Abstract
Context:
There are various regions in India that have high levels of fluoride in drinking water sources. Many people residing in such places suffer from dental fluorosis (DF).
Aims:
To evaluate the prevalence of DF in children residing in Salem and also to find any correlation between DF and other related factors.
Materials and Methods:
One school from each block of Salem (total 21 blocks) was selected for the study. A single examiner had evaluated untreated caries, lesions, and DF (for permanent anterior teeth and molars) using the Dean's fluorosis index, in all children. Water fluoride level determination at each school was done using the Tamil Nadu Water Fluoridation and Drainage Board field kit. Other factors that may have contributed to DF were assessed using a questionnaire, which was provided to each student. The data obtained were statistically analyzed using the SPSS software version 11.5.
Statistical Analysis:
Chi-square test was used for statistical analysis.
Results:
DF was present in 56.9% of the children examined. It was mostly seen in 9 years old (72%) and male (59%) children. A positive correlation was found between the occurrence of DF and the duration of residence in a place with high water fluoride content, consumption of borewell water (64%), the parts per million of fluoride in drinking water, consumption of black tea (59%). However, no correlation was found between DF, dental caries, consumption of milk, or consumption of foods cooked in aluminum vessels.
Conclusion:
There was a correlation between DF and factors such as male gender, bore well water consumption, black tea consumption and the duration of residence in a place with high water fluoride content.
Keywords: Black tea, bore well water, dental fluorosis, Salem, school water, Tamil Nadu
Introduction
Endemic fluorosis is a public health problem in India where approximately 62 million people including six million children suffer from fluorosis because of the consumption of water containing high fluoride concentrations.[1] Fluorosis was first described by Shortt et al. as a public health problem in different parts of India.[2] Due to its strong electronegativity, fluoride is attracted to positively charged calcium in teeth and bones, resulting in dental and skeletal fluorosis.[3] In Tamil Nadu (India), 10 out of 29 districts have shown significantly high fluoride content in their water resources. A recent study reported that high concentrations of fluoride in groundwater was found in the districts of Dharmapuri and Salem, closely followed by Coimbatore, Madurai, Tiruchirappalli, Dindigul, and Chidambaram. Tirunelveli, Pudukkottai, North Arcot, and Ramanad are however districts with low fluoride content in groundwater.[4] Salem has an area of 5245 km2 with a total population of 3,482,056 (2011 census). Salem has been further divided into 21 blocks with regard to educational management. A pilot study was conducted at a local school in Salem where dental fluorosis (DF) was found to be present in 30.8% of the children, out of which 31.1% were male and 30.3% were female.[5] The aim of this study was to evaluate the prevalence of DF in children residing in Salem and also to find any correlation between DF and other related parameters.
Materials And Methods
Ethical committee clearance was obtained from the institution for the oral examination of 5000 schoolchildren in Salem. The permission to conduct an oral examination of schoolchildren was obtained from the Chief Educational Officer of Salem. The 21 blocks of Salem that were included in this study were Veerapandi, Sengavalli, Pethanaickenpalayam, Panamarathupatti, Thalaivasal, Athur, Ayothiapattinam, Salem Oorakam, Vazhapadi, Yercaud, Salem Nagaram, Konganapuram, Kolathur, Nangavalli, Kadayapatti, Tharamangalam, Magudanchavadi, Mecheri, Sankagiri, Edappadi, and Omalur. One school from each block was selected for the study using the lottery method. Parental consent was obtained through the headmasters of each of the schools. Assent was also obtained before the oral examination. Children from different socioeconomic strata were selected for the study after they fulfilled the following inclusion criteria:
Children studying in government schools
Children in the age group of 9–14 years
Children who were born and brought up in Salem district
Children who were present on the day of the study
Children who agreed for the study.
Children with developmental defects of teeth or the absence of permanent teeth were excluded from the study.
Each child was asked to fill up the following details:
Age and sex
Place and duration of residence
Source of water for consumption: Tap/borewell/well/bottle/combination
Quantity of black tea and milk consumption per day
Whether aluminum vessels are used for cooking at home.
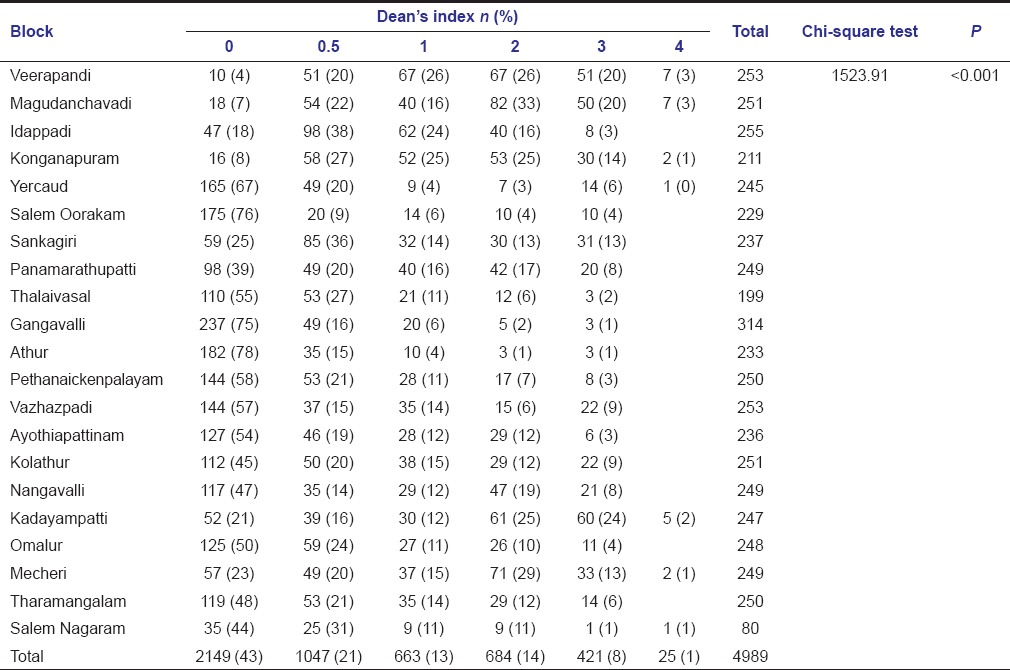
Prior to starting the study, an examiner received training to evaluate and score different grades of DF with the help of archival records of dental photographs from the Department of Oral Pathology. This examiner had evaluated untreated caries, lesions, and DF (for permanent anterior teeth and molars) using the Dean's fluorosis index in all the children, thereby eliminating any chance of inter-examiner variability. Examination of teeth was carried out under daylight, using sterile instruments from sealed pouches. Water fluoride level determination at each school was done using the Tamil Nadu Water Fluoridation and Drainage Board field kit [Figure 1]. Five milliliters of drinking water from each school was collected in the bottle provided and mixed with five drops of the reagent. Upon doing so, color change was observed in the water. The color of the water was then compared with a color coding chart to determine the fluoride level [Figure 2]. With this kit, fluoride levels ranging from 0 to 5 ppm could be assessed.
Figure 1.

Tamil Nadu Water Fluoridation and Drainage Board field kit
Figure 2.
Color change in water being matched with shade guide
Results
A total of 4989 children were examined, out of which 43.3% were boys and 56.7% were girls. DF was present in 56.9% of the children and was absent in 43.1%. A Dean's score of 0.5, 1, and 2 was found in 48% of the children, whereas 8.9% of the children presented with Dean's scores of 3 and 4 [Table 1]. The data obtained were statistically analyzed using the SPSS software (Version 11.5, IBM Corporation, Armonk, New York, USA). Chi-square test was used for statistical analysis.
Table 1.
Dean's index in children from different blocks of Salem district
DF was mostly found to affect 9 years old children (72%) compared with children of higher ages [Table 2]. The difference was found to be highly statistically significant (P < 0.001). Out of the children affected [Table 3], DF was found to be significantly more in males (59%) as compared with females (55%). The correlation between the occurrence of DF and the duration of residence in a place with high water fluoride content [Table 4] was found to be highly statistically significant (P = 0.004). DF was found mostly in children who consumed borewell water (64%) compared with those who consumed bottled water (59%), pipe water (57%), well water (47%), and water from all sources (57%). The differences were found to be highly statistically significant [P < 0.0001, Table 5]. A significant correlation was found between the occurrence of DF and the fluoride level [Table 6] in the drinking water of a particular school (P = 0.043). DF was found to occur more in children who consumed black tea (59%) than those who did not consume black tea [Table 7]. The difference was found to be highly statistically significant (P = 0.002). However, no correlation was found between DF, dental caries, consumption of milk, or the consumption of foods cooked in aluminum vessels [Tables 8–10].
Table 2.
Correlation between age and the occurrence of dental fluorosis
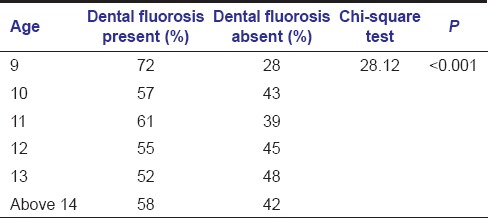
Table 3.
Correlation between sex and the occurrence of dental fluorosis
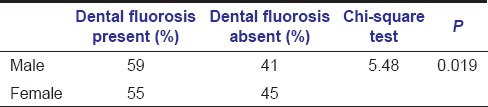
Table 4.
Correlation between duration of residence and the occurrence of dental caries
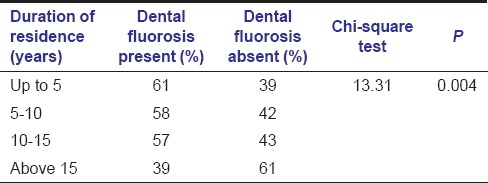
Table 5.
Correlation between the source of drinking water at home and the occurrence of dental fluorosis
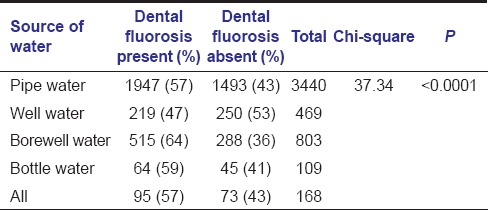
Table 6.
Correlation between water fluoride level and the occurrence of dental fluorosis
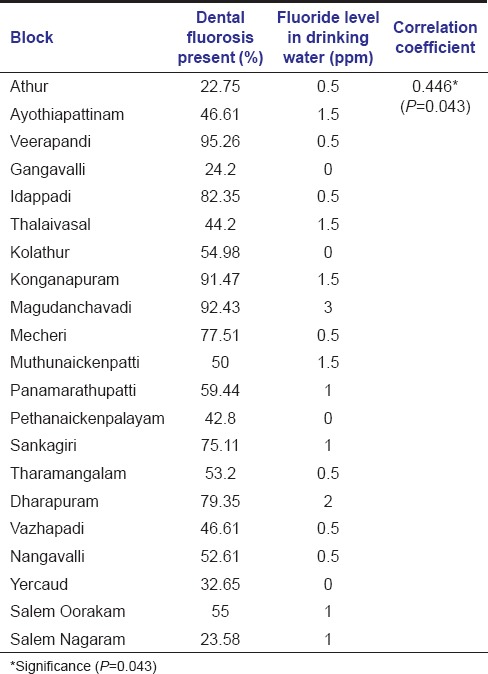
Table 7.
Correlation between black tea consumption and the occurrence of dental caries
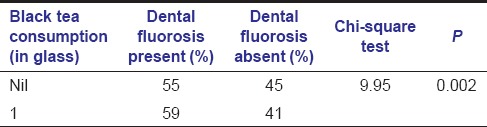
Table 8.
Correlation between the occurrences of dental caries and dental fluorosis
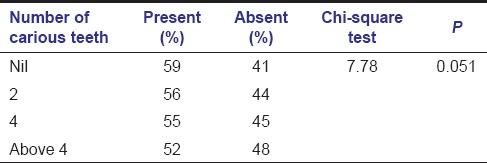
Table 10.
Correlation between the use of aluminum vessels for cooking and the occurrence of dental fluorosis
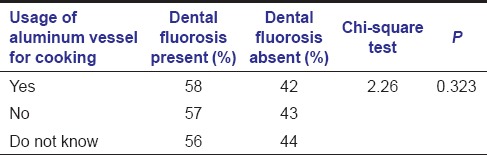
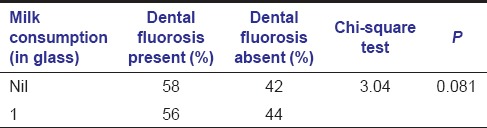
Table 9.
Correlation between the consumption of milk and the occurrence of dental fluorosis
Discussion
The Dean's index was used for examining DF because of its simplicity and uniformity of use in many previous studies. It is also the recommended index for use when the water fluoride level is below 5 ppm.[6]
DF was found mostly in 9 years old children (72%) compared with children of higher ages. However, this result differs from one that obtained by Choubisa et al., who found no correlation between age and the occurrence of DF.[7] This may be due to differences in the frequency of fluoride intake at different ages that would have corresponded with the development of certain teeth. It may also be due to variations in the water fluoride level where the children resided during the development of their permanent teeth.
Out of the children affected, DF was found to be significantly more in males (59%) as compared with females (55%). A similar finding was made by Kotecha et al.[8] However, DF was found to be more prevalent in female children in two previous studies.[9,10] The higher prevalence of DF in male children in the present study may be associated with greater physical activity that would have increased the consumption of drinking water.
DF was found mostly in children who consumed borewell water (64%). This is similar to the result obtained from another study in Tamil Nadu.[11] However, a prevalence of 57% was found in those who consumed only tap water. This showed that the tap water supplied by the municipality also contributed to the occurrence of DF. Children who consumed bottled water at home also presented with DF (59%). This may indicate that commercial bottled water of certain brands might also contain elevated fluoride content. In a study in Riyadh (Saudi Arabia), the mean fluoride concentration from 15 brands of commercial bottled water was found to be 0.79 mg/L while in two brands, discrepancies were found between the measured and labeled fluoride concentrations.[12] In Australia, 90% of the commercial bottled water brands were found to contain fluoride in concentrations <1.2 mg/L.[13]
Children who had continuously resided in an area with elevated water fluoride content for the first 5 years of their life showed more DF lesions when compared with those who resided in a similar area between 5 and 10 years of their life. This is in accordance with the fact that most permanent teeth including permanent incisors and first molars undergo crown formation within the first 5 years of life.
In this study, no correlation was found between the occurrences of dental caries and DF. It has been reported that the risk of dental caries was less when the fluoride content in drinking water was more.[8] However, when the fluoride content was moderate or high, the occurrence of caries was found to increase.[14] In a similar study, DMFT was found to increase when the severity of DF was up to grade 3 and found to decrease when the severity of DF was between grade 3 and grade 5.[15] In another study, a decline in DFS and DMFS was associated with water fluoride levels between 0 and 0.7 ppm, with little additional decline between 0.7 and 1.2 ppm of fluoride.[16] DF was found to occur more in children who consumed black tea (59%). A substantial amount of fluoride is released during tea infusion, and nearly, all (about 94.9%) of the fluoride released is absorbed by consumers.[17] Water brewed with tea leaves, increased its fluoride content by 3–4 times.[18] The rate and extent of fluoride absorption from the gastrointestinal tract are reduced by the ingestion of foods rich in calcium, such as milk or infant formula.[19] In rats, a diet rich in calcium increases the fecal fluoride excretion such that fluoride loss equals or exceeds fluoride intake.[20] The incidence of DF among children who did not consume milk (37.4%) was higher than those who consumed milk (7.1%), in two areas in Jiangxi (China) endemic for DF.[21] However, in the present study, no significant correlation was found between DF and the consumption of milk. Cooking in aluminum vessels using fluoridated water results in the formation of aluminum fluoride complexes that get absorbed rapidly from the intestine resulting in fluoride toxicity.[22] In this study, no correlation was found between cooking in aluminum vessels and the occurrence of DF. This could probably be because many of the children were unaware of the type of vessels used for cooking at home. A significant correlation was found between the occurrence of DF and the ppm of fluoride in the drinking water of a particular school (P = 0.043). The prevalence of DF was greatest in Magudamchavady (92.43%) where the school water fluoride level was 3 ppm and least in Gangavalli and Yercaud where the school water fluoride level was 0 ppm. DF was also found in children from three other blocks, where the quantity of fluoride in school drinking water was found to be 0 ppm. This could have probably occurred due to the consumption of water with high fluoride levels at home. A similar observation was made in a study conducted at Kanyakumari (Tamil Nadu) where areas with low fluoride levels in drinking water showed higher occurrence of DF and vice versa.[9] A study conducted in Andhra Pradesh (India) revealed that the level of fluoride in ground water would vary based on various factors such as the depth of borewells, distance from the sea, levels of chloride/calcium/magnesium, pH, and alkalinity.[23] These factors would have also affected the results of the present study.
Conclusion
The prevalence of DF is significantly high among the children of Salem (Tamil Nadu, India), where the water fluoride level was found to be between 0 and 3 ppm. DF was most commonly seen in 9 years old children than in children of higher ages. The prevalence of DF was greater in males. The occurrence of DF was directly proportional with the duration of residence in a place with high water fluoride content. There was a direct correlation between the occurrence of DF, bore well water consumption, black tea consumption, and the fluoride content in drinking water. However, no correlation was found between DF, dental caries, consumption of milk, or the consumption of foods cooked in aluminum vessels.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Susheela AK. Fluorosis management programme in India. Curr Sci. 1999;77:1250–6. [Google Scholar]
- 2.Shortt HE, Pandit CG, Raghavachari TN. Endemic fluorosis in the Nellore district of South India. Indian Med Gaz. 1937;72:396–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Susheela AK, Kumar A, Bhatnagar M, Bahadur R. Prevalence of endemic fluorosis with gastro-intestinal manifestations in people living in some North Indian villages. Fluoride. 1993;26:97–104. [Google Scholar]
- 4.Sendesh Kannan K, Ramasubramanian V. Assessment of fluoride contamination in ground water using GIS, Dharmapuri district, Tamil Nadu, India. Int J Eng Sci Technol. 2011;3:1077–85. [Google Scholar]
- 5.Ramesh M, Shankar R, Krishnan R, Malathi N, Aruna RM. Prevalence of dental fluorosis in the district of Salem, Tamil Nadu, South India: A pilot study. J Orofac Sci. 2014;6:37–40. [Google Scholar]
- 6.Rozier RG. Epidemiologic indices for measuring the clinical manifestations of dental fluorosis: Overview and critique. Adv Dent Res. 1994;8:39–55. doi: 10.1177/08959374940080010901. [DOI] [PubMed] [Google Scholar]
- 7.Choubisa SL, Choubisa L, Choubisa D. Osteo-dental fluorosis in relation to age and sex in tribal districts of Rajasthan, India. J Environ Sci Eng. 2010;52:199–204. [PubMed] [Google Scholar]
- 8.Kotecha PV, Patel SV, Bhalani KD, Shah D, Shah VS, Mehta KG. Prevalence of dental fluorosis and dental caries in association with high levels of drinking water fluoride content in a district of Gujarat, India. Indian J Med Res. 2012;135:873–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Murugan A, Subramanian A. Studies on dental fluorosis in low fluoride areas in the Southern Most Parts of India. Aust J Basic Appl Sci. 2011;5:329–33. [Google Scholar]
- 10.Gopalakrishnan P, Vasan RS, Sarma PS, Nair KS, Thankappan KR. Prevalence of dental fluorosis and associated risk factors in Alappuzha district, Kerala. Natl Med J India. 1999;12:99–103. [PubMed] [Google Scholar]
- 11.Periakali P, Subramanian S, Eswaramoorthi S, Arul B, Rao NR. Distribution of fluoride in the ground water of Salem and Namakkal districts, Tamil Nadu. J Appl Geochem. 2001;3:120–32. [Google Scholar]
- 12.Aldrees AM, Al-Manea SM. Fluoride content of bottled drinking waters available in Riyadh, Saudi Arabia. Saudi Dent J. 2010;22:189–93. doi: 10.1016/j.sdentj.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mills K, Falconer S, Cook C. Fluoride in still bottled water in Australia. Aust Dent J. 2010;55:411–6. doi: 10.1111/j.1834-7819.2010.01262.x. [DOI] [PubMed] [Google Scholar]
- 14.Wondwossen F, Astrøm AN, Bårdsen A, Bjorvatn K. Perception of dental fluorosis amongst Ethiopian children and their mothers. Acta Odontol Scand. 2003;61:81–6. doi: 10.1080/00016350310001415. [DOI] [PubMed] [Google Scholar]
- 15.Tuli A, Rehani U, Aggrawal A. Caries experience evidenced in children having dental fluorosis. Int J Clin Pediatr Dent. 2009;2:25–31. doi: 10.5005/jp-journals-10005-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heller KE, Eklund SA, Burt BA. Dental caries and dental fluorosis at varying water fluoride concentrations. J Public Health Dent. 1997;57:136–43. doi: 10.1111/j.1752-7325.1997.tb02964.x. [DOI] [PubMed] [Google Scholar]
- 17.Li C, Ni D. Effect of fluoride on chemical constituents of tea leaves. Fluoride. 2009;42:237–43. [Google Scholar]
- 18.Pehrsson PR, Patterson KY, Perry CR. The fluoride content of select brewed and microwave-brewed black teas in the United States. J Food Compos Anal. 2011;24:971–5. [Google Scholar]
- 19.Spak CJ, Ekstrand J, Zylberstein D. Bioavailability of fluoride added by baby formula and milk. Caries Res. 1982;16:249–56. doi: 10.1159/000260605. [DOI] [PubMed] [Google Scholar]
- 20.Whitford GM. Intake and metabolism of fluoride. Adv Dent Res. 1994;8:5–14. doi: 10.1177/08959374940080011001. [DOI] [PubMed] [Google Scholar]
- 21.Chen YX, Lin MQ, Xiao YD, Gan WM, Min D, Chen C. Nutrition survey in dental fluorosis-afflicted areas. Fluoride. 1997;30:77–80. [Google Scholar]
- 22.Khandare A, Rasaputra K, Meshram I, Rao S. Effects of smoking, use of aluminium utensils and tamarind consumption on fluorosis in a fluorotic village of Andhra Pradesh, India. Fluoride. 2010;43:128–33. [Google Scholar]
- 23.Rao OK, Venkateswarlu P. Concentration of fluoride in ground water and its distribution between coastal and central areas in S.P.S.R. Nellore district. Rasayan J Chem. 2011;4:488–91. [Google Scholar]


