
Her arterial blood gas (ABG) analysis revealed pH of 7.47, pCO2 of 41 mmHg, and pO2 of 39 mmHg. Her leukocyte count was quite high at 33000 × 103 /μL. Her sputum for acid fast-Bacilli and Gram's stain was negative. Chest radiographic findings showed inhomogeneous bilateral opacification in lower lung zones. The rest of the laboratory tests, including liver function test, kidney function test, coagulation profile, urine examination, etc., were normal.
Two-dimensional echocardiography, proBNP, and electrocardiogram were normal. Work up of anti-nuclear antibodies, angiotensin converting enzyme, DsDNA antibodies, antinuclear and cytoplasmic antibodies, rheumatoid arthritis factor, extractable nuclear antigen profile, and anti-phospholipid anti bodies were negative. Blood and urine cultures were sterile. She was initially treated with noninvasive ventilation, oxygen therapy, antibiotics such as combination antibiotic regimen with pipercillin-tazobactam with and clarithromycin.
High-resolution computed tomography (HRCT) thorax revealed bilateral diffuse confluent consolidation in lower lung zones [Figure 1a–c]. Bronchoscopy followed by bronchoalveolar lavage (BAL) was performed (Gene XPERT real-time PCR). Molecular diagnostic test for Tuberculosis was negative; BAL galactomannan was insignificant. BAL cultures were negative. Transbronchial lung biopsy was performed from the right lower lobe, biopsy report of which came out to be AFOP [Figure 1d and e]. She was treated with 40 mg prednisolone twice daily along with bronchodilators and oxygen therapy. Lung opacities decreased significantly after 3 days of the steroid treatment. Her ABG also improved significantly with pO2 at 92 mmHg and her saturation at 95%. She was initially on high flow oxygen mask which came down to minimum level and eventually she did not require any oxygen therapy after 5 days of steroid therapy initiation. The patient was discharged after about 10 days of hospitalization. Her review HRCT thorax showed significant improvement. She is currently on prednisolone and on regular follow-up.
Figure 1.
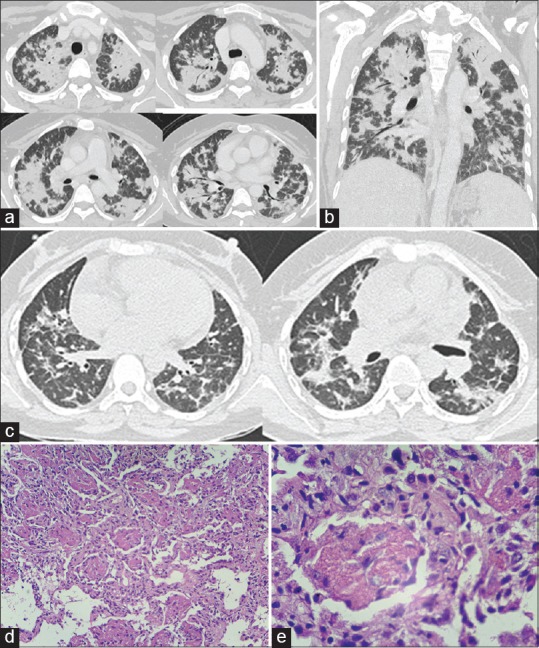
(a) Axial and (b) cornal computed tomography through lungs: Geographical distribution of widespread consolidation with ground glass opacities and septal thickening in both lungs. (c) Axial computed tomography taken after 15 days after treatment: resolution of large component of organizing consolidation with residual ground glass opacities and mild septal thickening. (d and e) Intra-alveolar fibrin in the form of “Fibrin balls” without formation of hyaline membranes (H and E, ×100)
Discussion
AFOP was first reported in detail in 17 case reports in 2002.[1] PubMed search revealed 23 cases reported so far. AFOP has been reported in all age groups with average age being 62 years originally described by Beasley et al. Males are more commonly affected.[1] It has been reported that AFOP may occur as an idiopathic variety or in association with clinical conditions, including collagen vascular diseases, drug reactions, occupational or environmental exposures, as well as various infections. In addition, several cases have no origin cause or association.[1,2,3] Retrospective follow-up of these patients shows two varieties of progression. A subacute variety and a severe variety which usually leads to respiratory failure and the prognosis of the severe variety is not promising.[1] On average, severe form of AFOP causes death within 29 days of onset.[1] However, the subacute variety has a much better prognosis and treatment. Our patient suffered from this variety. This variety seems to resemble cryptogenic organizing pneumonia (COP) in terms of prognosis and recovery following corticosteroid treatment. AFOP has been described with many other conditions in the past while twelve reported cases were idiopathic. Therefore, there could be an association between autoimmune disease and AFOP.[6,7]
In our case, the clinical presentation of the patient showed typical signs of COP. There was no evidence of malignancy or any other factors known to be related with pneumonia. However, lung biopsy revealed that the patient has unusual histological pattern that was identified as AFOP. Nevertheless, it is important to note that sub-acute forms of this disease seem to be mistaken for COP. Therefore, histological diagnosis is essential for distinguishing the two through CT-guided or bronchoscopic biopsy. The most commonly used methods to obtain a tissue sample include video-assisted thoracoscopic biopsy and a CT-guided biopsy. Transbronchial biopsy as in our case has also been rarely used so far.[1,3,6,7,8,9,10,11,12,13] Diagnosis of AFOP in Indian case reports has been achieved through CT guided biopsy followed by treatment of the disease by prednisolone.[12]
Numerous treatment modalities have been used for AFOP. The most common and successful has been corticosteroids. Other agents successfully used include cyclophosphamide, azathioprine, and mechanical ventilation.[12,13] Different corticosteroid dosages have been used. Our patient was treated with prednisolone 40 mg twice daily. There was a dramatic and remarkable clinical response. She required intensive care support for 5 days eventually being discharged home after 10 days of hospitalization.
Conclusion
By this study, we suggest that AFOP should be taken into consideration and differential diagnosis of severe acute pneumonias with no significant co-morbidities. Diagnosis is mostly biopsy proven, and treatment through corticosteroids is quite promising. Patients having the subacute variety of the disease have excellent prognosis with corticosteroids.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- 1.Beasley MB, Franks TJ, Galvin JR, Gochuico B, Travis WD. Acute fibrinous and organizing pneumonia: A histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med. 2002;126:1064–70. doi: 10.5858/2002-126-1064-AFAOP. [DOI] [PubMed] [Google Scholar]
- 2.Cordier JF. Cryptogenic organising pneumonia. Eur Respir J. 2006;28:422–46. doi: 10.1183/09031936.06.00013505. [DOI] [PubMed] [Google Scholar]
- 3.Damas C, Morais A, Moura CS, Marques A. Acute fibrinous and organizing pneumonia. Rev Port Pneumol. 2006;12:615–20. [PubMed] [Google Scholar]
- 4.Voloudaki AE, Bouros DE, Froudarakis ME, Datseris GE, Apostolaki EG, Gourtsoyiannis NC. Crescentic and ring-shaped opacities. CT features in two cases of bronchiolitis obliterans organizing pneumonia (BOOP) Acta Radiol. 1996;37:889–92. doi: 10.1177/02841851960373P289. [DOI] [PubMed] [Google Scholar]
- 5.Kofteridis DP, Bouros DE, Vamvakas LN, Stefanaki KS, Voludaki AE, Barbounakis EM, et al. Pneumothorax complicating fatal bronchiolitis obliterans organizing pneumonia. Respiration. 1999;66:266–8. doi: 10.1159/000029371. [DOI] [PubMed] [Google Scholar]
- 6.Labarinas S, Gumy-Pause F, Rougemont AL, Baerlocher G, Leibundgut EO, Porret N, et al. Is acute fibrinous and organizing pneumonia the expression of immune dysregulation? J Pediatr Hematol Oncol. 2013;35:139–43. doi: 10.1097/MPH.0b013e31827e5782. [DOI] [PubMed] [Google Scholar]
- 7.Valim V, Rocha RH, Couto RB, Paixão TS, Serrano EV. Acute fibrinous and organizing pneumonia and undifferentiated connective tissue disease: A case report. Case Rep Rheumatol. 2012;2012:549298. doi: 10.1155/2012/549298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hariri LP, Unizony S, Stone J, Mino-Kenudson M, Sharma A, Matsubara O, et al. Acute fibrinous and organizing pneumonia in systemic lupus erythematosus: A case report and review of the literature. Pathol Int. 2010;60:755–9. doi: 10.1111/j.1440-1827.2010.02586.x. [DOI] [PubMed] [Google Scholar]
- 9.Sauter JL, Butnor KJ. Expanding the spectrum of pulmonary histopathological manifestations of anti-synthetase syndrome: Anti-EJ-associated acute fibrinous and organizing pneumonia. Histopathology. 2014;65:581–2. doi: 10.1111/his.12420. [DOI] [PubMed] [Google Scholar]
- 10.Guimarães C, Sanches I, Ferreira C. Acute fibrinous and organising pneumonia. BMJ Case Rep 2012. 2012:pii: Bcr0120113689. doi: 10.1136/bcr.01.2011.3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhatti S, Hakeem A, Torrealba J, McMahon JP, Meyer KC. Severe acute fibrinous and organizing pneumonia (AFOP) causing ventilatory failure: Successful treatment with mycophenolate mofetil and corticosteroids. Respir Med. 2009;103:1764–7. doi: 10.1016/j.rmed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Mittal V, Kulshrestha R, Arya A, Bajaj P. Acute fibrinous and organising pneumonia presenting as complete lung consolidation. Singapore Med J. 2011;52:e88–90. [PubMed] [Google Scholar]
- 13.Kuza C, Matheos T, Kathman D, Heard SO. Life after acute fibrinous and organizing pneumonia: A case report of a patient 30 months after diagnosis and review of the literature. J Crit Care. 2016;31:255–61. doi: 10.1016/j.jcrc.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


