Abstract
We describe 2 cases of reversible cerebral vasoconstriction syndrome (RCVS) with refractory headache aborted by intravenous magnesium. Case 1 is a 53-year-old woman with subarachnoid hemorrhage due to RCVS presented with refractory headache and persistent vasospasm, despite aggressive treatment with calcium channel blockers (CCBs) and systemic corticosteroids. Subsequently, she experienced dramatic relief of symptoms with intravenous magnesium therapy. She continued oral maintenance therapy and remained symptom free. Case 2 is a 71-year-old female with bilateral temporo-occipital infarcts due to RCVS, presented with refractory headache and persistent vasospasm on transcranial Doppler (TCD), despite aggressive treatment with CCBs. She experienced dramatic relief of symptoms with intravenous magnesium and resolution of vasospasm on TCD. Magnesium may be beneficial for the treatment of refractory headaches in patients with RCVS. Future studies are needed to determine whether it should be considered as a first-line agent.
Keywords: reversible cerebral vasoconstriction syndrome, headache, transcranial Doppler (TCD), magnesium
Introduction
Reversible cerebral vasoconstriction syndrome (RCVS) is a vasculopathy that typically presents with thunderclap headache and can be associated with neurological deficits.1 Associated complications include ischemic infarcts, intracerebral hemorrhage, and subarachnoid hemorrhage.2 Since the pathophysiology includes vasospasm, calcium channel blockers (CCBs) have been used to treat symptoms, particularly headache. While most patients are thought to benefit from this therapy, there are limited data to support its use. In the largest RCVS case series, Singhal et al described a benefit of CCB monotherapy.3 While most patients have improvement in headache symptoms with CCB, a small proportion have refractory symptoms. We report 2 cases of RCVS who improved dramatically after treatment with magnesium. Informed consent was obtained from both the patients. The report is exempt from full institutional review board review because it is a short case series.
Case 1
A 53-year-old woman presented with a severe headache of sudden onset. Her neurological examination was normal. Initial computed tomography (CT) scan of the head showed subarachnoid hemorrhage over the right medial aspect of the frontal and parietal lobes. She underwent a cerebral angiogram, which revealed focal narrowing of the pericallosal artery (Figure 1) and was diagnosed with RCVS. Prior to onset of symptoms, she had been taking paroxetine for depression, which was discontinued. She was started on verapamil and discharged home. She continued to have severe headaches during follow-up. The dosing of verapamil was increased on multiple occasions up to 240 mg daily. She presented to the emergency department with persistent headaches and was given 2 g of intravenous magnesium. She reported relief within 15 minutes of initiation of the infusion. Patient was continued on magnesium oxide 200 mg twice a day. A CT angiogram (CTA) of the brain did not show any focal or diffuse narrowing suggesting any vasospasm. During follow-up clinic visits, she reported no headaches.
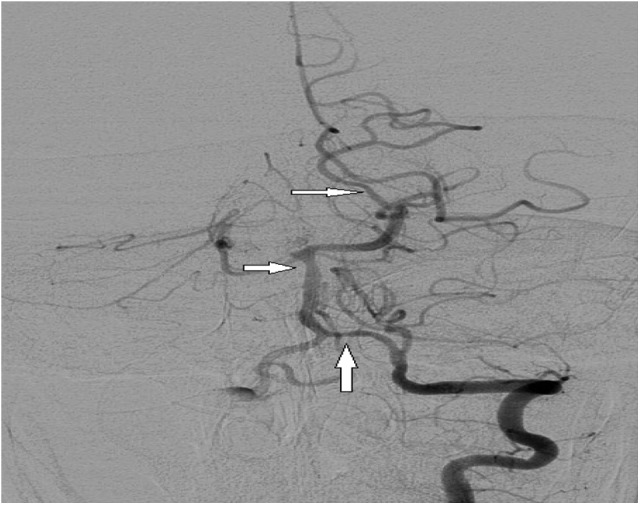
Figure 1.

Cerebral angiogram showing spasm of the pericallosal artery.
Case 2
A 71-year-old woman presented with a severe headache of sudden onset. Her neurological examination showed a right inferior visual field deficit. Magnetic resonance imaging of the brain showed an acute infarct of the bilateral parieto-occipital lobes. She underwent a cerebral angiogram, which revealed focal narrowing of the left vertebral, basilar and left posterior cerebral arteries and was diagnosed with RCVS (Figure 2). She also underwent transcranial Doppler (TCD) which showed elevated velocities in the vertebral (76 cm/s) and basilar (72 cm/s) arteries. Prior to the onset of symptoms, she had been taking pseudoephedrine for nasal congestion. She was started on verapamil and discharged home. She continued to have severe headaches during follow-up. Repeat TCD revealed persistently elevated velocities in the vertebral (79 cm/s) and basilar (73 cm/s) arteries. The dose of verapamil was increased on multiple occasions up to 240 mg daily. She presented to the emergency department with persistent headaches and was given 4 g of intravenous magnesium. She reported relief within 15 minutes of initiation of the infusion. Transcranial Doppler revealed normal velocities in vertebral (41 cm/s) and basilar (35 cm/s). During follow-up clinic visits, she reported no headaches and continues on oral magnesium oxide 200 mg once daily.
Figure 2.
Cerebral angiogram showing spasm of left vertebral, basilar, and posterior cerebral artery.
Discussion
Reversible cerebral vasoconstriction syndrome is cerebrovascular syndrome that predominantly affects women aged 20 to 50.3,4 The prominent symptom is thunderclap headache. Headaches are typically diffuse and may be associated with photophobia, phonophobia, nausea, and vomiting. The pathophysiology involves diffuse, multifocal narrowing of intracranial arteries. Vasospasm is thought to be secondary to disturbance of vascular tone control of intracranial vessels.3-5 Reversible cerebral vasoconstriction syndrome is often idiopathic but has been associated with childbirth, serotonergic antidepressants, sympathomimetics, and dopaminergic drugs.3-5 The diagnosis is usually established through intracranial vascular studies such as TCD, magnetic resonance angiography (MRA), CTA, and conventional angiography.6,7 Because vasospasm is seen on imaging studies, CCBs have been widely used with improvement in headache symptoms in most patients. Resolution of headache usually occurs by 6 months.3-7 However, there is a subset of patients who do not respond to CCBs.8 Some of these patients can have significant morbidity and mortality.9,10
There are no significant predictors of clinical worsening in patients with RCVS; however, peri- and postpartum statuses have been suggested as risk factors.9,10 Additionally, Singhal et al found that focal neurologic deficits and use of glucocorticoids in treatment are independent predictors of poor outcome. Reports have been published on the use of magnesium as a second-line treatment for these patients.9,10 This approach stems from the experience of magnesium as a prophylactic agent for preventing vasospasm in aneurysmal subarachnoid hemorrhage (SAH), with studies ultimately showing minor or no benefit in SAH.11,12 Magnesium has been reserved for patients having RCVS, with deterioration leading to worsening of neurological deficits. It is also mainly used in peri- and or postpartum patients because of its proven safety profile in these patients.9,10
We describe the use of intravenous magnesium as an abortive therapy in nonpregnant females with dramatic improvement. Our second patient provides neurosonologic evidence of resolution of vasospasm after treatment with magnesium. We propose that intravenous magnesium should be considered as an abortive therapy even in the initial phase of the presentation instead of waiting for clinical worsening. Moreover, oral formulations can be used as a maintenance therapy. Some patients have devastating outcomes, therefore there may be a role for prospectively monitoring patients on different therapy regimens clinically as well with noninvasive techniques such as TCD or MRA for effectiveness.6-8
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Call GK, Fleming MC, Sealfon S, Levine H, Kistler JP, Fisher CM. Reversible cerebral segmental vasoconstriction. Stroke. 1988;19(9):1159–1170. [DOI] [PubMed] [Google Scholar]
- 2. Ducros A, Bousser MG. Reversible cerebral vasoconstriction syndrome. Pract Neurol. 2009;9(5):256–267. [DOI] [PubMed] [Google Scholar]
- 3. Singhal AB, Hajj-Ali RA, Topcuoglu MA, et al. Reversible cerebral vasoconstriction syndromes: analysis of 139 cases. Arch Neurol. 2011;68(8):1005–1012. [DOI] [PubMed] [Google Scholar]
- 4. Ducros A, Boukobza M, Porcher R, Sarov M, Valade D, Bousser MG. The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome. A prospective series of 67 patients. Brain. 2007(130):3091–3101. [DOI] [PubMed] [Google Scholar]
- 5. Chen SP, Fuh JL, Lirng JF, Chang FC, Wang SJ. Recurrent primary thunderclap headache and benign CNS angiopathy: spectra of the same disorder? Neurology. 2006;67(12):2164–2169. [DOI] [PubMed] [Google Scholar]
- 6. Chen SP, Fuh JL, Chang FC, Lirng JF, Shia BC, Wang SJ. Transcranial color doppler study for reversible cerebral vasoconstriction syndromes. Ann Neurol. 2008;63(6):751–757. [DOI] [PubMed] [Google Scholar]
- 7. Chen SP, Fuh JL, Wang SJ, et al. Magnetic resonance angiography in reversible cerebral vasoconstriction syndromes. Ann Neurol. 2010;67(5):648–656. [DOI] [PubMed] [Google Scholar]
- 8. Katz BS, Fugate JE, Ameriso SF, et al. Clinical worsening in reversible cerebral vasoconstriction syndrome. JAMA Neurol. 2014;71(1):68–73. [DOI] [PubMed] [Google Scholar]
- 9. Fugate JE, Wijdicks EF, Parisi JE, et al. Fulminant Postpartum Cerebral Vasoconstriction Syndrome. Arch Neurol. 2012;69(1):111–117. [DOI] [PubMed] [Google Scholar]
- 10. Singhal AB. Postpartum Angiopathy with reversible posterior leukoencephalopathy. Arch Neurol. 2004;61(3):411–416. [DOI] [PubMed] [Google Scholar]
- 11. Dorhout Mees SM, Algra A, Vandertop WP, et al. ; MASH-2 study group. Magnesium for aneurysmal subarachnoid haemorrhage (MASH-2): a randomised placebo-controlled trial. Lancet. 2012;380(9836):44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reddy D, Fallah A, Petropoulos JA, Farrokhyar F, Macdonald RL, Jichici D. Prophylactic magnesium sulfate for aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurocrit Care. 2014;(21):356–364. [DOI] [PubMed] [Google Scholar]


