Abstract
Background
To evaluate the anatomical and visual outcomes by par plana vitrectomy with or without internal limiting membrane (ILM) peeling in highly myopic eyes with macular hole retinal detachment (MHRD).
Methods
MEDLINE (Ovid, PubMed) and EMBASE were used for data collection up to September 30, 2015. The parameters of anatomical success, macular hole closure and improved best corrected visual acuity (BCVA) at or beyond 6 months after operation were assessed as the primary outcome measurement. The meta-analysis was performed with the fixed-effects model.
Results
Seven comparative analyses involving a total of 373 patients were included in the present meta-analysis. Statistically the pooled data showed significant relative risk (RR) in terms of primary reattachment between ILM peeling and non-peeling groups (RR, 1.19; 95 % CI, 1.04 to 1.36; P = 0.012). An effect favoring ILM peeling with regard to macular hole closure was also detected (RR, 1.71; 95 % CI, 1.20 to 2.43; P = 0.003). However, no statistically significant difference was found in the improved BCVA (logarithm of the minimum angle of resolution) at 6 months or more (95 % CI, −0.31 to 0.44; P = 0.738).
Conclusions
There is no proved benefit of postoperative visual improvement. However, the available evidences from this study suggested a superiority of ILM peeling over no peeling for myopic patients with MHRD.
Background
Retinal detachment resulting from macular hole (MHRD) is one of the most vision-threatening complications to high myopias, with the incidence reported to be 67.7 % in myopic eyes between −8D and −3.25D [1]. Although the pathogenesis is not completely understood, the elongation of the axial length, the posterior staphyloma formation, the tangential traction of vitrous cortex and epiretinal membrane may be related factors [2, 3]. The rigidity of the internal limiting membrane (ILM) has also been considered to be an important factor [4]. For this reason, par plana vitrectomy (PPV) combined with ILM peeling was believed to be one of the beneficial procedures for those patients. The rationale includes relieving macular traction completely and increasing the flexibility of retina to conform better to the posterior staphyloma [5].
There were growing studies supporting the benefit of ILM peeling for myopic MHRD [6, 7]. However, the conflict results also found from other authors there were no significant association between ILM peeling and primary anatomical reattachment or macular hole closure rate [8–10]. In addition, ILM removal has been shown technically more challenging in patients with myopic maculopathy, even assisted with perfluorocarbon liquids for flattened retina and with the aid of vital dyes [11].
Evidences for comparing the benefits and complications of ILM peeling versus no peeling are largely lacking. Thus, in this study we compared anatomical and functional success rates of PPV with or without ILM peeling for MHRD in high myopias. Despite of the limitation of differences in the original study design, selection criteria and allocation protocol, in this meta-analysis we intend to design and make clear the optimal techniques by pooling available published studies.
Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12].
Strategy for data collection
The databases of MEDLINE (Ovid, PubMed) and EMBASE were used for data collection up to September 30, 2015. The articles collected from these databases were related to MHRD in highly myopic eyes. The following search strategy was used: (“macular hole” OR MH) AND (“retinal detachment” OR RD) AND (myopi* OR myopia [mesh]) AND (vitrectomy) AND (“inner limiting membrane” OR “internal limiting membrane” OR ILM) AND (removal OR peeling). All studies were limited to the English language.
Inclusion and exclusion criteria
All cases recruited for this study were considered to follow the included and excluded criteria. The inclusive criteria included a) studies that compared outcomes of par plana vitrectomy with ILM peeling vs. non-peeling in highly myopic eyes with MHRD; b) detailed description of surgical procedures; and c) the follow up period no less than 6 months. The exclusive criteria included a) previous history of PPV; b) presence of peripheral retinal break or proliferative vitreo-retinopathy before the primary surgery; c) use of silicone oil tamponade in the primary surgery; d) use of scleral buckling, including macular buckling in the primary study; and e) studies with inadequate records of postoperative reattachment rates, macular hole closure rates or postoperative best corrected visual acuity (BCVA) at ≥6 months.
Data extraction
Two reviewers independently extracted the data that met the inclusion criteria. After the first extraction, data were rechecked and any disagreement regarding eligibility during the extraction was resolved by discussion. The information extracted from each study included the first author, publication year, country, trial type, age, gender, number of subjects, follow-up time, preoperative and postoperative BCVA. Intraoperative and postoperative complications were also recorded. The outcomes of interest that were extracted included the anatomical success, macular hole closure, and improved BCVA at ≥6 months.
Outcome measurements
The measurements include a) Anatomical success was defined as the complete disappearance of the subretinal fluid and neurosensory retinal reattachment to the underlying retinal pigment epithelium; b) Macular hole closure was defined by optical coherence tomography as the complete disappearance of the hole and absence of neurosensory defect over the fovea; and c) The logarithm of the minimum angle of resolution (logMAR) improved BCVA at ≥6 months.
Assessment of study quality
The quality of the included studies was assessed by two independent authors (XXG and JG) using a previously reported system by Downs and Blacks [13]. The system comprises 27 items distributed among 5 subscales regarding reporting (10 items), external validity (3 items), bias (7 items), confounding (6 items), and power (1 item). Discrepancies in the qualitative assessment were resolved by discussion until consensus was reached. The total score of each trial was expressed as a percentage of the maximum achievable score. Studies with a quality score of ≥50 % were considered to have adequate quality.
Statistical analysis
The meta-analysis was conducted using the Stata software package (version 12.0; Stata Corp). The relative risk (RR) was measured with 95 % confidence interval (CI) for dichotomous variables, whereas the weighted mean difference (WMD) was calculated with the 95 % CI for continuous variables. A P value less than 0.05 was considered statistically significant. Statistical heterogeneity among trials was analyzed using the Pearson’s chi-square test and I2 tests. If there was significant heterogeneity between studies, a random-effects model was employed; otherwise, a fixed effects model was used to obtain summary RR or WMD.
Results
Data assessment
The search identified a total of 174 publications after duplicates removed. 129 studies were excluded after abstract evaluation. Of 45 publications that initially were considered potentially relevant, 38 finally were excluded. Seven comparative studies were included in the present meta-analysis involving a total of 373 patients who underwent PPV in highly myopic eyes with MHRD (Fig. 1). All studies fulfilled the quality criteria, with Downs and Blacks scores ≥50 % (Table 1).
Fig. 1.
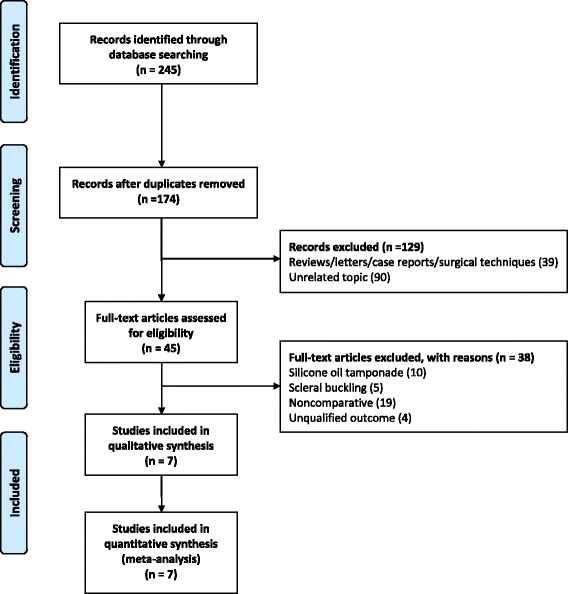
A flow diagram of strategies for the data collection
Table 1.
Characteristics and quality scoring components of included studies
| Trial, year | Study design | Location | Number of eyes | Quality score component | Overall effect | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | Overall | Percentage | ||||
| Ikuno (2003) [14] | Retrospective, nonrandomized, comparative study | Japan | 14/2 | 8 | 2 | 3 | 3 | 0 | 16 | 50.00 % |
| Lam (2006) [15] | Retrospective, interventional, comparative case series | China | 44/13 | 9 | 2 | 2 | 3 | 2 | 18 | 56.25 % |
| Li KK (2010) [17] | Prospective interventional, comparative, case control study | China | 10/9 | 10 | 2 | 3 | 2 | 0 | 17 | 53.13 % |
| Li X (2009) [9] | Prospective, randomized controlled, multicenter study | China | 65/46 | 10 | 2 | 4 | 2 | 3 | 21 | 65.63 % |
| Nakanishi (2008) [10] | Retrospective, multicenter, interventional case series | Japan | 40/9 | 9 | 2 | 2 | 2 | 2 | 17 | 53.13 % |
| Uemoto (2004) [18] | Retrospective, nonrandomized, comparative study | Japan | 13/12 | 10 | 2 | 3 | 3 | 0 | 18 | 56.25 % |
| Wei (2013) [16] | Retrospective, comparative, case control study | China | 47/49 | 10 | 2 | 3 | 3 | 2 | 20 | 62.50 % |
Surgical techniques
The surgical procedures were generally consistent with little difference in each study. Briefly, after the vitreous cortex was completely removed after visualization with or without triamcinolone acetonide, ILM was peeled in a circular motion with the aid of ICG or not. The peeling area was 2 ~ 3 DD in the study by Ikuno [14], 3 ~ 4 DD in the studies by Lam [15], Wei [16], and within the vascular arcade by Li KK [17], Uemoto [18]. After ILM peeling, argon endolaser photocoagulation was performed at the macular hole margin in the study by Lam [15]. Gas tamponade was finally performed using either sulfur hexafluoride (SF6) or perfluoropropane (C3F8) or room air. Patients were instructed to keep prone position for at least 7 days after surgery (Table 2).
Table 2.
Characteristics of various studies on surgical procedures for myopic macular hole with retinal detachment
| Trial, year | Vital dyes | Area of ILM peeling | Type of tamponade gas | Face-down duration | Other treatment | Intraoperative and postoperative complications |
|---|---|---|---|---|---|---|
| Ikuno (2003) [14] | ICG | 2–3 DD | 14 % or 16 % C3F8 | 2 weeks | No | Posterior capsule opacification Cataract Recurrent RD |
| Lam (2006) [15] | ICG | 3–4 DD | 12 % C3F8/air mixture | 7–10 days | Endolaser at the MH margin | Suprachoroidal hemorrhage Iatrogenic retinal breaks Cataract Glaucoma |
| Li KK (2010) [17] | TA and 0.15 % trypan blue | Between superotemporal and inferotemporal vascular arcades | 14 % C3F8 | 2 weeks | No | Transient increased IOP |
| Li X (2009) [9] | TA or ICG | NA | 14 % C3F8/air mixture | 3 weeks | No | Iatrogenic retinal tear Elevated IOP |
| Nakanishi (2008) [10] | TA and ICG | NA | SF6 or C3F8 | At least 1 week | No | Iatrogenic retinal breaks Temporary elevations of IOP Vitreous hemorrhage |
| Uemoto (2004) [18] | 0.25 % ICG | Within the vascular arcade | 24 % SF6 or 14 % C3F8 or room air | 1 week | No | Iatrogenic retinal breaks Epiretinal membrane Nuclear cataract |
| Wei (2013) [16] | TA ± 0.5 % ICG ± | 3–4 DD | 14 % C3F8/air mixture | 2 weeks | No | Retinal breaks Epiretinal membrane MH reopen Cataract Glaucoma |
DD disc diameter, ICG indocyanine green, ILM internal limiting membrane, IOP intraocular pressure, MH macular hole, NA not available, TA triamcinolone acetonide
Anatomical success
Primary anatomical reattachment was achieved in 173 of 219 patients in the ILM peeling group compared with 96 of 138 patients in the group without ILM peeling. Meta-analysis shows statistically significant RR in terms of primary reattachment between ILM peeling and non-peeling groups (RR, 1.19; 95 % CI, 1.04 to 1.36; P = 0.012), with no heterogeneity identified (I2 = 38. 6 %; P = 0.148) (Fig. 2 and Table 3). Begg’s test (P = 0.188) indicated no serious publication bias in these included studies.
Fig. 2.
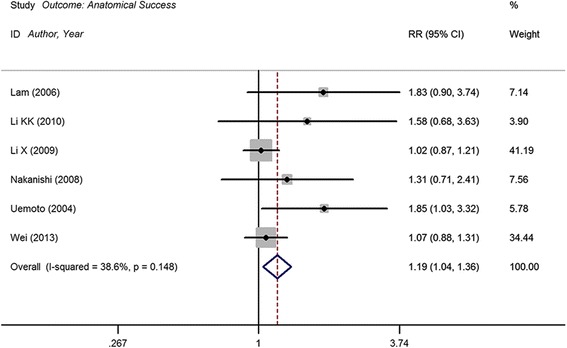
Forest plot of primary anatomical reattachment of internal limiting membrane (ILM) peeling group vs. no peeling group. CI = confidence interval; RR = relative risk
Table 3.
Main results of meta analysis
| Outcome | No. of studies | No. of eyes | Test for heterogeneity | Overall effect | |||||
|---|---|---|---|---|---|---|---|---|---|
| ILM peeling | ILM preserved | x 2 | I2 | P | WMD/RR (95 % CI) | Z | P | ||
| Primary anatomic reattachment [9, 10, 15–18] | 6 | 219 | 138 | 8.15 | 38.6 % | 0.148 | 1.19(1.04, 1.36) | 2.52 | 0.012 |
| Macular hole closure[14–18] | 5 | 127 | 83 | 2.47 | 0.0 % | 0.650 | 1.71 (1.20, 2.43) | 2.95 | 0.003 |
| Improved BCVA at ≥6 months[14, 18] | 2 | 27 | 14 | 0.17 | 0.0 % | 0.677 | 0.06 (−0.31, 0.44) | 0.33 | 0.738 |
BCVA best corrected visual acuity, ILM internal limiting membrane, RR relative risk, WMD weighted mean difference
Macular hole closure
Macular hole closure was achieved in 74 of 127 patients in the ILM peeling group compared with 27 of 83 patients in the ILM-preserved group. Meta-analysis shows statistically significant RR in terms of macular hole closure rates between ILM peeling and non-peeling groups (RR, 1.71; 95 % CI, 1.20 to 2.43; P = 0.003), with no heterogeneity identified (I2 = 0. 0 %; P = 0.650) (Fig. 3 and Table 3). The assessment of macular hole closure using Begg’s test (P = 0.327) demonstrated no publication bias in included trials.
Fig. 3.
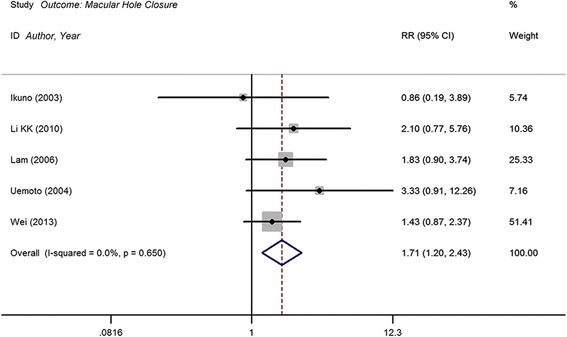
Forest plot of macular hole closure of internal limiting membrane (ILM) peeling group vs. no peeling group. CI = confidence interval; RR = relative risk
Improved logMAR BCVA after surgery at ≥6 months
Only 2 studies reported results on improved BCVA for ILM-removed and ILM-preserved groups. The WMD in the improved logMAR BCVA between ILM peeling and non-peeling groups was 0.06 (95 % CI, −0.31 to 0.44). Meta-analysis showed no statistically significant difference (P = 0.738), with no heterogeneity identified (I2 = 0. 0 %; P = 0.677) (Fig. 4 and Table 3). Due to the limited number of trials, publication bias was not assessed.
Fig. 4.
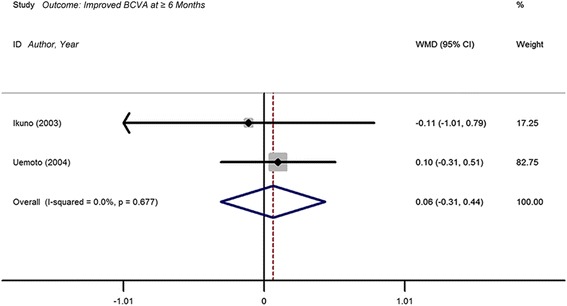
Forest plot of the weighted mean difference (WMD) of improved BCVA at ≥6 months comparing internal limiting membrane (ILM) peeling group with no peeling group. CI = confidence interval
Discussion
To the best of our knowledge, this is the first meta-analysis that assesses efficacy and safety of ILM peeling vs. no peeling for myopic MHRD. We reviewed seven comparative studies involving a total of 373 patients who underwent PPV with or without ILM peeling. The pooled outcomes from this meta-analysis, using a fixed effects model, indicated that ILM-peeled group got higher rates of anatomical reattachment success and macular hole closure. However, no significant difference for improvement of BCVA was detected between the two groups with initial surgery. The result from this study provided important findings that may be helpful in the selection of surgical maneuvers.
Six of the trials reported the success rate of the primary anatomical reattachment. Our meta-analysis showed that ILM-peeled group had higher reattachment rate. ILM peeling may help to completely remove macular traction caused by overlying retinal tissues on the ILM and subsequently improve the elasticity of the adjacent retina, aiding in the conformity to the posterior staphyloma [4]. In contrast, in an analysis of the factors predicting anatomical success among patients with myopic MHRD, Lim et al. found that ILM peeling was not a significant predictor of success. They suggested that the role of ILM peeling for tangential traction relief was diminished by the elongation of axial length [8].
Studies included in our meta-analysis showed that macular hole closure rate in ILM peeling group ranged from 42.9 to 70.5 % (results not shown). Statistical difference was identified between ILM peeling group and non-peeling group. In a recently published meta-analysis evaluating the effects of ILM peeling for full thickness macular hole, Spiteri Cornish et al. found evidences favoring ILM peeling in terms of primary and final macular hole closure [19]. ILM may act as a scaffold for cell migration and consequent fibroglial proliferation. Thus, ILM peeling was considered to relieve the contraction of epiretinal cellular constituents adjacent to the macular hole. In addition, the tangential traction of residual vitreous or epiretinal membranes (ERMs) may be completely released after ILM removal. These factors can ensure better closure of macular hole and recovery of macular shape [20].
Our study indicated that no obvious visual improvement was achieved in these myopic eyes with MHRD, in despite of anatomical and surgical success. Similarly, in a study to evaluate the efficacy of PPV for each stage of myopic macular traction, no difference of postoperative BCVA was found between patients with and without ILM peeling [21]. Besides anatomical success and macular hole closure, visual acuity can be affected by many other factors that are hard to assess. The duration of the detachment, the time of surgery and the previous changes, including atrophy of the RPE and choriocapillaris at the posterior pole, may be influential factors for the final visual outcomes in myopic MHRD. Additionally, it could take longer time to observe the effect of ILM peeling on the visual acuity, but the studies with a longer follow-up are largely missing.
ILM peeling has been considered to cause mechanical retinal damage, including physiological alterations in Müller cells [22], irregularities of nerve fiber layer [23], small paracentral scotomas [24], loss of Müller cell endfeet within the peeling area and weakening of macular glial structure [25, 26]. ILM removal even resulted in the development of postoperative full-thickness macular holes in some cases of myopic foveoschisis [27]. More recently, a retinal dimple sign was identified in highly myopic eyes after ILM peeling by an image of en face OCT [28]. Additionally, due to the osmolarity effects or phototoxic properties, studies showed that ICG may have potential retinal toxicity with injury to RPE cells and ganglion cells during ILM peeling [29, 30].
There are growing evidences favored the effects of ILM peeling for MHRD. It was reported that fibroblast-like cells, collagen fibrils and acellular collagen fibers have been detected by transmission electron microscopy on the vitreous surface of ILM in myopic MHRD [31]. ILM peeling was believed to remove the collagen fiber and cellular constituents that may be responsible for gliosis stimulation and foveal traction in myopic maculopathy, indicating the efficacy of ILM removal for MHRD. In addition, ILM peeling was considered to be one of the important prognostic factors associated with a higher anatomical success rate for retinal detachment resulting from myopic macular hole [15]. However, due to the retinal thinning and friability in severely myopic patients, ILM peeling is technically more difficult, even assisted with effective dyes and performed by experienced vitreoretinal surgeons [11]. In the pathologic myopia, axial length elongation and posterior staphyloma formation often result in retinal thinning at macula area, peeling of ILM is likely to pose an increased risk for surgical trauma. Future studies are needed to make clear the safety of ILM peeling for retinal detachment arising from macular hole in highly myopic eyes.
It is worthy to note the relatively limited powers of our meta-analysis when considering the results. First, this study was limited by the low quality of the retrospective studies included and the lack of randomized controlled trials-based evidences. Most studies were carried out with small sample size, nonrandomized nature or no double blinding. The only randomized study did not show any outcome of macular hole closure, whereas other studies were more likely to be prone to publication bias. Although the study quality was assessed, the system may not assign sufficient importance to the comparability of the data from the peeling and non-peeling groups. This may compromise the efficacy of this instrument in controlling potential biases. In addition, results on improved BCVA were only obtained from 2 studies, which may restrict its reliability. Moreover, the follow-up duration was different in each included study, which may also result in difference and corresponding biases. Thus, the interpretation of the results may be greatly affected. Second, this study was limited to use published index, therefore the papers, particularly those published in languages other than English may have failed to be included. Third, the parameters of interest may have a large degree of heterogeneity. For example, due to the potential complications of long-term use, silicone oil was generally reserved for redetachment cases in most studies. In this analysis, we excluded the studies with silicone oil tamponade in primary surgery. Last, adjunctive procedures were dependent and postoperative management was variable among each surgeon, which may affect the final outcomes.
However, in this study we had the detailed protocol before initiating the analysis, the explicit methods for trials selection, and data extraction, which helped to minimize the likelihood of bias.
Conclusions
This study suggests that ILM peeling is a more effective and safer procedure in highly myopic eyes with MHRD, but it does not seem to offer significant visual advantages compared with non-ILM peeling. More standard-designed studies with prospective randomized control, incorporating larger sample sizes, and long-term follow-up could help to provide more reliable evidences.
Abbreviations
BCVA, best corrected visual acuity; CI, confidence interval; ILM, internal limiting membrane; logMAR, the logarithm of the minimum angle of resolution; MHRD, macular hole retinal detachment; PPV, par plana vitrectomy; PRISM, preferred reporting items for systematic reviews and meta-analyses; RR, relative risk; WMD, weighted mean difference
Acknowledgements
We do not have someone to acknowledge to.
Funding
No funding was obtained for this study.
Availability of data and materials
Not applicable.
Authors’ contributions
XXG, JG and XM collected the data. XXG and JG assessed the quality of the included studies. XXG and XM performed the statistical analysis. XXG, XYP and JW drafted the manuscript. XYP and JW conceived and designed the study. YI reviewed and revised the manuscript. All authors have read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Ethics and consent to participate
Not applicable.
Contributor Information
Jun Wang, Email: drwangjun@yeah.net.
Xiaoyan Peng, Email: drpengxy@yeah.net.
References
- 1.Morita H, Ideta H, Ito K, Yonemoto J, Sasaki K, Tanaka S. Causative factors of retinal detachment in macular holes. Retina. 1991;11:281–4. doi: 10.1097/00006982-199111030-00002. [DOI] [PubMed] [Google Scholar]
- 2.Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004;122:1455–60. doi: 10.1001/archopht.122.10.1455. [DOI] [PubMed] [Google Scholar]
- 3.Ishida S, Yamazaki K, Shinoda K, Kawashima S, Oguchi Y. Macular hole retinal detachment in highly myopic eyes: ultrastructure of surgically removed epiretinal membrane and clinicopathologic correlation. Retina. 2000;20:176–83. doi: 10.1097/00006982-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn F. Internal limiting membrane removal for macular detachment in highly myopic eyes. Am J Ophthalmol. 2003;135:547–9. doi: 10.1016/S0002-9394(02)02057-3. [DOI] [PubMed] [Google Scholar]
- 5.Sayanagi K, Ikuno Y, Tano Y. Tractional internal limiting membrane detachment in highly myopic eyes. Am J Ophthalmol. 2006;142:850–2. doi: 10.1016/j.ajo.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 6.Kadonosono K, Yazama F, Itoh N, Uchio E, Nakamura S, Akura J, Sawada H, Ohno S. Treatment of retinal detachment resulting from myopic macular hole with internal limiting membrane removal. Am J Ophthalmol. 2001;131:203–7. doi: 10.1016/S0002-9394(00)00728-5. [DOI] [PubMed] [Google Scholar]
- 7.Oie Y, Emi K, Takaoka G, Ikeda T. Effect of indocyanine green staining in peeling of internal limiting membrane for retinal detachment resulting from macular hole in myopic eyes. Ophthalmology. 2007;114:303–6. doi: 10.1016/j.ophtha.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 8.Lim LS, Tsai A, Wong D, Wong E, Yeo I, Loh BK, Ang CL, Ong SG, Lee SY. Prognostic factor analysis of vitrectomy for retinal detachment associated with myopic macular holes. Ophthalmology. 2014;121:305–10. doi: 10.1016/j.ophtha.2013.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Wang W, Tang S, Zhao J. Gas injection versus vitrectomy with gas for treating retinal detachment owing to macular hole in high myopes. Ophthalmology. 2009;116:1182–7. doi: 10.1016/j.ophtha.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Nakanishi H, Kuriyama S, Saito I, Okada M, Kita M, Kurimoto Y, Kimura H, Takagi H, Yoshimura N. Prognostic factor analysis in pars plana vitrectomy for retinal detachment attributable to macular hole in high myopia: a multicenter study. Am J Ophthalmol. 2008;146:198–204. doi: 10.1016/j.ajo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Spaide RF, Fisher Y. Removal of adherent cortical vitreous plaques without removing the internal limiting membrane in the repair of macular detachments in highly myopic eyes. Retina. 2005;25:290–5. doi: 10.1097/00006982-200504000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and nonrandomized studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ikuno Y, Sayanagi K, Oshima T, Gomi F, Kusaka S, Kamei M, Ohji M, Fujikado T, Tano Y. Optical coherence tomographic findings of macular holes and retinal detachment after vitrectomy in highly myopic eyes. Am J Ophthalmol. 2003;136:477–81. doi: 10.1016/S0002-9394(03)00269-1. [DOI] [PubMed] [Google Scholar]
- 15.Lam RF, Lai WW, Cheung BT, Yuen CY, Wong TH, Shanmugam MP, Lam DS. Pars plana vitrectomy and perfluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthalmol. 2006;142:938–44. doi: 10.1016/j.ajo.2006.07.056. [DOI] [PubMed] [Google Scholar]
- 16.Wei Y, Wang N, Zu Z, Bi C, Wang H, Chen F, Yang X. Efficacy of vitrectomy with triamcinolone assistance versus internal limiting membrane peeling for highly myopic macular hole retinal detachment. Retina. 2013;33:1151–7. doi: 10.1097/IAE.0b013e31827b6422. [DOI] [PubMed] [Google Scholar]
- 17.Li KK, Tang EW, Li PS, Wong D. Double peel using triamcinolone acetonide and trypan blue in the management of myopic macular hole with retinal detachment: a case–control study. Clin Experiment Ophthalmol. 2010;38:664–8. doi: 10.1111/j.1442-9071.2010.02333.x. [DOI] [PubMed] [Google Scholar]
- 18.Uemoto R, Yamamoto S, Tsukahara I, Takeuchi S. Efficacy of internal limiting membrane removal for retinal detachments resulting from a myopic macular hole. Retina. 2004;24:560–6. doi: 10.1097/00006982-200408000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Spiteri Cornish K, Lois N, Scott NW, Burr J, Cook J, Boachie C, Tadayoni R, la Cour M, Christensen U, Kwok AK. Vitrectomy with internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole. Ophthalmology. 2014;121:649–55. doi: 10.1016/j.ophtha.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 20.Uemoto R, Yamamoto S, Aoki T, Tsukahara I, Yamamoto T, Takeuchi S. Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol. 2002;86:1240–2. doi: 10.1136/bjo.86.11.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taniuchi S, Hirakata A, Itoh Y, Hirota K, Inoue M. Vitrectomy with or without internal limiting membrane peeling for each stage of myopic traction maculopathy. Retina. 2013;33:2018–25. doi: 10.1097/IAE.0b013e3182a4892b. [DOI] [PubMed] [Google Scholar]
- 22.Terasaki H, Miyake Y, Nomura R, Piao CH, Hori K, Niwa T, Kondo M. Focal macular ERGs in eyes after removal of macular ILM during macular hole surgery. Invest Ophthalmol Vis Sci. 2001;42:229–34. [PubMed] [Google Scholar]
- 23.Ito Y, Terasaki H, Takahashi A, Yamakoshi T, Kondo M, Nakamura M. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology. 2005;112:1415–20. doi: 10.1016/j.ophtha.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 24.Haritoglou C, Gass CA, Schaumberger M, Ehrt O, Gandorfer A, Kampik A. Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol. 2001;132:363–8. doi: 10.1016/S0002-9394(01)01093-5. [DOI] [PubMed] [Google Scholar]
- 25.Wolf S, Schnurbusch U, Wiedemann P, Grosche J, Reichenbach A, Wolburg H. Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology. 2004;111:238–43. doi: 10.1016/j.ophtha.2003.05.022. [DOI] [PubMed] [Google Scholar]
- 26.Newman E, Reichenbach A. The Müller cell: a functional element of the retina. Trends Neurosci. 1996;19:307–12. doi: 10.1016/0166-2236(96)10040-0. [DOI] [PubMed] [Google Scholar]
- 27.Gao X, Ikuno Y, Fujimoto S, Nishida K. Risk factors for development of full-thickness macular holes after pars plana vitrectomy for myopic foveoschisis. Am J Ophthalmol. 2013;155:1021–7. doi: 10.1016/j.ajo.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 28.Sakimoto S, Ikuno Y, Fujimoto S, Sakaguchi H, Nishida K. Characteristics of the retinal surface after internal limiting membrane peeling in highly myopic eyes. Am J Ophthalmol. 2014;158:762–8. doi: 10.1016/j.ajo.2014.06.024. [DOI] [PubMed] [Google Scholar]
- 29.Haritoglou C, Gandorfer A, Gass CA, Schaumberger M, Ulbig MW, Kampik A. The effect of indocyanine-green on functional outcome of macular pucker surgery. Am J Ophthalmol. 2003;135:328–37. doi: 10.1016/S0002-9394(02)01969-4. [DOI] [PubMed] [Google Scholar]
- 30.Jackson TL, Hillenkamp J, Knight BC, Zhang JJ, Thomas D, Stanford MR, Marshall J. Safety testing of indocyanine green and trypan blue using retinal pigment epithelium and glial cell cultures. Invest Ophthalmol Vis Sci. 2004;45:2778–85. doi: 10.1167/iovs.04-0320. [DOI] [PubMed] [Google Scholar]
- 31.Sakaguchi H, Ikuno Y, Choi JS, Ohji M, Tano T. Multiple components of epiretinal tissues detected by triamcinolone and indocyanine green in macular hole and retinal detachment as a result of high myopia. Am J Ophthalmol. 2004;138:1079–81. doi: 10.1016/j.ajo.2004.06.078. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


