Abstract
Background
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect almost any organ system, including the kidneys. Using a large national dataset, our goal was to compare the morbidity as measured by hospitalization and mortality rates between hemodialysis patients with end-stage renal disease (ESRD) secondary to SLE to those with ESRD due to other causes.
Methods
The risk of hospitalization was calculated by Poisson regression with clustering for repeated measures using the United States Renal Data System (USRDS) Hospitalization Analytic File in strata of pediatric and adult patients. Cox proportional hazard ratio was used to assess the mortality risk in hospitalized patients. Subjects were censored at transplantation or end of follow-up.
Results
Adult patients with ESRD secondary to SLE were hospitalized more frequently than other adults (incidence rate ratio (IRR): 1.43, 95% confidence interval (CI): 1.15–1.77) and had a higher risk of death (hazard ratio (HR): 1.89, 95% CI: 1.66–2.5). Mortality was higher in hospitalized pediatric patients with SLE compared to pediatric patients with other causes of ESRD (HR: 2.01, 95% CI: 1.75–2.31) and adults with SLE (HR: 2.05, 95% CI: 1.79–2.34).
Conclusion
Our study demonstrates that there is a trend toward increased hospitalization rates in pediatric and adult patients with SLE. Among these hospitalized patients with SLE, there is an increased risk of death due to cardiovascular disease.
Keywords: Systemic lupus erythematosus, hemodialysis, hospitalization, mortality
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease that affects 20 to 150 women per 100,000, with a higher prevalence in patients of African American and Asian descent.1,2 SLE also presents in childhood, accounting for up to 10% of patients with pediatric rheumatic diseases and approximately 20% of all SLE patients.3,4 Kidney involvement is common in these patients, with up to 60% of adults and 80% of pediatric patients presenting with some form of kidney disease.3,5 Some of these patients will progress on to endstage renal disease (ESRD) and require renal replacement therapy.
We have previously shown that pediatric and adult patients with ESRD secondary to SLE have an increased risk of death compared to patients with other causes of ESRD.6 Our goal in this manuscript was to define morbidity in patients with SLE using rates of hospitalization as a surrogate marker for morbidity. We also explored mortality rates in this specific hospitalized patient population. We compared three groups: 1) pediatric hemodialysis (HD) patients with ESRD secondary to SLE vs. pediatric HD patients with other causes of ESRD; 2) adult HD patients with ESRD secondary to SLE vs. adults HD patients with ESRD secondary to other causes; and 3) pediatric vs. adult HD patients with ESRD secondary to SLE.
Patients and methods
United States Renal Data System (USRDS)
The USRDS, operated by the National Institute of Diabetes and Digestive and Kidney Diseases and the Health Care Financing Administration, collects data on mortality and hospitalization from patients in the United States receiving renal replacement therapy. To be included in the database, patients must be receiving chronic renal replacement therapy or have undergone kidney transplantation. Patients are excluded from the USRDS dataset if they receive dialysis only for an acute kidney injury, die of kidney failure before receiving renal replacement therapy, or do not accept renal replacement therapy.7
In this analysis, we used the USRDS Hospitalization Analytic File, which includes clinical and demographic information only on patients who were hospitalized. The data are collected through claim forms and reported back to the USRDS. Patients receiving peritoneal dialysis were excluded because there were <20 pediatric patients with SLE receiving this modality.
Variables
Demographic and clinical characteristics were explored among adults and children in the USRDS Hospitalization Analytic File. According to the USRDS definition, pediatric patients were defined as age ≤ 18 years at first ESRD service. Causes of ESRD were dichotomized into SLE (ICD 9 code: 710.0) vs. all other diagnoses. Other clinical information from the USRDS included age at dialysis onset, gender, race and years receiving dialysis.
Data analysis
In order to capture patients receiving relatively standardized care for SLE (i.e. cyclophosphamide for treatment of diffuse proliferative glomerulonephritis), only patients starting dialysis after Jan. 1, 1990, were included in the analysis.
Differences in clinical characteristics such as age, race and gender between patients were determined by two-tailed Student t-test for continuous data or chi-squared test of proportions. Differences in the duration of dialysis during the time at risk were determined by two-tailed Student t-test for continuous data.
The number of hospitalizations per time at risk for each patient was calculated. The time at risk was determined from the date of first ESRD service after Jan. 1, 1990, to Dec. 31, 2004, the last date of USRDS data collection period in this dataset. Patients were censored at kidney transplantation or at the end of follow-up. Incidence rate ratios (IRRs) of hospitalization were calculated using Poisson regression modeling, with clustering of observations by patient to account for repeated measurements. All models were tested for goodness of fit. Confounders included in the analysis were age, gender and race. P-values less than 0.05 were considered significant.
The number of days hospitalized per time at risk was calculated and compared by Student t-test. A sensitivity analysis was performed after exclusion of outliers, defined as patients with a number of hospitalizations or hospitalized days greater than 1.5 times the interquartile range for that period.
In order to determine if there was a difference in mortality between hospitalized patients with SLE and hospitalized patients with other causes of ESRD, Cox proportional hazard models were constructed to determine the hazard ratio (HR) of death. In these models, the population was the hospitalized patients identified in the above analysis with the time at risk Jan. 1, 1990–Dec. 31, 2004, and patients were excluded if they received kidney transplant or were lost to follow-up. The proportional hazards assumption was not violated for any variable over time (p values >0.05 by means of global test of Schoenfeld residuals). Data were analyzed using STATA, version 9 (Stata Corporation, College Station, TX).
Results
There were a total of 359,633 patients identified who were maintained on hemodialysis (HD) between Jan. 1, 1990, and Dec. 31, 2004. There were 9930 patients with ESRD secondary to SLE, 619 pediatric patients with an age at first ESRD dialysis service ≤18 years, and 9311 adults with SLE. Demographic characteristics are presented in Table 1.
Table 1.
Demographic characteristics of cohort
|
SLE causing ESRD
|
Other causes of ESRD
|
|||
|---|---|---|---|---|
| Peds N = 619 | Adults N = 9311 | Peds N = 9733 | Adults N = 340,000 | |
| Mean age at initiation of HD (years (SD)) | 15.8 (2.5) | 35.9 (12.3) | 11.7 (5.7) | 53.1 (15.9) |
| Years on HD (SD) | 2.7 (4.1) | 1.1 (2.3) | 1.4 (3.3) | 0.7 (2.1) |
| % Black race | 73 | 63 | 40 | 48 |
| % Female | 82 | 86 | 48 | 50 |
Pediatric patients with ESRD secondary to SLE were older with an increased female and black race predominance compared to other pediatric patients (p-value < 0.01). Adults with ESRD secondary to SLE were younger with an increased female and black race percentage compared to other adults (p-value<0.01). SLE: systemic lupus erythematosus: ESRD: end-stage renal disease; HD: hemodialysis; SD: standard deviation.
Pediatric patients with SLE were older than other pediatric patients with ESRD maintained on HD; in contrast, adult patients with SLE were younger than other adult patients with ESRD (p < 0.01). There was an increased percentage of female gender and African American race in patients with SLE, both pediatric and adult populations, compared to other patients (p < 0.01).
Pediatric HD patients with ESRD secondary to SLE had a trend toward a higher rate of hospitalization compared to other pediatric patients, although it did not reach statistical significance (IRR: 1.08, 95% CI: 0.9–1.4). Even after controlling for age, race and gender, the trend remained (IRR: 1.04, 95% CI: 0.8–1.34). African American pediatric patients with SLE had a higher rate of hospitalization compared to Caucasians (IRR: 3.8, 95% CI: 1.7–8.5). Female pediatric patients with SLE also had a higher rate of hospitalization compared to males (IRR: 4.7, 95% CI: 1.7–12.8). The number of days hospitalized is shown in Table 2.
Table 2.
Interquartile range of hospitalized days by age and diagnosis
| Pediatric patients |
Adult patients |
|||
|---|---|---|---|---|
| Percentile | SLE | Other | SLE | Other |
| 25 | 2 | 2 | 2 | 2 |
| 50 | 5 | 4 | 5 | 4 |
| 75 | 9 | 7 | 8 | 8 |
| mean | 7.2 | 6.4 | 7.3 | 7 |
There was no significant difference in hospitalized days by interquartile percentage rank. However, the mean number of hospitalized days was higher in pediatric and adult patients with SLE. SLE: systemic lupus erythematosus.
The mean number of days hospitalized was higher in the pediatric patients with SLE compared to the others (7.2 vs. 6.4, p = 0.01).
There were a myriad of reasons for hospitalizations. The top three reasons for hospitalization in pediatric patients with SLE, excluding the diagnosis of SLE, were infection (8%), complications from surgical procedure (7%) and hypertension (6%). For other pediatric patients, the three most common reasons for hospitalizations included arteriovenous (AV) graft complication (12%), infection of dialysis access (6%) and sepsis (3%).
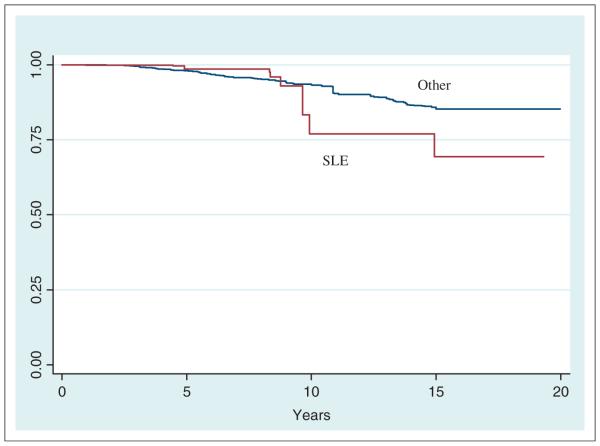
There was an increased risk of death in the hospitalized pediatric patients with ESRD secondary to SLE compared to pediatric patients with other causes of ESRD (HR: 2.01, 95% CI: 1.75–2.31) (Figure 1); 308 pediatric patients with SLE and 2556 patients with other causes of ESRD died during follow-up.
Figure 1. Kaplan-Meier comparison of hospitalized pediatric patients with ESRD.
Pediatric patients with SLE had a two-fold higher risk of death compared to pediatric patients with other causes of ESRD; SLE: systemic lupus erythematosus; ESRD: end-stage renal disease.
The three most frequent reasons for death in the pediatric patients with SLE included cardiac arrest (36%), septicemia (20%) and cerebro-vascular accident (13%). In those without SLE, cardiac arrest occurred in 21%, other causes of death in 20%, and septicemia in 6%.
Adult patients with ESRD secondary to SLE had an increased rate of hospitalization compared to other adult patients (IRR: 1.43, 95% CI: 1.15–1.77). Patients with SLE were hospitalized longer compared to their counterparts without SLE (7.3 days vs. seven days, p = 0.02). Even after controlling for age, race and gender, there was a significant difference in hospitalization between the adult groups, with a higher rate in the adults with SLE compared to others (IRR: 1.36, 95% CI: 1.51–1.97).
The three most frequent reasons for hospitalization in the adult patients with SLE included HD access infection (7%), hypertension (6%) and heart failure (4%). In those without SLE, 14% were hospitalized for infection, 7% for heart disease and 6% for hypertension.
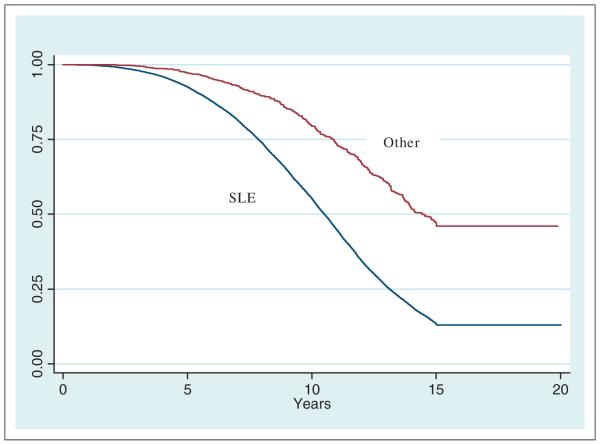
Patients who died during follow-up included 5478 adults with SLE and 270,821 patients with other causes of ESRD. In adjusted analysis, hospitalized adults with SLE had a higher risk of death compared to adults with other causes of ESRD (HR: 1.72, 95% CI: 1.51–1.97) (Figure 2).
Figure 2. Kaplan-Meier comparison of hospitalized adult patients with ESRD.
Adult patients with ESRD secondary to SLE had a higher risk of death compared to other adults; SLE: systemic lupus erythematosus; ESRD: end-stage renal disease.
The three top reasons for death in the adults with SLE included cardiac arrest (21%), other/unknown (12%) and septicemia (11%). In those with other causes of ESRD, the causes of death included cardiac arrest (24%), acute myocardial infarction (9%) and other/unknown (8%).
There was an increased rate of hospitalization in adults with ESRD secondary to SLE compared to the pediatric SLE population (IRR 1.23, 95% CI: 1.03–1.47), but no difference in the length of hospitalization (7.2 days vs. 7.3 days, p = 0.8). However, the risk of death was higher in the hospitalized pediatric SLE population compared to hospitalized adults with SLE (HR: 2.05, 95% CI: 1.79–2.34).
Discussion
In this study, we found that adult HD patients with ESRD secondary to SLE had a higher risk of hospitalization compared to patients with ESRD secondary to other causes. Although there was a trend toward increased risk of hospitalizations in pediatric patients with SLE, it was not statistically significant.
Hospitalizations for patients with SLE have increased over time. In a report from the Centers for Disease Control, in 1988 there were <60,000 admissions for adults with SLE; this increased to >100,000/year by 2000. An analysis of 2004 data from the Nationwide Inpatient Sample estimated 141,000 hospitalizations with a diagnosis of SLE. Hospitalized patients with SLE were more likely to be younger, of the black race and female compared to patients without lupus. Patients with SLE also had longer length of hospital stay compared to other patients.8–10 For patients with ESRD, overall hospitalization rates have remained stable, with approximately two admissions per year per dialysis patient with a mean hospitalization stay of 14 days.11
In this study of HD patients, there was a striking increase in the risk of death in hospitalized children and adults with SLE compared to patients with ESRD secondary to other causes. This risk was increased in the pediatric patients with SLE even when compared to hospitalized adults who also had ESRD secondary to SLE. The most common reason for death among pediatric and adult patients with SLE was secondary to cardiovascular disease.
In a prior study of the USRDS, we found that mortality was higher in pediatric and adult patients with ESRD secondary to SLE compared to other patients.6 In this current study, the mortality rate was high even when focusing on just the hospitalized patients with ESRD and SLE. Interestingly, the most common reason for hospitalizations in both the pediatric and adult populations was infections, not cardiovascular disease.
Patients with SLE are often immunosuppressed for treatment of their underlying disease, and this can increase the risk of infections. Cytomegalovirus (CMV) antigenemia has been reported in 18%–44% of patients with SLE, and antigen concentrations are higher in patients after treatment with glucocorticoids or cyclophosphamide.12
There have been reports of atherosclerosis associated with CMV infections. Heart transplant recipients who were positive for CMV antibody had a higher incidence of atherosclerosis compared to CMV-negative recipients.13 Animal models have shown that mice infected with CMV had a significant increase in pro-inflammatory cytokines as well as an increase in arterial blood pressure.14 It is not clear if there is a link between infections and cardiovascular disease in patients with SLE, but it is an intriguing possibility.
SLE is a chronic inflammatory condition and this environment may contribute to the development of cardiovascular disease. C-reactive protein and tumor necrosis factor-a, markers of inflammation, have been shown to be elevated in atherosclerotic disease. Increased carotid intimamedia thickness, a surrogate of subclinical atherosclerosis, has been shown to be increased in pediatric and adult patients with SLE.15–18 In addition, increased disease activity and damage scores in adults with SLE correlate with atherosclerosis.19 In the USRDS dataset, there is no information on disease activity in patients with SLE, and we are not able to assess cardiovascular disease and inflammation in these patients. One hypothesis for the increased cardiovascular deaths in the pediatric SLE population, however, may be due to a chronic inflammatory state compared to other patients with ESRD.
This study is limited by the retrospective nature of the data. Sicker patients may have died before data was recorded in the USRDS, or may have been placed on hemodialysis rather than peritoneal dialysis or transplant. This may lead to a selection bias, excluding the sickest patients from the analysis. In addition, we cannot comment on SLE disease activity or medications that were used to treat patients with SLE, as this data were not included in the USRDS dataset. This may impact the risk for cardiovascular disease, as patients treated with glucocorticoids may have lipid abnormalities that predispose them to cardiovascular disease.
Using this large national dataset, we show that there is a trend toward higher hospitalization rates in pediatric patients with SLE and a significant difference in hospitalizations between adult patients with SLE and patients with ESRD secondary to other causes. In pediatric as well as adult SLE patients who were hospitalized, there was an increased risk of death, primarily due to cardiovascular disease. This suggests that pediatric and adult patients with ESRD secondary to SLE should be carefully monitored for risk factors for cardiovascular disease, including non-conventional risk factors such as reducing infections and controlling inflammation that may contribute to atherosclerosis.
Acknowledgments
Funding
This work was supported by a National Institutes of Health grant 5K23AR052736 under Dr. Sule.
Footnotes
Reprints and permissions: http://www.sagepub.co.uk/journalsPermissions.nav
Conflict of interest
None declared.
References
- 1.Jimenez S, Cervera R, Font J, Ingelmo M. The epidemiology of systemic lupus erythematosus. Clin Rev Allergy Immunol. 2003;25:3–12. doi: 10.1385/CRIAI:25:1:3. [DOI] [PubMed] [Google Scholar]
- 2.Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58:15–25. doi: 10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- 3.Stichweh D, Arce E, Pascual V. Update on pediatric systemic lupus erythematosus. Curr Opin Rheumatol. 2004;16:577–587. doi: 10.1097/01.bor.0000137852.42270.0f. [DOI] [PubMed] [Google Scholar]
- 4.Kamphuis S, Silverman ED. Prevalence and burden of pediatric-onset systemic lupus erythematosus. Nat Rev Rheumatol. 2010;6:538–546. doi: 10.1038/nrrheum.2010.121. [DOI] [PubMed] [Google Scholar]
- 5.Bogdanovic R, Nikolic V, Pasic S, et al. Lupus nephritis in childhood: a review of 53 patients followed at a single center. Pediatr Nephrol. 2004;19:36–44. doi: 10.1007/s00467-003-1278-y. [DOI] [PubMed] [Google Scholar]
- 6.Sule S, Fivush B, Neu A, Furth S. Increased risk of death in pediatric and adult patients with ESRD secondary to lupus. Pediatr Nephrol. 2011;26:93–98. doi: 10.1007/s00467-010-1640-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Renal Data System USRDS 2004 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. 2004 www.usrds.org. [Google Scholar]
- 8.Urowitz MB, Gladman DD, Tom BD, Ibanez D, Farewell VT. Changing patterns in mortality and disease outcomes for patients with systemic lupus erythematosus. J Rheumatol. 2008;35:2152–2158. doi: 10.3899/jrheum.080214. [DOI] [PubMed] [Google Scholar]
- 9.Krishnan E. Hospitalization and mortality of patients with systemic lupus erythematosus. J Rheumatol. 2006;33:1770–1774. [PubMed] [Google Scholar]
- 10.Ward MM. Hospital experience and mortality in patients with systemic lupus erythematosus: which patients benefit most from treatment at highly experienced hospitals? J Rheumatol. 2002;29:1198–1206. [PubMed] [Google Scholar]
- 11.Foley RN, Collins AJ. End-stage renal disease in the United States: an update from the United States Renal Data System. J Am Soc Nephrol. 2007;18:2644–2648. doi: 10.1681/ASN.2007020220. [DOI] [PubMed] [Google Scholar]
- 12.Berkun Y, Zandman-Goddard G, Barzilai O, et al. Infectious antibodies in systemic lupus erythematosus patients. Lupus. 2009;18:1129–1135. doi: 10.1177/0961203309345729. [DOI] [PubMed] [Google Scholar]
- 13.Grattan MT, Moreno-Cabral CE, Starnes VA, Oyer PE, Stinson EB, Shumway NE. Cytomegalovirus infection is associated with cardiac allograft rejection and atherosclerosis. JAMA. 1989;261:3561–3566. [PubMed] [Google Scholar]
- 14.Cheng J, Ke Q, Jin Z, et al. Cytomegalovirus infection causes an increase of arterial blood pressure. PLoS Pathog. 2009;5:e1000427. doi: 10.1371/journal.ppat.1000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schanberg LE, Sandborg C, Barnhart HX, et al. Premature atherosclerosis in pediatric systemic lupus erythematosus: risk factors for increased carotid intima-media thickness in the atherosclerosis prevention in pediatric lupus erythematosus cohort. Arthritis Rheum. 2009;60:1496–1507. doi: 10.1002/art.24469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roman MJ, Shanker BA, Davis A, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med. 2003;349:2399–2406. doi: 10.1056/NEJMoa035471. [DOI] [PubMed] [Google Scholar]
- 17.Asanuma Y, Kawai S, Aoshima H, Kaburaki J, Mizushima Y. Serum lipoprotein(a) and apolipoprotein(a) phenotypes in patients with rheumatoid arthritis. Arthritis Rheum. 1999;42:443–447. doi: 10.1002/1529-0131(199904)42:3<443::AID-ANR8>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 18.Petri M, Perez-Gutthann S, Spence D, Hochberg MC. Risk factors for coronary artery disease in patients with systemic lupus erythematosus. Am J Med. 1992;93:513–519. doi: 10.1016/0002-9343(92)90578-y. [DOI] [PubMed] [Google Scholar]
- 19.Shang Q, Tam LS, Li EK, Yip GW, Yu CM. Increased arterial stiffness correlated with disease activity in systemic lupus erythematosus. Lupus. 2008;17:1096–1102. doi: 10.1177/0961203308092160. [DOI] [PubMed] [Google Scholar]