Abstract
The aim of the present study was to compare the techniques of dynamic intensity-modulated radiation therapy (IMRT) and three-dimensional conformal radiotherapy (3DCRT) in patients with gastric cancer. Implementation of the IMRT technique does not significantly affect the minimum and maximum dose levels in the planning target volume (PTV), but more effectively protects the critical organs. The study group consisted of 25 patients. The results of the analysis of the conformity index (CI) and the homogeneity index (HI) showed that the doses in the PTV regions were at a comparable level. The CI for the PTV was 0.95 for the 2-field technique, 0.95 for the 3-field technique, 0.96 for the 4-field technique and 0.94 for the IMRT technique. The CIs for these techniques for the clinical target volume (CTV) were 0.96, 0.96, 0.97 and 0.96, respectively, and the CIs for the gross tumor volume (GTV) were 0.99, 0.99, 0.99 and 0.98, respectively. The HI values for the PTV were 1.12 for the 2-field technique, 1.12 for the 3-field technique, 1.09 for the 4-field technique and 1.09 for the IMRT technique, and the HI values for the CTV were 1.12, 1.12, 1.09 and 1.08 for the same techniques, respectively. The HI values for the GTV were 1.09, 1.09, 1.07 and 1.06, respectively, which indicated significantly superior performance in the regions of healthy tissue. Statistical study was based on Friedman's rank analysis of variance to determine the level of reliability of the tested groups of variables (P<0.001). The present study demonstrated that the IMRT technique in the pre-operative radiotherapy of gastric cancer patients results in superior treatment tolerance and reduces the risk of damage to healthy tissue that is in close proximity to the irradiated area.
Keywords: gastric cancer, neoadjuvant chemoradiotherapy, radiation therapy, three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, protection of organ at risk
Introduction
In 2012, 952,000 new cases of gastric cancer were registered, making the disease the fourth most common cancer in the world (1). Gastric cancer was the third leading cause of mortality due to malignant neoplasms (723,000 cases). The treatment results for this cancer remain disappointing. The 5-year survival rate ranges from 10 to 30% across Europe (2). Since the publication of the results of the INT 0116 study, post-operative chemoradiotherapy has become the standard of care in a number of cancer centers around the world (3). Ongoing studies are focused on improving the efficacy of the local treatment of gastric cancer. One promising direction of this research is the use of pre-operative radiotherapy or chemoradiotherapy (4–10). Neoadjuvant therapy reduces the incidence of unresectable cases, increases the proportion of R0 resections and reduces the risk of local recurrence (5,7,11).
Initially, radiation therapy was based on the schema of two opposing fields, but treatment has gradually evolved towards multi-field techniques (9). Currently, radiotherapy offers the possibility of using radiation in the treatment of gastric cancer through non-coplanar, dynamic or rotating techniques, which make it possible to better protect organs at risk and potentially reduce the risk of radiation-induced reactions while retaining high conformity of the treatment plan (12). Over the last few years, the use of intensity-modulated radiation therapy (IMRT) has been increasing rapidly. There have been few publications on the technical aspects of pre-operative radiotherapy (13,14). At the Institute of Oncology, Gliwice Branch (Gliwice, Poland), pre-operative radiotherapy has been the subject of intense clinical research over the past 10 years.
The aim of the present study was to compare the plans created using the three-dimensional conformal radiation therapy (3DCRT) and dynamic IMRT techniques to assess the possibility of better protection of organs at risk and healthy tissues in patients with gastric cancer treated with pre-operative chemoradiotherapy.
Patients and methods
The present study received approval from the Ethics Committee of the Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology, Gliwice Branch (KB/493-59/09). The study group consisted of 25 patients (19 male, 6 female; average age, 69 years) with gastric cancer [adenocarcinoma T1-T4, N0-N3 and GI-GIII, according to AJCC (15)], who were treated at the Institute of Oncology, Gliwice Branch, between January 2006 and December 2011. All patients were administered neoadjuvant chemoradiotherapy. The total dose was 45 Gray (Gy) administered over five weeks (1.8 Gy per fraction). During chemotherapy, 325 mg/m2 5-fluorouracil (days 1–5) was applied.
Treatment and planning
Treatment planning was based on computed tomography (CT) scanning in the therapeutic position (supine, with the hands raised above the head) in a thermoplastic stabilizer (Somatom Definition Edge, Siemens AG, Munich, Germany). CT scanning was performed with contrast (uropolin) in 3-mm steps. Each patient drank 500 ml of water to fill the stomach, thus enhancing tumor visibility. Gross tumor volume (GTV) indicates a tumor that is visible on the CT scans. Area of clinical target volume (CTV) included a gastric tumor along with 5-cm margins (usually the stomach) and the regional lymph nodes: Perigastric, celiac trunk, splenic, pancreatic-duodenal, supra-pancreatic, portal vein and para-aortic (16). Planning target volume (PTV) was determined by adding a 1-cm margin around the CTV. On each 3DCT, the following critical organs were traced: Liver, left and right kidney, pancreas, spinal canal, intestine and spleen. All patients were treated using IMRT plans, and the 3DCRT plans have been added for comparison.
The planned total pre-operative radiotherapy dose in the patients with gastric cancer was 45 Gy in 25 fractions.
The treatment plans for each patient were developed on the Eclipse treatment planning system (version 10.0; Varian Medical Systems UK Ltd., Crawley, UK). Plans were created using the 2-field technique, the multi-field (three- and four-field) technique and the IMRT technique. Treatment plans met the criteria recommended in Reports 50 and 62 by the International Commission on Radiation Units and Measurements (ICRU; www.icru.org), determining the level of the minimum dose to the PTV of 95% and a maximum dose not exceeding 107%.
Assumptions and parameters
Plans were compiled with the following assumptions for the protection of the organs at risk: Less than 30% of the liver volume received 30 Gy isodose (V30 of 30%); less than 30% of the kidney volume received 20 Gy isodose (V20 of 30%); and for the spinal canal, a maximum dose of <50 Gy. A significant portion of the pancreas and spleen were always within the area of the PTV.
The treatment plans were approved based on a dose-volume histogram (DVH) analysis using the following determined parameters: The minimum, mean, modal, median and maximum doses in the GTV, CTV and PTV; the maximum, mean and median doses of the spinal canal; the maximum, medium, modal and median doses of the liver, the kidneys, the pancreas and the spleen; and the total volume for the kidney.
In addition, the defined volumes of the aforementioned organs were exposed to 10, 15, 20 and 30-Gy dose ranges and were analyzed for each of the techniques.
Analysis
The V10 to V100 values for the critical organs with respect to the planned radiation dose were also analyzed. The established values for normal tissue dose were based on the healthy tissue overdosage factor (HTOF) of Salt (12,16–18). The conformity index (CI) and the homogeneity index (HI) values for the target volume were calculated according to the following formulae (13,17,19–21): i) CIRTOG = VRI / TV; where the volume of the reference isodose (VRI) is the volume of the PTV receiving a 95% reference/planned dose, and the target volume (TV) is the volume of the PTV. ii) HI = Imax / RI; where Imax is the maximum dose to the target, and RI is the reference dose in the PTV. iii) HTOF = HTVRI / TV; where healthy tissue volume covered by the reference isodose (HTVRI) is the tissue/organ volume that received the planned dose to the PTV.
The level of significance of the results for the individual statistical analysis techniques were based on Friedman's rank analysis of variance (P<0.001). All the statistical computations were performed using Statistica software, version 10 (StatSoft, Inc., Tulsa, OK, USA).
Results
Target volumes
The average minimum dose in the PTV for each technique was as follows: 42.71 Gy (2-field), 42.94 Gy (3-field), 43.33 Gy (4-field) and 42.45 Gy (IMRT). The detailed results are shown in Table I. The average minimum doses in the PTV were compared between each technique with the following P-values: 2 vs. 3 fields, P=0.014; 2 vs. 4 fields, P=0.001; 2 fields vs. IMRT, P=0.270; 3 vs. 4 fields, P=0.006; 3 fields vs. IMRT, P=0.058; and 4 fields vs. IMRT, P=0.001. Only the 4-field technique showed a significant difference in the minimum dose in the PTV compared with the IMRT technique (P=0.001).
Table I.
Parameters of the absorbed dose (Gy) in the planning target volume for three-dimensional conformal radiotherapy and IMRT.
| Technique | Median Dmin (range)a | Median Dmax (range)b | Median Dmean (range)c | Median Dmod (range)d | Median Dmed (range)e |
|---|---|---|---|---|---|
| 2-field | 42.7 (40.5–44) | 50.3 (46.6–53.9) | 46.8 (45.1–49.1) | 46.5 (45.2–48.2) | 46.8 (45.1–49) |
| 3-field | 42.9 (40.5–44.5) | 50.3 (46.1–55.9) | 46.9 (45.1–50) | 46.4 (45–49.2) | 46.8 (45.1–49.7) |
| 4-field | 43.3 (42.7–44.8) | 49.0 (46.2–50.7) | 46.2 (45–47.6) | 46.0 (44.2–47) | 46.1 (45.1–47.5) |
| IMRT | 42.5 (38.4–44.1) | 48.9 (47.3–52.4) | 45.9 (44.5–47.2) | 45.9 (44.1–47.3) | 45.9 (44.5–47.3) |
IMRT, intensity-modulated radiation therapy.
P=0.001
P<0.001
P<0.001
P=0.230
P<0.010. Median Dmin, median of all minimum doses; median Dmax, median of all maximum doses; median Dmean, median of all mean doses; median Dmod, median of all modal doses; median Dmed, median of all median doses.
The average maximum dose values in the PTV for 2 fields, 3 fields, 4 fields and IMRT were 50.3, 50.3, 49.3 and 48.9 Gy, respectively. The location of the maximum dose (Dmax) was tested and compared with the Dmax value for the PTV, external contours and critical organs. The results are shown in Table II.
Table II.
Maximum dose (Gy) in the organs at risk for three-dimensional conformal radiotherapy and IMRT.
| Technique | Spinal canal | Liver | Left kidney | Right kidney | Pancreas | Spleen | External |
|---|---|---|---|---|---|---|---|
| 2-field | 47.71 | 49.89 | 45.73 | 45.78 | 48.12 | 48.21 | 50.99 |
| (45.6–52) | (47.1–53.1) | (27.6–50.8) | (35.3–49) | (46–51.4) | (45.9–51.8) | (47.1–55.5) | |
| 3-field | 43.82 | 49.46 | 45.52 | 44.82 | 48.44 | 49.99 | 50.64 |
| (14.7–48.6) | (46.4–53.6) | (24.8–50.3) | (29.9–48) | (45.7–54.6) | (46–58) | (46.4–58) | |
| 4-field | 38.57 | 48.33 | 45.63 | 44.50 | 47.17 | 47.67 | 49.49 |
| (26.2–46.6) | (46.2–51.1) | (40.5–47.8) | (25.5–56.2) | (45.6–49.2) | (45.9–49.9) | (46.4–58) | |
| IMRT | 41.26 | 47.68 | 42.42 | 40.56 | 47.63 | 48.10 | 49.99 |
| (34.5–50.3) | (45.2–50.7) | (22.5–49.1) | (28.3–47.4) | (44.8–49.9) | (45.9–51.7) | (47.1–571) |
Data are presented as median (range), IMRT, intensity-modulated radiation therapy.
In the 2-field techniques and IMRT, the maximum dose to the PTV was comparable to the maximum dose over the entire volume of the body. This indicates the location of the hot spots in the PTV. However, in the case of the 2-field technique, the maximum dose was reported in the critical organs, which was a vast area that received a high dose.
Conformity and heterogeneity index
The following results were obtained in the CI for the PTV: 0.949 for the 2-field technique, 0.954 for the 3-field technique, 0.962 for the 4-field technique and 0.943 for IMRT (P<0.001). The CI for the CTV amounted to 0.957, 0.961, 0.969 and 0.955 (P<0.001), and the CI for the GTV amounted to 0.988, 0.992, 0.985 and 0. 983 (P<0.001).
In examining the ratio of HI for the PTV, the following results were obtained: 1.118 for the 2-field technique, 1.117 for the 3-field technique, 1.089 for the 4-field technique and 1.087 for IMRT (P<0.001). The CI for the CTV amounted to 1.115, 1.118, 1.088 and 1.082 (P<0.001), and the CI for the GTV amounted to 1.085, 1.087, 1.066 and 1.063 (P<0.001). Analogously, the average dose values for the CTV were determined relative to the PTV volume. The results are shown in Table III.
Table III.
Average dose values (Gy) in the clinical target volume.
| Technique | Median Dmin (range)a | Median Dmax (range)b | Median Dmean (range)c | Median Dmod (range)d | Median Dmed (range)e |
|---|---|---|---|---|---|
| 2-field | 43.0 (41.1–44.7) | 50.2 (46.5–53.8) | 46.8 (45.1–49.2) | 46.5 (45.2–48.2) | 46.0 (45.1–49.1) |
| 3-field | 43.3 (41.2–44.6) | 50.3 (46.1–55.9) | 46.9 (45–50.1) | 46.6 (45–50.1) | 46.9 (45–49.4) |
| 4-field | 43.6 (42.5–44.9) | 49.0 (46.1–50.5) | 46.2 (45–47.6) | 45.9 (44.2–47) | 46.1 (45.1–47.5) |
| IMRT | 43.0 (41–44.1) | 48.7 (46.3–52.4) | 46.0 (44.5–47.2) | 45.9 (44.2–47.3) | 46.0 (44.5–47.3) |
IMRT, intensity-modulated radiation therapy.
P=0.001
P<0.001
P=0.010
P=0.110
P=0.010. Median Dmin, median of all minimum doses; median Dmax, median of all maximum doses; median Dmean, median of all mean doses; median Dmod, median of all modal doses; median Dmed, median of all median doses.
The CI indices for the studied techniques for the average of the minimum dose in the GTV, CTV and PTV were essentially ranked at the same level. The interpretation of the minimum dose distribution in the target volume should be based on all plans for a highly satisfactory result in the tested range. Analysis of the coefficient of HI describing the dose homogeneity indicates a clear difference in the assessment of the 3DCRT and IMRT plans. While the best uniformity of the dose distribution was observed with the dynamic techniques (1.08), the HI indices for the two- and three-field techniques (1.12) were relatively high, although they did not exceed the maximum dose of the tolerable minimum dose level. The high toxicity of the combined treatment for post-operative gastric cancer should be carefully considered; it partially covered the PTV, but also affected healthy tissue and critical organs. Minimizing the hot spots in the target areas and hence producing better uniformity while reducing the total dose to the critical organs should ensure less toxic radiation.
HTOF assumes values from 0 to 0.5. Values close to 0.5 indicate a high dose to the study volume, whereas values closer to 0 indicate that the study volume is less vulnerable. Table IV show HTOF values for the organs at risk.
Table IV.
Mean healthy tissue overdosage factor values for the organs at risk for three-dimensional conformal radiotherapy and IMRT.
| Technique | Spinal canal | Liver | Pancreas | Spleen | Left kidney | Right kidney |
|---|---|---|---|---|---|---|
| 2-field | 0.27 | 0.13 | 0.46 | 0.41 | 0.22 | 0.10 |
| 3-field | 0.22 | 0.17 | 0.46 | 0.40 | 0.19 | 0.12 |
| 4-field | 0.18 | 0.23 | 0.45 | 0.39 | 0.18 | 0.09 |
| IMRT | 0.17 | 0.17 | 0.45 | 0.36 | 0.12 | 0.07 |
IMRT, intensity-modulated radiation therapy.
Spinal canal
The criterion for the maximum dose to the spinal canal of <45 Gy was not fulfilled in the 2-field plans (47.7 Gy); in the other techniques, the average maximum dose was <44 Gy.
Liver
The criterion for the protection of the liver was a V30 of 30%. This value was obtained for 64% of the plans for the 2-field technique, 68% of the plans for the 3-field technique, 52% of the plans for the 4-field technique and 80% of the plans for IMRT. The average dose was fulfilled only for the 2-field and IMRT plans, reaching 27.1 Gy and 24.8 Gy, respectively. In other multi-field techniques, a 30-Gy dose was administered to higher than 30% of the liver volume (Table V).
Table V.
Liver volume (%) values in association with dose (Gy) (P<0.001).
| Technique | 10 Gy | 15 Gy | 20 Gy | 30 Gy |
|---|---|---|---|---|
| 2-field | 39.2 (19–79) | 35.8 (17–69) | 32.2 (16–56) | 27.1 (13–49) |
| 3-field | 53.0 (20–90) | 39.8 (18–80) | 35.7 (17–76) | 31.0 (15–68) |
| 4-field | 82.0 (63–96) | 68.6 (20–95) | 58.7 (17–92) | 32.9 (16–61) |
| IMRT | 65.1 (22–90) | 53.8 (17–88) | 42.4 (14–81) | 24.8 (11–40) |
Data are presented as median (range) % values. IMRT, intensity-modulated radiation therapy.
Pancreas and spleen
In the case of the spleen and pancreas, there are no guidelines for their protection during radiotherapy for stomach cancer (Tables VI and VII).
Table VI.
Association between irradiated volume of the pancreas (%) and absorbed dose (Gy) for three-dimensional conformal radiotherapy and IMRT (P<0.39–0.86).
| Technique | 10 Gy | 15 Gy | 20 Gy | 30 Gy |
|---|---|---|---|---|
| 2-field | 100.0 | 99.9 | 99.8 | 99.7 |
| 3-field | 99.9 | 99.8 | 99.8 | 99.7 |
| 4-field | 100.0 | 100.0 | 99.8 | 99.4 |
| IMRT | 100.0 | 99.9 | 99.9 | 99.6 |
Data are presented as the median % values. IMRT, intensity-modulated radiation therapy.
Table VII.
Association between irradiated volume of the spleen (%) and absorbed dose (Gy) for three-dimensional conformal radiotherapy and IMRT (P=0.02).
| Technique | 10 Gy | 15 Gy | 20 Gy | 30 Gy |
|---|---|---|---|---|
| 2-field | 96.6 (53–100) | 95.3 (48–100) | 93.8 (42–100) | 90.5 (34–100) |
| 3-field | 97.7 (67–100) | 96.4 (63–100) | 94.9 (58–100) | 90.5 (48–100) |
| 4-field | 97.7 (66–100) | 96.7 (60–100) | 94.8 (55–100) | 87.4 (39–100) |
| IMRT | 95.9 (48–100) | 93.9 (40–100) | 91.1 (32–100) | 83.0 (15–100) |
Data are presented as median (range) % values. IMRT, intensity-modulated radiation therapy.
Right and left kidney
The criterion for the protection of the kidneys was a V20 of 30%, and it was met in the case of the right kidney. For the left kidney, only the IMRT plans allowed a dose of <20 Gy in 30% of its volume to be obtained. For the left kidney, this value was obtained for 24% of the plans for the 2-field technique, 24% of the plans for the 3-field technique, 28% of the plans for the 4-field technique and 64% of the plans for IMRT (P=0.030). In the patients treated with the 3DCRT technique, in which it was not possible to obtain a predetermined criterion dose/volume for each kidney, the method of summing up the volume of the two kidneys was used, and the DVH evaluation was performed for the acceptance of the treatment plan in accordance with a predetermined criterion. Table VIII shows the association between the volumes of the right and left kidneys and the dose levels of 10, 15, 20 and 30 Gy (P<0.001).
Table VIII.
Asocation between irradiated volume of the right and left kidney and absorbed dose for three-dimensional conformal radiotherapy and IMRT.
| Technique | 10 Gy | 15 Gy | 20 Gy | 30 Gy |
|---|---|---|---|---|
| Right kidney | ||||
| 2-field | 33.8 (4–71) | 28.2 (3–65) | 24.0 (2–58) | 18.5 (0–49) |
| 3-field | 41.4 (4–90) | 30.5 (2–71) | 25.5 (1–69) | 18.6 (0–58) |
| 4-field | 36.1 (2–73) | 26.3 (1–53) | 21.0 (0–42) | 11.8 (0–31) |
| IMRT | 27.5 (2–67) | 18.5 (1–53) | 11.9 (0–27) | 4.6 (0–17) |
| Left kidney | ||||
| 2-field | 46.7 (7–90) | 43.3 (2–79) | 40.8 (1–75) | 36.5 (0–61) |
| 3-field | 56.7 (2–99) | 51.5 (1–100) | 47.6 (0–100) | 40.4 (0–100) |
| 4-field | 62.0 (15–100) | 54.7 (10–100) | 49.4 (1–100) | 31.6 (0–91) |
| IMRT | 47.4 (3–100) | 36.4 (2–98) | 26.9 (0.5–85) | 14.5 (0–41) |
Data are presented as median (range) % values. IMRT, intensity-modulated radiation therapy.
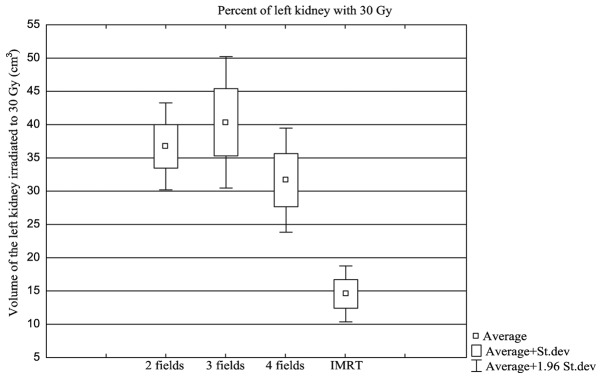
The most interesting result in the protection of critical organs, was observed in the left kidney, which is an organ that is located in the immediate vicinity of the PTV and was exposed to a high dose of radiation during the radiotherapy for stomach cancer (Fig. 1).
Figure 1.
Percentage of the left kidney exposed to 30 Gy in each of the analyzed techniques. St. dev, standard deviation. IMRT, intensity-modulated radiation therapy.
Discussion
Comparisons between conformal treatment planning and IMRT are challenging due to different methods of prescription and reporting of the absorbed doses. ICRU Report 50 used a dose-at-a-point prescription for 3DCRT. By contrast, ICRU Report 83 did not favor a particular point, but favored the volume. This method of treatment planning is based on a dose-volume prescription. ICRU Report 83 changed the methods of dose reporting. This report recommended the near-minimum (D98%) and near-maximum (D2%) values instead of the previously recommended doses. In Report 50, the absorbed dose in the PTV, by definition, ranged from 95–107% of the prescribed absorbed dose. In the present study, a local minimum is accepted, and in this way, an absorbed dose is not dependent on a single computation point. D50% is considered to best correspond to the previously defined dose at the ICRU reference point. The new recommendations emphasize the value of homogeneity and conformity indexes.
The CI for the studied techniques for the average of the minimum dose was ranked practically at the same level for the GTV, CTV and PTV structures. The interpretation of the minimum dose distribution in the target should consider all plans for a highly satisfactory result in the tested range. Analysis of the coefficient of HI describing the dose homogeneity in the test structure shows a clear difference in the assessment of the 3DCRT and IMRT plans. While the best uniformity of the dose distribution is observed with the dynamic techniques (1.08), the HI indices for the 2- and 3-field techniques (1.17) showed a relatively high maximum dose, although the minimum dose level was tolerable. There is a relatively high toxicity of the combined treatment for gastric cancer, where the healthy tissue and the critical organs are covered by the PTV. Minimizing the maximum dose to the target volumes, and, hence, achieving better uniformity should ensure less radiation therapy toxicity.
The greatest differences were observed in the case of the spinal canal and the two kidneys. Relatively low HTOF factor values are associated with the dynamic techniques.
In addition, the occurrence of the largest dose gradient over the external volume also refers to the IMRT techniques. It appears that pre-operative/post-operative radiotherapy should focus on techniques that are currently highly specialized, such as the dynamic techniques, but also the rotary techniques, for example, RapidArc.
A review of the available studies on 3DCRT for gastric cancer published by Morganti et al (22) clearly indicated that conformal techniques do not achieve optimal treatment plans (23). It is more appropriate to focus attention on the possibilities offered by advanced dynamic or rotating techniques. In 2004, Wieland et al described the first attempts to assess the rotational techniques comparing the coverage of large areas of PTV that were planned with IMRT and RapidArc techniques (24). The first report on the results of a comparison of the dynamic techniques (IMRT) and conformal radiotherapy for post-operative gastric cancer was published by Minn et al in 2010 (25). Over a 2-year period, the studied group included 57 patients who were treated with combined chemoradiotherapy. Site treatment success and treatment toxicity were evaluated, and the study concluded that IMRT, in terms of toxicity, is comparable to conformal techniques (61.2 vs. 61.5%). The data regarding the critical organs, such as the liver and the kidneys, were presented based on the dose averages. It was concluded that the IMRT techniques better protect the liver and kidneys. However, there is no indication of the maximum dose level of radiation in the entire volume, which results in high doses to a volume of the intestines and may increase the toxicity of radiation, regardless of the type of radiation therapy used (25). The most recent publication that compared irradiation techniques in patients with gastric cancer was that by Ma et al in 2013; the plans created for 15 patients involving 5- and 7-field IMRT and 3DCRT techniques were evaluated (26). The study assessed the volume of the PTV indices based on CI and HI analysis, as in the present study. The results in terms of dose uniformity in the target area indicated that IMRT was better than conformal techniques. The number of fields ranged from 4 to 8, and the most commonly used was the 5-field technique. The use of the 5-field IMRT techniques did not improve the degradation in the kidney, although at high doses for the liver and spinal canal, IMRT was clearly shown to be a safer technique.
Overall, the use of conformity and homogeneity indices for the evaluation of target volumes indicate that the dynamic techniques provide good GTV, CTV and PTV coverage of high and uniform dose areas during radiotherapy for gastric cancer. Clearly improved protection of organs at risk is ensured with the IMRT technique compared with the conformal techniques. Dynamic techniques should replace the multi-field conformal techniques for gastric cancer radiotherapy, mainly due to the far superior protection of organs at risk. It is, however, also the amount and location of the maximum dose of dynamic plans that should improve treatment tolerance.
Acknowledgements
The original manuscript was edited by Managing Editor-American Journal Experts (www.aje.com).
References
- 1.http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. [Aug 09;2014 ];International Agency for Research on Cancer, World Health Organization: Globocan 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Accessed. [Google Scholar]
- 2.Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F, Capocaccia R. EUROCARE Working Group: EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Reslts and commentary. Eur J Cancer. 2009;45:931–991. doi: 10.1016/j.ejca.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 3.Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, Haller DG, Ajani JA, Gunderson LL, Jessup JM, Martenson JA. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 4.www.nccn.org/professionals/physician_gls/f_guidelines.asp. [Dec 11;2012 ];NCCN: Practice Guidelines in Oncology version 2. 2010 Accessed. [Google Scholar]
- 5.Zhang ZX, Gu XZ, Yin WB, Huang GJ, Zhang DW, Zhang RG. Randomized clinical trial on the combination of preoperative irradiation and surgery in the treatment of adenocarcinoma of gastric cardia (ACG)-report on 370 patients. Int J Radiat Oncol Biol Phys. 1998;42:929–934. doi: 10.1016/S0360-3016(98)00280-6. [DOI] [PubMed] [Google Scholar]
- 6.Sindelar WG, Kinsella TJ. Randomized trial of resection and intraoperative radiotherapy in locally advanced gastric cancer. Proc Ann Meet Am Soc Clin Oncol. 1987;6:A357. [Google Scholar]
- 7.Ito H, Clancy TE, Osteen RT, Swanson RS, Bueno R, Sugarbaker DJ, Ashley SW, Zinner MJ, Whang EE. Adenocarcinoma of the gastric cardia: What is optimal surgical approach? J Am Coll Surg. 2004;199:880–886. doi: 10.1016/j.jamcollsurg.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Ajani JA, Mansfield PF, Janjan N, Morris J, Pisters PW, Lynch PM, Feig B, Myerson R, Nivers R, Cohen DS, Gunderson LL. Multi-institutional trial of preoperative chemoradiotherapy in patients with potentially resectable gastric carcinoma. J Clin Oncol. 2004;22:2774–2780. doi: 10.1200/JCO.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Allal AS, Zwahlen D, Bründler MA, de Peyer R, Morel P, Huber O, Roth AD. Neoadjuvant radiochemotherapy for locally advanced gastric cancer: Long-term results of a phase I trial. Int J Radiat Oncol Biol Phys. 2005;63:1286–1289. doi: 10.1016/j.ijrobp.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 10.Wydmański J, Suwinski R, Poltorak S, Maka B, Miszczyk L, Wolny E, Bielaczyc G, Zajusz A. The tolerance and efficacy of preoperative chemoradiotherapy followed by gastrectomy in operable gastric cancer, a phase II study. Radiother Oncol. 2007;82:132–136. doi: 10.1016/j.radonc.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 11.Hallissey MT, Dunn JA, Ward LC, Allum WH. The second British stomach cancer group trial of adjuvant radiotherapy or chemotherapy in respectable gastric cancer: Five year follow-up. Lancet. 1994;343:1309–1312. doi: 10.1016/S0140-6736(94)92464-3. [DOI] [PubMed] [Google Scholar]
- 12.Huchet A, Caudry M, Belkacémi Y, Trouette R, Vendrely V, Causse N, Récaldini L, Atlan D, Maire JP. Volume-effect and radiotherapy [II] part II: Volume-effect and normal tissue. Cancer Radiother. 2003;7:353–362. doi: 10.1016/S1278-3218(03)00082-9. (In French) [DOI] [PubMed] [Google Scholar]
- 13.Soyfer V, Corn BW, Melamud A, Alani S, Tempelhof H, Agai R, Shmueli A, Figer A, Kovner F. Three-Dimensional non-coplanar conformal radiotherapy yields better results than traditional beam arrangements for adjuvant treatment of gastric cancer. Int J Radiat Oncol Biol Phys. 2007;69:364–369. doi: 10.1016/j.ijrobp.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 14.Matzinger O, Gerber E, Bernstein Z, Maingon P, Haustermans K, Bosset JF, Gulyban A, Poortmans P, Collette L, Kuten A. EORTC-ROG expert opinion: Radiotherapy volume and treatment guidelines for neoadjuvant radiation of adenocarcinomas of the gastroesophageal junction and the stomach. Radiother Oncol. 2009;92:164–175. doi: 10.1016/j.radonc.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Edge BD, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Manual. 7th. Springer-Verlag; New York, NY: 2010. [Google Scholar]
- 16.Wydmański J, Mohanti BK. An appraisal of radiation therapy techniques for adjuvant and neoadjuvant therapy in gastric cancer. J Radiother Pract. 2008;7:67–75. doi: 10.1017/S1460396908006298. [DOI] [Google Scholar]
- 17.Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: A review. Int J Radiat Oncol Biol Phys. 2006;64:333–342. doi: 10.1016/j.ijrobp.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 18.Lomax NJ, Scheib SG. Quantifying the degree of conformity in radiosurgery treatment planning. Int J Radiat Oncol Biol Phys. 2003;55:1409–1419. doi: 10.1016/S0360-3016(02)04599-6. [DOI] [PubMed] [Google Scholar]
- 19.Lefkopoulos D, Dejean C, El-Balma H, Platoni K, Grandjean P, Foulquier J, Schlienger M. Proc. of the XIIIth Intern. Conf. on: Computers in Radiation Therapy. XIIIth ICCR, Heidelberg, Germany: 2000. Determination of dose-volumes parameters to characterise the conformity of stereotactic treatment plans; pp. 356–358. [Google Scholar]
- 20.Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: Final report of RTOG protocol 90–05. Int J Radiat Oncol Biol Phys. 2000;47:291–298. doi: 10.1016/S0360-3016(99)00507-6. [DOI] [PubMed] [Google Scholar]
- 21.Stanley J, Breitman K, Dunscombe P, Spencer DP, Lau H. Evaluation of stereotactic radiosurgery conformity indices for 170 target volumes in patients with brain metastases. J Appl Clin Med Phys. 2011;12:3449. doi: 10.1120/jacmp.v12i2.3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morganti AG, Di Castelnuovo A, Massaccesi M, Cellini F, Cilla S, Macchia G, Forte P, Buwenge M, Digesu C, Ferro M, et al. Planning comparison between standart and conformal 3D techniques in post-operative radiotherapy of gastric cancer: A systematic review. Br J Radiol. 2013;86:20130274. doi: 10.1259/bjr.20130274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leong T, Willis D, Joon DL, Condron S, Hui A, Ngan SY. 3D conformal radiotherapy for gastric cancer-results of a comparative planning study. Radiother Oncol. 2005;74:301–306. doi: 10.1016/j.radonc.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Wieland P, Dobler B, Mai S, Hermann B, Tiefenbacher U, Steil V, Wenz F, Lohr F. IMRT for postoperative treatment of gastric cancer: Covering large target volumes in the upper abdomen: A comparison of step-and-shoot and an arc therapy approach. Int J Radiat Oncol Biol Phys. 2004;59:1236–1244. doi: 10.1016/j.ijrobp.2004.02.051. [DOI] [PubMed] [Google Scholar]
- 25.Minn AY, Hsu A, La T, Kunz P, Fisher GA, Ford JM, Norton JA, Visser B, Goodman KA, Koong AC, Chang DT. Comparison of intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy as adjuvant therapy for gastric cancer. Cancer. 2010;116:3943–3952. doi: 10.1002/cncr.25246. [DOI] [PubMed] [Google Scholar]
- 26.Ma H, Han J, Zhang T, Ke Y. Comparison of dosiology between three dimensional conformal and intensity-modulated radiotherapies (5 and 7 fields) in gastric cancer post-surgery. J Huazhong Univ Sci Technolog Med Sci. 2013;33:759–764. doi: 10.1007/s11596-013-1193-9. [DOI] [PubMed] [Google Scholar]