Abstract
Purpose
To evaluate the ability of baseline clinical, morphological, and functional factors to predict the conversion to primary open-angle glaucoma (POAG) in ocular hypertensive (OHT) patients.
Methods
This single-center prospective longitudinal observational study included 116 eyes of 116 OHT patients followed for a 10-year period. All patients had intraocular pressure (IOP) ≥24 mm Hg in one eye and >21 mm Hg in the other eye, normal visual fields (VFs) and normal optic disc (OD) appearance in both eyes at baseline. All OHT patients were untreated at baseline with subsequent treatment upon need according to clinical judgement. Only one eye per subject was randomly selected. Patient age, gender, IOP, central corneal thickness (CCT), and ibopamine test results were collected at baseline. All patients underwent standard automated perimetry, short-wavelength automated perimetry (SWAP), frequency-doubling technology, confocal scanning laser ophthalmoscopy (CSLO), and scanning laser polarimetry (SLP) at baseline and every 6 months thereafter. Main outcome measure was the conversion to POAG, defined as the development of reproducible VF and/or OD abnormalities attributable to glaucoma. Cox proportional hazards models were used to identify the baseline factors predictive of POAG conversion.
Results
During the 10-year follow-up, 25% of eyes converted to POAG. In multivariate Cox models, baseline factors that were significant predictors of POAG development included: older age (hazard ratio (HR) 1.0, 99% confidence intervals (CIs) 1.0–1.2, per 1 year older); SWAP Glaucoma Hemifield test ‘outside normal limits' (HR 4.3, 99% CIs 1.2–17.9); greater SLP ‘Inter-eye Symmetry' (HR 1.1, 99% CIs 0.4–3.0, per 1 unit lower); lower CSLO Rim Volume (HR 1.1, 99% CIs 0.3–3.2, per 0.1 mm3 lower); and greater CSLO cup-to-disc ratio (HR 6.0, 99% CIs 3.6–16.8, per 0.1 unit greater).
Conclusions
The baseline parameters that proved to be useful in assessing the likelihood of an OHT patient to develop POAG included age, functional variables provided by SWAP, and structural variables provided by SLP and CSLO. In this cohort of patients, baseline IOP, CCT, and ibopamine provocative test results were not significant predictors of POAG conversion.
Introduction
Ocular hypertension (OHT) has been shown to be the most important risk factor in the development of primary open-angle glaucoma (POAG),1, 2, 3, 4, 5 and intraocular pressure (IOP) reduction has proven to be beneficial in halting or delaying POAG onset6 and progression.7 The treatment of all OHT patients, however, is not justified because of the high prevalence of OHT;8 the low conversion rate to POAG;3, 4, 5 and the cost and possible adverse effects of treatment.
In order to prevent the onset of POAG in OHT patients, previous large prospective cohort studies3, 4, 5 have attempted to identify predictive factors of the conversion of OHT to POAG, in order to identify those OHT patients who might benefit from close observation and early treatment. Older age, higher IOP, larger vertical or horizontal cup-to-disc (C/D) ratio, greater standard automated perimetry (SAP) pattern standard deviation (PSD) and thinner central corneal thickness (CCT) at baseline have all been found to be significant predictors for the onset of POAG in OHT patients in large multicenter long-term clinical trials, such as the Ocular Hypertension Treatment Study (OHTS)3 and the European Glaucoma Prevention Study (EGPS).5 The OHTS–EGPS prediction model has been validated in large independent populations showing predictive value.9, 10 Other risk factors for POAG are age, race, positive family history, and low diastolic perfusion pressure.1, 2, 11, 12, 13
Although SAP and ophthalmoscopic examination of the optic disc (OD) are still considered to be the clinical gold standards in the diagnosis and follow-up of glaucoma,14, 15 several new instrumental tests have been shown to provide earlier detection of functional or morphological glaucomatous damage,16, 17 including short-wavelength automated perimetry (SWAP),18 frequency-doubling technology (FDT),19 confocal scanning laser ophthalmoscopy (CSLO) with Heidelberg Retina Tomography (HRT),20 and scanning laser polarimetry (SLP).21 The ability of predictive models may improve with the inclusion of parameters provided by these new non-conventional perimetric tests and imaging instruments.
Ibopamine (3,4 di-isobutyrrylester of N-methyldopamine) is a D1-dopamine and alpha-adrenergic agonist that induces an increased aqueous humor production and a noncycloplegic mydriasis when instilled in the conjunctival sac.22 Previous studies have demonstrated that ibopamine eye drops can cause an IOP increase in subjects having a reduced functioning of the outflow structures, which include patients with: POAG, normal tension glaucoma, positive family history, and hydrodynamic disorders caused by corticosteroids; healthy patients, on the other hand, tend to show no influence on IOP with ibopamine.23, 24 The ibopamine test has been reported to be an efficient provocative test in the management of glaucoma and patients at risk.25
The purpose of this study was to determine whether higher IOP values, lower CCT measurements, positive ibopamine test results, SAP, SWAP, FDT, CSLO, or SLP alterations at baseline might be associated with an increased risk for development of POAG in OHT patients.
Materials and methods
This single-center prospective longitudinal clinical observational study included 133 OHT patients. Only one eye per subject was randomly selected using a computer-generated randomized number assignment if both eyes met the inclusion criteria.
OHT patients were cases referred by general ophthalmologists sent for further assessment and follow-up to the Department of Ophthalmology Glaucoma Center of the S. Maria della Misericordia Hospital, Udine, Italy, and were prospectively and consecutively evaluated. Eligible OHT patients were consecutive cases of either newly diagnosed or periodically monitored OHT patients in our Glaucoma Center, and were enrolled between 1 January and 30 September 2003.
The study was in compliance with Institutional Review Boards (IRBs) and HIPAA requirements and it was approved by the IRB of the Azienda Ospedaliero-Universitaria ‘Santa Maria della Misericordia', Udine, Italy.
The study was in compliance with the tenets of the Declaration of Helsinki Principles. The nature and purpose of the study were explained in detail to all participants, and informed consent (in accordance with the Ethical Review Committee regulations) was obtained from all 133 participants prior to testing.
Inclusion criteria were: IOP (before medication) ≥24 mm Hg in one eye and >21 mm Hg in the other eye, on at least three Goldmann applanation tonometry (GAT) measurements; normal OD and retinal nerve fiber layer (RNFL) appearance in both eyes; two normal and reliable SAP VF test results in both eyes; best-corrected visual acuity better than or equal to 0.7; open anterior chamber angle; absence of ocular pathology other than OHT, mild cataract and rare macular drusen; reliable SAP, SWAP, and FDT test results; good CSLO and SLP image quality; and willingness to provide written informed consent. Normal OD and RNFL appearance were clinically defined as: inter-eye vertical cup-disk asymmetry <0.2; C/D ratio <0.6; and, the absence of diffuse or focal rim thinning, cupping, localized pallor, optic disk hemorrhage, or RNFL defects. The criteria for normal SAP results were defined as not having a cluster of three or more points with P-value <5% in the pattern deviation probability (PDP) plot, and PSD and glaucoma hemifield test (GHT) results within normal limits.26
Exclusion criteria included: age <30 years; ocular congenital abnormalities; ametropia >±5 diopters; pupil diameter <2 mm; angle alterations; acquired ocular diseases; secondary causes of high IOP (ie, pseudoexfoliation syndrome, pigment dispersion syndrome, iridocyclitis, trauma, and corticosteroid use); POAG or other primary or secondary glaucoma; systemic pathologies that could be associated with glaucoma (eg, systemic hypotension, cardiovascular diseases, and diabetes); other diseases that could cause VF loss (eg, neurological disorders, pituitary lesion, and demyelinating diseases); medication that could modify VF results; OD abnormalities; media opacities preventing good image scans; previous intraocular surgery (excluding cataract surgery performed at least 6 months prior); pregnant or nursing women; and debilitating diseases that limit the patient's ability in performing all testing procedures at least twice yearly for 10 years.
All participants enrolled in the study were by definition untreated at baseline. During the follow-up, IOP therapy could be added and modified based on the judgement of the treating clinician. An IOP ≥27 mm Hg, a CCT ≤500 μm, and the presence of an immediate blood relative affected by glaucoma were strong indicators for adding or modifying the anti-glaucoma medications.
The baseline visit included: demographic and clinical data collection; complete ophthalmologic examination, including IOP and CCT measurements, gonioscopy, and optic disc evaluation using the slit-lamp and a Volk 78-D lens; ibopamine provocative test; functional tests, including SAP, SWAP, and FDT VF testing; and morphological tests, including CSLO and SLP imaging. The follow-up visits were performed at 6 months intervals for 10 years or until a censored event, and included: complete ophthalmologic examination; functional tests, including SAP, SWAP, and FDT VF testing; morphological tests, including CSLO and SLP imaging. Baseline and follow-up visits were performed by a single glaucoma specialist (CT).
Tests and instruments
IOP was taken with GAT. CCT was measured with ultrasonic pachymetry (Altair pachymeter, Optikon 2000, Rome, Italy).
The ibopamine test was performed by instilling 2% ibopamine (3,4 di-isobutyrrylester of N-methyldopamine) twice (interval of 5 min between drops) in the conjunctival sac, followed by repeat IOP measurements. The test is considered positive if there is an IOP increase of ≥3 mm Hg 45 min after instillation.25
SAP testing was performed using the Humphrey Field Analyzer (HFA) II 750 (Carl Zeiss Meditec, Inc., Dublin, CA, USA) 30–2 test with Standard Swedish Interactive Thresholding Algorithm strategy. Reliability criteria included false-positive <15%, false-negative <33%, and fixation losses <20%.
The FDT N-30 full-threshold procedure was used (Welch Allyn FDT, Skaneateles Falls, NY, USA and Carl Zeiss Meditec, Inc.).19 The stimulus is a sinusoidal grating of low spatial frequency (0.25 cycles/degree) with high temporal frequency (25 Hz); a Modified Binary Search strategy is utilized. Reliability criteria included fixation loss, false negative and false positive <33%.
SWAP18 was performed using the HFA II (Carl Zeiss Meditec, Inc.). A full-threshold 30–2 test was used with a blue (440 nm) size V (1.72°) 200 msec duration stimulus on yellow background (530 nm). SAP testing reliability criteria were used.
SAP, SWAP, and FDT VF testing were administered in random order, with a rest interval of at least 10 min between tests.
CSLO imaging was performed with the HRT II (Heidelberg Engineering, Heidelberg, Germany, software version 1.4.1.5).20 Exclusion criteria included: acquisition sensitivity <90% SD >40 microns; poor OD centration or image clarity. HRT classification is based on the Moorfields Regression Analysis (MRA) analysis, which includes: ‘Within normal limits' (confidence interval (CI) <95%); ‘Borderline' (95–99.9% CI); and, ‘Outside normal limits' (CI>99.9%).
SLP imaging was performed with GDx VCC (Carl Zeiss Meditec, Inc.; software version 5.1.0) equipped with a variable corneal compensator (VCC).21 The parameters include mean RNFL thickness average for: the entire 360° (TSNIT average); temporal (335–24°), superior (25–144°), nasal (145–214°), and inferior (215–334°) quadrants. Inclusion criteria included: quality scores >8, residual anterior segment retardation ≤15 nm, and typical scan score >25.
Main outcome measure
The main outcome measure was the conversion from OHT to POAG, defined as the development of reproducible VF abnormalities (functional endpoint) and/or OD or RNFL abnormalities (morphological endpoint) attributable to glaucoma. Morphological endpoint was met if at least one of the following was evident: ONH excavation, that is, undermining of the neural rim; notching involving ≥2 clock hours; focal or diffuse thinning of neural rim area involving ≥2 clock hours; focal or generalized atrophy of the RNFL. Functional endpoint was reached when at least one of the Anderson and Patella criteria27 was met: (1) a cluster of three points in the PDP plot, located in typical glaucomatous areas, having P<5%, with at least one point with P<1% none of the points could be edge points unless they were located immediately above or below the nasal horizontal meridian; (2) PSD <5% (3) GHT result outside normal limits. Confirmed VF defect required three consecutive, abnormal VF test results, with VF damage in the same test locations. The morphological and/or functional endpoint was reached based on masked consensus grading of two expert graders. Adjudication by a third expert grader was completed in cases of disagreement. The confirmation that the endpoint was attributable to POAG and the exclusion of artifacts as possible causes of VF or OD abnormalities were determined after masked review of the clinical charts by a third masked evaluator.
The endpoint time was defined as the time of development of POAG for patients showing conversion; and as the time of the last visit of the follow-up for non-converters.
Statistical analysis
Data distribution were analyzed using the Kolmogorov–Smirnov test. Comparisons between groups were assessed using the unpaired Student's t-test and the Mann–Whitney test. Differences between proportions were evaluated using the χ2-test. Univariate and multivariate Cox proportional hazard models were used to identify the baseline factors that were predictive of POAG conversion.
The variables considered in the univariate models included the following:
Demographic and clinical data: age, sex, CCT; baseline IOP;
Ibopamine test results: (positive vs negative; IOP peak 45 min after ibopamine administration and differences in IOP (ΔIOP) in comparison with pre-test IOP value;
SAP: mean deviation (MD), PSD, number of significantly abnormal areas with P<5% and P<1% in the PDP plot and GHT result. For baseline VF, the second obtained normal and reliable VF was used for the analysis.
SWAP: MD, PSD, number of significantly abnormal areas with P<5% and P<1% in the PDP plot, and GHT test result;
FDT: MD, PSD, number of significantly abnormal areas with P<5% and P<1% in the PDP plot. An abnormal FDT examination was defined by the presence of at least two areas with P<5% or worse on the PDP plot or by the presence of a PSD with P<5% or worse.28
HRT II: all parameters listed on the HRT Stereometric Analysis printout;
GDx VCC: nerve fiber indicator, inter-eye symmetry, TSNIT average, TSNIT-SD, superior average and inferior average.
Variables with P<0.1 in the univariate model were considered in a multivariate model. Cox proportional hazards multivariate model was performed using a backward strategy, with a statistical significance cutoff for variable screening of 0.05. The statistical analysis was performed using SPSS 11.0 for Windows (SPSS, Inc., Chicago, IL, USA). Statistical significance was defined as P<0.05.
Results
The 10-year follow-up results are summarized in Table 1. Of the 116 patients that completed the 10-year follow-up, 29 (25%) developed POAG and 87 (75%) did not by the end of the trial (30 September 2013). Mean follow-up time was 85.9±42 months (range 12–120) for converters and 115.3±5.0 months (range 108–120) for non-converters. Median conversion time was 48±20.1 months (range 12–84).
Table 1. Ten-year follow-up results.
| No. of cases | |
|---|---|
| Included patients | 133 |
| Patients that discontinuated the follow-up | 17 |
| Adverse events | 7 |
| Unwillingness to continue the follow-up | 10 |
| Patients that completed the follow-up | 116 |
| Patients that underwent cataract surgery during the follow-up | 15 |
| Non-convertes to POAG | 87 |
| Converters to POAG | 29 |
| Reaching a functional endpoint | 10 |
| Reaching a morphological endopoint | 19 |
| Based on optic disc damage | 13 |
| Based on retinal nerve fiber layer damage | 4 |
| Based on both optic disc and retinal nerve fiber layer damage | 2 |
| Patients that underwent anti-glaucoma treatment | 92 |
| Non-converters | 67 |
| Converters | 25 |
| Patients that did not untergo anti-glaucoma treatment | 24 |
| Non-converters | 20 |
| Converters | 4 |
Abbreviation: POAG, primary open-angle glaucoma.
The comparisons of baseline variables for all OHT eyes that either developed PAOG or did not are shown in Table 2. A statistically significant difference was found at baseline between converters and nonconverters for the following parameters: age, SWAP number points with P<5% on the PDP plot; number of eyes with SWAP GHT ‘outside normal limits' GDx VCC inter-eye Symmetry; all HRT II variables with exception to disc area, cup volume, mean cup depth, maximum cup depth, and the number of eyes with MRA ‘outside normal limits'.
Table 2. Comparison of baseline variables between converters and non-converters.
| Variables | Converters (no. of eyes=29) | Non-converters (no. of eyes=87) | Inter-groups differences |
|---|---|---|---|
| Mean±SDa | Mean±SDa | P-value | |
| Demographic and clinical data | |||
| Demographic data | |||
| Age (years) | 67.8±8.9 | 63.4±8.2 | 0.02b |
| Sex (Male/Female) | 16/13 | 40/47 | 0.09c |
| Clinical data | |||
| IOP (mmHg) | 25.4±3.6 | 25.6±3.6 | 0.82b |
| CCT (μm) | 563.8±41.5 | 561.5±39.9 | 0.79b |
| Anti-glaucoma treatment (yes/no) | 25/4 | 67/20 | 0.29c |
| Chemical tests | |||
| Ibopamine test | |||
| Test result (pos/neg) | 20/9 | 51/36 | 0.23c |
| Δ IOP (mmHg) | 6.2±4.7 | 5.4±4.9 | 0.42b |
| IOP peak (mmHg) | 27.0±6.0 | 27.0±5.0 | 0.96b |
| Functional tests | |||
| SAP | |||
| MD (dB) | −0.56±1.3 | −0.26±1.1 | 0.23b |
| PSD (dB) | 1.6±0.3 | 1.6±0.3 | 0.79b |
| Number of points with P<5% | 2.0±2.1 | 2.0±2.2 | 0.62d |
| Number of points with P<1% | 0.0±0.4 | 0.0±0.5 | 0.11d |
| GHT ‘outside normal limits' (yes/no) | 0/29 | 0/87 | 1.0c |
| SWAP | |||
| MD (dB) | 0.81±2.5 | 0.59±2.5 | 0.68b |
| PSD (dB) | 3.15±0.8 | 2.9±0.6 | 0.11b |
| Number of points with P<5% | 2.0±3.6 | 1.0±3.1 | 0.006d |
| Number of points with P<1% | 0.0±0.8 | 0.0±0.6 | 0.44d |
| GHT ‘outside normal limits' (Yes/No) | 5/24 | 3/84 | 0.03c |
| FDT | |||
| MD | 1.0±2.3 | 0.43±2.0 | 0.20b |
| PSD | 3.8±0.8 | 3.75±1.3 | 0.76b |
| Number of areas with P<5% | 2.0±2.6 | 2.0±2.2 | 0.40d |
| Number of areas with P<1% | 0.0±0.7 | 0.0±0.9 | 0.51d |
| FDT test result (normal/abnormal) | 12/17 | 46/41 | 0.17c |
| Structural tests | |||
| GDxVCC | |||
| NFI | 19.0±6.5 | 19.3±6.4 | 0.81b |
| TSNIT average (μm) | 56.2±5.6 | 56.6±5.2 | 0.72b |
| TSNIT SD | 68.1±7.6 | 68.2±6.8 | 0.94b |
| Superior average (μm) | 63.6±8.1 | 64.3±7.5 | 0.69b |
| Inferior average (μm) | 22.3±4.7 | 21.5±4.3 | 0.40b |
| Inter-eye symmetry | 0.83±0.1 | 0.86±0.1 | 0.04b |
| HRT II | |||
| Disc area (mm2) | 1.93±0.4 | 1.96±0.4 | 0.75b |
| Cup area (mm2) | 0.47±0.3 | 0.35±0.2 | 0.03b |
| Rim area (mm2) | 1.46±0.3 | 1.61±0.3 | 0.04b |
| Cup volume (mm3) | 0.09±0.1 | 0.06±0.1 | 0.07b |
| Rim volume (mm3) | 0.36±0.1 | 0.45±0.1 | 0.002b |
| C/D Ratio | 0.23±0.1 | 0.17±0.1 | 0.01b |
| Linear C/D Ratio | 0.45±0.2 | 0.39±0.1 | 0.01b |
| Mean cup depth (mm) | 0.19±0.1 | 0.18±0.1 | 0.33b |
| Maximum cup depth (mm) | 0.52±0.2 | 0.51±0.2 | 0.91b |
| Cup shape measure | −0.17±0.1 | −0.20±0.1 | 0.04b |
| Height variation contour (mm) | 0.30±0.1 | 0.40±0.1 | 0.004b |
| Mean RNFL thickness (mm) | 0.20±0.1 | 0.26±0.1 | 0.004b |
| RNFL cross sectional area (mm2) | 1.10±0.4 | 1.30±0.4 | 0.001b |
| MRA ‘outside normal limits' (yes/no) | 0/29 | 0/87 | 1.0c |
Abbreviations: CCT, central corneal thickness; C/D, cup/disc; CI, confidence interval; FDT, frequency-doubling technology; GDxVCC, scanning laser polarimetry with variable corneal compensator; GHT, glaucoma hemifield test; HRT, Heidelberg retina tomography; IOP, intraocular pressure; MD, mean deviation; MRA, Moorfields regression analysis; NFI, nerve fiber indicator; PSD, pattern standard deviation; RNFL, retinal nerve fiber layer; SAP, standard automated perimetry; SWAP, short-wavelength automated perimetry.
Median±SE for non-normally distributed variables.
Unpaired t-test.
χ2-test.
Mann–Whitney test.
Table 3 lists the univariate and multivariate hazard ratios with CIs and P-values for the development of POAG among OHT patients for each putative predictive baseline factor. All variables with P<0.1 in the univariate model were entered in a multivariate model. In univariate analysis, baseline variables significantly predictive of the development of POAG included: patient age, SWAP PSD, SWAP number points with P<5% on the PDP plot, SWAP GHT ‘outside normal limits', GDx VCC inter-eye symmetry, HRT II cup area, rim area, cup volume, rim volume, C/D ratio, linear C/D ratio, cup shape measure, height variation contour, mean RNFL thickness, and RNFL cross sectional area. Baseline variables significantly associated with the development of POAG in both uni- and multi-variate models included: patient age, SWAP GHT ‘outside normal limits', GDx VCC inter-eye symmetry, HRT II rim volume and HRT II C/D ratio.
Table 3. Univariate and Multivariate Cox proportional hazard models for the development of primary open-angle glaucoma among patients with ocular hypertension.
| Variables |
Univariate model |
Multivariate model |
||||
|---|---|---|---|---|---|---|
| HR | 99% CI | P-value | HR | 95% CI | P-value | |
| Demographic and clinical data | ||||||
| Demographic data | ||||||
| Age (per 1 year older) | 1.1 | 1.0–1.2 | 0.01 | 1.0 | 1.0–1.1 | 0.047 |
| sex (Male) | 1.1 | 0.8–1.3 | 0.62 | — | — | — |
| Clinical data | ||||||
| IOP (per 1 mm Hg higher) | 1.0 | 0.9–1.1 | 0.85 | — | — | — |
| CCT (per 1 μm lower) | 1.0 | 0.9–1.0 | 0.75 | — | — | — |
| Anti-glaucoma treatment (yes) | 1.6 | 0.6–3.5 | 0.39 | — | — | — |
| Chemical tests | ||||||
| Ibopamine test | ||||||
| Test result (positive) | 1.5 | 0.6–2.4 | 0.28 | — | — | — |
| Δ IOP (per 1 mm Hg higher) | 1.0 | 0.9–1.1 | 0.45 | — | — | — |
| IOP peak (per 1 mm Hg higher) | 1.0 | 0.9–1.1 | 0.87 | — | — | — |
| Functional tests | ||||||
| SAP | ||||||
| MD (per 0.1 dB lower) | 0.8 | 0.5–1.2 | 0.18 | — | — | — |
| PSD (per 0.1 dB higher) | 0.9 | 0.2–3.9 | 0.91 | — | — | — |
| Number of points with P<5% (per point abnormal) | 1.0 | 0.8–1.2 | 0.81 | — | — | — |
| Number of points with P<1% (per point abnormal) | 1.3 | 0.6–2.8 | 0.35 | — | — | — |
| GHT (outside normal limits) | NA | NA | NA | — | — | — |
| SWAP | ||||||
| MD (per 0.1 dB lower) | 1.0 | 0.8–1.3 | 0.71 | — | — | — |
| PSD (per 0.1 dB higher) | 1.6 | 0.8–3.2 | 0.07 | 0.7 | 0.6–2.2 | 0.48 |
| Number of points with P<5% (per point abnormal) | 1.5 | 0.9–3.2 | 0.03 | 1.0 | 0.9–1.2 | 0.76 |
| Number of points with P<1% (per point abnormal) | 1.3 | 0.7–2.2 | 0.27 | — | — | — |
| GHT (outside normal limits) | 3.4 | 0.8–13.6 | 0.002 | 4.3 | 1.4–13.5 | 0.01 |
| FDT | ||||||
| (per 0.1 dB lower) | 1.1 | 0.9–1.4 | 0.16 | — | — | — |
| (per 0.1 dB higher) | 1.0 | 0.7–1.5 | 0.71 | — | — | — |
| Number of areas with P<5% (per area abnormal) | 1.1 | 0.9–1.3 | 0.32 | — | — | — |
| Number of areas with P<1% (per area abnormal) | 0.9 | 0.4–1.8 | 0.64 | — | — | — |
| Test result (abnormal) | 1.2 | 0.8–1.5 | 0.28 | — | — | — |
| Structural tests | ||||||
| GDxVCC | ||||||
| NFI (per 1 unit higher) | 1.0 | 0.9–1.1 | 0.74 | — | — | — |
| TSNIT average (per 10 μm thinner) | 1.0 | 0.9–1.1 | 0.80 | — | — | — |
| TSNIT SD (per 10 μm greater) | 1.0 | 0.9–1.1 | 1.0 | — | — | — |
| Superior Average (per 10 μm thinner) | 1.0 | 0.9–1.1 | 0.67 | — | — | — |
| Inferior Average (per 10 μm thinner) | 1.0 | 0.9–1.2 | 0.45 | — | — | — |
| Inter-eye symmetry (per 1 unit lower) | 1.2 | 0.6–3.6 | 0.03 | 1.1 | 0.7–2.7 | 0.02 |
| HRT II | ||||||
| Disc area (per 0.1 mm2 greater) | 0.8 | 0.3–2.5 | 0.76 | — | — | — |
| Cup area (per 0.1 mm2 greater) | 4.9 | 1.4–16.7 | 0.01 | 2.0 | 1.1–6.9 | 0.48 |
| Rim area (per 0.3 mm2 lower) | 0.9 | 0.2–3.1 | 0.04 | 0.7 | 0.4–1.3 | 0.25 |
| Cup volume (per 0.1 mm3 greater) | 3.7 | 1.2–9.8 | 0.06 | 1.2 | 0.8–4.8 | 0.62 |
| Rim volume (per 0.1 mm3 lower) | 0.8 | 0.3–2.6 | 0.002 | 1.1 | 0.5–2.8 | 0.005 |
| C/D ratio (per 0.1 unit greater) | 6.2 | 3.2–17.7 | 0.008 | 6.0 | 3.9–14.9 | 0.02 |
| Linear C/D ratio (per 0.1 units greater) | 4.1 | 1.8–9.2 | 0.06 | 1.4 | 1.0–2.0 | 0.10 |
| Mean cup depth (per 0.1 mm greater) | 1.3 | 1.0–1.7 | 0.51 | — | — | — |
| Maximum cup depth (per 0.1 mm greater) | 1.2 | 0.7–2.7 | 0.85 | — | — | — |
| Cup shape measure (per 0.1 unis greater) | 5.3 | 2.0–19.1 | 0.05 | 3.3 | 1.4–9.8 | 0.72 |
| Height variation contour (per 0.1 mm greater) | 2.7 | 1.7–4.1 | 0.003 | 1.5 | 1.2–1.7 | 0.61 |
| Mean RNFL thickness (per 0.2 mm lower) | 0.9 | 0.7–2.0 | 0.002 | 0.7 | 0.6–1.1 | 0.57 |
| RNFL cross sectional area (per 0.3 mm2 lower) | 0.7 | 0.4–2.1 | 0.003 | 0.4 | 0.3–1.0 | 0.66 |
| MRA (outside normal limits) | NA | NA | NA | — | — | — |
Abbreviations: C/D, cup/disc; CI, confidence interval; FDT, frequency-doubling technology; GDxVCC, scanning laser polarimetry with variable corneal compensator; GHT, glaucoma hemifield test; HR, hazard ratios; HRT, Heidelberg retina tomography; MD, mean deviation; MRA, Moorfileds regression analysis NA, not applicable; NFI, nerve fiber indicator; PSD, pattern standard deviation; RNFL, retinal nerve fiber layer; SAP, standard automated perimetry; SWAP, short-wavelength automated perimetry.
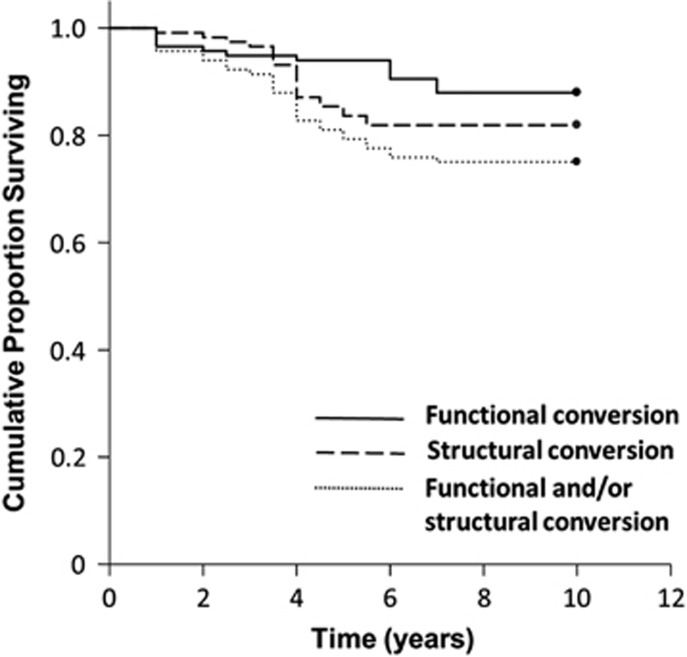
Figure 1 shows the Kaplan–Meier plots for the cumulative probability of survival from functional, morphological or mixed conversion to POAG. The conversion rate from OHT to POAG found in our study during the 10-year follow-up was 25%.
Figure 1.
Kaplan–Meier survival curves of our cohort of OHT patients. Cumulative proportion surviving=proportion without POAG conversion. Study endpoint was defined as the development of functional (continuous line), structural (dashed line), or functional and/or structural (dotted line) glaucomatous damage.
Discussion
Our study included one eye of 116 OHT patients, which were representative of our clinical practice and prospectively followed for a 10-year period. Intergroups comparison of the baseline variables and Cox univariate models revealed that some baseline parameters were significantly different between groups and significantly associated with the development of POAG, which included: age, functional abnormalities provided by SWAP, and structural parameters measured with GDxVCC and HRT II. Gender, IOP, CCT, ibopamine test results, SAP, and FDT variables were comparable between groups and were not predictive for glaucoma conversion.
Our results are in disagreement with several previous studies demonstrating that higher IOP,3, 4, 5, 9, 10 thinner CCT,3, 5, 9, 10, 28, 29, and greater SAP PSD3, 5, 9, 10 at baseline are predictive of the development of POAG among OHT subjects. The differences among results of the various studies could be related to several factors including: number and race of study population; anti-glaucoma therapy and other intercurrent factors during the follow-up; data collection methods used; VF and OD evaluation methods; definition of OHT and conversion to glaucoma. In particular, our study included only one eye per patient, whereas in the glaucoma predictive models developed by the OHTS,6 EGPS,13 and Diagnostic Innovation in Glaucoma Study (DIGS)30 studies, both eyes of each participant were included in the study if they met the inclusion criteria; the baseline predictive factors values were calculated by averaging the values of the two eyes of a single participant; and the end point was defined as the development of POAG in one eye per patient.
Differently from previous studies,6, 13, 30 numerous patients in our OHT cohort began IOP-lowering eye drop medication when needed based on the discretion of the attending physician therapy during the follow-up, which included 79.3% treated eyes. This may have reduced the significance of the baseline IOP as predictor, considering that IOP-related intercurrent factors, such as mean follow-up IOP and mean follow-up IOP reduction, have been demonstrated to be significant predictors for the glaucoma conversion in OHT patients.31
The mean CCT value of our cohort of patients was lower than that reported by other studies for OHT subjects.32, 33 Considering that a substantial number of OHT patients tend to have an overestimation of GAT IOP based on a thicker cornea,34 the significance of the CCT value as predictor for POAG development could be related to the proportion of false-positive OHT patients included in the study. Moreover, IOP and CCT values are related and this could have masked the real effect of both parameters in predicting POAG conversion.
As part of the inclusion criteria for our study, all OHT patients were required to have normal SAP results in both eyes. SAP was defined as normal based on the Hoddapp, Parrish and Anderson criteria,26 which tend to be more stringent than those used in previous studies,6, 13, 30 where normal VF test results were defined as a MD and PSD within 95% confidence limits and a GHT result within normal limits.
Our data are in disagreement with previous studies showing that FDT abnormalities35, 36 at baseline are predictive of the development of POAG among OHT subjects. FDT testing gave rise to a high percentage of abnormal results in our cohort of OHT subjects, which included 47.1% in the nonconverters and 58.6% in the converters subjects, and a low ability in discriminating between the two groups (P=0.17). The percentage of OHT subjects with abnormal FDT results found in our study was comparable to that reported by other authors,35, 36, 37, 38 yet greater than the number that would be expected to convert to glaucoma, suggesting that the high sensitivity of FDT in detecting early glaucomatous damage could be partially related to false positive results.
In agreement with our data, older age has been identified as a baseline risk factor for developing POAG among OHT patients in multiple progression studies.3, 5, 39 Moreover, our findings are in accordance with previous studies showing that the risk of POAG conversion in OHT and glaucoma suspects is significantly associated with the presence of baseline abnormalities in SWAP,40, 41 SLP,42 and CSLO.43, 44 The significantly higher proportion of SWAP, SLP, and CSLO alterations found in converters in comparison with nonconverters could be considered as a sign of early glaucomatous damage in eyes with normal SAP and OD examination results, rather than true risk factors.
The only SLP parameter showing predictive ability in our study was ‘Inter-eye Symmetry'. In agreement with these data, a predictive value of asymmetry between eyes in OHT patients for the development of POAG has been already reported for IOP,45 cup-to-disc ratio,5 and VF threshold.45
Although several HRT II parameters showed predictive ability, rim volume, C/D ratio, and mean RNFL thickness showed the best performance. These results are in accordance with the CSLO ancillary study of the OHTS, demonstrating that several baseline HRT parameters can be used to predict the development of POAG in OHT patients.43, 44
To the best of our knowledge, this is the first study evaluating the predictive ability of the ibopamine test for the conversion to glaucoma in OHT patients. The ability of the ibopamine test result in discriminating between converters and non-converters was very poor, with a sensitivity of 69% and a specificity of 41.4%, suggesting that a large proportion of the OHT subjects had a reduced outflow of the aqueous humor. Although several previous authors have demonstrated that the ibopamine test has high accuracy in differentiating glaucomatous eyes from normal46 and glaucoma suspect eyes,47 our data show that the positivity of the ibopamine test has no predictive value for the development of glaucoma. The results of the present study suggest that the ibopamine provocative test seems to be efficient in indicating the actual health status of the trabecular meshwork, but it seems unable to predict the evolution of the glaucomatous disease.
The results of the multivariate model suggest that patients with older age, SWAP GHT results ‘outside normal limits', lower GDx VCC inter-eye symmetry, lower HRT II rim volume, and greater HRT II C/D ratio exhibit an increased risk of glaucoma progression and may need enhanced treatment management. A smaller rim volume at baseline was one of the most consistent predictors of POAG in the multivariate models.
Figure 1 shows the Kaplan–Meier plots for the cumulative probability of survival from functional, morphological, or mixed conversion to POAG. The conversion rate from OHT to POAG found in our study was 21.5% during the initial 5-year follow-up and 25% during the entire 10-year follow-up. During the follow-up, our OHT patients were put on IOP-lowering eye drop medication when needed based on the discretion of the attending physician; thus, the study included both treated (79.3%) and untreated eyes (20.7%). The 5-year cumulative probability of developing POAG in large multicenter long-term clinical trials was 9.5% in the untreated group and 4.4% in the treated group in the OHTS;6 13.7% and 16.4%, respectively, in the untreated and treated patients in the EGPS;13 and 25% in a group of untreated OHT patients in the DIGS.30
In agreement with the EGPS,13 and in disagreement with the OHTS,12 the conversion rate was comparable between untreated (20.8%) and treated eyes (26.2% P=0.11). Converters were more likely to receive treatment (86.2%) than nonconverters (77%) during the study period, probably because they were deemed at higher risk for glaucoma by the treating clinician. The proportions of converters reaching a morphological, functional, or mixed endpoint, which were 51.7%, 27.6% and 20.7%, respectively, were comparable with those found in previous reports.6, 30 These results are in agreement with several previous studies, which show that structural damage may often be detected several years before the development of VF defects measured by SAP in early glaucoma.48, 49, 50
Our study has several limitations. A number of factors described as predictive for POAG among OHT eyes in previous studies were not evaluated in this study, including: family history of POAG, myopia, diabetes, race, cardiovascular disease, systemic blood hypo- and hypertension, ocular perfusion pressure, and local and systemic therapy.1, 2, 3, 5, 11, 12 The prediction model developed in our study incorporated only baseline variables. Models incorporating intercurrent risk factors may provide an improved risk assessment.48 The exact recruitment process data are not available, thus the precise number of patients that were approached, or considered ineligible or that did not give the consent to the study cannot be reported, which is a limiting factor of our study. Our OHT patients were treated upon need based on the discretion of the attending physician, thus both treated and untreated eyes were included in the study. Moreover, various anti-glaucoma medications were used to treat patients, which may have influenced the rate of glaucoma development in each individual. Another limitation in our study is related to the subjective nature of the OD assessment, even if the OD evaluations were performed in a standardized manner by highly trained graders. Finally, our findings may be not applicable to other clinical settings due to the specific population included in our cohort, in which certain risk factors may have a more important role than others.
In conclusion, the results of our study showed that, in a cohort of OHT patients which were representatives of our clinical practice, baseline older age, and functional abnormalities provided by SWAP, and structural alterations shown by GDxVCC and HRT II were significantly associated with the risk of future structural or functional glaucomatous damage among OHT patients. These findings may also have significant implications in the detection of early glaucomatous damage in OHT patients. Mean IOP, CCT, SAP PSD, and the ibopamine test results at baseline did not show any predictive value. Our study suggests that the combination of patient age with structural and functional variables provided by various instruments could help the clinician in better managing a general population of OHT patients, even if a predictive model alone cannot replace clinical judgment. Prospective studies based on a greater cohort of patients, longer follow-ups, and additional parameters are required to assess the clinically usefulness of future predictive models.
The authors declare no conflict of interest.
References
- Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans: the Baltimore Eye Survey. Arch Ophthalmol 1991; 109: 1090–1095. [DOI] [PubMed] [Google Scholar]
- Leske MC, Connell AM, Wu SY, Hyman LG, Schachat AP. Risk factors for open-angle glaucoma: The Barbados eye Study. Arch Ophthalmol 1995; 113: 918–924. [DOI] [PubMed] [Google Scholar]
- Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The Ocular Hypertension Treatment Study. Baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720. [DOI] [PubMed] [Google Scholar]
- Bengtsson B, Heijl A. A long-term prospective study of risk factors for glaucomatous visual field loss in patients with ocular hypertension. J Glaucoma 2005; 14: 135–138. [DOI] [PubMed] [Google Scholar]
- The European Glaucoma Prevention Study Group. Predictive factors for open-angle glaucoma among patients with ocular hypertension in the European Glaucoma Prevention Study. Ophthalmology 2007; 114: 3–9. [DOI] [PubMed] [Google Scholar]
- Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delay or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713. [DOI] [PubMed] [Google Scholar]
- Hejil A, Leske MC, Bengtsson B, Hyman L, Bengtsspn B, Hussein M, Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression. Results from the Early manifest Glaucoma Trial. Arch Ophthalmol 2002; 120: 1268–1279. [DOI] [PubMed] [Google Scholar]
- Tielsch JM, Katz J, Singh K, Quigley HA, Gottsch JD, Javitt J et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am J Epidemiol 1991; 134: 1102–1110. [DOI] [PubMed] [Google Scholar]
- Ocular Hypertension Treatment Study Group, European Glaucoma Prevention Study Group. Validated prediction model for the development of primary open-angle glaucoma in individuals with ocular hypertension. Ophthalmology 2007; 114: 10–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takwoingi Y, Botello AP, Burr JM, Azuara-Blanco A, Garway-Heath DF, Lemij HG et al. External validation of the OHTS-EGPS model for predicting the 5-year risk of open-angle glaucoma in ocular hypertensives. Br J Ophthalmol 2014; 98: 309–314. [DOI] [PubMed] [Google Scholar]
- Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC. Family history and risk of primary open angle glaucoma: the Baltimore Eye Survey. Arch Ophthalmol 1994; 112: 69–73. [DOI] [PubMed] [Google Scholar]
- Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: The Egna-Neumarkt Study. Ophthalmology 2000; 107: 1287–1293. [DOI] [PubMed] [Google Scholar]
- The European Glaucoma Prevention Study Group. The results of the European Glaucoma Prevention Study. Ophthalmology 2005; 112: 366–375. [DOI] [PubMed] [Google Scholar]
- American Academy of Ophthalmology preferred practice patterns committee glaucoma panelPreferred Practice Patterns. Primary Open Angle Glaucoma Suspect. American Academy of Ophthalmology: San Francisco, CA, USA, 2002. [Google Scholar]
- Jonas JB, Budee WM, Panda-Jonas S. Ophthalmoscopic evaluation of the optic nerve Head. Surv Ophthalmol 1999; 43: 293–320. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Bowd C, Weinreb RN. Comparison of the GDx VCC Scanning Laser Polarimeter, HRT II Confocal Scanning Laser Ophthalmoscope, and Stratus OCT Optical Coherence Tomograph for the detection of glaucoma. Arch Ophthalmol 2004; 122: 827–837. [DOI] [PubMed] [Google Scholar]
- Spry PG, Johnson CA, Mansberger SL, Cioffi GA. Psychophysical investigation of ganglion cell loss in early glaucoma. J Glaucoma 2005; 14: 11–19. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Adams AJ, Casson EJ Blue-on-yellow perimetry: A five year overview. In: Mills RP (ed). Perimetry Update 1992/93. Kugler Publications: New York, USA, 1993; 459–466. [Google Scholar]
- Johnson CA, Samuels JS. Screening for glaucomatous visual field loss with frequency-doubling perimetry. Invest Ophthalmol Vis Sci 1997; 38: 413–425. [PubMed] [Google Scholar]
- Kruse FE, Burk RO, Völcker HE, Zinser G, Harbarth U. Reproducibility of topographic measurements of the optic nerve head with laser tomographic scanning. Ophthalmology 1989; 96: 1320–1324. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Weinreb RN. Individualized compensation of anterior segment birefringence during scanning laser polarimetry. Invest Ophthalmol Vis Sci 2002; 43: 2221–2228. [PubMed] [Google Scholar]
- Virno M, Taverniti L, De Gregorio F, Sedran L, Longo F. Increase in aqueous humor production following D1-receptor activation by means of ibopamine. Int Ophthalmol 1996-1997; 20: 141–146. [DOI] [PubMed] [Google Scholar]
- Virno M, De Gregorio F, Pannarale MR. Ocular pressure increase by ibopamine discloses aqueous humor outflow changes in Normal Tension Glaucoma. Acta Ophthalmol Scand 2000; 78: 12–13. [DOI] [PubMed] [Google Scholar]
- Azevedo H, Ciarniello MG, Rosignoli MT, Dionisio P, Cunha-Vaz J. Effects of ibopamine eye drops on intraocular pressure and aqueous humor flow in healthy volunteers and patients with open-angle glaucoma. Eur J Ophthalmol 2003; 13: 370–376. [DOI] [PubMed] [Google Scholar]
- De Gregorio F, Pecori Giraldi J, Pannarale L, Saccucci S, Virno M. Ibopamine in glaucoma diagnostic: a new pharmacological provocative test. Int Ophthalmol 1996–1997; 20: 151–155. [DOI] [PubMed] [Google Scholar]
- Hoddapp E, Parrish RK, Anderson DR. Clinical Decision in Glaucoma. The CV Mosby: St Louis, 1993; 52–61. [Google Scholar]
- Anderson D, Patella V. Automated Static Perimetry. Mosby: St. Louis, 1999; 117. [Google Scholar]
- Medeiros FA, Sample PA, Weinreb RN. Corneal thickness measurements and visual function abnormalities in ocular hypertensive patients. Am J Ophthalmol 2003; 135: 131–137. [DOI] [PubMed] [Google Scholar]
- Zeppieri M, Brusini P, Miglior S. Corneal thickness and functional damage in patients with ocular hypertension. Eur J Ophthalmol 2005; 15: 196–201. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Weinreb RN, Sample PA, Gomi CF, Bowd C, Crowston JG et al. Validation of a predictive model to estimate the risk of conversion from ocular hypertension to glaucoma. Arch Ophthalmol 2005; 123: 1351–1360. [DOI] [PubMed] [Google Scholar]
- Miglior S, Torri V, Zeyen T, Pfeiffer N, Vaz JC, Adamsons I, EGPS Group. Intercurrent factors associated with the development of open-angle glaucoma in the European Glaucoma Prevention Study. Am J Ophthalmol 2007; 144: 266–275. [DOI] [PubMed] [Google Scholar]
- Copt RP, Thomas R, Mermoud A. Corneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucoma. Arch Ophthalmol 1999; 117: 14–16. [DOI] [PubMed] [Google Scholar]
- Brandt JD, Beiser JA, Kass MA, Gordon MO. Central corneal thickness in the Ocular Hypertension Treatment Study (OHTS). Ophthalmology 2001; 108: 1779–1788. [DOI] [PubMed] [Google Scholar]
- Johnson M, Kass MA, Moses RA, Grodzki WJ. Increased corneal thickness simulating elevated intraocular pressure. Arch Ophthalmol 1978; 96: 664–665. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Sample PA, Weinreb RN. Frequency doubling technology perimetry abnormalities as predictors of glaucomatous visual field loss. Am J Ophthalmol 2004; 137: 863–871. [DOI] [PubMed] [Google Scholar]
- Bagga H, Feuer W, Greenfield DS. Detection of psychophysical and structural injury in eyes with glaucomatous optic neuropathy and normal standard automated perimetry. Arch Ophthalmol 2006; 124: 169–176. [DOI] [PubMed] [Google Scholar]
- Sample PA, Bosworth CF, Blumenthal EZ, Girkin C, Weinreb RN. Visual function-specific perimetry for indirect comparison of different ganglion cell populations in glaucoma. Invest Ophthalmol Vis Sci 2000; 41: 783–790. [PubMed] [Google Scholar]
- Zeppieri M, Brusini P, Parisi L, Johnson CA, Sampaolesi R, Salvetat ML. Pulsar perimetry in the diagnosis of early glaucoma. Am J Ophthalmol 2010; 149: 102–112. [DOI] [PubMed] [Google Scholar]
- Quigley HA, Enger C, Katz J, Sommer A, Scott R, Gilbert D. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Arch Ophthalmol 1994; 112: 644–649. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Adams AJ, Casson EJ, Brandt JD. Blue-on-yellow perimetry can predict the development of glaucomatous visual field loss. Arch Ophthalmol 1993; 111: 645–650. [DOI] [PubMed] [Google Scholar]
- Sample PA, Taylor JD, Martinez GA, Lusky M, Weinreb RN. Short-wavelength color visual fields in glaucoma suspects at risk. Am J Ophthalmol 1993; 115: 225–233. [DOI] [PubMed] [Google Scholar]
- Mohammadi K, Bowd C, Weinreb RN, Medeiros FA, Sample PA, Zangwill LM. Retinal nerve fiber layer thickness measurements with scanning laser polimetry predict glaucomatous visual field loss. Am J Ophthalmol 2004; 138: 593–601. [DOI] [PubMed] [Google Scholar]
- Zangwill LM, Weinreb RN, Beiser JA, Berry CC, Cioffi GA, Coleman AL et al. Baseline topographic optic disk measurements of primary open-angle glaucoma: The Confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment Study. Arch Ophthalmol 2005; 123: 1188–1197. [DOI] [PubMed] [Google Scholar]
- Weinreb RN, Zangwill LM, Jain S, Becerra LM, Dirkes K, Piltz-Seymour JR et al. Predicting the onset of glaucoma: The confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment Study. Ophthalmology 2010; 117: 1674–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine RA, Demirel S, Fan J, Keltner JL, Johnson CA, Kass MA, Ocular Hypertension Treatment Study Group. Asymmetries and visual field summaries as predictors of glaucoma in the Ocular Hypertension Treatment Study. Invest Ophthalmol Vis Sci 2006; 47: 3896–3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magacho L, Lima FE, Costa ML, Fayad FA, Guimaraes NL, Avila MP. Ibopamine provocative test and glaucoma: consideration of factors that may influence the examination. Curr Eye Res 2004; 28: 189–193. [DOI] [PubMed] [Google Scholar]
- Ullrich K, Craig JE, Landers J. Ibopamine challenge testing can be used to differentiate glaucoma suspects from glaucoma patients. Clin Experiment Ophthalmol 2014; 42: 342–346. [DOI] [PubMed] [Google Scholar]
- Chauhan BC, McCormick TA, Nicolela MT, LeBlanc RP. Optic disc and visual field changes in a prospective longitudinal study of patients with glaucoma: comparison of scanning laser tomography with conventional perimetry and optic disc photography. Arch Ophthalmol 2001; 119: 1492–1499. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol 2009; 127: 1250–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sehi M, Zhang X, Greenfield DS, Chung Y, Wollstein G, Francis BA et al. Retinal nerve fiber layer atrophy is associated with visual field loss over time in glaucoma suspect and glaucomatous eyes. Am J Ophthalmol 2013; 155: 73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]