Abstract
Purpose of the Study:
Demographic projections suggest that the older Latino population will experience the fastest growth among all racial/ethnic groups; and by 2050 will constitute 20% of the nation’s seniors. Yet, Latino Alzheimer’s elders and their families remain underrepresented in the health care system and caregiver intervention studies. To address this gap, this study tested the effectiveness of Circulo de Cuidado, a culturally-sensitive, cognitive behavioral (CBT) group intervention, in supporting Latino families’ ability to manage the disease’s neuropsychiatric symptoms and improve caregiver well-being.
Design and Methods:
Using a randomized controlled trial design, 67 caregivers were assigned to the CBT experimental condition or the psychoeducational (PED) control condition and interviewed at baseline, post-group, and 3 months follow-up. The 2 manualized interventions had the same structure: 5 weekly 90-minute group sessions, followed by telephone coaching at 3, 6, 9 and 12 weeks post-group.
Results:
Repeated measures analysis of covariance revealed significant group by time interaction effects. Compared with the PED participants, CBT participants reported lower neuropsychiatric symptoms in their relative, less caregiver distress about neuropsychiatric symptoms, a greater sense of caregiver self-efficacy, and less depressive symptoms over time.
Implications:
Our findings offer preliminary evidence that a culturally tailored, CBT group intervention targeted toward neuropsychiatric symptom management has positive psychological benefits for Latino caregivers.
Key Words: Alzheimer’s disease, Caregiver stress, Intervention, Latino/a, Psychosocial, Caregiving—informal, Cultural competence practice
Demographic projections indicate that the older Latino population will experience the fastest growth among all older racial and ethnic groups in the United States during the next several decades. In 2010, slightly less than 2.8 million or 6.9% of Americans 65 and older self-identified as being Hispanic of any race; yet, it is estimated that by 2050 the older Latino population will reach 17.5 million and constitute 20% of the nation’s seniors (Federal Interagency Forum on Aging-Related Statistics [FIFARS], 2012). As is true of the entire 65-plus population in the United States, the older Latino population is not only growing in size, but it is also growing older. In fact, Latinos, on average, now experience greater longevity than do non-Latino Whites and African Americans. Longer life expectancy is a tremendous success story; however, advanced old age is also associated with greater risk for a number of chronic health conditions, including Alzheimer’s disease and related dementias (ADRD; FIFARS, 2012). Evidence suggests that older Latino adults are approximately 1.5 times more likely to have ADRD than older White adults (Gurland et al., 1999). It is estimated that dementia rates among U.S. Latinos will increase sixfold, rising from 200,000 to 1.3 million by 2050 (Novak & Riggs, 2004). Some research also suggests an earlier average age for ADRD onset in Latinos as compared with Whites in the United States. Clark and colleagues (2007), for example, found that Latinos exhibited dementia symptoms on average 6.8 years earlier than did Anglos.
Despite these statistics, there is ample evidence that many Latino elders and their family members are not receiving services to reduce their risk or manage their dementia. Research has documented a number of reasons why Latinos are underrepresented in the formal care system, including health insurance, linguistic, and cultural barriers (Aranda, Villa, Trejo, Ramírez, & Ranney, 2003). Cultural insensitivity on the part of formal care providers, for example, can lead to a sense of mistrust and/or disappointment in the health care system for many Latinos. In the Latino culture, confianzo (trust) takes time and it is important to develop relationships; thus, personalismo (a sense of personal connection) and continuity in care provider are highly desired. The current reality is that Latinos are more likely to receive the diagnosis at later stages of the disease and thus are less likely to access early interventions or treatments (Ayalon & Arean, 2004). Developing formal services to support Latino caregivers is of crucial importance as Latino elders are more likely to be living with relatives than Anglo elders. Among Latino women aged 65 and older, almost 80% live with a spouse or another relative (FIFARS, 2012). Familismo (a strong sense of family), respeto (respect) for elders, and a commitment to care for vulnerable loved ones are strengths of the Latino community. Ultimately, the earlier age of onset of the dementia, coupled with their longer life expectancy, means that Latino families may be providing care for much longer periods of time than non-Latino families.
Latinos also remain underrepresented in ADRD caregiver intervention research. Llanque and Enriquez’s (2012) literature review found only 10 intervention studies published between 2000 and 2011, which specifically targeted interventions for Latino caregivers of dementia relatives. Seven of these 10 studies were part of the National Institutes of Health (NIH)-funded Resources for Enhancing Alzheimer’s Caregiver Health Study (REACH) I and II study (Elliott, Burgio, & Decoster, 2010; Wisniewski et al., 2003). The majority of the 10 studies were conducted in California and Florida, in large urban areas in which the Latino communities—primarily Mexican or Cuban American communities—have been established for decades or centuries (Llanque & Enriquez, 2012). Yet, there are now 16 states that have at least a half million Latino residents. And, as often emphasized, the Latino population in the United States is very heterogeneous; it is comprised of individuals of different racial backgrounds, which come from more than 20 different countries.
The purpose of this study was to address this critical resource need through the development and evaluation of Circulo de Cuidado (Circle of Care), a Spanish language, culturally sensitive, targeted cognitive behavioral (CBT) group intervention for Latino ADRD caregivers coping with their relatives’ neuropsychiatric symptoms. Circulo de Cuidado’s primary focus on neuropsychiatric symptom management was driven by evidence that these symptoms (i.e., agitation, apathy, depression, hallucination), which are reported in more than 80% of ADRD persons, are associated with marked functional decline in the patient and are a source of considerable distress for their caregivers. Disruptive behaviors, such as wandering, agitation, and verbal assaults, have consistently been found to be associated with a decrease in psychological well-being and an increase in distress and burden among caregivers (Gaugler, Davey, Pearlin, & Zarit, 2000; Pinquart & Sorensen, 2003). These neuropsychiatric symptoms (or problem behaviors) are also a leading precipitant to nursing home placement (de Vugt et al., 2005). Finally, some research suggests that Latino elders with dementia exhibit a higher level of functional impairment and greater number of dementia-related problem behaviors than do Anglo elders (Pinquart & Sorensen, 2005; Sink, Covinsky, Newcomer, & Yaffe, 2004).
The decision for Circulo de Cuidado to be an individualized, targeted, CBT group intervention was informed by the past two decades of psychosocial caregiver intervention research, particularly the NIH REACH I and II studies. Importantly, since 2001, there have been a series of systematic reviews and meta-analyses, which suggest that individualized, targeted, multicomponent interventions may be more effective than education alone or broader psychoeducational (PED) interventions (Acton & Kang, 2001; Brodaty, Green, & Koschera, 2003; Cooke, McNally, Mulligan, Harrison, & Newman, 2001; Gallagher-Thompson & Coon, 2007; Pinquart & Sorensen, 2006; Schulz et al., 2002; Selwood, Johnston, Katona, Lyketsos, & Livingston, 2007; Yin, Zhou, & Bashford, 2002. Circulo de Cuidado is based on a prior CBT group intervention, Project Care that demonstrated success in improving Anglo ADRD caregivers’ psychological well-being and in which the principal investigator was a team member (Gonyea, O’Connor, & Boyle, 2006). A number of modifications were introduced, however, to increase its relevancy for Latino caregivers, including changes in the recruitment approach, curriculum content, and the delivery methods. Underlying all was a perspective that language and culture provide the experiential context for the understanding of health. Our culturally bound beliefs, values, and preferences influence how we interpret health and illness as well as health care messages. Offering the intervention in Spanish, through bilingual MSW social workers with extensive practice experience in the Latino community, removed linguistic barriers and allowed participants to better articulate the nature of their caregiving experience within their own cultural framework.
We view the study as making several contributions to the field. Importantly, it is first Latino caregiver intervention study to specifically target neuropsychiatric symptom management. As previously noted, research suggests that Latinos experience a greater number of dementia-related problem behaviors than do Anglos (Chen, Borson, & Scanlan, 2000; Sink, Covinsky, Newcomer, & Yaffe, 2004). Although there are conflicting findings regarding the impacts of neuropsychiatric symptoms on Latino caregivers’ well-being, perhaps partly due to differences in the subgroups studied (i.e., Cuban Americans and Mexican Americans) and use of different mental health measures, Hinton and his colleagues argue that “more research is needed on the relationship of neuropsychiatric symptoms in demented patients to Latino caregiver mental health, especially in view of studies showing that Latino caregivers suffer higher rates of depression compared with European American caregivers” (Hinton, Haan, Geller, & Mungas, 2003, p. 670).
Responding to the paradigm shift in social science research away from viewing Latinos or Hispanics as a monolithic group, the study extends the Alzheimer’s caregiver intervention research to two understudied subpopulations of Latinos—individuals whose nations of origin were Puerto Rico or the Dominican Republic—as well as to a relatively understudied region of the nation, New England (Losada et al., 2006). Finally, this study, which uses a CBT framework, is still one of a relatively small number of scientifically rigorous evaluations of a theoretically driven, culturally tailored caregiver intervention with Latino populations. Napoles and her colleagues’ (2010) systematic review of dementia caregiver intervention studies published between 1980 and 2009 found only 18 out of 47 articles reported outcomes by caregiver ethnicity and only 11 reported cultural tailoring, of which 8 were from the REACH initiative (Napoles, Chadiha, Eversley, & Moreno-John, 2010).
Methods
Design and Hypotheses
This study was conducted in urban communities in eastern Massachusetts, a state in which the Latino population is predominately from Puerto Rico and the Dominican Republic. A randomized controlled trial was used to evaluate the efficacy of Circulo de Cuidado; through block randomization, caregivers were assigned to one of two study arms: the CBT treatment experimental condition or the PED control condition. The decision to have a PED group control condition was based on feedback from community advisors that a wait-list control group strategy would not be well received. For both ethical reasons and to recruit and retain participants, it was felt important to offer something to families in the control condition. Many Latino families expressed frustrations with “being stuck on waiting lists” and “feeling disrespected” by agencies. Also, individuals, particularly those who entered the country without documents, were very wary of being placed on any list. As the most widely available resource for ADRD families, the PED condition was viewed as the “standard care.”
The study’s design and methods were approved by the Boston University Institutional Review Board. Participants were interviewed in Spanish in their homes by trained bilingual interviewers prior to the start of the group intervention (baseline), at the end of the group (post-test), and three months later (follow-up) to assess the intervention effects. Post-test and follow-up, it was predicted that CBT participants, as compared with PED participants, would report the following: [H1] lower levels of neuropsychiatric symptom severity in their ADRD relatives; [H2] lower levels of caregiver neuropsychiatric symptom distress; [H3] a greater sense of caregiver self-efficacy; [H4] lower levels of caregiver depressive symptoms; and [H5] lower levels of caregiver anxiety.
A Culturally Sensitive Framework
In addition to the use of Spanish language and bilingual staff, efforts were undertaken to incorporate themes, messages, and materials, which were consistent with the values, beliefs, and lived experiences of the Latino Alzheimer’s families in all phases of the research project. In Massachusetts, approximately 53% of Latinos are foreign-born or born in a U.S. territory. Similar to other immigrant groups in the United States, immigrant Latinos often face a multitude of challenges, including acculturation stress, race/ethnic discrimination, and linguistic isolation. Among all racial/ethnic groups in Massachusetts, Latinos currently experience the highest rate of poverty; slightly more than one-third of Latinos live below the federal poverty level. Almost 3 out of 10 Latino adults have not completed high school. Nearly half of Massachusetts Latinos report speaking English “not very well”; only 19% of Latinos report speaking English only in their homes (Montel & Patten, 2012). It was anticipated that a significant number of study participants’ caregiving experiences would be impacted by the complex problems associated with discrimination, linguistic isolation, and financial insecurity, including unemployment or underemployment, substandard housing, and the presence of multiple chronic health problems. A broader social contextual framework was, therefore, adopted in the curriculum and by the group leaders to acknowledge the complexity of the families’ caregiving experiences, and case examples incorporated many of these previously identified themes. Finally, educational obtainment statistics underscored the need to ensure that the project’s visual materials would be accessible to individuals with lower literacy levels.
Prior research has highlighted racial and ethnic variation in knowledge and understanding of dementia; studies suggest that minority elderly and those with less formal education are more likely to attribute the neuropsychiatric symptoms associated with the disease to causes other than ADRD, including normal aging, personality, genetics, mental illness, and/or other medical conditions (Hinton, Chambers, & Velásquez, 2009). For many Latinos, the disease’s problem behaviors are thought to reflect a mental health versus a physical health problem—that is, the impacted person is seen as suffering from nervios (nerve problems) or thought to be loco (crazy) (Gallagher-Thompson, Solano, Coon, & Arean, 2003). Because of the significant social stigma of mental illness within the Latino culture, the presence of dementia can lead to denial, secrecy, and shame within the family. As Henderson and Guitierrez-Mayka (1992, p. 67) share, “The concepto de familia operates to diffuse the stigma of a single case of Alzheimer’s disease to all family members. If one has a stigmatized disease (e.g., is ‘crazy’), the entire family shares responsibility.” Recognizing these factors, as well as based on advice from community members, our outreach efforts used the words “problemas de memoria” (memory problems) versus dementia and described the intervention as educational (versus therapeutic) offering families the opportunity to “ganar habilidades para manejar major el cuidado de u ser quirido” (“learn tools to better manage care for your loved one”). An important beginning point in the intervention was a discussion on the etiology of Alzheimer’s, the disease stages and associated behavioral changes, and caregivers’ reactions to the diagnosis and behavioral changes. Finally, in the last session, reflecting the educational framework, participants received a certificate honoring their completion of the program; these certificates were highly valued by the families.
Familismo, the primary importance of family over the individual, has often been cited as a core value within the Latino culture. Although familismo is often presumed to be a protective factor against negative caregiver outcomes, past research has produced either mixed or relatively weak findings of an association (Losada et al., 2006). These findings may be partly attributable to the conceptualization (and measurement) of familism as a unidimensional construct. Recent theoretical and empirical work suggests that familism is multidimensional, including the domains of family obligation (i.e., cultural values requiring care of vulnerable members), family solidarity (i.e., cultural expectations that members will be supportive in times of need), and family as referents (i.e., the family sets the rules and guidance for individuals’ roles and behaviors; Knight & Sayegh, 2010; Losada et al., 2008). This multidimensional conceptualization informed our content of family communication and problem solving and led to a greater sensitivity as to how these values were experienced, internalized, and expressed by participants.
Finally, the importance of personalismo and confianzo to relationship building in the Latino culture shaped a number of project decisions. For example, a key decision was to place the intervention in the local communities—that is, we knew that it was less likely that individuals would travel outside of their physical and psychological sense of neighborhood to participate. Further, in each community, we formed partnerships with locally well-regarded organizations and typically offered the interventions in one of these sites. Research also suggests that clinicians who are experienced as cold or distant by their Latino clients will experience higher attrition rates (Aviera, 2002). Thus, in both conditions, the groups were small, informal, and highly interactive, involving a great deal of chatting. Each group chose the type of preferred refreshments and often suggested the use of a particular bodega. Each week the group leader arrived early and stayed late to provide ample time and space for mutual exchange.
Intervention Conditions
Both conditions incorporated the previously identified culturally sensitive framework, and each used a manualized five-week, 90-min weekly session model in which the small group didactic sessions were highly interactive. Participants had weekly at-home assignments; and, all received a caregiver manual that highlighted the core content of the five weekly sessions. Although prepared to offer the sessions and manuals in Spanish or English, based on participants’ preferences, all was done in Spanish. Again, participants received a certificate of completion in the final session.
The decision to limit the group intervention to five weeks was driven by a desire to create an intervention that would be feasible for both agencies to implement and families to participate in. As follow-up to the group experience, participants received brief 10–15-min coaching telephone calls from the group leader at 3-, 6-, 9-, and 12-weeks postgroup reinforcing the intervention’s core objectives. The follow-up telephone coaching was seen as a relatively low-cost strategy to be person-centered and extend or strengthen the intervention’s impact. Further, the follow-up telephone contact was viewed as respecting the cultural value of personalismo and honoring the relationship building that had occurred in the groups.
Experimental Condition
The CBT group intervention devoted a significant amount of time to teaching caregivers the rationale and use of the antecedents-behaviors-consequences (A-B-C) problem-solving approach to behavior change. Caregivers learned to set reasonable goals and practice behavior modification or activation techniques to make successive approximation to larger goals. Although delivered in a group setting, the particular behavior focus was individualized or tailored to the specific concerns of each caregiver. Increasing caregivers’ and care recipients’ engagement in pleasant activities and improving communication were also an important component of the intervention. Once again, the type of pleasant activities was individualized and defined by the participant. Additionally, caregivers were offered guidance in ways to better identify and manage their own distress. Weekly sessions always ended with the use of relaxation techniques or exercises. Throughout the sessions, the use of problem-solving exercises, often performed in smaller groups or pairs, led to very active engagement; individuals were encouraged to share their personal experiences and jointly practice the newly taught skills and techniques. The group leader used Bandura’s four identified self-efficacy enhancing strategies—mastery experience, modeling, social persuasion, and altering of emotional/somatic state—to reinforce caregivers’ sense of mastery of new skills. Participants’ weekly at-home assignments offered them the ability to practice the new skills/techniques and then report back and share their experiences with the group.
Control Condition
The PED condition’s sessions focused on educating caregivers about topics such as memory loss and the general progression of Alzheimer’s disease, tips to finding community resources, strategies for working together with doctors, home safety issues, and communication in the context of Alzheimer’s. Participants actively engaged in a series of group exercises such as “evaluate your stress level” and shared information about the types of challenges they faced, their own caregiving strategies, and tips on helpful local resources. Weekly at-home assignments include tasks such as completing an ADRD home safety checklist and identifying potentially needed modifications.
Participant Recruitment
As previously noted, we formed local partnerships with well-respected agencies. Yet despite agencies’ enthusiasm and support of our project, they typically did not know specific Latino ADRD families. Even in communities with sizeable Latino populations, older Latinos were often not part of, or only a very limited segment of, the aging agencies’ client bases. We also found that Latino organizations were more often focused on services for children, youth, and younger families rather than issues relevant to elders. Only one Spanish-speaking ADRD caregiver support group existed in the entire state. Thus, we came to view the Latino ADRD families as largely “hidden families.”
Several strategies were implemented for the recruitment of study participants, including: (a) professional outreach to local health care, home care, and housing staff, especially bilingual staff; (b) media outreach through community access television, radio, and neighborhood newspapers as well as postings in storefronts, (c) public speaking about aging and memory loss at community meetings, particularly at Latino organizations and senior housing sites, and (d) coordination with the Massachusetts/New Hampshire Alzheimer’s Association’s Latino outreach coordinator. Similar to Gallagher-Thompson and colleagues (2004), our highest recruitment rates were achieved through professional referrals, and we share their perception that Latino cultural values played a role in the success of these community partnerships. Typically, we found potential participants because of a single bilingual agency staff member who had a personal relationship with the family. Over the course of the study we experienced, much like the families, the fragile nature of these bonds. Limited bilingual staff, coupled with turnovers in personnel, often meant that there were significant periods of time during which agencies lacked Spanish-speaking staff.
The participant inclusion criteria were that the caregiver identifies (a) his/her ethnicity as Latino or of Hispanic origin, (b) she/he provided a minimum of 5hr weekly in direct caregiving, on average, in the past month, (c) the care recipient has been diagnosed with possible or probable Alzheimer’s disease, and (d) the care recipient is currently exhibiting at least one neuropsychiatric symptom. Individuals were not eligible to participate if the care recipient had a history of severe psychotic disorder (e.g., schizophrenia) or substance abuse. All interested individuals completed a brief telephone screen to determine their eligibility. If the caregiver was eligible and interested in participating, a baseline interview was scheduled. All individuals preferred to communicate in Spanish during all aspects of the study, including the telephone screen, the three interview sessions (pre-, post-, and follow-up), and the group experiences.
Figure 1 shows the flow of participants through the trial. Among the 90 individuals who sought information, 67 met the study’s eligibility criteria and completed baseline interviews. The primary reasons for ineligibility were that the care recipient was not currently exhibiting any neuropsychiatric symptoms, she/he had another type of dementia (i.e., Parkinson’s-related dementia or Lewy body dementia) or chronic disease (i.e., multiple sclerosis, stroke), or she/he was currently residing outside of Massachusetts and therefore not receiving the minimum hours of direct family care. In terms of the two arms of the study, 33 caregivers were randomly assigned to the CBT condition and 34 were randomly assigned to the PED condition. The attrition was low; the reasons for loss are reported in the flowchart. In total, 29 CBT condition caregivers and 28 PED condition caregivers completed all three assessments, pre-, post-, and follow-up.
Figure 1.
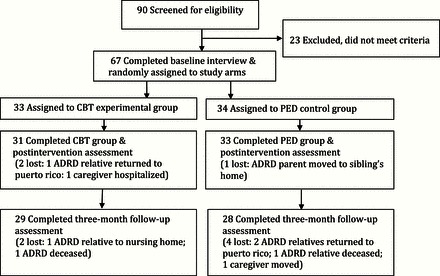
Flowchart of study participants. ADRD = Alzheimer’s disease and related dementias; CBT = cognitive behavioral therapy condition; PED = psychoeducational condition.
Measures
The primary outcome measures were caregiver’s assessment of the ADRD relative’s neuropsychiatric symptom severity, caregiver’s level of distress to the neuropsychiatric symptoms, caregiver’s sense of self-efficacy, caregiver depression, and caregiver anxiety. Each of the specific instruments is identified; as the Cronbach alphas remained stable across the three time points, only baseline Cronbach alphas are reported.
“Neuropsychiatric symptom severity” was tapped using a Spanish version of the Neuropsychiatric Inventory-Severity scale (NPI-S; Cummings et al., 1994; Hinton et al., 2003). The scale assesses the frequency and severity of 10 neuropsychiatric symptoms (delusions, hallucinations, dysphoria, apathy, euphoria, disinhibitions, aggressiveness and agitation, irritability, anxiety, and aberrant motor activity). Caregivers rate the frequency of each symptom on a scale of 1–4, 1 being “occasionally, less than once per week” and 4 being “very frequently, once or more per day.” Scores are summed to provide a total symptom frequency rating. Symptom severity for each of the 10 symptoms is rated on a scale of 1 (mild) to 3 (marked). Frequency and severity scores are multiplied to provide a total score; higher scores correspond to higher disturbances. The baseline Cronbach alpha was .92.
“Neuropsychiatric symptom-related distress” was assessed using a Spanish version of the Neuropsychiatric Inventory-Distress (NPI-D; Cummings et al., 1994; Hinton et al., 2003). Caregivers were asked to rate from 0 to 5 how distressed they are by the above 10 neuropsychiatric symptoms, with 0 being “not at all distressed” to 5 being “very distressed.” Scores are summed to provide a total distress score, with a higher score indicating greater disturbance. A Cronbach alpha of .91 was computed at baseline.
“Depressive symptomology” was measured by a Spanish version of the Center for Epidemiological Studies-Depression Scale (CES-D; Radloff, 1977; Robinson, Gruman, Gaztambide, & Blank, 2002). This 20-item index asks individuals to rate the frequency at which they experienced depressive symptoms within the past week from 0 to 3, with 0 being “rarely or never” to 3 being “most or all of the time.” The baseline Cronbach alpha was .90.
“Caregiver self-efficacy” was measured with a Spanish version of the Revised Scale for Caregiving Self-Efficacy (RSCSE) (Steffen, McKibbin, Zeiss, Gallagher-Thompson, & Bandura, 2002). This 15-item scale assesses three aspects of self-efficacy: obtaining respite, responding to disruptive behaviors, and controlling upsetting thoughts. Caregivers rate their level of certainty regarding their ability using a scale, with 0 being “not at all certain” and 100 being “very certain.” A baseline Cronbach alpha of .86 was obtained for total score.
“Caregiver anxiety” was measured by a Spanish version of the State Anxiety Inventory-State (STAI-S; Spielberger, Gorusch, Lushene, Vagg, & Jacobs, 1983). The 20-item index asks individuals how much they agree with statements such as “I feel nervous” over the past week. Response options range from 1 (not at all) to 4 (very much); thus, a higher total score reflects higher anxiety levels. The baseline Cronbach alpha was .92.
Statistical Analyses
All randomized participants with data at baseline were included and analyzed on an intention-to-treat principle (Hollis & Campbell, 1999). The rationale for this approach is that incomplete data may affect results in two ways: it may bias the estimates of the intervention effect and may be responsible for a substantial loss of statistical power. In this study, there were no missing data at baseline on the demographic or outcome variables and, as reflected in Figure 1, limited participant attrition occurred at post-test (three cases) and follow-up (six cases). To overcome the potential effect of missing data due to participant attrition, missing data on the core outcome measures (i.e., neuropsychiatric symptoms, self-efficacy, depression, and anxiety) post-treatment and follow-up were estimated using the multiple imputation procedure. We also repeated analyses without imputation for missing post-tests to compare against the intention-to-treat results.
As an initial step, bivariate analysis was performed to determine the equivalence of the participants in the two conditions on background and outcome variables at baseline. Repeated measures analysis of covariance (ANCOVA) was used to test the hypotheses; the predictor variables were condition (CBT vs. PED) and time (baseline, post-test, and follow-up) on the dependent variables of caregiver mental health outcomes. The Condition × Time interaction effects were considered to be the most important because we hypothesized significant different changes over time in outcomes for participants in the two arms of the study rather than significant main effects of condition or time. We evaluated potential confounders of care receiver functional limitations and neuropsychiatric symptom severity by entering them as covariates in the analyses of the four caregiver outcomes of neuropsychiatric symptom distress, self-efficacy, depression, and anxiety. Prior to conducting the repeated measures ANCOVA, analysis was undertaken to confirm the variables were normally distributed; there was no evidence of skewness or kurtosis on any of the measures. All tests were two-sided, and an alpha level of .05 was used to determine statistical significance. Finally, to quantify the clinical significance of the CBT intervention, effect size was assessed using Cohen’s d.
Results
Caregiver and Care Recipient Characteristics
As reflected in Table 1, the 67 caregiver participants were predominately Latino daughters (55.2%) and wives (23.9%) whose cultural identities were primarily Dominican (41.8%) or Puerto Rican (46.3%). Their mean age was 54.6 years (SD = 3.1). More than three quarters (79%) had spent their childhood living outside the 50 states and almost two-thirds (64.2%) indicated that they spoke only Spanish at home. Educational obtainment was relatively low; 28.4% had less than a high school education and 47.8% had just a high school or GED degree. Most lived in financially strained households; 67.2% reported annual household incomes of $30,000 or less. In terms of paid employment, 37.3% worked full-time and another 23.9% worked part-time. Approximately 63% lived in the same household as their ADRD relative, and the remaining lived close by. The participants provided, on average, almost 12hr of support daily to their relative.
Table 1.
Baseline Comparison of Caregiver (CG) and Care Receiver (CR) Characteristics: CBT and PED Groups
| Variable | CBT group (n = 33) M (SD) or f (%) | PED group (n = 34) M (SD) or f (%) | x 2 or t |
|---|---|---|---|
| CG gender, female | 32 (97.0) | 32 (94.1) | x 2 = .000 |
| CG relationship | x 2 = .798 | ||
| Spouse | 9 (27.3) | 8 (21.4) | |
| Child | 17 (51.5) | 21 (61.8) | |
| Other | 7 (21.2) | 5 (14.7) | |
| CG married, yes | 13 (39.4) | 14 (41.2) | x 2 = .022 |
| CG age, years | 55.91 (12.95) | 55.50 (13.59) | t = −0.13 |
| CG family’s cultural roots | x 2 = 3.20 | ||
| Puerto Rican | 15 (45.5) | 16 (47.1) | |
| Dominican | 14 (42.3) | 14 (41.1) | |
| Central American | 3 (9.1) | 1 (2.9) | |
| Cuban | 0 (0.0) | 2 (5.9) | |
| Colombian | 1 (3.0) | 1 (2.9) | |
| CG childhood primarily in the states, yes | 7 (24.1) | 7 (25.0) | x 2 = .023 |
| CG primary language spoken at home | x 2 = 1.96 | ||
| Spanish | 19 (57.6) | 24 (70.6) | |
| Bilingual-Spanish and English | 13 (39.4) | 10 (29.4) | |
| English | 1 (3.0) | 0 (0.0) | |
| CG education-highest degree | x 2 = .573 | ||
| Less than high school | 9 (27.3) | 10 (29.4) | |
| High school degree or GED | 15 (45.5) | 17 (50.0) | |
| Associate or technical degree | 7 (21.2) | 6 (17.6) | |
| Bachelor’s degree | 2 (6.1) | 1 (2.9) | |
| CG employment status | x 2 = .1.18 | ||
| Full-time | 13 (39.4) | 12 (35.3) | |
| Part-time | 6 (18.2) | 10 (29.4) | |
| Not in paid labor force | 14 (42.4) | 12 (35.3) | |
| CG annual household income | x 2 = 2.17 | ||
| Less than $10,000 | 4(12.1) | 6 (17.6) | |
| $10,000–$20,000 | 6 (18.2) | 10 (29.4) | |
| $20,001–$30,000 | 10 (30.3) | 9 (26.5) | |
| Greater than $30,000 | 13 (39.4) | 9 (26.5) | |
| CR gender, female | 20 (60.6) | 22 (64.7) | x 2 = .042 |
| CR age, years | 73.5 (8.7) | 76.1 (6.8%) | t = −1.47 |
| CR childhood primarily in the states, yes | 2 (6.1) | 0 (0.0) | x 2 = .460 |
| CR primary language at home, Spanish | 27 (93.1) | 26 (92.9) | x 2 = 2.29 |
| CR OARS total ADL and IADL score (> score, > impairment) | 12.29 (5.28) | 11.52 (6.17) | t = 0.50 |
Note: ADL = activities of daily living; IADL= instrumental activities of daily living; CBT = cognitive behavioral therapy condition; CG = caregiver; CR = care receiver; PED = psychoeducational condition.
The majority (62.7%) of the ADRD care recipients were females; typically in their mid- or late-70s. Almost all had spent their childhoods outside of the United States and currently spoke only Spanish in their homes. Reflected in the average ADL (activities of daily living) and IADL (instrumental activities of daily living) scores, the relatives required considerable assistance in performing the functions of everyday life. No significant differences were found at baseline between the participants in the CBT and PED conditions in terms of the background characteristics (Table 1) or the five outcome measures (Table 2).
Table 2.
Baseline Comparison of Caregivers on Outcome Measures: CBT and PED Groups
| Outcome measures | CBT (n = 33) M (SD) | PED (n = 34) M (SD) | t (65) |
|---|---|---|---|
| Neuropsychiatric Inventory-Severity scale | 21.70 (6.90) | 21.76 (7.98) | 0.04 |
| Neuropsychiatric Inventory-Distress scale | 17.94 (6.84) | 17.91 (7.30) | −0.02 |
| Revised Scale for Caregiver Self-Efficacy | 69.11 (12.76) | 69.19 (9.01) | 0.28 |
| Center for Epidemiological Studies-Depression scale | 14.39 (6.14) | 14.41 (6.31) | 0.12 |
| State-Trait Anxiety Inventory-State scale | 37.09 (10.25) | 37.12 (9.69) | 0.01 |
Note: CBT = cognitive behavioral therapy condition; PED = psychoeducational condition.
CBT Intervention Effectiveness
Results of the repeated measures ANCOVA are shown in Table 3. The data revealed statistically significant Condition × Time interaction effects for the severity of neuropsychiatric symptoms in the ADRD relative (NPI-S; p < .001), neuropsychiatric symptom distress (NPI-D) of the caregiver (p < .001), caregiver sense of self-efficacy (RSCSE; p < .001), and caregiver depression (CES-D; p < .01). No significant interaction effect was found, however, for caregiver anxiety (STAI-S; p > .05). No covariate changed the significance of any of the caregiver mental health outcome variables in the analyses. We also repeated our analyses without the imputation (i.e., including only participants with post-test data on the outcome variables), significant Condition × Time differences in neuropsychiatric symptom severity and distress, self-efficacy, and depression were the same as reported previously.
Table 3.
Comparison of Treatment Conditions at Baseline, Post-test, and Follow-up on Outcomes: Repeated Measures ANCOVA
| Variable | CBT (n = 33)M (SD) | PED (n = 34)M (SD) | F | ||
|---|---|---|---|---|---|
| Condition × Time | Condition | Time | |||
| NPI-S | 21.96*** | 0.28 | 7.14** | ||
| Baseline | 21.70 (6.90) | 21.76 (7.98) | |||
| Post-test | 20.67 (6.94) | 22.03 (9.10) | |||
| Follow-up | 20.52 (6.98) | 22.09 (8.46) | |||
| NPI-D | |||||
| Baseline | 17.94 (6.84) | 17.91 (7.30) | 24.02*** | 0.40 | 6.68** |
| Post-test | 16.64 (7.02) | 17.85 (7.26) | |||
| Follow-up | 16.39 (7.02) | 18.26 (7.37) | |||
| RSCSE | 26.28*** | 0.22 | 16.98*** | ||
| Baseline | 69.11 (12.75) | 69.19 (9.01) | |||
| Post-test | 70.36 (12.44) | 69.29 (8.80) | |||
| Follow-up | 70.27 (12.43) | 69.15 (8.88) | |||
| CES-D | 9.74** | 0.08 | 7.92 ** | ||
| Baseline | 14.39 (6.14) | 14.41 (6.31) | |||
| Post-test | 13.79 (5.85) | 14.38 (6.10) | |||
| Follow-up | 13.82 (5.88) | 14.44 (6.07) | |||
| STAI-State | 1.54 | 0.01 | 1.54 | ||
| Baseline | 37.09 (10.25) | 37.12 (9.69) | |||
| Post-test | 36.85 (9.88) | 37.09 (9.61) | |||
| Follow-up | 36.96 (10.00) | 37.12 (9.68) | |||
Notes: ANCOVA = analysis of covariance; CBT = cognitive behavioral therapy condition; CES-D = Center for Epidemiological Studies-Depression scale; NPI-D = Neuropsychiatric Inventory-Distress scale; NPI-S = Neuropsychiatric Inventory-Severity scale; PED = psychoeducational condition; RSCSE = Revised Scale for Caregiving Self-Efficacy; STAI = State Anxiety Inventory-State.
**p < .01. ***p < .001.
Compared with caregivers in the PED condition, caregivers in the CBT condition reported over time lower levels of neuropsychiatric symptoms severity in their ADRD relative (H1), less distress about the neuropsychiatric symptoms (H2), a greater sense of self-efficacy in providing care (H3) and less depressive symptoms (H4) at the completion of the intervention and three months later. However, the differences in anxiety between the two conditions over time did not prove to be significant (H5). Additional post hoc paired comparisons underscored the different trajectories in caregiver outcomes for the two treatment conditions. The PED participants, on average, remained largely unchanged over the six months; there were neither significant gains nor declines in the measured mental health outcomes (p > .05). In contrast, the CBT participants reported statistically significant improvements in self-efficacy and depression between baseline and postintervention (p < .001), and these gains were maintained at three months. In terms of neuropsychiatric symptom distress, CBT participants not only experienced a significant reduction in distress after completion of the group experience (p < .001), but they also reported statistically lower distress at three-month follow-up compared with immediately post group (p < .01). The magnitude of relative improvement in the CBT (experimental) condition on the outcome variables, however, was modest, ranging from “very small” in terms of self-efficacy and depression (d = .10) to “small” in terms of neuropsychiatric symptom severity (d = .20) and distress (d = .27).
Two exploratory analyses were also undertaken to examine if treatment effects over time varied by either caregiver relationship (adult child/spouse) or ethnic identity (Puerto Rican/Dominican). In fact, no statistically significant three-way interactions were found between caregiver relationship, time, and treatment group or between identity, time, and treatment group. However, due to the small cell sample sizes resulting from crossing factors for the three-way interaction terms, these analyses are viewed as tentative.
Discussion
In this article, we provide preliminary evidence of Circulo de Cuidado’s efficacy, including that the positive effects of the CBT group intervention continue to last beyond the duration of the program, at least for a further three months. We attribute certain characteristics of the CBT intervention as contributing to the positive results in this study, including its targeted focus on neuropsychiatric symptoms, a phenomenon that caregivers find particularly distressful. Another important factor was the cultural tailoring of the intervention. As previously noted, culturally bound beliefs, values, and preferences influence how health, illness, and health care messages are interpreted. Offering the intervention in Spanish removed linguistic barriers and allowed participants to better articulate the nature of their caregiving experience within their own cultural framework and addressed a critical need “to be heard.” Further, the importance of personalismo was incorporated into all stages of the research project. The group didactic experience was highly interactive and informal. Morano and Bravo (2002), for example, suggest that the promotion of informal conversation and the sharing of homemade treats enhanced their PED intervention for Latino ADRD caregivers. In our study, the group experience not only allowed for mutual support but also provided an environment for the leaders’ use of Bandura’s self-efficacy enhancing strategies. Further, although a group experience, the interventions were tailored to focus on the specific needs of the individual caregiver, including the selection of the type of problem behavior on which to focus, the choice of the type of pleasant activities to engage in with their relative, and the identification of the type of stress-reduction techniques to employ. Additionally, the caregivers found the A-B-C problem-solving approach to behavior change relatively easy to understand and implement.
The telephone coaching also allowed another opportunity to be “person-centered” and address the specific concerns of each caregiver. Further, it offered the ability to continue to support the caregiver and reinforce skill building (after the group’s completion) without the added burdens of cost, time, and travel. The transition from the group experience to the telephone coaching/check-ins also fit with our desire to not abruptly terminate the relationship with the caregiver and respect the cultural value of personalismo. The individualized or person-centered nature of the intervention, coupled with the bonding experience between the group members and the facilitator, contributed to limit the dropout rate despite the complexity of the caregivers’ lives.
In reviewing our findings, it is important to consider the study’s limitations. The majority of participants were midlife women who had immigrated to the United States primarily from Puerto Rico or the Dominican Republic; there were few male participants. Further, the study findings are based on a relative small sample size and the study lacked a no-treatment or wait-list control group. It is unknown as to whether differences in the experimental (CBT) and control (PED) participants’ background characteristics would have emerged as more important or how the study outcomes would have been affected if a greater number of participants had been enrolled. Lack of statistical power made the analysis of subgroups difficult. However, the positive findings in a study with limited power are encouraging.
Another limitation was the reliance on self-report measures from the caregivers, particularly in regards to the ADRD relative’s neuropsychiatric symptoms. It is possible that caregivers may have been more positive in describing their relatives’ symptoms because of the effort they had put into learning skills to modify problem behaviors during the intervention program. It is also possible that caregivers’ emotional state may have an uncontrolled impact on the interpretation of their relative’s behavior. Further, the study only assessed impact immediately upon completion of the group and at three-month follow-up. An unanswered question is whether over time the CBT intervention would lead to a series of changes in the way in which the caregiver addresses the ADRD neuropsychiatric symptoms, making it easier to cope with the intense demands of this progressive debilitating long-term disease. Longer-term efficacy is a critical issue because ADRD caregiving typically carries on for several years. Thus, there is as a need for future research that both has a larger sample size and assesses treatment effects longitudinally.
It is also important to note that the broader social environment in which the intervention study was conducted may have influenced the results. The groups occurred in the “physical” and “psychological” neighborhood in which the participants resided and felt comfortable and the “hosting sites” were local organizations, which were well regarded by Latinos and seniors. Finally, the MSW group facilitators were not only bilingual, but very experienced and highly skilled in the delivery of health and social services within Latino communities.
Despite these limitations, this study makes an important contribution to the field. As evidenced in recent systematic reviews of the caregiver intervention research, there is a relative paucity of scientifically rigorous evaluations of a culturally tailored, theoretically driven caregiver intervention with Latino populations. This study offers encouraging evidence that a culturally sensitive, CBT group intervention has the potential to increase Latino family caregivers’ symptom appraisal and problem-solving skills to manage neuropsychiatric symptoms in the ADRD relatives, increase their sense of self-efficacy, and decrease their level of distress.
Funding
This research was supported by grants from the Alzheimer’s Association Investigator Initiated Research Grant Program (IIRG-08-91262) and the Jacob & Valeria Langeloth Foundation (Project Number 1229). E. Velásquez is supported by a National Institutes of Health T32 training grant (AG000158).
Acknowledgments
We thank all the caregivers involved in this study and the Alzheimer’s Association Massachusetts/New Hampshire Chapter for their support of our endeavors.
References
- Acton G. J., Kang J. (2001). Interventions to reduce the burden of caregiving for an adult with dementia: A meta-analysis. Research in Nursing & Health, 24, 349–360. doi:10.1002/nur.1036 [DOI] [PubMed] [Google Scholar]
- Aranda M. P., Villa V. M., Trejo L., Ramírez R., Ranney M. (2003). El Portal Latino Alzheimer’s Project: Model program for Latino caregivers of Alzheimer’s disease-affected people. Social Work, 48, 259–271. doi:10.1093/sw/48.2.259 [DOI] [PubMed] [Google Scholar]
- Aviera A. (2002). Culturally sensitive and creative therapy with Latino clients. California Psychologist, 35, 18. [Google Scholar]
- Ayalon L., & Arean P. A (2004). Knowledge of Alzheimer’s disease in four ethnic groups of older adults. International Journal of Geriatric Psychiatry, 19, 51–57. doi:10.1002/gps.1037 [DOI] [PubMed] [Google Scholar]
- Brodaty H., Green A., Koschera A. (2003). Meta-analysis of psychosocial interventions for caregivers of people with dementia. Journal of the American Geriatrics Society, 51, 657–664. doi:10.1034/j.1600-0579.2003.00210.x [DOI] [PubMed] [Google Scholar]
- Chen J. C., Borson S., Scanlan J. M. (2000). Stage-specific prevalence of behavioral symptoms in Alzheimer’s disease in a multi-ethnic community sample. The American Journal of Geriatric Psychiatry, 8, 123–133. [PubMed] [Google Scholar]
- Clark C. M., DeCarli C., Mungas D., Chui H. I., Higdon R., Nunez J., Van Belle G. (2007). Earlier onset of Alzheimer disease symptoms in Latino individuals compared with Anglo individuals. Archives of Neurology, 62, 774–778. doi:10.1001/archneur.62.5.774 [DOI] [PubMed] [Google Scholar]
- Cooke D. D., McNally L., Mulligan K. T., Harrison M. J., Newman S. P. (2001). Psychosocial interventions for caregivers of people with dementia: A systematic review. Aging & Mental Health, 5, 120–135. doi:10.1080/713650019 [DOI] [PubMed] [Google Scholar]
- Cummings J. L., Mega M., Gray K., Rosenberg-Thompson S., Carusi D. A., Gornbein J. (1994). The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology, 44, 2308–2314. doi:10.1212/WNL.44.12.2308 [DOI] [PubMed] [Google Scholar]
- de Vugt M. E., Stevens F., Aalten P., Lousberg R., Jaspers N., Verhey F. R. (2005). A prospective study of the effects of behavioral symptoms on the institutionalization of patients with dementia. International Psychogeriatrics, 17, 577–589. doi:10.1017/S1041610205002292 [DOI] [PubMed] [Google Scholar]
- Elliott A. F., Burgio L. D., Decoster J. (2010). Enhancing caregiver health: Findings from the resources for enhancing Alzheimer’s caregiver health II intervention. Journal of the American Geriatrics Society, 58, 30–37. doi:10.111/j.1532-5415.2009,02631.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. (2012). Older Americans 2012: Key indicators of well-being Retrieved July 1, 2012, from http://www.agingstats.gov/main_site/default.aspx
- Gallagher-Thompson D., Coon D. W. (2007). Evidence-based psychological treatments for distress in family caregivers of older adults. Psychology and Aging, 22, 37–51. doi:10/1037/0882-7974.22.1.37 [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D., Singer L. S., Depp C., Mausbach B. T., Cardenas V., Coon D. W. (2004). Effective recruitment strategies for Latino and Caucasian dementia family caregivers in intervention research. The American Journal of Geriatric Psychiatry, 12, 484–490. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D. Solano N. Coon D., & Arean P (2003). Recruitment and retention of Latina dementia caregivers in intervention research: Issues to face, lessons to learn. Gerontologist, 43, 45–51. doi:10.1093/geront/43.1.45 [DOI] [PubMed] [Google Scholar]
- Gaugler J. E., Davey A., Pearlin L. I., Zarit S. H. (2000). Modeling caregiver adaptation over time: The longitudinal impact of behavior problems. Psychology and Aging, 15, 437–450. doi:10.1037/0882-7974.15.3.437 [DOI] [PubMed] [Google Scholar]
- Gonyea J. G., O’Connor M. K., Boyle P. A. (2006). Project CARE: A randomized controlled trial of a behavioral intervention group for Alzheimer’s disease caregivers. The Gerontologist, 46, 827–832. doi:10.1093/geront/46.6.827 [DOI] [PubMed] [Google Scholar]
- Gurland B. J., Wilder D. E., Lantigua R., Stern Y., Chen J., Killeffer E. H., Mayeux R. (1999). Rates of dementia in three ethnoracial groups. International Journal of Geriatric Psychiatry, 14, 481–493. doi:10.1002/(SICI)1099–1166(199906)14:6<481:AID-GPS959>3.0.CO;2–5 [PubMed] [Google Scholar]
- Henderson J. N. & Gutierrez-Mayka M (1992). Ethnocultural themes in caregiving to Alzheimer’s patients in Hispanic families. Clinical Gerontologist, 11, 59–74. doi:10.1300/J018v11n03_05 [Google Scholar]
- Hinton L., Chambers D., Velásquez A. (2009). Making sense of behavioral disturbances in persons with dementia: Latino family caregiver attributions of neuropsychiatric inventory domains. Alzheimer Disease and Associated Disorders, 23, 401–405. doi:10.1097/WAD/0b013e3181a6bc21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton L., Haan M., Geller S., Mungas D. (2003). Neuropsychiatric symptoms in Latino elders with dementia or cognitive impairment without dementia and factors that modify their association with caregiver depression. The Gerontologist, 43, 669–677. doi:10.1093/geront/43.5.669 [DOI] [PubMed] [Google Scholar]
- Hollis S., Campbell F. (1999). What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ, 319, 670–674. doi:http://dx.doi.org/10.1136/bmj.319.7211.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight B. G., Sayegh P. (2010). Cultural values and caregiving: The updated sociocultural stress and coping model. The Journal of Gerontology. Series B, Psychological Sciences and Social Sciences, 65B, 5–13. doi:10.1093/geronb/gbp096 [DOI] [PubMed] [Google Scholar]
- Llanque S. M., Enriquez M. (2012). Interventions for Hispanic caregivers of patients with dementia: A review of the literature. American Journal of Alzheimer’s Disease and Other Dementias, 27, 23–32. doi:10.1177/1533317512439774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada A., Knight B. G., Márquez-González M., Montorio I., Etxeberría I., Peñacoba C. (2008). Confirmatory factor analysis of the familism scale in a sample of dementia caregivers. Aging & Mental Health, 12, 504–508. doi:10.1080/13607860802224227 [DOI] [PubMed] [Google Scholar]
- Losada A., Robinson Shurgot G., Knight B. G., Márquez M., Montorio I., Izal M., Ruiz M. A. (2006). Cross-cultural study comparing the association of familism with burden and depressive symptoms in two samples of Hispanic dementia caregivers. Aging & Mental Health, 10, 69–76. doi:10.1080/13607860500307647 [DOI] [PubMed] [Google Scholar]
- Montel S., & Patten E (2012). Latinos in the 2012 election: Massachusetts Retrieved December 13, 2013, from http://www.pewhispanic.org/2012/10/01/latinos-in-the-2012-election- massachusetts/.
- Morano C. L., Bravo M. (2002). A psychoeducational model for Hispanic Alzheimer’s disease caregivers. The Gerontologist, 42, 122–126. doi:10.1093/geront/42.1.122 [DOI] [PubMed] [Google Scholar]
- Napoles A. M., Chadiha L., Eversley R., Moreno-John G. (2010). Reviews: Developing culturally sensitive dementia caregiver interventions: Are we there yet? American Journal of Alzheimer’s Disease and Other Dementias, 25, 389–406. doi:10.1177/1533317510370957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak K., & Riggs J (2004). Hispanics/Latinos and Alzheimer’s disease Retrieved June 3, 2011, from http://www.alz.org/natinal/documents/report_hispanic.pdf
- Pinquart M., & Sorensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 15, 250–267. doi:10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2005). Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist, 45, 90–106. doi:10.1093/geront/45.1.90 [DOI] [PubMed] [Google Scholar]
- Pinquart M., & Sorensen S (2006). Helping caregivers of persons with dementia: Which interventions work and how large are their effects? International Psychogeriatrics, 18, 577–595. doi:10.1017/S1041610206003462 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Robinson J. Gruman C. Gaztambide S., & Blank K (2002). Screening for depression in middle-aged and older Puerto Rican primary care patients. Journal of Gerontology: Medical Science, 57A, M308–M314. doi:10.1093/gerona/57.5.M308 [DOI] [PubMed] [Google Scholar]
- Schulz R. O’Brien A. Czaja S. Ory M. Norris R. Martire L. M. . . . Stevens A (2002). Dementia caregiver intervention research: In search of clinical significance. The Gerontologist, 42, 589–602. doi:10.1093/geront/42.5.589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selwood A., Johnston K., Katona C., Lyketsos C., Livingston G. (2007). Systematic review of the effect of psychological interventions on family caregivers of people with dementia. Journal of Affective Disorders, 101, 75–89. doi:10.1016/j.jad.2006.10.025 [DOI] [PubMed] [Google Scholar]
- Sink K. M., Covinsky K. E., Newcomer R., Yaffe K. (2004). Ethnic differences in the prevalence and pattern of dementia-related behaviors. Journal of the American Geriatrics Society, 52, 1277–1283. doi:10.1111/j.1532-5415.2004.52356.x [DOI] [PubMed] [Google Scholar]
- Spielberger C. D. Gorusch R. L. Lushene R. Vagg P. R., & Jacobs G. A (1983). Manual for the state-trait anxiety inventory (Form Y). Mountain View, CA: Consulting Psychologist Press. [Google Scholar]
- Steffen A. M., McKibbin C., Zeiss A. M., Gallagher-Thompson D., Bandura A. (2002). The revised scale for caregiving self-efficacy: Reliability and validity studies. The Journal of Gerontology. Series B, Psychological Sciences and Social Sciences, 57, P74–P86. doi:10.1093/geronb/57.1.P74 [DOI] [PubMed] [Google Scholar]
- Wisniewski S. R., Belle S. H., Marcus S. M., Burgio L. D., Coon D. W., Ory M. G., Burns R. (2003). The Resources for Enhancing Alzheimer’s Caregiver Health (REACH): Project design and baseline characteristics. Psychology and Aging, 18, 375–384. doi:10.1037/0882-7974.18.3.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin T. Zhou Q., & Bashford C (2002). Burden on family members. Caring for frail elderly: A meta-analysis of interventions. Nursing Research, 52, 199–208. doi:10.1097/00006199-200205000-00009 [DOI] [PubMed] [Google Scholar]


