Abstract
Aims
The aim of this study was to compare transscleral resection technique performed without hypotensive anaesthesia (TSRWH) with iodine-125 brachytherapy (IBT) in the treatment of choroidal melanoma.
Patients and methods
This was a retrospective surgical cohort study. Nineteen eyes treated with TSRWH were matched with 53 eyes treated with IBT according to: tumour size, distance to fovea, distance to optic nerve, and follow-up time. Best-corrected visual acuity (BCVA), local recurrence, secondary enucleation, metastasis, overall and specific survival, and complications were evaluated.
Results
Patients treated with TSRWH had significantly better BCVA than those treated with IBT. The local recurrence risk was significantly higher when ciliary body was involved (HR=11.4, 95% CI 2.24–49.7, P=0.04). Metastatic disease was observed in 14 of 53 patients (26.4%) in the IBT group vs 3 patients (15.8%) in the TSRWH group (P=0.531). Multivariate analysis showed that iris involvement (HR=16.0, 95% CI 4.2–170.2, P=0.033) and large tumour (HR=2.3, 95% CI 1.2–4.8, P=0.04) increased the probability of metastasis. During follow-up, six patients (11.3%) in IBT group died vs two (10.5%) in the TSRWH group (P≥0.999). Nine patients required secondary enucleation: 5 (9.4%) in the IBT group vs 4 (21.1%) in the TSRWH group (P=0.231). The most common complications in IBT group were radiation-induced retinopathy (45.3%), neovascular glaucoma (28.3%), and macular oedema (24.5%), whereas rhegmatogenous retinal detachment (21.1%), ocular hypertension (21.1%), and submacular haemorrhage (15.8%) were the most frequent complications after TSRWH.
Conclusion
TSRWH is a technically challenging procedure. However, when performed successfully, this technique achieves better preservation of visual acuity than IBT and without the limitations inherent in hypotensive anaesthesia.
Introduction
Uveal melanoma is the most common primary intraocular tumour in adults.1, 2 The most widely used eye-preserving treatment is brachytherapy, primarily iodine brachytherapy (IBT). Large tumour size and proximity to the optic nerve or fovea are associated with the loss of vision owing to radiation-induced retinopathy, optic neuropathy, maculopathy, and secondary glaucoma.3, 4, 5, 6
Transscleral resection (TSR) has been described as a primary procedure to treat uveal melanoma in patients who are not expected to have good outcomes after conventional brachytherapy.7, 8, 9 Some studies7, 8, 9 suggest that TSR may achieve better vision preservation than IBT while avoiding many of the complications associated with brachytherapy.
In conventional TSR, systolic blood pressure is reduced to 40–60 mm Hg for ~60 min to prevent excessive bleeding. Patients with cardiovascular risk factors for hypotensive anaesthesia and older patients are not suitable for this surgery.10
In the study reported here, we compare transscleral resection technique performed without hypotensive anaesthesia (TSRWH) with IBT in terms of visual acuity (VA), local recurrence, metastasis, survival (overall and specific), secondary enucleation, and complications.
Materials and methods
This study is based on a retrospective surgical cohort of patients diagnosed with uveal melanoma and treated at our hospital. From a cohort of 556 eyes (556 patients), 72 eyes (72 patients) with choroidal melanoma were selected for the present study. All patients were treated at the Ocular Oncology Unit of the Ophthalmology Department of Bellvitge University Hospital and at the Brachytherapy Department of the Catalan Institute of Oncology (ICO in Spanish).
We selected 19 consecutive choroidal melanoma patients who had undergone TSRWH and matched these to 53 patients treated with IBT alone. The matching was performed according to tumour size, distance to fovea, distance to optic nerve, and duration of follow-up. Patient confidentiality was protected by national data confidentiality laws. This study was approved by the clinical research ethics committee of Bellvitge University Hospital (Reference: PR176/13) and adheres to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects in accordance with our institutional guidelines. The clinical and demographic characteristics of enroled patients are presented in Tables 1 and 2.
Table 1. Clinical and demographic characteristics of enroled patients (quantitative variables).
| IBT (n=53); mean or median | SD (range) or IQR (range) | TSRWH (n=19); mean or median | SD (range) or IQR (range) | P-valuea | |
|---|---|---|---|---|---|
| Age (years)b | 66.17 | 25.67 (29.5–85.4) | 57.25 | 16.35 (32.1–73.3) | 0.178 |
| Visual acuity (Snellen chart)b | 20/50 | 20/40 (20/20 000–20/20) | 20/200 | 20/36 (20/20 000–20/20) | 0.029 |
| Visual acuity (LogMAR)b | 0.4 | 0.5 (0–3.0) | 1.0 | 1.08 (0–3.0) | 0.025 |
| Height (mm)b | 9.0 | 2.0 (6.0–11.0) | 11.0 | 2.0 (4.0–12.0) | <0.001 |
| Tumour horizontal base (mm)b | 15.0 | 3.0 (8.0–20.0) | 14.0 | 4.0 (11.0–20.0) | 0.312 |
| Tumour vertical base (mm)c | 14.0 | 2.76 (7.0–20.0) | 13.0 | 2.16 (9.0–19.0) | 0.317 |
| Largest tumour diameter (mm)c | 15.5 | 2.59 (8.0–20.0) | 14.7 | 2.46 (11.0–20.0) | 0.285 |
| Distance from posterior tumour margin to fovea (mm)b | 9.0 | 6.0 (6.0–18.0) | 12.0 | 4.0 (6.0–18.0) | 0.181 |
| Distance from posterior tumour margin to optic nerve (mm)b | 9.0 | 5.5 (3.0–18.0) | 10.0 | 7.0 (4.0–15.0) | 0.188 |
Abbreviations: IBT, iodine-125 brachytherapy; IQR, interquartile range; TSRWH, transscleral resection performed without hypotensive anaesthesia.
P-values were obtained by Mann–Whitney's U-test (age, visual acuity, height, tumour horizontal base, distance from posterior tumour margin to fovea, and distance from posterior tumour margin to optic nerve) or Student's t-test (tumour vertical base and largest tumour diameter) as needed.
Median.
Mean. The bold values indicate P<0.05.
Table 2. Clinical and demographic characteristics of enroled patients (qualitative variables).
|
IBT (n=53) |
TSRWH (n=19) |
P-valuea | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | |||||
| Women | 28 | 52.8 | 10 | 52.6 | 0.988 |
| Men | 25 | 47.2 | 9 | 47.4 | |
| Eye | |||||
| Right | 24 | 45.3 | 9 | 47.4 | 0.876 |
| Left | 29 | 54.7 | 10 | 52.6 | |
| COMSb | |||||
| Medium | 11 | 20.8 | 3 | 15.8 | 0.747 |
| Large | 42 | 79.2 | 16 | 84.2 | |
| TNMc | |||||
| T2 | 5 | 9.4 | 3 | 15.8 | 0.736 |
| T3 | 41 | 77.4 | 14 | 73.7 | |
| T4 | 7 | 13.2 | 2 | 10.5 | |
| Ciliary body involvement | |||||
| No | 40 | 75.5 | 13 | 68.4 | 0.550 |
| Yes | 13 | 24.5 | 6 | 31.6 | |
| Iris involvement | |||||
| No | 50 | 94.3 | 16 | 84.2 | 0.184 |
| Yes | 3 | 5.7 | 3 | 15.8 | |
| Angle involvement | |||||
| No | 51 | 96.2 | 17 | 89.5 | 0.283 |
| Yes | 2 | 3.8 | 2 | 10.5 | |
| Exudative RD | |||||
| No | 17 | 32.1 | 6 | 31.6 | 0.968 |
| Yes | 36 | 67.9 | 13 | 68.4 | |
| Visual acuity | |||||
| <20/200 | 6 | 11.3 | 6 | 31.6 | 0.069 |
| ≥20/200 | 47 | 88.7 | 13 | 68.4 | |
| RBM | |||||
| No | 41 | 77.4 | 10 | 52.6 | 0.042 |
| Yes | 12 | 22.6 | 9 | 47.4 | |
Abbreviations: IBT, iodine-125 brachytherapy; RBM, rupture of Bruch's membrane; RD, retinal detachment; TSRWH, transscleral resection performed without hypotensive anaesthesia.
P-values were obtained by χ2-test (sex, eye, ciliary body involvement, TNM, exudative retinal detachment, and RBM) or Fisher's exact test (COMS, iris, angle involvement, and visual acuity) as needed.
According to COMS classification.
According to the ‘T' category of the 7th edition of AJCC staging. The bold value indicates P<0.05.
Preoperative assessment and follow-up
Preoperative assessments included the best-corrected VA (BCVA; evaluated with Snellen-20 feet and the logarithm of the minimum angle of resolution (LogMAR)), complete slit lamp exploration, indirect ophthalmoscopy, A- and B-scan ultrasound, and fundus photography. Tumour height, tumour horizontal base, tumour vertical base, largest basal diameter, tumour margins, and distances from the posterior margin to the fovea and to the optic disc were evaluated. We also assessed for involvement of the ciliary body, iris, and anterior chamber angle, as well as the presence of exudative retinal detachment and vitreous haemorrhage. The tumour size was classified according to the criteria established by the Collaborative Ocular Melanoma Study (COMS)11 classification system and according to the tumour size categories published in the 7th edition of the American Joint Committee of Cancer12 staging system. All patients were evaluated and monitored for metastatic disease, including the following tests: serum biochemistry with liver function tests, liver ultrasound, chest radiography, and examination by an oncologist.
Iodine-125 brachytherapy
All brachytherapy procedures were performed by the same surgeon (JMC) using iodine-125 COMS-type plaques at the Brachytherapy Department of the ICO. Transscleral illumination was used to assess tumour margins with the patient under local anaesthesia and sedation. In all cases, a minimum safety margin of 2 mm was used. Patients were hospitalised at the ICO during the course of brachytherapy treatment.
Initial follow-up was performed ~15 days after the procedure and at 3 months. Follow-up assessment, including surveillance for metastasis, was performed every 6 months for the first 5 years and annually thereafter.
Eyes treated with IBT received a median dose to the tumour apex of 85 Gy (range, 57.8–105.9 Gy) within a median of 120 h (range, 60–140 h) at a median dose rate of 82 cGy/h (range, 50–197.8 cGy/h). The median doses delivered to the optic disc and fovea were 35.7 Gy (range, 23.8–196.3 Gy) and 40 Gy (range, 0–220 Gy), respectively.
Combined TSR
All TSRWH procedures were performed by the same surgeon (JMC) at Bellvitge University Hospital. This technique involves three main steps: (1) standard phacoemulsification with IOL implant followed by (2) transescleral tumour resection, and finally (3) a pars plana vitrectomy with silicone oil filling.
Phacoemulsification cataract surgery
In all cases, the lens was removed by phacoemulsification through a small incision (up to 3 mm) before tumour resection, and a 3-piece foldable acrylic IOL was implanted.
Transscleral local resection
TSR has been described previously,10 but we have introduced some important modifications to this procedure. The most notable being the avoidance of hypotensive anaesthesia during surgery: instead, systolic blood pressure was maintained between 100 and 110 mm Hg during the surgical intervention. Episcleral blood vessels were cauterised using bipolar diathermy to minimise any scleral bleeding. The tumour margins were identified by transillumination and marked on the sclera with a felt-tipped pen. A polygonal posterior-hinged lamellar scleral flap around the tumour was created, of ~80% of the scleral thickness, taking free apparent tumour margins by about 3 mm. To avoid haemorrhage, any vortex veins overlying the scleral flap were cauterised before being divided, applying bipolar diathermy both extraocularly and to the intrascleral portion of the vein after cautiously exposing as much of the vessel as possible. The eye was decompressed by performing a limited vitrectomy with a vitrector using illumination from surgical microscope. This step improves the access to the posterior uvea and facilitates local excision by reducing retinal bulging through the scleral window. Once a complete dissection of lamellar flap was created, incisions were made in the deep sclera about 2 mm inside the superficial scleral flap using a 15° microsurgical knife. This scleral incision was extended around the tumour with a blunt curved corneal left and right hand Castroviejo scissors. The deep scleral incision was kept inside the superficial scleral incisions, to create a stepped wound edge, which facilitates subsequent closure. The uveal tract was exposed (a different colour between tumour and normal choroid could be seen) and cauterised externally using an intraocular laser probe (532 nm; 400–600 mW and continuous mode) in order to reduce the risk of haemorrhage. Subsequently, the tumour was excised with the deep scleral lamella and a frill of normal uvea using again curved corneal left and right hand Castroviejo scissors. Care was taken to preserve the underlying retina, or in case of ciliary tumours we conserve as much of the ciliary epithelium as possible. Interrupted 8–0 nylon sutures were placed at the corners of the polygonal scleral flap, and thereafter along all the margins of it. The conjunctiva was closed with 7–0-braided polyglactin sutures.
In all cases, pars plana vitrectomy (20–23-gauge) was performed with a panoramic viewing system. Core vitrectomy, haemorrhage removal (when necessary), and posterior hyaloid dissection were performed. In three cases, we administered a subretinal recombinant tissue plasminogen-activator injection owing to submacular haemorrhage. Laser endophotocoagulation (settings 0.2 s, 200–300 mW) was performed at the margins of the surgical resection (coloboma). Laser retinopexy was followed by fluid-air exchange and silicone oil injection (1000–5000 cs). Postoperatively, patients received prophylactic oral steroids and antibiotics, as well as topical antibiotics, steroids, and mydriatics. The silicone oil was removed between 4 and 6 months after surgery.
Patients were instructed to maintain a face-down position for 1 week after surgery. Adjuvant IBT (75 Gy to a depth of 2–3 mm) was administered in 17 of 19 eyes after the TSR procedure. Postoperative follow-up was performed at 1 day, 1 week, 1 month, 3 months, and 6 months. Thereafter, follow-up, including surveillance for metastasis, was performed every 6 months for the first 5 years.
Outcome variables
Outcome variables evaluated were (1) BCVA; (2) local recurrence; (3) metastasis; (4) overall survival (OS) and cause-specific survival (CSS); (5) secondary enucleation, and complications (ie, radiation-induced retinopathy, retinal detachment, glaucoma, corneal oedema, submacular haemorrhage, vitreous haemorrhage, and macular oedema).
Statistical analysis
Patient clinical and demographic characteristics and follow-up data were obtained from a database file, and subsequently exported to IBM SPSS Statistics v 20.0 for Windows (SPSS, Chicago, IL, USA). Descriptive analysis was performed, and measures of the central tendency (mean and median) and dispersion (standard deviation, range, interquartile range) were determined depending on the distribution of the variable (Kolmogorov–Smirnov or Shapiro–Wilk tests). For quantitative variables, the Student's t-test or the Mann–Whitney's U-test were used, as appropriate, to compare baseline and after treatment characteristics resulting from TSRWH or iodine-125 brachytherapy. To evaluate differences in proportions, the χ2-test or Fisher's exact test were used as needed.
In the evaluation of BCVA, measurements such as counting fingers and hand motion were set equal to 20/2000 (2 on the LogMAR scale) and 20/20 000 (3 on the LogMAR scale), respectively. Eyes with no light perception were counted as having 20/200 000 (4 on the LogMAR scale). Complications and their effect on BCVA were taken into consideration. We registered the BCVA in the follow-up period after the treatment-related complications had been treated and VA was stabilized. The enucleated eyes were excluded from VA analysis at the end of treatment. The complication rate and the average time to complication development were registered for both procedures.
A Kaplan–Meier analysis was performed to determine predictors of local recurrence, enucleation, metastatic disease, and OS and CSS. Those variables that were significantly associated with survival on the log-rank test (P<0.05) were subsequently analysed using a Cox regression model. Effect estimates were expressed as hazard ratios (HR) with 95% confidence intervals (95% CI). All statistical tests were two-tailed, and P-values of <0.05 were deemed significant.
Results
The baseline characteristics of both groups were largely similar, although some differences were observed. At diagnosis, eyes in the TSRWH group had worse Snellen BCVA and LogMAR and higher tumours than eyes in the IBT group (Tables 1 and 2).
Visual acuity
The final BCVA for TSRWH-treated eyes at the end of the follow-up period was better (in terms of percentage) than BCVA of eyes in the IBT group: 20/200 or better in 31.2% of the eyes in the IBT group vs 53.3% in the TSRWH group, although this difference was not statistically significant (χ2-test, P=0.121; Table 3). On Cox regression analysis, the treatment type had no significant influence on maintaining a VA≥20/200 (HR=0.847, 95% CI 0.32–2.24, P=0.739); similarly, none of the following variables influenced the likelihood of maintaining VA≥20/200: age, tumour height, largest basal diameter, distance to fovea, and distance to optic nerve.
Table 3. Treatment outcomes and follow-up.
|
IBT (n=53) |
TSRWH (n=19) |
P-valuea | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Final VA (Snellen-20 feet)b | |||||
| <20/200 | 33 | 68.8 | 7 | 46.7 | 0.121 |
| ≥20/200 | 15 | 31.2 | 8 | 53.3 | |
| Metastatic disease | |||||
| No | 39 | 73.6 | 16 | 84.2 | 0.531 |
| Yes | 14 | 26.4 | 3 | 15.8 | |
| Local recurrence | |||||
| No | 50 | 94.3 | 17 | 89.5 | 0.602 |
| Yes | 3 | 5.7 | 2 | 10.5 | |
| Enucleation | |||||
| No | 48 | 90.6 | 15 | 78.9 | 0.231 |
| Yes | 5 | 9.4 | 4 | 21.1 | |
| Enucleation cause | |||||
| Local recurrence | 3 | 5.7 | 2 | 10.5 | 0.602 |
| NVG | 2 | 3.8 | 0 | 0 | ≥0.999 |
| Corneal oedema | 0 | 0 | 2 | 10.5 | 0.067 |
| Overall death | |||||
| No | 47 | 88.7 | 17 | 89.5 | ≥0.999 |
| Yes | 6 | 11.3 | 2 | 10.5 | |
| Specific death | |||||
| No | 48 | 90.6 | 17 | 89.5 | ≥0.999 |
| Yes | 5 | 9.4 | 2 | 10.5 | |
| Parameters with MCT | Mean or median | SD (range) or IQR (range) | Mean or median | SD (range) or IQR (range) | P-valuea |
| Final VA (Snellen chart)b | 20/20 000 | 20/160 (20/200 000–20/25) | 20/200 | 20/34 (20/20 000–20/20) | 0.027 |
| Final VA (LogMAR)b | 3 | 2.15 (0.1–4.0) | 1 | 1.78 (0–3.0) | 0.029 |
| Follow-up (months)c | 55.9 | 28.6 (9.6–107.8) | 50.9 | 25.6 (9.6–102.5) | 0.506 |
Abbreviations: IBT, iodine-125 brachytherapy; IQR, interquartile range; MCT, measures of central tendency; NVG, neovascular glaucoma; TSRWH, transscleral resection performed without hypotensive anaesthesia; VA, visual acuity.
Median with IQR (range) were obtained for Snellen chart and LogMAR.
P-values were obtained by χ2-test (final VA<20/20 and ≥20/200) or Fisher's exact test (metastatic disease, local recurrence, enucleation, enucleation cause, overall death, and specific death) as needed for the qualitative variables, and by Mann–Whitney's U-test (final VA Snellen and LogMAR) or Student's t-test (follow-up) as needed for the quantitative variables.
Enucleated patients were excluded of BCVA analysis.
Mean, SD, and range were obtained for the follow-up. The bold values indicate P<0.05.
Local recurrence, metastasis, and survival
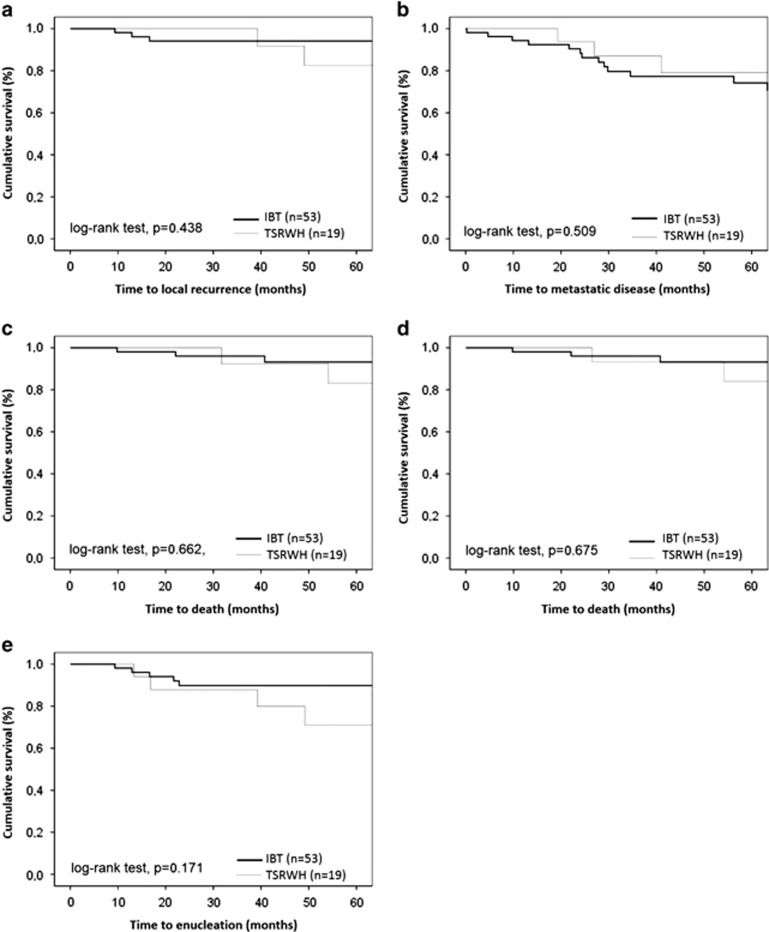
Local recurrence occurred in 5 eyes (3 in the IBT group (5.7%) vs 2 eyes (10.5%) in the TSRWH group; Fisher's exact test, P=0.602; Table 3). Notably, the two patients in the TSRWH group with local recurrence had not received adjuvant brachytherapy. On the basis of the Kaplan–Meier estimate, the percentage of eyes expected to be free of local recurrence was 94.1% in the IBT group and 82.5% in the TSRWH group at 5-year follow-up (log-rank test, P=0.438; Figure 1a). Cox regression analysis showed that eyes with ciliary body involvement had an increased risk (HR=11.4, 95% CI 2.24–49.7, P=0.04) of developing local recurrence irrespective of treatment, sex, age, tumour height, largest basal diameter, distance to optic nerve or to fovea, and iris or angle involvement.
Figure 1.
(a–e) TSRWH vs iodine-125 brachytherapy. (a) Kaplan–Meier curve showing percentage of eyes with choroidal melanoma without local recurrence after treatment. (b) Kaplan–Meier curve showing metastasis free-survival after treatment. (c) Kaplan–Meier curve of OS after treatment. (d) Kaplan–Meier curve of specific survival after treatment. (e) Kaplan–Meier curve showing percentage of patients with choroidal melanoma retaining the involved eye after treatment.
Metastasis was observed in 14 of 53 patients in the IBT group (26.4%) and in three patients (15.8%) in the TSRWH group (Fisher's exact test, P=0.531; Table 3). The estimated Kaplan–Meier proportion of patients without metastatic disease was expected to be 74.2% in the IBT group and 79.1% in the TSRWH group at 5-year follow-up (log-rank test, P=0.509; Figure 1b). All patients with metastatic disease presented liver spread. Other metastatic locations included lungs (2), bone marrow (2), peritoneum (1), skin (1), and the central nervous system (1).
Cox regression analysis showed that iris involvement (HR=16.0, 95% CI 4.2–170.2, P=0.033) and the largest tumour diameter (HR=2.3, 95% CI 1.2–4.8, P=0.04) increased the probability of metastasis, irrespective of treatment, tumour height, largest distance to optic nerve or to fovea, and local recurrence.
Eight patients (six in the IBT group and two in the TSRWH group) died during the follow-up period (11.3% vs 10.5%, respectively; Fisher's exact test, P≥0.999; Table 3). The Kaplan–Meier analysis of OS predicted 93.2% survival (IBT) vs 83% (TSRWH) at 5-year follow-up (log-rank test, P=0.662; Figure 1c); CSS was expected to be 93.2% (IBT) and 84% (TSRWH; log-rank test, P=0.675; Figure 1d). Cox regression analysis revealed that local recurrence had a negative impact on both OS (HR=17.3, 95% CI 2.8–107.1, P=0.002) and CSS (HR=18.5, 95% CI 2.9–116.4, P=0.002).
Secondary enucleation rates
Nine eyes required secondary enucleation: 5 (9.4%) in the IBT group and 4 (21.1%) in the TSRWH group (Fisher's exact test, P=0.231). According to Kaplan–Meier estimates, the probability of conserving the involved eye at 5 years post treatment was 89.8% (IBT) and 70.9% (TSRWH; log-rank test, P=0.171; Figure 1e). Cox regression analysis revealed that local recurrence (HR=39.0, 95% CI 12.8–79.4, P<0.001) and angle involvement (HR=22.3, CI 10.4–73.1, P=0.002) were significant risk factors for secondary enucleation.
Treatment-related complications
In the IBT group, the most frequent complications were radiation-induced retinopathy followed by neovascular glaucoma and macular oedema. Rhegmatogenous retinal detachment (RRD) and ocular hypertension were the most common complications of eyes treated with TSRWH. The complication rates and the mean time to emergence are presented in Table 4.
Table 4. Frequencies of complications and average time to development of both procedures.
| Complications of IBT | n=53 (%) | Average time to development in months |
|---|---|---|
| Radiation-induced retinopathya | 24 (45.3) | 20.8±10.6 (4.3–46.3) |
| Neovascular glaucomaa | 15 (28.3) | 25.6±11.7 (11.9–63.5) |
| Macular oedemaa | 13 (24.5) | 19.2±13.8 (11.3–43.2) |
| Vitreous haemorrhagea | 12 (22.6) | 29.0±16.3 (7.7–63.3) |
| Radiation-induced cataracta | 9 (17.0) | 11.3±5.9 (3.6–20.7) |
| Recurrent exudative retinal detachmenta | 7 (13.2) | 14.0±9.4 (4.0–28.5) |
| Scleral necrosisa | 4 (7.5) | 19.2±6.43 (11.3–26.3) |
| Complications of TSRWH | n=19 (%) | Average time to development in months |
| Rhegmatogenous retinal detachmenta | 4 (21.1) | 2.3±1.8 (0.23–3.0) |
| Ocular hypertensiona | 4 (21.1) | 1.3±0.24 (0.14–2.3) |
| Submacular haemorrhageb | 3 (15.8) | — |
| Corneal oedemac | 2 (10.5) | 10.1 (8.74–11.43) |
| Epiretinal membranec | 2 (10.5) | 12.2 (6.2–18.3) |
| Secondary glaucomac | 2 (10.5) | 19.3 (13.4–25.2) |
| Silicone oil emulsification (anterior chamber)c | 2 (10.5) | 3.9 (2.1–5.8) |
Abbreviations: IBT, iodine-125 brachytherapy; TSRWH, transscleral resection performed without hypotensive anaesthesial.
Mean±SD (range).
Perioperative complication.
Mean (range).
Discussion
The most extensive TSR technique is performed under hypotensive anaesthesia to minimise bleeding;10 however, this approach is not feasible in patients who cannot tolerate this type of anaesthesia. To resolve this problem, we performed an alternative approach to the classic technique. This procedure involves phacoemulsification of the lens with IOL, transscleral tumour resection, and a pars plana vitrectomy with silicone oil injection. TSRWH increases the number of patients eligible for TSR despite the presence of systemic diseases such as uncontrolled hypertension, renal disease, cerebrovascular disease, or ischaemic heart disease.
Using phacoemulsification with IOL implant, we were able to treat all cataracts shortly after diagnosis. Moreover, this technique permits completion of an extensive vitrectomy encompassing the extreme periphery without damaging the lens. Finally, the addition of pars plana vitrectomy was useful to evaluate and manage any induced haemorrhage, retinal damage, or residual tumour. In addition, the use of silicone oil may prevent late bleeding.
Visual acuity
Several studies have compared TSR with IBT. Puusaari et al8 reported that the mean VA after TSR was 20/320 to 20/640 through the first 5 years, approximately one line better than the mean VA after IBT (which varied between 20/640 and 20/1250). Two other studies (both matched case-control studies) carried out by Bechrakis et al9 and Kivelä et al7 found that patients treated with TSR had a significantly higher probability of retaining ambulatory vision compared with patients who underwent IBT.
In our study, VA impairment after TSRWH was limited to the first 3 months after surgery, likely because of the aggressive nature of TSR, which often results in early post-operative complications. In contrast, eyes treated with IBT continued to lose VA over time owing to treatment-related complications (eg, radiation-induced retinopathy, neovascular glaucoma, macular oedema, vitreous haemorrhage, and recurrent exudative retinal detachment). As a result, more than half of the eyes in the TSRWH group had a final BCVA≥20/200 vs less than one in three eyes in the IBT group. However, it should be noted that this difference was not statistically significant and, moreover, on Cox regression analysis, treatment with TSRWH was not found to be a significant independent predictor of retaining a BCVA≥20/200.
Local recurrence
The most common concern about local resection is the potential for local recurrence owing to incomplete tumour resection or residual intrascleral melanoma. According to some studies, the local recurrence rates at 5 years after treatment may vary from 7 to 24% after TSR with adjuvant brachytherapy, and between 5 and 10% after IBT.7, 8, 9, 10, 11, 12, 13, 14, 15 In their case-control study, Kivelä et al7 found a 35% local recurrence rate for TSR vs only 5% for IBT; importantly, however, when adjuvant brachytherapy was added, local recurrence decreased to 15%. Puusaari et al8 reported a 5-year local recurrence rate of 41% after TSR but only 7% after IBT in large melanomas.
Bechrakis et al13 evaluated long-term tumour control after TSR in 210 patients with large uveal melanomas. Local recurrence rates were 24 and 32% at 5 and 10 years, respectively. In a study carried out by Damato et al,14 286 patients were evaluated for the development of delayed local recurrence, which occurred in 57 cases (19.9%). Large basal diameter>16 mm and lack of adjuvant brachytherapy, between others, were identified as common risk factors for local recurrence after TSR.13, 14
In our study we did not find any significant differences in local recurrence rates between the TSRWH and IBT groups at 5-year follow-up (5.7 vs 10.5%). Moreover, no local recurrences were observed in eyes treated with TSRWH plus adjuvant brachytherapy (17 of 19 eyes). Cox regression analysis showed that eyes with ciliary body involvement had a significant risk of developing local recurrence regardless of the treatment group. Ciliary involvement has been described as a risk of local recurrence for large uveal melanoma after IBT.15 The local recurrence rate in the TSRWH group in our study was lower than rates described by other groups, probably because, for all our patients, we systematically reviewed the tumour margin and coloboma by complete vitrectomy; this permitted us to better manage the surgical margin or any residual tumour by direct visualisation. Moreover, in most patients, we also performed adjuvant brachytherapy.
Metastatic spread
In terms of metastasis, our results were in line with the existing literature. We found no significant differences in the 5-year rate of metastasis between the two treatment groups (21% for TSRWH vs 26% for IBT). We found that iris involvement and largest tumour diameter increased the risk of metastasis. This finding is interesting given that iris involvement has not been previously described as a risk factor for metastasis. Iris involvement might be a confounding factor because of the fact that all patients with iris extension had large tumours that were affecting the choroid and ciliary body at the same time. We already know that large choroidal tumours with extension to ciliary body are more difficult to treat and thus have an increased risk of local recurrence and metastasis.13, 15, 16
Similar rates of metastasis after TSR have been described.13, 16 Some variables associated with metastasis have been identified: tumour thickness, extraocular spread, local recurrence, largest basal diameter>16 mm, lack of adjuvant brachytherapy, and secondary enucleation.13, 16
OS and CSS
In our study, we found no differences between the two groups in 5-year OS and CSS rates. These findings are similar to those reported by other authors.7, 9, 17 They have observed that survival time after treatment was correlated with basal tumour diameter, TNM stage, extraocular spread, ciliary involvement, sex, mitotic count, and closed loops. In our study, by contrast, the only predictor of survival on the multivariate analysis was local recurrence, which negatively affected both OS and CSS.
Secondary enucleation
Although over 20% of eyes in the TSRWH group required secondary enucleation vs just under 10% in the IBT group, this difference was not statistically significant. It is important to point out that those eyes (two in the group of TSRWH) that did not receive adjuvant brachytherapy developed local recurrence and were enucleated. If we had considered only the eyes treated with TSRWH and adjuvant IBT, we would have obtained a lower enucleation rate. Surprisingly, corneal oedema due to silicone oil was the other cause of enucleation. Kivelä et al7 showed that after TSR, indications for secondary enucleation were local tumour recurrence and untreatable retinal detachment. Our Kaplan–Meier estimates showed that the probability of conserving the involved eye at 5 years post-treatment was ~90% in the IBT group vs 71% in the TSRWH group. Multivariate analysis showed that local recurrence and angle involvement were the only two significant risk factors for secondary enucleation. The incidence of enucleation reported by Puusaari et al8 (28% for TSR vs 10% for IBT) and Shields et al15 (24% at 5 years after IBT) was similar to our study. In contrast, Damato et al18 reported an actuarial rate of secondary enucleation of 11.1% at 5-year follow-up.
Major treatment-related complications
The major complications of IBT in our study were radiation-induced retinopathy, neovascular glaucoma, vitreous haemorrhage, macular oedema, cataract, exudative retinal detachment, and scleral necrosis. It is worth remarking that the reported radiation-induced retinopathy rate is highly variable, ranging from 10 to 63%.19, 20, 21 In the TSRWH group the adjuvant brachytherapy adds more safety in local tumour control, taking into account the possibility of inadequate excision margins. We chose to deliver 75 Gy to an imaginary residual tumour of 2–3 mm with IBT plaque. This consideration may have been responsible for less ocular morbidity in the TSRWH group. In IBT group, the whole tumour and its microscopic extensions form the basis of the clinical target volume to be treated. Obviously, these cases received a significantly higher dose when compared with a hypothetical residual tumour and/or cells in the TSRWH group. Thus, radiation-induced effects would be more frequent after primary IBT.
The rate of RRD in the TSRWH group was 21% (n=4). All patients with macula-on retinal detachment were treated successfully with pars plana vitrectomy (anatomical success was achieved in 100% with no evidence of recurrence in the follow-up period). An early incidence of this complication suggests that retinal tears occurred during tumour resection, especially in thick tumours. In a prospective study carried out by Damato et al,22 RRD occurred in 28 of 156 eyes (18%). Puusaari et al8 reported a 43% 5-year cumulative incidence of RRD after TSR. Although we routinely performed vitrectomy in the TSRWH group, this intervention does not appear to improve the RRD rate previously reported by Damato et al.22
Study limitations
Although we considered tumour location, distance to optic nerve and fovea, and size when selecting patients for inclusion, other prognostic factors (histopathology, genetic expression profile, and chromosomal abnormalities) may have influenced the survival rates. In addition, when the number of events is small, Cox regression analysis has limitations that make it difficult to draw any definitive conclusions. An ideal scenario would require a randomized, controlled, multicentric, prospective study; however, the feasibility of such a study is questionable given the many important technical challenges that would have to be overcome.
Conclusions
The findings from this study suggest that TSR with adjuvant brachytherapy is a safe procedure that can be performed without hypotensive anaesthesia. Patients treated with TSRWH may achieve a better final BCVA than those treated with IBT with acceptable rates of local recurrence, enucleation, metastatic disease, and survival. The complications associated with TSRWH are owing to an aggressive approach with early post-operative events. In contrast, patients treated with IBT experience delayed complications several years after treatment owing to the lasting effect of radiation on the eye. Prospective studies with large numbers of patients are required before a definitive role for TSRWH can be established.
The authors declare no conflict of interest.
References
- Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment and survival. Ophthalmology 2011; 118(9): 1881–1885. [DOI] [PubMed] [Google Scholar]
- Virgili G, Gatta G, Ciccolallo L, Capocaccia R, Biggeri A, Crocetti E et al. Incidence of uveal melanoma in Europe. Ophthalmology 2007; 114(12): 2309–1. [DOI] [PubMed] [Google Scholar]
- Semenova E, Finger PT. Palladium-103 plaque radiation therapy for American Joint Committee on cancer T3- and T4-staged choroidalmelanomas. JAMA Ophthalmol 2014; 132(2): 205–213. [DOI] [PubMed] [Google Scholar]
- Berry JL, Dandapani SV, Stevanovic M, Lee TC, Astrahan M, Murphree AL et al. Outcomes of choroidal melanomas treated with eye physics: a 20-year review. JAMA Ophthalmol 2013; 131(11): 1435–1442. [DOI] [PubMed] [Google Scholar]
- Marconi DG, de Castro DG, Rebouças LM, Bernardes Gil GO, Fogaroli RC, Conte Maia MA et al. Tumor control, eye preservation, and visual outcomes of ruthenium plaque brachytherapy for choroidal melanoma. Brachytherapy 2013; 12(3): 235–239. [DOI] [PubMed] [Google Scholar]
- Finger PT, Chin KJ, Tena LB. A five-year study of slotted eye plaque radiation therapy for choroidal melanoma: near, touching, or surrounding the optic nerve. Ophthalmology 2012; 119(2): 415–422. [DOI] [PubMed] [Google Scholar]
- Kivelä T, Puusaari I, Damato B. Transscleral resection vs iodine brachytherapy for choroidal malignant melanomas 6 millimeters or more in thickness: a matched case-control study. Ophthalmology 2003; 110(11): 2235–2244. [DOI] [PubMed] [Google Scholar]
- Puusaari I, Damato B, Kivelä T. Transscleral local resection vs iodine brachytherapy for uveal melanomas that are large because of tumour height. Graefes Arch Clin Exp Ophthalmol 2007; 245(4): 522–533. [DOI] [PubMed] [Google Scholar]
- Bechrakis NE, Bornfeld N, Zöller I, Foerster MH. Iodine 125 plaque brachytherapy vs transscleral tumor resection in the treatment of large uveal melanomas. Ophthalmology 2002; 109(10): 1855–1861. [DOI] [PubMed] [Google Scholar]
- Damato BE, Groenewald C, Foulds WS Surgical resection of choroidal melanoma In: Ryan SJ ed. Retina 5th edn. Elsevier Saunders: China, 2013; vol 3, pp 2299–2306. [Google Scholar]
- Factors predictive of growth and treatment of small choroidal melanoma: COMS Report No. 5. The Collaborative Ocular Melanoma Study Group. Arch Ophthalmol 1997; 115(12): 1537–1544. [DOI] [PubMed] [Google Scholar]
- Malignant melanoma of the uvea. En, Edge SB, Byrd DR, Compton CC et al eds. AJCC Cancer Staging Manual, 7th edn. Springer: New York, NY, USA, 2010; pp 547–559. [Google Scholar]
- Bechrakis NE, Petousis V, Willerding G, Krause L, Wachtlin J, Stroux A et al. Ten-year results of transscleral resection of large uveal melanomas: local tumour control and metastatic rate. Br J Ophthalmol 2010; 94(4): 460–466. [DOI] [PubMed] [Google Scholar]
- Damato BE, Paul J, Foulds WS. Risk factors for residual and recurrent uveal melanoma after trans-scleral local resection. Br J Ophthalmol 1996; 80(2): 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields CL, Naseripour M, Cater J, Shields JA, Demirci H, Youseff A et al. Plaque radiotherapy for large posterior uveal melanomas (≥8-mm thick) in 354 consecutive patients. Ophthalmology 2002; 109(10): 1838–1849. [DOI] [PubMed] [Google Scholar]
- Damato BE, Paul J, Foulds WS. Risk factors for metastatic uveal melanoma after trans-scleral local resection. Br J Ophthalmol 1996; 80(2): 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damato BE, Heimann H, Kalirai H, Coupland SE. Age, survival predictors, and metastatic death in patients with choroidal melanoma: tentative evidence of a therapeutic effect on survival. JAMA Ophthalmol 2014; 132(5): 605–613. [DOI] [PubMed] [Google Scholar]
- Damato B, Lecuona K. Conservation of eyes with choroidal melanoma by a multimodality approach to treatment: an audit of 1632 patients. Ophthalmology 2004; 111(5): 977–983. [DOI] [PubMed] [Google Scholar]
- Wen JC, Oliver SC, McCannel TA. Ocular complications following I-125 brachytherapy for choroidal melanoma. Eye 2009; 23(6): 1254–1268. [DOI] [PubMed] [Google Scholar]
- Jones R, Gore E, Mieler W, Murray K, Gillin M, Albano K et al. Posttreatment visual acuity in patients treated with episcleral plaque therapy for choroidal melanomas: dose and dose rate effects. Int J Radiat Oncol Biol Phys 2002; 52(4): 989–995. [DOI] [PubMed] [Google Scholar]
- Mameghan H, Karolis C, Fisher R, Mameghan J, Billson FA, Donaldson EJ et al. Iodine-125 irradiation of choroidal melanoma: clinical experience from the Prince of Wales and Sydney Eye Hospitals. Australas Radiol 1992; 36(3): 249–252. [DOI] [PubMed] [Google Scholar]
- Damato B, Groenewald CP, McGalliard JN, Wong D. Rhegmatogenous retinal detachment after transscleral local resection of choroidal melanoma. Ophthalmology 2002; 109(11): 2137–2143. [DOI] [PubMed] [Google Scholar]