Abstract
Metabolomic profiling is an increasingly important method for identifying potential biomarkers in cancer cells with a view towards improved diagnosis and treatment. Nuclear magnetic resonance (NMR) provides a potentially noninvasive means to accurately characterize differences in the metabolomic profiles of cells. In this work, we use 1H NMR to measure the metabolomic profiles of water soluble metabolites extracted from isogenic control and oncogenic HRAS-, KRAS-, and NRAS-transduced BEAS2B lung epithelial cells to determine the robustness of NMR metabolomic profiling in detecting differences between the transformed cells and their untransformed counterparts as well as differences among the RAS-transformed cells. Unique metabolomic signatures between control and RAS-transformed cell lines as well as among the three RAS isoform-transformed lines were found by applying principal component analysis to the NMR data. This study provides a proof of principle demonstration that NMR-based metabolomic profiling can robustly distinguish untransformed and RAS-transformed cells as well as cells transformed with different RAS oncogenic isoforms. Thus, our data may potentially provide new diagnostic signatures for RAS-transformed cells.
Keywords: Oncogenic RAS, 1H NMR metabolomics, 1D NOESY, Fieller’s method for unpaired data
Introduction
It has long been appreciated that the metabolism of normal and malignant cells can significantly differ (Warburg, 1956). Measuring the cellular metabolomic profiles can therefore provide a “snapshot” of the degree of oncogenic malignancy in cancer cells (Griffin & Schockor, 2004). One particularly important technique that can measure metabolomic profiles is nuclear magnetic resonance (NMR). NMR is a noninvasive method that can provide highly reproducible and quantitative metabolomic information and has been previously used to detect metabolic fingerprints from a variety of oncogenic pathways (Morvan & Demidem, 2007; Southam et al., 2008).
One of the earliest applications of cellular NMR metabolomics has been to look for biomarkers associated with activation of the RAS oncogene (Aboagye & Bhujwalla, 1999; Ronen et al., 2001). The RAS oncogene, which can exist in either of the HRAS, KRAS, or NRAS isoforms, is found mutated in approximately 30% of all human cancers and produces aggressive, treatment resistant tumors (Fernandez-Medarde & Santos, 2011). Of the three major isoforms, KRAS is found to be the most commonly mutated in human tumors. NRAS is also found activated in certain tumor types such as melanoma, whereas HRAS mutations are rarely found in human cancers (Bos, 1989). The three isoforms, which differ in their membrane-targeting domain, were historically considered to be redundant in their function (Castellano & Santos, 2011). However, a number of studies have shown that the three isoforms are functionally different (Li, Zhu & Guan, 2004; Walsh & Bar-Sagi, 2001; Yan et al., 1998) with tumors sustaining distinct oncogenic versions of RAS showing different progression characteristics (Parikh, Subrahmanyam & Ren, 2007; Whitwam et al., 2007). Accordingly, high-throughput noninvasive means of detecting RAS signatures from tumor cells are likely to aid in effective diagnosis and design of treatment regimens that target RAS-specific pathways (Downward, 2003; Omerovic et al., 2008). However to our knowledge, differences in the metabolomic profiles between normal cells and cells transformed with either of oncogenic HRAS, KRAS, or NRAS have not been previously investigated. Anticipating that there will be robust differences between untransformed and RAS-transformed cells, we employed a cell culture system to validate the NMR methodology described in this study.
Specifically, we analyzed BEAS2B immortalized lung epithelial cells stably transformed with either an empty retroviral vector or with either one of the activated versions of the RAS isoforms, HRAS, KRAS and NRAS, as a proof-of-principle system to determine whether 1H NMR-based metabolomics could be used to identify unique metabolomic signatures between the RAS-transformed and control cells as well as among the different RAS isoform-transformed cell lines. The advantage of this cell culture system is the isogenic background among the four cell lines as well as the ability to generate the requisite numbers of stably transformed cells for consistent NMR characterization. Our NMR characterization of the metabolomic profiles indicated that each RAS isoform possesses a distinct metabolomic signature that has bearing on its observed cell-physiologic transformative effects.
Materials and Methods
DNA constructs and viral transduction
The retroviral pBABE KRASV12, HRASV12 and NRASQ61 DNA constructs were obtained from Addgene. Stable transduction of the pBABE empty vector and the RAS constructs into BEAS2B cells was performed as previously described (Patel et al., 2012). Transduced cells were selected in 2.5 µg/ml puromycin-containing complete culture media for a minimum period of 5–7 days (corresponding to the time taken for untransduced BEAS2B cells to die completely in selection media). Oncoprotein overexpression relative to the control cells was verified via Western blotting as previously described (Patel et al., 2012).
Cell culture
BEAS2B cells were obtained from the American Type Culture Collection. All cells were grown at 37 °C in 21% oxygen and 5% CO2. BEAS2B cells and their derivative lines were maintained in DMEM:F12 complete base media supplemented with 10% fetal bovine serum and 100 units/ml penicillin-streptomycin. All cell culture reagents were obtained from Life Technologies. For each cell line, ten biological replicates were generated by initially seeding ten different 15 cm dishes (Nunclon) with an initial plating of approximately 1 × 106 cells for the control cells, 1.5 × 106 cells for the HRAS- and KRAS-transformed cells, and 2 × 106 for the NRAS-transformed cells (differences in the initial seedings were used to compensate for differences in cellular growth rates so that by the end of the growth period, approximately the same number of cells for each cell line was obtained). In total, all forty plates were seeded at approximately the same time and were allowed to proliferate for a period of four days with the media changed every 48 h. After four days, the cells were trypsinized for approximately two minutes and counted using a Moxi automatic cell counter (VWR) with size parameters adjusted to exclude apoptotic cells. The average final cell counts were (1.107 ± 0.050) × 107 cells per control sample, and (1.558 ± 0.291) × 107, (1.486 ± 0.124) × 107, and (1.613 ± 0.156) × 107 cells per HRAS-, KRAS-, and NRAS-transformed sample, respectively. This corresponded to an average population doubling time of 27.68 h for the control cells and 28.43 h, 29.02 h, and 31.89 h for the HRAS-, KRAS-, and NRAS-transformed cells, respectively. After counting, the cells were pelleted at 1,500 rpm for 5 min at 4 °C with the pellets immediately snap-frozen in liquid nitrogen and stored at –80 °C.
Metabolite extraction
The extraction of hydrophilic metabolites from cell pellets was performed using previously established procedures (Gottschalk et al., 2008). Briefly, cell pellets in a 1.5 ml Eppendorf tubes were resuspended by adding 500 µl of a 2:1 (v∕v) ice-cold solution of methanol (Sigma-Aldrich) and chloroform (Sigma-Aldrich) followed by 3–5 min of vortexing and manual mixing for at least 10 min until a clear solution was obtained. Next, 250 µl of ice-cold chloroform and 250 µl of ice-cold water were each added to the sample, which was then vortexed for 5–7 min to yield a cloudy solution. The sample was sonicated at room temperature for ten minutes followed by centrifugation at 13,000 rpm for 5 min at 4 °C in order to yield three layers. The hydrophilic layer was transferred to a fresh Eppendorf tube followed by bubbling with nitrogen gas (Airgas) to remove any residual methanol. The samples were placed under a high speed vacuum concentrator at room temperature until dried, and the dried hydrophilic layer was stored in a –80 °C freezer until needed.
NMR sample preparation, acquisition, and processing
The dried hydrophilic layer was resuspended in 400 µl of deuterated PBS at pH = 7.6 that was prepared as previously reported (Sambrook, Fritsch & Maniatis, 1989). The pH of each sample was adjusted to 7.6 by the addition of either dilute HCl or NaOH as needed to ensure that each metabolite appeared at the same chemical shift in all samples. In each sample, 0.5 µl of a 0.1 M aqueous solution of DSS (Sigma Aldrich) was added for chemical shift referencing. After vortexing, each sample was transferred into a 5 mm NMR tube.
The 1H NMR spectra were acquired on a 500 MHz Bruker Avance spectrometer (operating at 500.13 MHz for 1H observation) equipped with a 5 mm TCI 500S2 H-C/N-D-05 Z cryoprobe head at 298 K. Each sample was tuned and matched, reshimmed, and the 90°pulse length was recalibrated (90°pulse lengths ranged between 10 and 12 µs). The 1H NMR spectra were acquired using a standard Bruker 1D NOESY pulse program with water presaturation and spoiler gradients applied during the relaxation delay, “noesygppr1d.2” as shown in Fig. 1A. This pulse sequence provides good solvent suppression without rolling baselines (Beckonert et al., 2007; Mckay, 2011). The following experimental parameters were used in all measurements: sweep width of 10.33 kHz, 65 K acquisition points, a 2 s recycle delay during which a 93 Hz water presaturation pulse was applied, τmix = 101.2 ms, θ = 7.5°–9°, and 256 scans were acquired for each sample. Half-sine shaped pulsed field gradients of duration 1 s with maximum gradient strengths of G1 = 24 G/cm and G2 = –23.7 G/cm were used in Fig. 1A along with a 200 µs gradient stabilization delay placed after each gradient pulse. After acquisition, all FIDs were imported into the Chenomx NMR Suite Profiler (version 7.6., Chenomx Inc., Edmonton, Canada). The data were Fourier transformed after multiplication by an exponential window function with a line broadening of 0.5 Hz, and the spectra were manually phase corrected and baseline adjusted using a cubic-spine function. From the initial set of ten biological replicates for each cell line, only 8 of the control, 7 of the HRAS, 9 of the KRAS, and all 10 of the NRAS samples provided measureable NMR signal from resonances other than the solvent peak. Therefore, the results presented in this work represent data obtained from those NS = 8 biological replicates of the control cells, and those NS = 7, NS = 9, and NS = 10 biological replicates of the HRAS-, KRAS-, and NRAS-transformed cells.
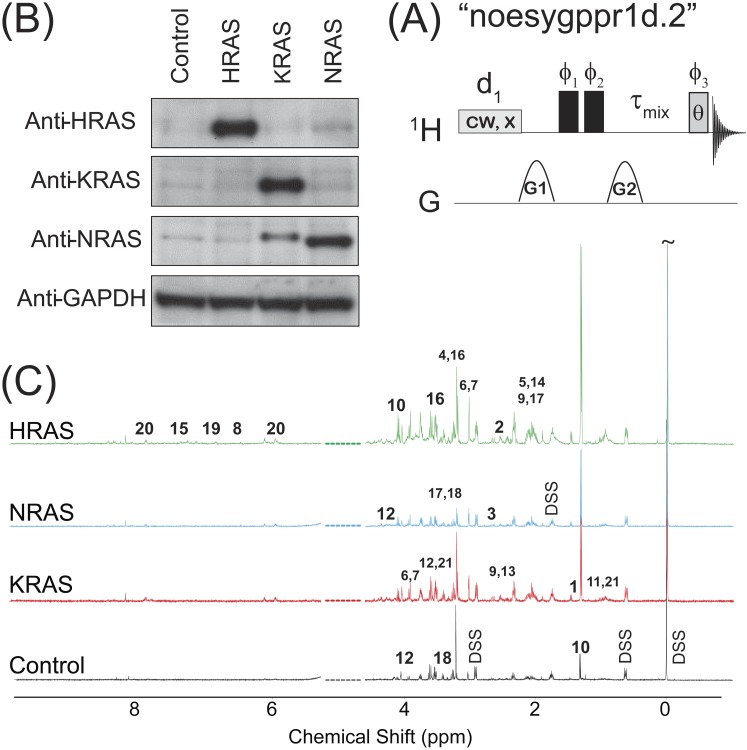
Figure 1. NOESY pulse sequence, Western Blots, and Representative Spectra.
(A) The 1D NOESY with presaturation pulse sequence. (B) Western blots depicting the control and oncogenic HRAS-, KRAS-, and NRAS-transformed cells. (C) Representative spectra obtained from the 1D NOESY sequence applied to samples made from the control and HRAS-, NRAS-, and KRAS-transformed cells. The spectra were normalized so that the DSS resonance at δ = 0 ppm had the same intensity in all spectra for display purposes only. The spectral region for the water resonance is not shown, and certain metabolite resonances are labeled using the codes 1–21 given in Table 1.
The Chenomx NMR Suite Profiler was used to identify metabolites by fitting compound signatures from the provided NMR spectral library. In total, 37 metabolites were identified by NMR. The effective NMR metabolite concentration in each sample, Smetabolite, was calculated using the Chenomx NMR Suite Profiler by determining the heights of the compound signatures that best fit the sample spectra with the effective concentration of the internal DSS standard being set to SDSS = 0.1248 mM, which was the actual DSS concentration in each sample. The table of identified metabolites and their signals was then exported and saved in an Excel worksheet.
Statistical analysis
The “effective” NMR cellular content for metabolite α (moles/cell) taken from the sth biological replicate of a given cell type, , was calculated by multiplying Sα by the NMR sample volume (400.5 µl) and by dividing by the number of cells used to make up each NMR sample. is related to the actual cellular content for metabolite α, , by the relationship
| (1) |
where and fα are dimensionless proportionality factors. The sample- and cell type-independent factor fα is taken to depend only upon the experimental NMR acquisition parameters (such as recycle delays, mixing times, magnetic field strength, etc.) and metabolite α’s spin topology and relaxation properties. This contribution can in principle be found by applying the 1D NOESY sequence in Fig. 1A to prepared standards. The sample- and cell type-dependent factor in Eq. (1) is due to the overall metabolite extraction efficiency, which can vary from sample to sample and depends quite sensitively on cell handling (Duarte et al., 2009) and the particular metabolic quenching and extraction method employed in the study.
The various were used to calculate the “effective” NMR fraction of metabolite α in each sample, , as follows:
| (2) |
As defined in Eq. (2), is dimensionless and independent of the number of cells in a given biological replicate that were used to make the sample. More importantly, is independent of the sample-dependent fluctuation factor, in Eq. (1). The total intensity normalization in Eq. (2) is analogous to that used in spectral binning analysis commonly employed in NMR metabolomic studies. Furthermore, if the various fα are identical for each metabolite, i.e., fα = f for all metabolites, then in Eq. (2) is simply the mole fraction of metabolite α for a given cell type (in general, this is not the case, and fα ≠ fβ).
An ANOVA test, implemented using the MATLAB function “anova1” available in MATLAB’s Statistics toolbox, was first used to test the hypotheses that for each metabolite α, where represents the average value of x for a given cell type. The BY algorithm (Benjamini & Yekutieli, 2001) implemented in MATLAB (Groppe, 2010) with the false discovery rate set to 0.01 was then applied to the p-values from the ANOVA analysis to determine those metabolites where significantly differed (adjusted p-values with p ≤ 0.01) between at least two cell types. For those metabolites identified by the ANOVA test, further post-hoc/multiple comparison testing using the BY algorithm was performed to identify which pair(s) of cell types significantly differed (adjusted p-values with p ≤ 0.01, which are given in Table S1). Finally, a PCA of the various was performed using the “pca” command in the Statistics toolbox in MATLAB, which by default, centers the data before performing the PCA.
Due to the similar average values of the “effective” NMR glutamate content, , observed in both the control and RAS-transformed cells (Fig. S1) and the relatively large glutamate signals observed in all cells lines (only the lactate signals were larger on average), an alternative to the total intensity normalization scheme used in Eq. (2) was also investigated whereby the metabolite signals were normalized by the observed glutamate signal in each sample. In this case, the glutamate normalized signal for metabolite α is given by:
| (3) |
is directly proportional to the ratio of the actualcellular metabolite α to glutamate content, and, like in Eq. (2), it is also independent of the sample-dependent fluctuation factor, . A PCA of the various was also performed, where in this case only 36 metabolites were considered in the analysis since in each sample by definition (Eq. (3)).
One advantage of using glutamate normalization in Eq. (3) compared with using total metabolite normalization in Eq. (2) is that the ratio of ξα,glutamate between different cell types is independent of the fα factors and depends only on the actual cellular metabolite contents:
| (4) |
The ratio in Eq. (4) is equivalent to the relative fold change in the ratio of the actual cellular metabolite α to glutamate content between different cell types. In those instances where a significant difference in between at least two cell types was identified by ANOVA and post-hoc/multiple comparison testing, quantitative confidence intervals for the ratio in Eq. (4) were calculated using Fieller’s method for unpaired data (Motulsky, 1995). In this case, the (100 − α)% confidence range for in Eq. (4), which is denoted by , is given by (Motulsky, 1995):
| (5) |
where N1 and N2 are the number of biological replicates of cell types 1 and 2, respectively, μ1 and σ1 are the average and standard deviations for , respectively, μ2 and σ2 are the average and standard deviations for , respectively, , and is the th quantile of the t-distribution with N1 + N2 − 2 degrees of freedom. If g ≥ 1, the relative fold change in cellular metabolite to glutamate content cannot be calculated using Eq. (5). The MATLAB files and commands used in the statistical analysis of the metabolomics data is given as File S1.
Results and Discussion
Generation of isogenic cell lines for the study
The results of immunoblotting total protein lysates from the four cell types against the various RAS isoforms are shown in Fig. 1B. Western blotting with antibodies against HRAS (first lane), KRAS (second lane) and NRAS (third lane) confirmed that the cells expressed the appropriate RAS isoforms. Uniformity of loading was also confirmed by immunoblotting against GAPDH, a housekeeping gene, as shown in the bottom lane of Fig. 1B. Previous characterizations of these cell lines have also confirmed that the introduction of the RAS oncogene confers soft agar colony growth in these cells, which is indicative of oncogenic transformation (Rai et al., 2011; Patel et al., 2015; Giribaldi et al., 2015).
NMR-based characterization and PCA of metabolomic profiles
Representative spectra taken from a single biological replicate of the control and HRAS-, KRAS-, and NRAS-transformed cells are shown in Fig. 1C, where the spectra were normalized so that the DSS resonance at δ = 0 ppm had the same intensity in all spectra for display purposes only. Certain key metabolites are labeled using the codes, 1–21, given in Table 1.
Table 1. Table of chemical shifts and splitting patterns for metabolites identified by NMR.
List of identified metabolites from the hydrophilic layer, with their corresponding CHEBID, chemical shifts (ppm) and splitting patterns (s, singlet; d, doublet; t, triplet; q, quartet; m, multiplet; dd, doublet of doublets; ddd, doublet of doublet of doublets; bs, broad singlet; bd, broad doublet; bt, broad triplet) used in the Chenomx analysis of the 1H spectra. The labels 1–21 are for those metabolites that exhibited a significant difference (adjusted p-values ≤0.01) between at least two cell types in either their “effective” NMR metabolite fraction, in Eq. (2), or their glutamate normalized signal, in Eq. (3).
| Metabolite [CHEBI ID] | 1H chemical shifts (ppm) and multiplicity |
|---|---|
| Acetate [15366] | 1.90(s) |
| Alanine, 1 [16977] | 1.47(d), 3.77(q) |
| Beta-alanine, 2 [16958] | 2.54(t), 3.16(t) |
| Arginine [16467] | 1.64(m), 1.72(m), 1.88(m), 1.92(m), 3.42(t), 3.75(t) |
| AXP [15422, 16027, 16761] | 4.22(m), 4.29(m), 4.39(m), 4.57(t), 4.8(m), 6.14(d), 8.26(s), 8.52(bs) |
| Aspartate, 3 [17053] | 2.67(dd)a |
| Choline, 4 [15354] | 3.19(s), 3.51(m), 4.06(m) |
| Choline alfoscerate, 5 [16870] | 2.14(s), 3.22(bs), 3.75(m), 4.54(m) |
| Citrate [30769] | 2.51(d)a, 2.68(d)a |
| Creatine, 6 [16919] | 3.02(s), 3.92(s) |
| Creatine phosphate, 7 [17287] | 3.03(s), 3.94(s) |
| Formate [30751] | 8.44(s) |
| Fumarate, 8 [18012] | 6.51(s) |
| Glutamate [16015] | 2.04(dddd), 2.12(dddd), 2.31(ddd)a, 2.36(ddd)a, 3.74(dd) |
| Glutamine, 9[18050] | 2.10(m), 2.14(m), 2.42(m), 2.47(m), 3.76(t) |
| Glutathione [16856] | 2.14(m), 2.17(m), 2.53(m), 2.57(m), 2.93(dd)a, 2.97(dd)a, 3.75(dd)a, 3.77(dd)a, 3.79(dd)a, 4.55(bt) |
| Glycine [15428] | 3.55(s) |
| Isocitrate [151] | 3.02(s), 3.94(s) |
| Isoleucine [17191] | 0.93(t), 0.99(d), 1.25(m), 1.46(m), 1.97(m), 3.66(d) |
| Lactate, 10 [422] | 1.32(d), 4.10(q) |
| Leucine, 11 [15603] | 0.94(d), 0.96(d), 1.67(m), 1.70(m), 1.73(m), 3.70(m) |
| Malate [6650] | 2.35(dd), 2.66(dd), 4.29(bd) |
| Myo-inositol, 12 [17268] | 3.26(t), 3.52(dd), 3.61(dd)a, 4.05(t) |
| N-acetylaspartate, 13 [21547] | 2.00(s), 2.48(dd), 2.68(dd), 4.38(ddd) |
| N-acetylcysteine, 14 [28939] | 2.07(s), 2.90(dd)a, 2.93(dd)a, 4.37(m) |
| N-acetyYc [17533] | 1.91(m), 2.03(s), 2.10(m), 2.30(m), 2.33(m), 4.15(m) |
| [NADZ]d [15846, 16908] | 8.165(s), 8.41(s), 9.33(s) |
| [NADPZ]d [16474, 18009] | 8.14(s), 8.41(s), 9.29(s) |
| Phenylalanine, 15 [17295] | 3.11(dd), 3.37(dd), 3.98(dd), 7.31(d)a, 7.36(m), 7.41(m) |
| Phosphocholine, 16 [18132] | 3.21(bs), 3.58(m), 4.15(m) |
| Proline, 17 [17203] | 1.98(m), 2.03(m), 2.06(m), 2.34(m), 3.33(m), 3.41(m), 4.12(dd) |
| Pyruvate [32816] | 2.36(s) |
| Succinate [15741] | 2.39(s) |
| Taurine, 18 [15891] | 3.25(t), 3.41(dd) |
| Tyrosine, 19 [17895] | 3.04(dd), 3.18(dd), 3.93(dd), 6.88(d)a, 7.18(d)a |
| UDP-Xb, 20[17200, 18066, 18307] | 3.44(t), 3.53(td), 3.76(t), 3.78(dd), 3.86(m), 3.89(m), 4.19(ddd)a, 4.24(ddd)a, 4.27(m), 4.36(m), 4.37(m), 5.59(dd), 5.96(d), 5.98(bd), 7.94(d) |
| Valine, 21 [16414] | 0.98(d), 1.03(d), 2.26(hd), 3.60(d) |
| DSS | 0.00(s), 0.63(m), 1.76(m), 2.91(m) |
Notes.
Multiplet with second-order couplings.
For UDP-X can be UDP-galactose, UDP-glucose, or UDP-glucoranate.
For N-acetylY, the resonances used in the analysis stand for N-acetylglutamate, N-acetylglycine, and/or (and most likely) N-acetylglutamine.
Only the listed resonances were used in the analysis of [NADZ] {[NADH] and/or [NAD+]}, and [NADPZ] {[NADPH] and/or [NADP+]}.
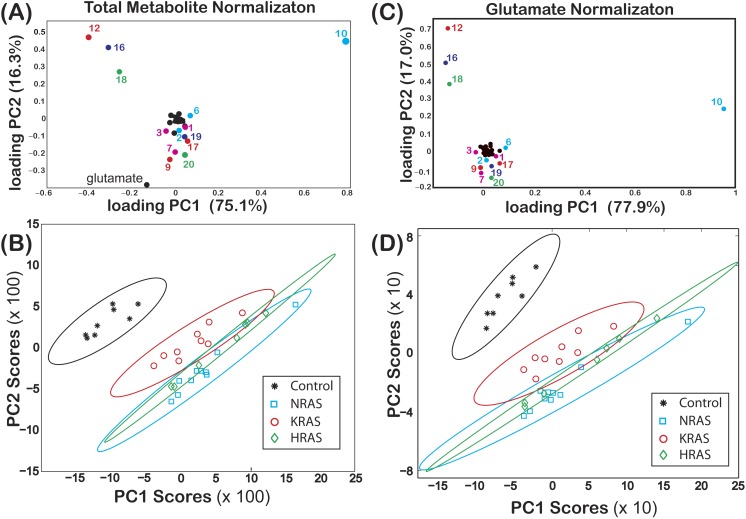
The loadings of PC1 (score of 75.1%) and PC2 (score of 16.3%) from a PCA of are shown in Fig. 2A, where some of the components of both PC1 and PC2 are labeled using the codes given in Table 1. In Fig. 2B, a score plot of PC1 vs. PC2, with the corresponding 99% confidence ellipses (Hoover, 1984) drawn for convenience, shows non-overlapping grouping between the control and the RAS-transformed cells. Similar results were also observed when performing a PCA of as shown in Figs. 2C and 2D.
Figure 2. Loadings and score plots for effective NMR metabolite fractions.
PCA of the effective NMR metabolite fractions, xmetabolite in Eq. (2), and glutamate normalized signals, ξmetabolite,glutamate in Eq. (3), for (asterisks) control and (diamonds) HRAS-, (circles) KRAS-, and (squares) NRAS-transformed cells. Loading plots for xmetabolite[(A) PC1 (75.1%) and PC2 (16.3%)] and ξmetabolite,glutamate [(C) PC1 (77.9%) and PC2 (17.0%)] are shown. The identities of certain metabolites are denoted by the labels given in Table 1. Score plots of PC2 versus PC1 of centered data with the corresponding 99% confidence ellipses (Hoover, 1984) are shown for both the (B) xmetabolite and (D) ξmetabolite,glutamate data. The results in this figure are from NS = 8 biological replicates of the control cells and NS = 7, NS = 9, and NS = 10 biological replicates of the HRAS-, KRAS-, and NRAS-transformed cells, respectively.
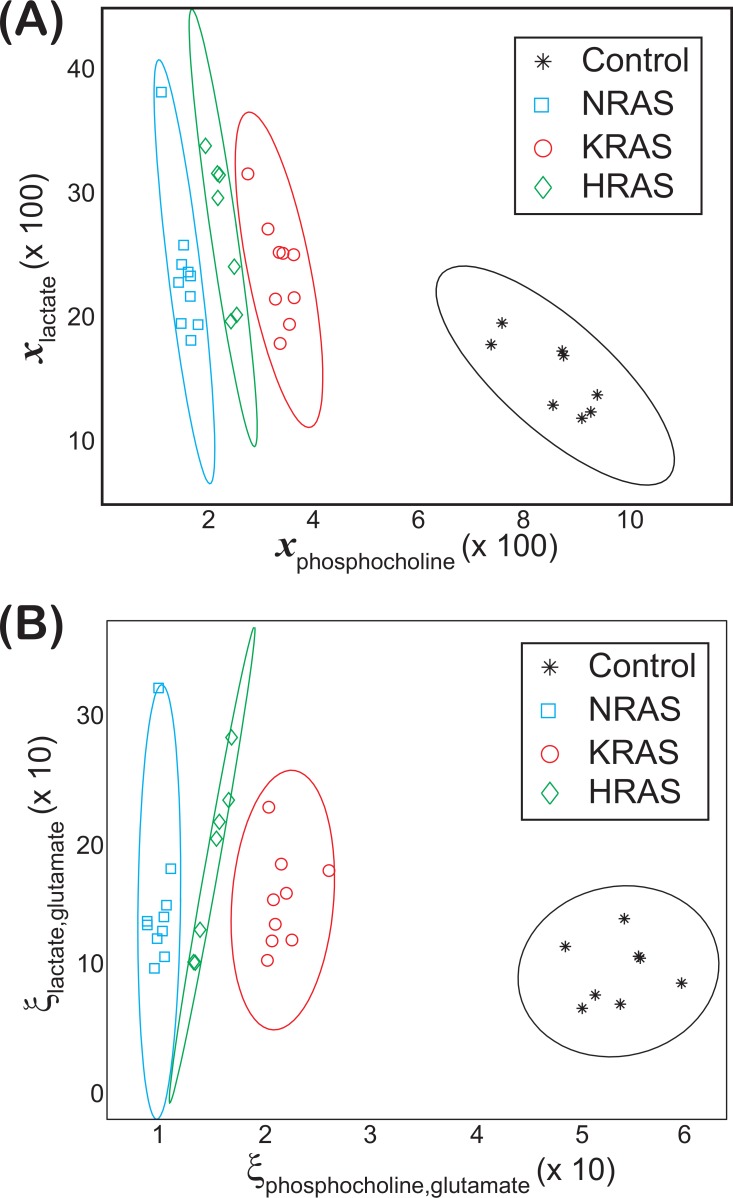
Non-overlapping groupings at the 99% confidence level between all cell lines were found by plotting vs. as shown in Fig. 3A, which were mainly due to differences in the phosphocholine levels between cell types (Fig. 4). Likewise, non-overlapping groupings between all cell lines, this time at a slightly lower confidence level of 97.5%, were also found by plotting vs. as shown in Fig. 3B.
Figure 3. Groupings observed for both the lactate vs. phosphocholine NMR metabolite fractions and glutamate normalized signals.
Scatter plots of both (A) the NMR metabolite fractions for lactate, , versus phosphocholine, and (B) the glutamate normalized lactate, , versus phosphocholine, , found in the (asterisks) control and (diamonds) HRAS-, (circles) KRAS-, and (squares) NRAS-transformed cells. Confidence ellipses (Hoover, 1984) indicate that non-overlapping groupings for all four cell types can be observed at the (A) 99% for the NMR metabolites fractions and at the (B) 97.5% confidence levels for the glutamate normalized signals. In both cases, the results are from NS = 8 biological replicates of the control cells and NS = 7, NS = 9, and NS = 10 biological replicates of the HRAS-, KRAS-, and NRAS-transformed cells, respectively, are shown.
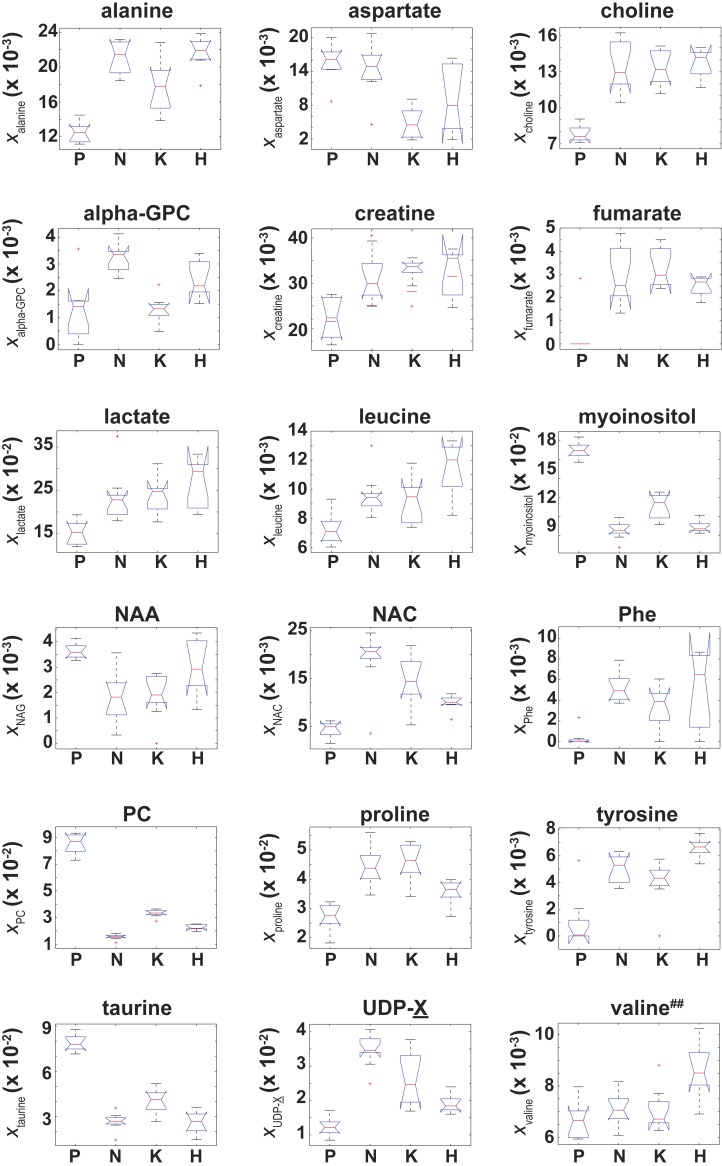
Figure 4. Box plots of the NMR metabolite fractions identified by ANOVA analysis.
Box plots of for those 18 metabolites identified by an ANOVA analysis which indicated was unequal between at least two of the four cell types. While the ANOVA analysis identified , post-hoc/multiple comparison testing could not identify any significant differences in between the cell lines, which is denoted by the superscript ‘##’.
Of the 37 metabolites identified by NMR, an ANOVA analysis indicated that 18 metabolites had a significant (adjusted p-values with p ≤ 0.01) difference in their “effective” NMR metabolite fraction (xα in Eq. (2)) between at least two of the four cell types. Box plots of for these 18 metabolites are given in Fig. 4. Of these 18 metabolites, post-hoc/multiple comparison testing using the BY algorithm found that for 17 metabolites was significantly different between the control cells and at least one of the RAS-transformed cell types whereas the “effective” NMR cellular content for 6 metabolites significantly differed in at least two of the three RAS-transformed cell lines (adjusted p-values ≤ 0.01, which are given in Table S1). It should be noted that while the ANOVA analysis indicated that was unequal between at least two of the four cell types, post-hoc/multiple comparison testing could not identify any significant difference in between cell lines.
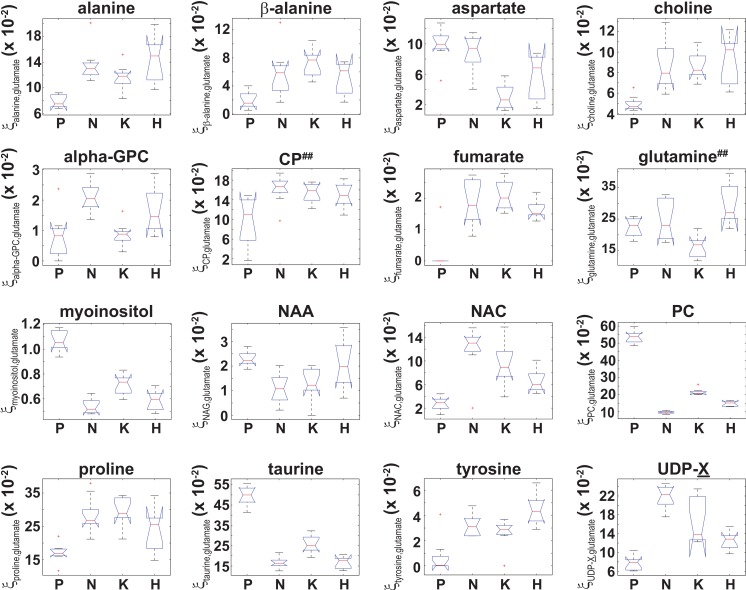
Similarly, an ANOVA analysis of the glutamate normalized metabolite content indicated that 16 metabolites had a significant (adjusted p-values with p ≤ 0.01) difference in (Eq. (3)) between at least two of the four cell types, and box plots of for those 16 metabolites are shown in Fig. 5. Post-hoc/multiple comparison testing indicated that significantly differed between the control cells and at least one of the RAS-transformed cell types for 13 metabolites whereas significantly differed between at least two of the three RAS-transformed cell lines for only 6 metabolites (adjusted p −values ≤ 0.01, which are given in Table S2). It should also be noted that while the ANOVA analysis indicated that and were unequal between at least two of the four cell types, post-hoc/multiple comparison testing could not identify any significant difference in either or between the cell lines. In those instances where a significant difference in between two cell types was identified by ANOVA and post-hoc/multiple comparison testing, the 99% confidence intervals for the relative fold change in the actual cellular metabolite to glutamate content between those cell types, , were calculated using Fieller’s method (Eq. (5)) and are given in Table 2. However, even though significant differences between the RAS-transformed and control cells for and between the HRAS-transformed and control cells for were observed (Fig. 5 and Table S2), the 99% CIs for the relative fold change in the cellular fumarate to glutamate content and the cellular tyrosine to glutamate content could not be calculated due to the small signals and large scatter observed for both tyrosine and fumarate in the control cells (which gave g > 1 in Eq. (5)).
Figure 5. Box plots of the glutamate normalized signals identified by ANOVA analysis.
Box plots of for those 16 metabolites that were identified by an ANOVA analysis that indicated was unequal between at least two of the four cell types. While the ANOVA analysis identified both and , post-hoc/multiple comparison testing could not identify any significant differences in either and between the cell lines, which is denoted by the superscript ‘##’.
Table 2. 99% confidence intervals for relative fold change in the ratio of actual cellular metabolite to glutamate content between cell types.
99% confidence intervals (CIs) for the relative fold change in glutmate normalized signals between cell lines calculated using Fieller’s method (Motulsky, 1995) in Eq. (5). The lower and upper limits of the 99% CIs are denoted by subscripts that bracket the middle of the CI interval (Louis & Zeger, 2009). The abbreviation, n.s., indicates those cases when there was no significant statistical difference in found between cell lines from post-hoc testing using the BY algorithm (Benjamini & Yekutieli, 2001) at a false discovery rate of 0.01. The 99% CIs for the relative fold changes in the cellular fumarate to glutamate content in all RAS-transformed cells relative to control cells and in the cellular tyrosine to glutamate content in HRAS-transformed cells relative to control cells could not be calculated due to the small signals and large scatter of fumarate and tyrosine observed in the control cells (which gave g > 1 in Eq. (5)).
| Metabolite α | |||
|---|---|---|---|
| Alanine | n.s. | 1.191.51.81 | 1.371.752.13 |
| β-alanine | n.s. | 2.076.3410.61 | n.s. |
| Choline | n.s. | 1.401.792.18 | 1.281.782.28 |
| N-acetylcysteine | n.s. | 1.864.116.37 | 2.685.348.01 |
| Proline | n.s. | 1.391.792.20 | 1.311.722.13 |
| UDP-X | 1.241.692.15 | 1.482.253.03 | 2.282.943.60 |
| Aspartate | n.s. | 0.140.330.52 | n.s. |
| Myo-inositol | 0.450.550.65 | 0.580.680.77 | 0.440.510.58 |
| N-acetylaspartate | n.s. | n.s. | 0.220.470.72 |
| Phosphocholine | 0.240.280.31 | 0.360.400.45 | 0.160.180.20 |
| Taurine | 0.260.340.42 | 0.420.520.62 | 0.280.340.40 |
NMR-based identification of metabolite differences among the transformed and control cell lines reflect RAS-driven physiologic alterations
Due to the Warburg effect (Warburg, 1956), it is well known that oncogenic transformed cells undergo aerobic glycolysis as opposed to oxidative phosphorylation (Dang, 2012). To establish the validity of our data against known metabolic changes, we assessed how differences in the NMR signals from lactate and alanine, two major byproducts of glycolytic metabolism (DeBerardinis et al., 2007), varied among the different cell lines. The lactate NMR signal was the largest NMR signal observed in all cell lines (Fig. 4), and lactate was also the largest component to PC1 in the PCA analyses of both xmetabolite and ξmetabolite,glutamate in Fig. 2. In fact, and were found to be statistically larger than (Fig. 4 and Table S1). The cellular alanine to glutamate content was found to be elevated between 50%–75% in KRAS- and NRAS-transformed cells relative to the control cells (Table 2), which is consistent with the reported phenotype of increased aerobic glycolysis in oncogenic RAS-transformed cells (Hahn & Weinberg, 2002), although we should point out that our study provides only a steady-state snapshot of the metabolic profile.
The cellular UDP-X (i.e., UDP-glucose, UDP-galactose, and/or UDP-glucourinate), which are important molecules in glucose metabolism and in the formation of cellular polysaccharides (Berg, Tymoczko & Stryer, 2002), to glutamate content was elevated between a factor of 1.69–2.94 in the RAS-transformed cells lines relative to the control cells (Table 2). Likewise, the cellular N-acetylcysteine, a thiolic antioxidant (Oikawa et al., 1999), to glutamate content was also elevated in all RAS-transformed cells relative to control cells (Fig. 5) with statistically significant differences occurring for the KRAS- and NRAS-transformed cells, where was 4.11 and 5.34 times larger relative to control cells, respectively (Table 2). The elevated levels of N-acetylcysteine in RAS-transformed cells is a significant finding given that RAS-transformed cells are known to exhibit elevated redox protective mechanisms (Young et al., 2004).
The metabolomic signatures of two cellular osmolytes, taurine and myo-inositol, also showed significant differences between the RAS-transformed and control cells. The cellular taurine to glutamate content and the cellular myo-inositol to glutamate content were between 50–66% and 32–45% smaller in all RAS-transformed cells relative to the control cells, respectively (Table 2). As osmolytes regulate the apoptotic cell death pathway (Lang et al., 2005), the functional relevance of the lower values of and observed in RAS-transformed cells may be related to their relative resistance to stress-induced programmed cell death.
An unexpected result from our study was the cellular phosphocholine to glutamate levels. Choline metabolism is an important component in lipid biogenesis (Glunde, Bhujwalla & Ronen, 2011). The cellular phosphocholine to glutamate content in our study was between 60–82% smaller in the RAS-transformed cells relative to the control cells, and statistically significant differences among the RAS-transformed cells were also observed (Fig. 5 and Table S2). Similarly, the cellular choline to glutamate content was around 1.78 times larger in the KRAS- and NRAS-transformed cells relative to the control cells (Table 2). Although there are reports indicating phosphocholine levels correlate with elevated malignancy (Aboagye & Bhujwalla, 1999; Ronen et al., 2001), exceptions in the published literature suggest that this conclusion may be specific to the RAS isoform and cell type being studied (Eliyahu, Kreizman & Degani, 2007).
We have demonstrated in this work that 1H NMR can be used to identify unique metabolomic signatures between BEAS-2B immortalized lung epithelial cells and those transformed with the isoforms of the RAS oncogene as well as among the three RAS isoforms. Collectively, our results suggest that measuring cellular metabolomic profiles can help in distinguishing between normal and RAS-transformed cells along with potentially distinguishing among cancer cells expressing different RAS isoforms. In the future, these results may aid in the development of potential screening technology to determine particular cancer treatment regimens.
Supplemental Information
The adjusted p-values from post-hoc/multiple comparison testing of the effective NMR metabolite fractions ((1) in the main text) using the Benjamini Yekutieli (BY) algorithm (Benjamini & Yekutieli, 2001) with a false discover rate of 0.01. Only those metabolites where an ANOVA analysis indicated that the average value of NMR metabolite fraction was different between at least two of the four cell types are listed. Significant differences (adjusted p-values ≤0.01) are bolded in red.
The adjusted p-values from post-hoc/multiple comparison testing of the glutamate normalized signals, (Eq. (3) in the main text) using the Benjamini Yekutieli (BY) algorithm (Benjamini & Yekutieli, 2001) with a false discover rate of 0.01. Only those metabolites where an ANOVA analysis indicated that the average value of glutatmate normalized signal was different between at least two of the four cell types are listed. Significant differences (adjusted p-values ≤0.01) are bolded in red.
Box plots of NMR metabolite fraction for those 19 metabolites where an ANOVA test did not identify a significant difference in the average NMR metabolite fraction between at least two of the four cell types.
Box plots of the glutamate normalized signals for those 20 metabolites where an ANOVA test did not identify a significant difference in the average glutamate normalized signal between at least two of the four cell types.
Matlab files for Benjamini-Hochberg multiple comparison testing (fdr_bh.m), calculating confidence intervals using Fieller’s theorem (fieller.m), and for calculating confidence ellipses (ellipso.m and plot_ellipse.m). The file MetabolomicsPeerJMatlabCommands.m gives the commands used in statistical analysis of metabolomics data.
NMR sample metabolite concentration for N = 8, N = 10, N = 9, and N = 7 Biological replicates for the control (P) cells and NRAS-, KRAS-, and HRAS-transformed cells along with moxi cell counts for cells used to make those particular samples.
Acknowledgments
The authors wish to thank Dr. Danny Yakoub (UM) for comments about the manuscript.
Funding Statement
JDW received support from the Camille and Henry Dreyfus Foundation and the University of Miami. PR received support from a James and Esther King Florida Biomedical New Investigator Research Grant (09KN-11) and an NIH RO1 grant (RO1 CA175086). Support was also received from the National Science Foundation under CHE—1056846. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Vered Marks and Anisleidys Munoz performed the experiments, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Priyamvada Rai conceived and designed the experiments, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Jamie D. Walls conceived and designed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Data Availability
The following information was supplied regarding data availability:
The raw data has been supplied as Data S1.
References
- Aboagye & Bhujwalla (1999).Aboagye EO, Bhujwalla ZM. Malignant transformation alters membrane choline phospholipid metabolism of human mammary epithelial cells. Cancer Research. 1999;59:80–84. [PubMed] [Google Scholar]
- Beckonert et al. (2007).Beckonert O, Keun HC, Ebbels TMD, Bundy JG, Holmes E, Lindon JC, Nicholson JK. Metabolic profiling, metabolomics and metabonomic procedures for NMR spectroscopy of urine, plasma, serum, and tissue extracts. Nature Protocols. 2007;2:2692–2703. doi: 10.1038/nprot.2007.376. [DOI] [PubMed] [Google Scholar]
- Benjamini & Yekutieli (2001).Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. The Annals of Statistics. 2001;29:1165–1188. [Google Scholar]
- Berg, Tymoczko & Stryer (2002).Berg JM, Tymoczko JL, Stryer L. Biochemistry. 2002. Fifth edition. New York: W.H. Freeman. [Google Scholar]
- Bos (1989).Bos JL. ras oncogenes in human cancer: a review. Cancer Research. 1989;49:4682–4689. [PubMed] [Google Scholar]
- Castellano & Santos (2011).Castellano E, Santos E. Functional specificity of ras isoforms. Genes & Cancer. 2011;3:216–231. doi: 10.1177/1947601911408081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang (2012).Dang CV. Links between metabolism and cancer. Genes & Development. 2012;26:877–890. doi: 10.1101/gad.189365.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBerardinis et al. (2007).DeBerardinis RJ, Mancuso A, Daikhin E, Nissim I, Yudkoff M, Wehrli S, Thompson CB. Beyond aerobic glycolysis: transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:19345–19350. doi: 10.1073/pnas.0709747104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downward (2003).Downward J. Targeting RAS signaling pathways in cancer therapy. Nature Reviews Cancer. 2003;3:11–22. doi: 10.1038/nrc969. [DOI] [PubMed] [Google Scholar]
- Duarte et al. (2009).Duarte IF, Marques J, Ladeirinha AF, Rocha C, Lamego I, Calheiros R, Silva TM, Marques MPM, Melo JB, Carreira IM, Gil AM. Analytical approaches toward successful human cell metabolome studies by NMR spectroscopy. 2009. Analytical Chemistry. 2009;81:5023–5032. doi: 10.1021/ac900545q. [DOI] [PubMed] [Google Scholar]
- Eliyahu, Kreizman & Degani (2007).Eliyahu G, Kreizman T, Degani H. Phosphocholine as a biomarker of breast cancer: molecular and biochemical studies. International Journal of Cancer. 2007;120:1721–1730. doi: 10.1002/ijc.22293. [DOI] [PubMed] [Google Scholar]
- Fernandez-Medarde & Santos (2011).Fernandez-Medarde A, Santos E. Ras in cancer and developmental diseases. Genes & Cancer. 2011;2:344–358. doi: 10.1177/1947601911411084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giribaldi et al. (2015).Giribaldi MG, Munoz A, Halvorsen K, Patel A, Rai P. MTH1 expression is required for effective transformation by oncogenic H-RAS. Oncotarget. 2015;6:11519–11529. doi: 10.18632/oncotarget.3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glunde, Bhujwalla & Ronen (2011).Glunde K, Bhujwalla ZM, Ronen SM. Choline metabolism in malignant transformation. Nature Reviews Cancer. 2011;11:835–848. doi: 10.1038/nrc3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottschalk et al. (2008).Gottschalk M, Ivanova G, Collins DM, Eustace A, O’Connor R, Brougham DF. Metabolomic studies of human lung carcinoma cell lines using in vitro 1H NMR of whole cells and cellular extracts. NMR in Biomedicine. 2008;21:809–819. doi: 10.1002/nbm.1258. [DOI] [PubMed] [Google Scholar]
- Griffin & Schockor (2004).Griffin JL, Schockor JP. Metabolic profiles of cancer cells. Nature Reviews Cancer. 2004;4:551–561. doi: 10.1038/nrc1390. [DOI] [PubMed] [Google Scholar]
- Groppe (2010).Groppe D. Benjamini & Hochberg/Yekutieli procedure for controlling false discovery rate. 2010. Available at http://www.mathworks.com/matlabcentral/fileexchange/27418-benjamini-hochbergyekutieli-procedure-for-controlling-false-discovery-rate/content/ fdr_bh.m. MATLAB Central File Exchange.
- Hahn & Weinberg (2002).Hahn WC, Weinberg RA. Rules for making human tumor cells. New England Journal of Medicine. 2002;347:1593–1603. doi: 10.1056/NEJMra021902. [DOI] [PubMed] [Google Scholar]
- Hoover (1984).Hoover WE. Algorithms for confidence circles and ellipses. Rockville: Charting and Geodesic ServicesNOAA Technical Report. NOS 107 C & GS. 1984 Available at http://www.ngs.noaa.gov/PUBS_LIB/AlgorithmsForConfidenceCirclesAndEllipses_TR_NOS107_CGS3.pdf .
- Lang et al. (2005).Lang F, Foller M, Lang KS, Lang PA, Ritter M, Gulbins E, Vereninov A, Huber SM. Ion channels in cell proliferation and apoptotic cell death. Journal of Membrane Biology. 2005;205:147–157. doi: 10.1007/s00232-005-0780-5. [DOI] [PubMed] [Google Scholar]
- Li, Zhu & Guan (2004).Li W, Zhu T, Guan K-L. Transformation potential of RAS isoforms correlates with activation of phosphatidylinositol 3-kinase but not ERK. The Journal of Biological Chemistry. 2004;279:37398–37406. doi: 10.1074/jbc.M405730200. [DOI] [PubMed] [Google Scholar]
- Louis & Zeger (2009).Louis TA, Zeger SL. Effective communication of standard errors and confidence intervals. Biostatistics. 2009;10:1–2. doi: 10.1093/biostatistics/kxn014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mckay (2011).Mckay RT. How the 1D-NOESY suppresses solvent signal in metabonomics NMR spectroscopy. Concepts in Magnetic Resonance, Series A. 2011;38A:197–220. doi: 10.1002/cmr.a.20223. [DOI] [Google Scholar]
- Morvan & Demidem (2007).Morvan D, Demidem A. Metabolomics by proton nuclear magnetic resonance spectroscopy of the response to chloroethylnitrosourea reveals drug efficacy and tumor adaptive metabolic pathways. Cancer Research. 2007;67:2150–2159. doi: 10.1158/0008-5472.CAN-06-2346. [DOI] [PubMed] [Google Scholar]
- Motulsky (1995).Motulsky H. Intuitive biostatistics. First edition. New York: Oxford University Press; 1995. [Google Scholar]
- Oikawa et al. (1999).Oikawa S, Yamada K, Yamashita N, Tada-Oikawa S, Kawanishi S. N-acetylcysteine, a cancer chemopreventive agent, causes oxidative damage to cellular and isolated DNA. Carcinogenesis. 1999;20:1485–1490. doi: 10.1093/carcin/20.8.1485. [DOI] [PubMed] [Google Scholar]
- Omerovic et al. (2008).Omerovic J, Hammond DE, Clague MJ, Prior IA. Ras isoform abundance and signaling in human cancer cell lines. Oncogene. 2008;27:2754–2762. doi: 10.1038/sj.onc.1210925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikh, Subrahmanyam & Ren (2007).Parikh C, Subrahmanyam R, Ren R. Oncogenic NRAS, KRAS, and HRAS exhibit different leukemogenic potentials in mice. Cancer Research. 2007;67:7139–7146. doi: 10.1158/0008-5472.CAN-07-0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel et al. (2015).Patel A, Burton DGA, Halvorsen K, Balkan W, Reiner T, Perez-Stable C, Cohen A, Munoz A, Giribaldi MG, Singh S, Robbins DJ, Nguyen DM, Rai P. MutT Homolog 1 (MTH1) maintains multiple KRAS-driven pro-malignant pathways. Oncogene. 2015;34:2586–2596. doi: 10.1038/onc.2014.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel et al. (2012).Patel A, Muñoz A, Halvorsen K, Rai P. Creation and validation of a ligation-independent cloning (LIC) retroviral vector for stable gene transduction in mammalian cells. BMC Biotechnology. 2012;12:3. doi: 10.1186/1472-6750-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai et al. (2011).Rai P, Young JJ, Burton DGA, Giribaldi MG, Onder TT, Weinberg RA. Enhanced elimination of oxidized guanine nucleotides inhibits oncogenic RAS-induced DNA damage and premature senescence. Oncogene. 2011;30:1489–1496. doi: 10.1038/onc.2010.520. [DOI] [PubMed] [Google Scholar]
- Ronen et al. (2001).Ronen SM, Jackson LE, Belouche M, Leach MO. Magnetic resonance detect changes in phosphocholine associated with RAS activation and inhibition in NIH-3T3 cells. British Journal of Cancer. 2001;84:691–696. doi: 10.1054/bjoc.2000.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambrook, Fritsch & Maniatis (1989).Sambrook J, Fritsch JEF, Maniatis T. Molecular cloning: a laboratory manual. Second edition. Cold Spring Harbor, New York: Cold Spring Harbor Laboratory Press; 1989. Appendix B.12. [Google Scholar]
- Southam et al. (2008).Southam AD, Easton JM, Stentiford GD, Ludwig C, Arvanitis TN, Viant MR. Metabolic changes in flatfish hepatic tumours revealed by NMR-based metabolomics and metabolic correlation networks. Journal of Proteome Research. 2008;7:5277–5285. doi: 10.1021/pr800353t. [DOI] [PubMed] [Google Scholar]
- Walsh & Bar-Sagi (2001).Walsh AB, Bar-Sagi D. Differential activation of the Rac pathway by Ha-Ras and K-Ras. The Journal of Biological Chemistry. 2001;276:15609–15615. doi: 10.1074/jbc.M010573200. [DOI] [PubMed] [Google Scholar]
- Warburg (1956).Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- Whitwam et al. (2007).Whitwam T, VanBrocklin MW, Russo ME, Haak PT, Bilgili D, Resau JH, Koo HM, Holmen SL. Differential oncogenic potential of activated RAS isoforms in melanocytes. Oncogene. 2007;26:4563–4570. doi: 10.1038/sj.onc.1210239. [DOI] [PubMed] [Google Scholar]
- Yan et al. (1998).Yan J, Roy S, Apolloni A, Lane A, Hancock JF. Ras isoforms vary in their ability to activate Raf-1 and phosphoinositide 3-kinase. The Journal of Biological Chemistry. 1998;273:24052–24056. doi: 10.1074/jbc.273.37.24052. [DOI] [PubMed] [Google Scholar]
- Young et al. (2004).Young TW, Mei FC, Yang G, Thompson-Lanza JA, Liu JS, Cheng XD. Activation of antioxidant pathways in Ras-mediated oncogenic transformation of human surface ovarian epithelial cells revealed by functional proteomics and mass spectrometry. Cancer Research. 2004;64:4577–4584. doi: 10.1158/0008-5472.CAN-04-0222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The adjusted p-values from post-hoc/multiple comparison testing of the effective NMR metabolite fractions ((1) in the main text) using the Benjamini Yekutieli (BY) algorithm (Benjamini & Yekutieli, 2001) with a false discover rate of 0.01. Only those metabolites where an ANOVA analysis indicated that the average value of NMR metabolite fraction was different between at least two of the four cell types are listed. Significant differences (adjusted p-values ≤0.01) are bolded in red.
The adjusted p-values from post-hoc/multiple comparison testing of the glutamate normalized signals, (Eq. (3) in the main text) using the Benjamini Yekutieli (BY) algorithm (Benjamini & Yekutieli, 2001) with a false discover rate of 0.01. Only those metabolites where an ANOVA analysis indicated that the average value of glutatmate normalized signal was different between at least two of the four cell types are listed. Significant differences (adjusted p-values ≤0.01) are bolded in red.
Box plots of NMR metabolite fraction for those 19 metabolites where an ANOVA test did not identify a significant difference in the average NMR metabolite fraction between at least two of the four cell types.
Box plots of the glutamate normalized signals for those 20 metabolites where an ANOVA test did not identify a significant difference in the average glutamate normalized signal between at least two of the four cell types.
Matlab files for Benjamini-Hochberg multiple comparison testing (fdr_bh.m), calculating confidence intervals using Fieller’s theorem (fieller.m), and for calculating confidence ellipses (ellipso.m and plot_ellipse.m). The file MetabolomicsPeerJMatlabCommands.m gives the commands used in statistical analysis of metabolomics data.
NMR sample metabolite concentration for N = 8, N = 10, N = 9, and N = 7 Biological replicates for the control (P) cells and NRAS-, KRAS-, and HRAS-transformed cells along with moxi cell counts for cells used to make those particular samples.
Data Availability Statement
The following information was supplied regarding data availability:
The raw data has been supplied as Data S1.