Abstract
Gingival recession represents a clinical condition in adults frequently encountered in the general dental practice. It is estimated that 23% of adults in the US have one or more tooth surfaces with ≥ 3 mm gingival recession. Clinicians often time face dilemmas of whether or not to treat such a condition surgically. Therefore, we were charged by the editorial board to answer this critical question: “Does gingival recession require surgical treatment?” An initial condensed literature search was performed using a combination of gingival recession and surgery controlled terms and keywords. An analysis of the search results highlights our limited understanding of the factors that often guide the treatment of gingival recession. Understanding the etiology, prognosis and treatment of gingival recession continues to offer many unanswered questions and challenges in the field of periodontics as we strive to provide the best care possible for our patients.
Keywords: Gingival recession, Periodontal attachment loss, Esthetics, Surgical flaps, Connective tissue and Free gingival flaps
Introduction
Gingival recession is defined as when “the location of the gingival margin is apical to the cemento-enamel junction (CEJ)”.1 It is a common dental condition that affects a large number of patients. A survey of adults ranging from 30 to 90 years of age estimated that 23% of adults in the US have one or more tooth surfaces with ≥ 3 mm gingival recession.2 The prevalence, extent, and severity of gingival recession increased with age, with at least 40% of young adults and up to 88% of older adults have at least one site with 1 mm or more of recession (Table 1).3–5 Interestingly, other periodontal (e.g., oral hygiene and gingival bleeding) and health parameters (e.g., diabetes and alcohol intake) were not associated with the extent of recession.4
Table 1.
Study Documentation of Prevalence of Gingival Recession.
| Study Reference | Prevalence (%) | Adult Population Defined by | Comments |
|---|---|---|---|
| 2 | 23 | ≥ 3mm of recession | • NHANES Survey 1988–1994 |
| 3 | 50 | > 50 years of age with ≥ 1 sites | • Found in patients with both good and poor oral hygiene |
| 88 | > 65 years of age with ≥ 1 sites | • Facial surfaces most commonly affected | |
| 4 | 85 | Adults with ≥ 1 sites | • French population studied • Risk factors: age, gender, plaque index, smoking, missing teeth and gingival bleeding |
| 5, 6 | 40 | 16 – 25 years of age | • Evaluated facially-positioned teeth |
| 80 | 36 – 86 years of age |
Therapeutic options for recessions have been well documented with a high degree of success. Soft tissue grafting procedures represent one of the most common periodontal surgical procedures performed in the U.S., with periodontists performing on average over 100 of these procedures per year [ADA survey 2005–06]. What is not so clear is the etiology of this condition, the role of possible causative factors, and the need for treatment. With such a prevalent condition, it becomes critical to discriminate when to treat these lesions and which types of lesions require surgical treatment. The goal of this review is to examine these questions regarding this very common oral condition as well as to provide an overview of what is known about gingival recession defects and their treatment.
Etiology
The etiology of gingival recession is multifactorial; therefore, a single factor alone may not necessarily result in the development of gingival recession. Factors associated with gingival recession may be broadly categorized into two types, predisposing factors and precipitating factors, as summarized in Table 2. Predisposing factors are mainly variations of developmental morphology that may impose a higher risk of recession, while precipitating factors are acquired habits or conditions that introduce gingival recession.
Table 2.
Common risk factors of Gingival Recession.
| Predisposing factors | Precipitating factors |
|---|---|
|
|
(1) Predisposing factors
As the alveolar bone supports the overlying soft tissue, conditions that may cause bone dehiscence/fenestration defects are thought to increase the risk of developing gingival recession. Malpositioned teeth, especially facially positioned teeth are likewise thought susceptible to recession over time.5, 6
While it seems obvious that the lack of facial alveolar bone would lead to increased risk of gingival recession, it is not quite so simple. The prevalence of recession in these studies are not very different from the overall prevalence rates for recession.3–6 Furthermore, as any practitioner of periodontal surgery can attest, patients frequently have no facial alveolar bone without any signs of recession (Figure 1). Therefore, while the lack of alveolar bone may be a predisposing factor, there must be other factors that more directly contribute to this type of loss of gingival tissues.
Figure 1.

Differences between bone thickness and soft tissue recession. Clinical appearance (A) of lower left posterior quadrant of a 40 year old patient showing minimal signs of gingival recession in the absence of buccal bone over the teeth as evident in cone beam computer tomography images (B and C).
Gingival recession is thought to be more common in patients with thinner gingival tissues, compared to those with thicker gingival tissues. Facial gingival thickness has been positively associated with its underlying alveolar plate thickness.7 It seems likely that thinner tissue would be more susceptible to recession than thicker tissue, after non-surgical or surgical periodontal treatment.8, 9 Teeth with more prominent roots may have thinner alveolar bone and gingival tissues on the facial aspect creating a predisposing condition for recession, but as with alveolar bone it is not clear that lack of tissue thickness alone causes facial recession. Again, with thin gingival tissue as a predisposing factor recession may only develop in the presence of concurrent precipitating factors, e.g. inflammation and trauma, etc. While unproven, any differences in risk of gingival recession apparent between thin and thick tissue may be due more directly to precipitating factors involved. Without these precipitating factors, the gingival margin with thin tissues or lack of alveolar bone could remain unchanged.
Another factor frequently cited as a predisposing factor leading to gingival recession is a frenum pull. It is thought that when the attachment of the frenum is proximate to the gingival margin, the repeated stretch of the frenum during oral function could exert forces somehow compromising the mucosal tissue margin or oral hygiene in leading to gingival recession. However, cross-sectional studies failed to demonstrate an association of recessions with high frenum attachment.10, 11
Inadequate keratinized mucosa (KM), most commonly defined as equal or less than 2 mm, is frequently observed concurrently with gingival recession. Historically, it has been considered a predisposing factor of gingival recession. A cross-sectional study12 established a correlation between inadequate keratinized mucosa and increased gingival inflammation, which is a precursor of periodontal diseases leading to gingival recession. However, inadequate keratinized mucosa might simply be a consequence of gingival recession, rather than a cause of gingival recession. This is supported by an interventional, longitudinal study13 that concluded the attachment level could be maintained with control of gingival inflammation, even without adequate KM. This study with 32 subjects concluded that sites with insufficient attached mucosa (≤2 mm) due to gingival recession did not lose attachment or have additional recession over a period of 6 years. In the presence of inflammation, patients without adequate KM showed continuous attachment loss and additional recession. Therefore, poor oral hygiene may be considered a precipitating factor for gingival recession. However, another split-mouth design study14 following 73 subjects for 10 to 27 years found that teeth with recessions without receiving surgical treatment experienced an increase of the recession by 0.7–1.0 mm. Further, new recessions developed in 15 sites during the study period in the absence of inflammation. In contrast, teeth with gingival recession receiving a free gingival graft had a reduction of gingival recession by approximately 1.5 mm through creeping attachment. Therefore, although anatomic variants considered to be predisposing factors leading to recession do not always require treatment, with concurrent precipitating factors, surgical intervention may be indicated.
(2) Precipitating factors
The role of oral hygiene practices as contributing to the occurrence of gingival recession remains a major consideration in our understanding of the etiology, the prognosis, and the treatment. It is important to recognize that gingival recession may be associated with both extremes of oral hygiene; one occurring in patients with extremely good oral hygiene and the other in those with unfavorable oral hygiene as described above. In the former type, meticulous brushing is thought to introduce trauma to the gingiva leading to recession.15, 16 This type of recession is commonly seen on the facial side of canines and premolars and associated with overzealous brushing habits. Contrarily, poor oral hygiene is associated with recession due to plaque-induced inflammation and subsequent attachment loss. Surprisingly while the role of traumatic tooth brushing as a precipitating factor to gingival recession is well accepted, the evidence in support of this concept remains limited. It appears that a number of factors related to tooth brushing may contribute to recession. These factors include brushing force and brush hardness, frequency and duration of tooth brushing, as well as frequency of changing tooth brushes and the brushing techniques and types of manual or electric brushes used.17 In cases of both overzealous and insufficient oral hygiene, an underlying inflammatory response is likely to contribute to tissue destruction resulting in gingival recession. Another precipitating factor for recession is alveolar bone and soft tissue remodeling associated with generalized periodontal disease (Figure 2) or tooth extraction. This commonly occurs in the proximal sites of teeth adjacent to the extraction site and often results in circumferential exposure of root surfaces of involved teeth.
Figure 2.

Demonstration of generalized gingival recession due to chronic periodontitis, especially the mandibular anterior teeth. The chronic and horizontal pattern of the periodontium and the alveolar bone often result in circumferential exposure of root surfaces of several teeth.
Less commonly found, but clinically important, local gingival tissue trauma or irritation as found with tobacco chewing and oral piercing can lead to inflammatory changes in the tissues resulting in gingival recession.18 When smokeless tobacco is used, the tobacco is kept in the vestibule adjacent to mandibular incisors or premolars for a prolonged time. The gingival tissues can experience mechanical or chemical injury with the consequence of a recession.19 In the presence of labial or lingual piercings gingival recession is found in up to 80% of pierced individuals in mandibular and maxillary teeth.19 Additionally, oral piercing poses a 11-fold greater risk for developing gingival recession.19
One frequent concern for gingival recession is with orthodontic tooth movement (Figure 3).20 The risk for gingival recession in the mandibular incisors during or after orthodontic therapy is much studied, yet research in this area remains inconclusive. Most commonly, studies have evaluated orthodontic repositioning of the mandibular incisors as proclination, with the forward tipping or bodily movement more likely to lead to thinner alveolar bone and soft tissues on the facial aspect of the tooth, and retroclination, leading to an increased thickness of facial tissues. Studies evaluating the effects of orthodontic treatment on gingival recession typically suggest an incidence of 10–20% when evaluated for as long as 5 years following the completion of orthodontic therapy.21–25 These rates of occurrence, considered relative to the overall high prevalence found in adults, suggest that orthodontic tooth movement may provide only a minor contribution to the overall prevalence of gingival recession. Two recent studies have taken this discussion a step further in suggesting that the extent of gingival recession when it occurs following orthodontics may be small and of limited clinical concern, affecting only 10% of patients with most of these being readily treatable as Miller Class I lesions24, 26. These findings suggest that pre-orthodontic periodontal procedures directed at minimizing recession may not be justified in the majority of cases. A recent systematic review of this literature confirmed that while soft tissue augmentation as a pre-orthodontic procedure may be a clinically viable option, this treatment is not based on solid scientific evidence27.
Figure 3.
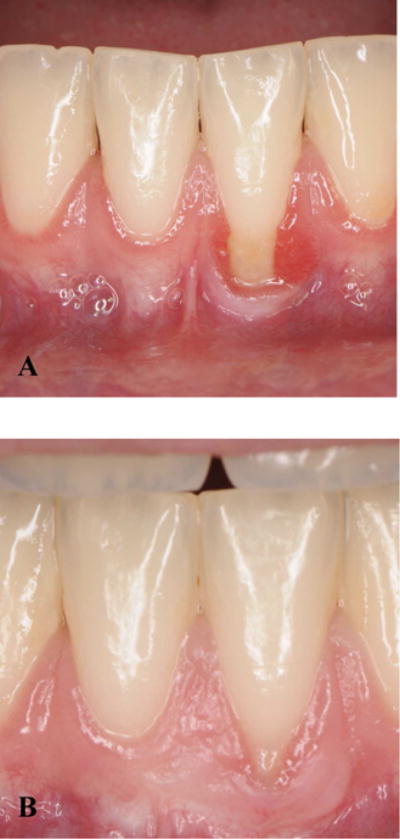
Illustration of an orthodontics-associated gingival recession and treatment. (A) Gingival recession with clinically-evident inflammation around tooth #24 developed during orthodontic treatment, leaving very minimal amount of attached mucosa (B) A free gingival graft was placed with a primary aim to increase the attached mucosa apical to the gingival margin. The soft tissue can be coronally advanced in the future to cover the root.
Courtesy of Dr. Jeff Li, DMD, Graduate Periodontics Resident, University of Michigan School of Dentistry.
Repeated scaling and root planing or periodontal surgeries on shallow pockets may induce clinical attachment loss, partially manifested by gingival recession28. It was concluded that the “critically probing depth” that determines if a certain procedure will gain or lose clinical attachment is 2.9 and 4.2 mm for scaling and root planing and the modified Widman flap procedure, respectively. It is thought that tissue remodeling in sites with shallow pockets during healing following these periodontal procedures may result in minor clinical attachment loss.
Pathogenesis of Gingival Recession
The loss of clinical attachment is apparent either as increased probing depth or as gingival recession29. A pre-clinical study30 inducing gingival recession by replacing rat incisors with acrylic resin implants suggested that gingival recession is associated with (1) local inflammation characterized by mononuclear cells, (2) breakdown of connective tissue and (3) proliferation of the oral and junctional epithelia into the site of connective tissue destruction. The two epithelial layers eventually fuse together, encroaching on the intervening connective tissue. The common keratinized layer differentiated and separated, forming a narrow cleft, bringing about a reduction in height of the gingival margin, which is manifest clinically as gingival recession. Thin tissue seems to recede more often in response to inflammation as a result of trauma to the tissues. Human histology from chronic and acute clefts, and wide recessions confirms the relevance of an inflammatory infiltrate in the pathogenesis of clefts vs. wide recessions.31 In all subtypes of recessions, the epithelium is acanthotic and proliferative and surrounded by an inflammatory infiltrate. In addition, in acute clefts associated with tooth brushing trauma, necrotic cells can be found. In wide recessions the dentogingival epithelium penetrates into the lamina propria, thereby decreasing the width of the lamina propria and allowing the dentogingival and oral epithelia to coalesce and resulting in loss of attachment to the tooth. The inflammatory infiltrate can span the entire thickness of the width of the gingiva thus promoting a recession. In thicker gingiva connective tissue free of inflammatory infiltrate may be interposed between oral and junctional epithelia preventing a recession.32
Factors to be considered for treating gingival recession
Does gingival recession require surgical treatment?” To address the question, the authors first conducted targeted searches in PubMed and Embase to capture a narrow set of studies focused on surgical treatment for gingival recession (Box 1). Reference lists of key studies from this result set were checked for additional studies relevant to the etiology, contributing factors of gingival recession and indications of surgical interventions. Subsequent searches were run in PubMed on themes identified during the initial literature review. An analysis of the search results identified factors that influence the decisions of whether or not to treat gingival recession, and based on which a stratified, evidence-based decision-making process (Figure 4) was formulated. Recessions adjacent to implants were excluded.
Box 1. The PubMed search designed to capture a narrow set of studies on surgical interventions for gingival recession.
(“gingival recession/surgery”[mh] OR (“gingival recession”[majr] OR (“gingival”[ti] AND (“recession”[ti] OR “recessions”[ti]))) AND (“oral surgical procedures”[majr] OR surgery[ti] OR surgeries[ti] OR surgic*[ti] OR operati*[ti])) AND english[la] NOT (animals[mh] NOT humans[mh]) NOT (case reports[pt] OR “case report”[ti])
Figure 4.
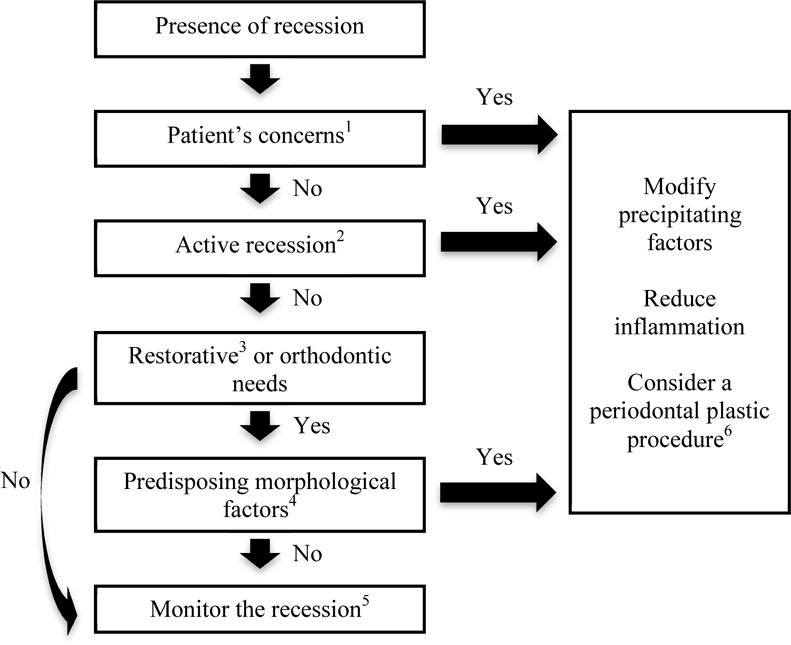
A flow chart of considerations for treating gingival recession. Generally, a periodontal plastic surgery is only rendered to address patients’ concerns or halt an active lesion. As the recession is confounded by multiple factors, currently there is no effective way to predict the occurrence of gingival recession. A preventive procedure is generally not recommended. Clinicians should make the best judgment by taking considerations of various predisposing and precipitating factors. Control of precipitating factors and reduction of periodontal inflammation should always precede a corrective surgery.
1. Patient concerns may include esthetics or root sensitivity, etc.
2. Active recession may be determined by comparing the size of the current lesion to previous records or judged by patient’s impression.
3. Restorative needs with an equal or subgingival margin, abutment for a removable partial denture, especially an RPI-bar denture, and overdenture abutment
4. Predisposing morphological factors may include inadequate keratinized mucosa, frenum pull, and thin tissue-type, etc., that might increase the risk of future recession.
5. Periodontal plastic surgery is not likely needed. However, regular prophylaxis/periodontal maintenance and modifying precipitating factors are required.
6. It is performed to augment the soft tissue either apical (e.g. a free gingival graft to increase the width of the keratinized mucosa) or coronal (a root coverage procedure) to the free gingival margin.
The flowchart starts with a consideration of patient’s concerns, followed by a consideration of the stability of the lesion, whether other dental needs are required, and last existing predisposing morphological factors that may trigger further gingival recession. The factors will be described in detail below.
1) Classification of Recession Defects
Clinically, a widely used classification system was proposed in 1985 by Dr. PD Miller, based on the predictability of achieving root coverage (Table 3).33 Full root coverage is anticipated in Class I and II recessions, in which interproximal tissues are still intact; on the other hand, in Class III recessions, only partial coverage is expected. Minimal root coverage is expected in Class IV recessions.
Table 3.
Diagnosis/Prognosis for Gingival Recession.
Miller’s classification
|
From Miller PD, Jr. Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int J Periodontics Restorative Dent 1985;5(2):14–37; with permission.
2) Patient’s concerns
While dentists view esthetics as the most important reason for root coverage procedures34, patients are often not even aware of recessions on their teeth since most of them are asymptomatic35. Only 28% of the clinically identified recession sites were perceived by patients as such, with a fraction being associated with dentin hypersensitivity or unaesthetic appearance. Female patients were more concerned about esthetics than males. Dentin hypersensitivity associated with gingival recession is more common in younger patients. The large discrepancy in number of diagnosed recessions and patient perceived recessions should prompt the dentist to be mindful when suggesting a root coverage procedure.
Unsatisfactory esthetics
In the event of gingival recession, the affected tooth looks longer and the free gingival margin may become asymmetric comparing right and left quadrants. Because of this unaesthetic appearance, patients may seek dental treatment with sites having an esthetic concern highly variable between patients.36 It is worth noting that few patients may seek esthetic treatment for recession on the mandibular teeth (Figure 5).
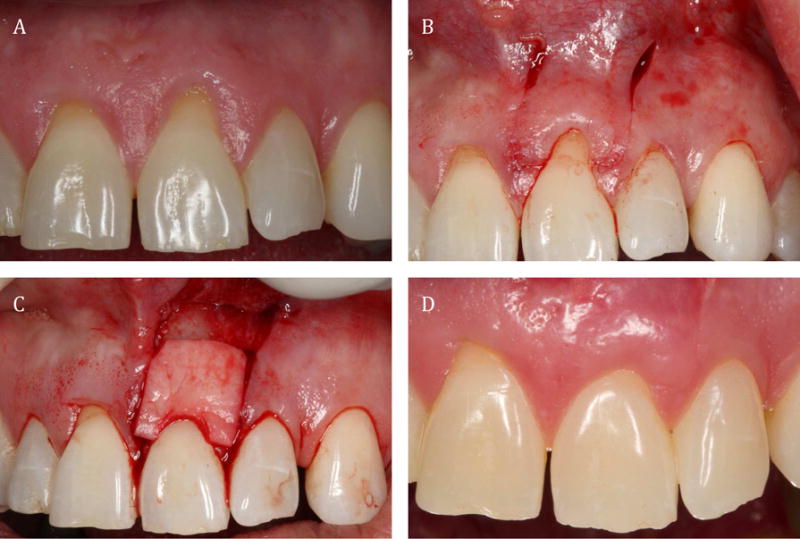
Figure 5.
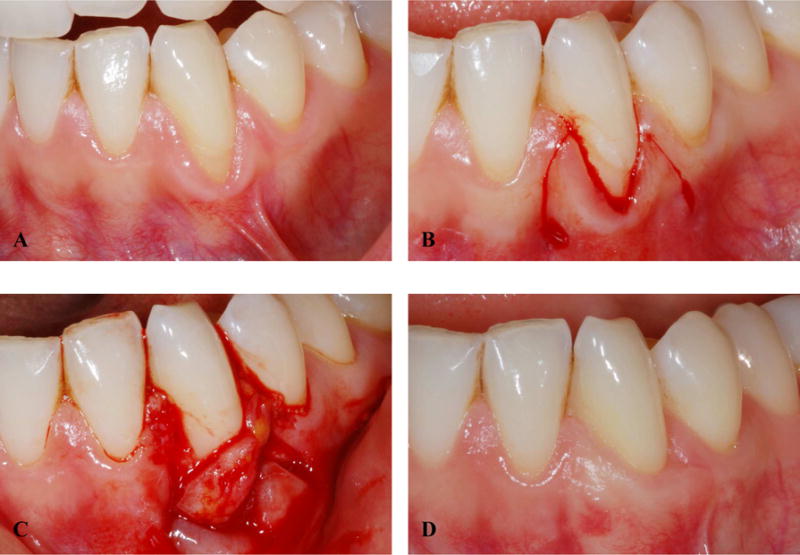
Treatment of gingival recession with a combined approach of coronally-advanced flap (CAF) and subepithelial connective tissue graft (SCTG). (A) An unaesthetic gingival recession site on tooth #22 is possibly due to excessive brushing and labial positioning. Note the potential for the frenum attachment to contribute to future complications. (B) A recipient bed was prepared. (C) A connective graft was harvested and transferred to the recipient site. (D) Six months after the surgery, the root was covered.
Root hypersensitivity
Root hypersensitivity (RS) affects from 3 to 57% of population.37 It is an unpleasant experience that may be initiated by various stimuli, such as cold. It is primarily caused by the exposure of root surfaces to the oral environment as a result of gingival recession.
Surgical root coverage procedures have been utilized to treat RS. A recent systematic review38 evaluated the effect of root coverage procedures for treating RS. Nine studies were included in this review, using various techniques for Miller Class 1 and 2 root coverage, including coronally-advanced flap (CAF) alone, CAF + enamel matrix derivative (EMD), CAF + subepithelial connective tissue graft (SCTG), semilunar coronally positioned flap, and SCTG with resin-modified glass-ionomer restoration. RS was evaluated as being present or absent, directly from the subjects’ opinions in most included articles. The results showed that in 55.55 % to 100 % of the cases RS decreased after a root coverage procedure. From a clinical point of view, it appears that surgical root coverage procedures may treat root hypersensitivity with more than 50% of success rate. This rate of reduction in symptoms may not be different from that found for topical interventions; however there are no studies to date directly making this comparison.39
A multicenter study40 with 85 subjects demonstrated the benefit of performing root coverage procedures for reduction of RS. At the baseline, approximately 40 % of the subjects reported RS as a reason for seeking treatment. At 6 months after randomly treated with CAF or CAF + SCTG, the prevalence of RS reduced to approximately 10 %. However, a systematic review38 found conflicting evidences for surgical root coverage procedures to reduce RS, reflecting our limited evidence confounded by the subjective nature of patients’ perceptions of RS along with extent of the defect and treatment variabilities in obtaining the complete coverage needed for resolution.41,42
3) Active recession (Progression)
A progressive lesion may warrant a surgical intervention to improve periodontal support by increasing the amount of soft tissue attachment and to halt disease progression (Figure 6).43 A longitudinal study44 showed that sites with recession had a higher risk of additional recession. A split-mouth design study14 following 73 subjects for 10 to 27 years found that teeth with gingival recession receiving a free gingival graft had a reduction of gingival recession by approximately 1.5 mm. The contralateral homogenous sites without receiving surgical treatment experienced an increase of the recession by 0.7–1.0 mm during the same timeframe. The clinical ramifications on tooth loss or patient-centered outcomes for this difference were not determined.
Figure 6.
Treatment of an active or progressing gingival recession site. (A) A decision was made to perform a coronally-advanced flap (CAF) and subepithelial connective tissue graft (SCTG) on tooth #3. (B) The graft was secured in place. (C) Results two years after the surgery showed a reversal of the gingival recession.
4) Restorative or orthodontic needs
Teeth with gingival recession may be at a higher risk of developing further recession when receiving a restoration with the potential to compromise the gingival tissues.45, 46. Valderhaug and Birkeland47 evaluated 329 crowns, most of which (59%) were placed subgingivally at the beginning of the study. After 5 years, only 32% of the crown margins remained below the gingival margin, suggesting that almost half of the teeth developed recession, with more attachment loss associated with subgingival restorations. Similarly, studies48, 49 comparing periodontal conditions between abutment and non-abutment teeth of removable partial dentures concluded that significantly more plaque accumulation and inflammation, deeper probing depths and more recession was associated with abutment teeth.
It has been discussed in an earlier section that orthodontic treatment may present a risk factor for gingival recession, although it may affect only 10–20% of patients. Therefore, patients with orthodontic or restorative needs should be closely monitored for signs of recession and may be suggested of surgical intervention, if indicated, especially for those with presence of other risk factors, e.g. thin tissue type.
Treatment goals
There are generally two goals for performing a surgery, depending on the goals an appropriate procedure is chosen: (1) augment soft tissues coronal to the gingival margin (root coverage), and (2) augment soft tissues apical to the gingival margin, that is provide a qualitative change to the existing soft tissues. Generally a root coverage procedure is preferred, especially if the patient’s main concern is the recession itself. However, there are some limitations with which we may not be able to achieve root coverage or the outcome is not predictable, e.g. Miller’s class 3 and 4 recessions.33 While the 2nd goal does not attempt to reduce the amount of recession, it could increase the thickness and width of the attached mucosa, preventing further recession. Many surgical procedures have been developed over the years to reach these goals. Because these procedures are not the focus of this manuscript, we only include a brief summary of commonly performed procedures in Table 4.50, 51
Table 4.
Modalities of treating a gingival recession.
| Modality | 1 - Root Coverage | 2 – Augment Keratinized Tissue |
|---|---|---|
| Goals | Augment soft tissues coronal to the gingival margin | Provide qualitative changes to the soft tissues apical to the gingival margin |
| Purposes |
|
|
| Predictability |
|
More predictable than root coverage procedures |
| Available procedures |
|
|
| Determining factors |
|
|
Data from Tatakis DN, Chambrone L, Allen EP, et al. Periodontal soft tissue root coverage procedures: a consensus report from the AAP regeneration workshop. J Periodontol 2015;86(2 Suppl):S52-5; and Oates TW, Robinson M, Gunsolley JC. Surgical therapies for the treatment of gingival recession. A systematic review. Ann Periodontol 2003;8(1):303–20.
Treatment outcomes of various surgical procedures
The effectiveness of various surgical procedures for correcting Miller Class I or II recessions have been investigated in a few systematic reviews.42, 51–54,55 The mean percentage of root coverage ranges widely from 50% to 97.3%. The coronally-advanced flap with subepithelial connective tissue graft (CAF + SCTG) is considered the gold standard for root coverage, which achieves approximately 80% root coverage. There is some evidence to suggest that the application of biologics, e.g. EMD or PDGF may promote tissue regeneration and increase the prevalence of complete coverage, however definitive studies remain to be done.42, 56 For augmenting soft tissues apical to gingival margin, FGG is still considered the gold standard for increasing the amount of KM.43 The 2nd generation (allografts/xenografts) (Figure 7) and 3rd generation (tissue-engineering) procedures eliminate the need of harvesting autogenous tissues and show promising outcomes.
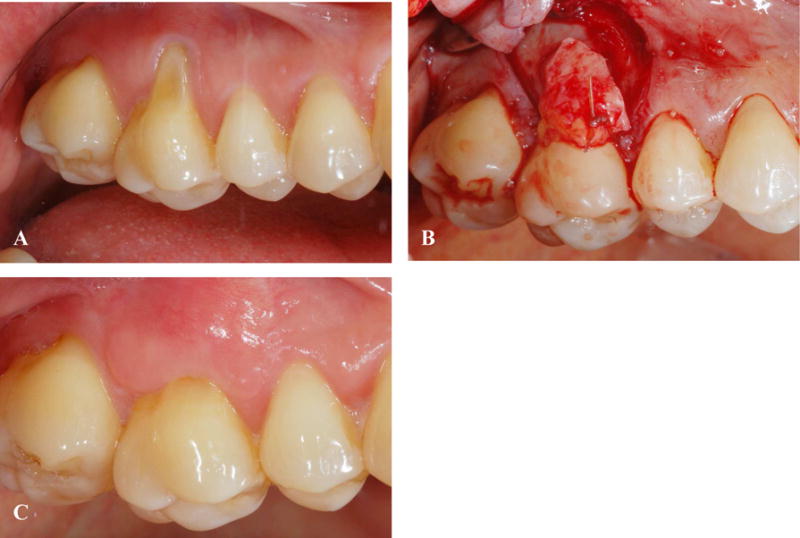
Figure 7.
Demonstration of a root coverage procedure with an allograft. (A) Gingival recession was found on teeth #8 and #9. (B) A coronally advanced flap was planned. (C) An allograft was placed on #9. (D) Results after 12 months showed satisfactory root coverage.
Courtesy of Prof. H-L Wang, Director of Graduate Periodontics Program, University of Michigan
Regarding patient morbidity, it was reported that more than half of the subjects experienced interference of daily life activities from these surgical procedures.40 Approximately 25%–35% of subjects reported some pain after the surgery for about 1 to 2 days, which prompted the use of some pain medications. Therefore, the benefits of receiving a surgery should be weighed carefully with the limited understanding of risks for progression, costs and possible morbidities.
Summary and final remarks
Given the high prevalence of gingival recession, and the therapeutic potential to successfully manage this condition, it is critical that we continue to improve our understanding of the etiology, prognosis, and treatment of this condition to assure that we continue to provide the best, evidence-based care possible. This review of predisposing and precipitating factors discusses common perceptions regarding these factors leading to the development of gingival recession. However, this review also represents how little is truly known in this regard. Our most recent and thorough evaluations of the evidence fail to clarify the role of toothbrushing, frenum attachment, and orthodontic movement in the progression of gingival recession. Furthermore, there is little evidence regarding the effectiveness of common treatments to prevent gingival recession relative to patient-centered outcomes.
While much remains to be known, it is clear that surgical interventions can successfully reduce recession. It is also clear that a small percentage of sites clearly benefit from these interventions. What is less clear is the benefit of the broad application of these interventions in sites with recession. Findings from several studies have suggested limited benefits from surgical interventions. Pini Prato (2000) found only 2 of 8 non-treated buccally erupting premolar sites to show 1 mm of gingival recession after two years, suggesting progression, even minor amounts, is not easily predicted in the absence of treatment. The benefits may also be in question relative to the amount of recession that may occur in the absence of treatment. After 10 to 27 years that, while 34 of 55 untreated sites showed some recession, the amounts of recession recorded after this extended period averaged 0.7 mm and ranged between 0 to 2 mm.14
As we look toward the continued development of evidence-based care, we need to look for new information to clarify these many unanswered questions, but we must always look to offer the best treatment options available to our patients based on what we know at that time within the context of the limitations in our knowledge. Understanding the etiology, prognosis and treatment of gingival recession continues to offer many unanswered questions and challenges in the field of periodontics as we strive to provide the best care possible for our patients.
Key Points.
Gingival recession is defined as when “the location of the gingival margin is apical to the cemento-enamel junction (CEJ)”.
23% of adults in the US have one or more tooth surfaces with ≥ 3 mm gingival recession.
The etiology of gingival recession is multifactorial, confounded by poorly defined contributions from predisposing and precipitating factors.
Predisposing factors include bone dehiscence, tooth malposition, thin soft and hard tissues, inadequate keratinized/attached mucosa, frenum pull, etc.
Precipitating factors include traumatic forces, e.g. excessive brushing, habits, e.g., smoking, oral piercing, plaque-induced inflammation and dental treatment, e.g. certain types of orthodontic tooth movement, equal/subgingival restorations, etc.
Surgical correction of a gingival recession is often considered when (1) a patient raises a concern about esthetics or tooth hypersensitivity, (2) there is active gingival recession, and (3) orthodontic/restorative treatment will be implemented on a tooth with presence of predisposing factors. The benefits of these treatment approaches are not well-supported in current literature relative to alternative approaches with control of possible etiological factors.
Possible surgical modalities for treating a gingival recession include: a root coverage or keratinized tissue augmentation.
A root coverage procedure is to augment soft tissues coronal to the gingival margin. Examples include coronally advanced flap with/without a subepithelial connective tissue graft, and an allograft, etc.
A keratinized tissue augmentation procedure is to provide qualitative changes to the soft tissues apical to the gingival margin. Examples include a free gingival graft and subepithelial connective tissue graft, etc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hsun-Liang Chan, Email: hlchan@umich.edu, Clinical Assistant Professor, Department of Periodontics and Oral Medicine, University of Michigan School of Dentistry, Ann Arbor, MI, Address: R3323B 1011 N. Univ. Ave., Ann Arbor, MI, 48105, Phone: 734-763-9539.
Yong-Hee Patricia Chun, Email: chuny@uthscsa.edu, Assistant Professor, Department of Periodontics, Department of Cellular and Structural Biology, University of Texas Health Science Center at San Antonio, Address: 7703 Floyd Curl Drive, San Antonio, TX, 78229, Phone: 210-567-3520.
Mark MacEachern, Email: markmac@umich.edu, Informationist, University of Michigan Taubman Health Sciences Library, Address: 1135 E Catherine St, Ann Arbor MI, 48105, Phone: 734-763-7406.
References
- 1.Peridontology AAP. Glossary of Periodontal Terms. 2001 [Google Scholar]
- 2.Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70(1):30–43. doi: 10.1902/jop.1999.70.1.30. [DOI] [PubMed] [Google Scholar]
- 3.Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134(2):220–5. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- 4.Sarfati A, Bourgeois D, Katsahian S, Mora F, Bouchard P. Risk assessment for buccal gingival recession defects in an adult population. J Periodontol. 2010;81(10):1419–25. doi: 10.1902/jop.2010.100102. [DOI] [PubMed] [Google Scholar]
- 5.Gorman WJ. Prevalence and etiology of gingival recession. J Periodontol. 1967;38(4):316–22. doi: 10.1902/jop.1967.38.4.316. [DOI] [PubMed] [Google Scholar]
- 6.Bernimoulin J, Curilovie Z. Gingival recession and tooth mobility. J Clin Periodontol. 1977;4(2):107–14. doi: 10.1111/j.1600-051x.1977.tb01890.x. [DOI] [PubMed] [Google Scholar]
- 7.Fu JH, Yeh CY, Chan HL, et al. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81(4):569–74. doi: 10.1902/jop.2009.090591. [DOI] [PubMed] [Google Scholar]
- 8.Anderegg CR, Metzler DG, Nicoll BK. Gingiva thickness in guided tissue regeneration and associated recession at facial furcation defects. J Periodontol. 1995;66(5):397–402. doi: 10.1902/jop.1995.66.5.397. [DOI] [PubMed] [Google Scholar]
- 9.Claffey N, Shanley D. Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol. 1986;13(7):654–7. doi: 10.1111/j.1600-051x.1986.tb00861.x. [DOI] [PubMed] [Google Scholar]
- 10.Lafzi A, Abolfazli N, Eskandari A. Assessment of the etiologic factors of gingival recession in a group of patients in northwest iran. J Dent Res Dent Clin Dent Prospects. 2009;3(3):90–3. doi: 10.5681/joddd.2009.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen-Hieu T, Ha Thi BD, Do Thu H, Tran Giao H. Gingival recession associated with predisposing factors in young vietnamese: a pilot study. Oral Health Dent Manag. 2012;11(3):134–44. [PubMed] [Google Scholar]
- 12.Lang NP, Loe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43(10):623–7. doi: 10.1902/jop.1972.43.10.623. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy JE, Bird WC, Palcanis KG, Dorfman HS. A longitudinal evaluation of varying widths of attached gingiva. J Clin Periodontol. 1985;12(8):667–75. doi: 10.1111/j.1600-051x.1985.tb00938.x. [DOI] [PubMed] [Google Scholar]
- 14.Agudio G, Nieri M, Rotundo R, et al. Periodontal conditions of sites treated with gingival-augmentation surgery compared to untreated contralateral homologous sites: a 10- to 27-year long-term study. J Periodontol. 2009;80(9):1399–405. doi: 10.1902/jop.2009.090122. [DOI] [PubMed] [Google Scholar]
- 15.Addy M, Mostafa P, Newcombe RG. Dentine hypersensitivity: the distribution of recession, sensitivity and plaque. J Dent. 1987;15(6):242–8. doi: 10.1016/0300-5712(87)90045-5. [DOI] [PubMed] [Google Scholar]
- 16.Niemi ML, Sandholm L, Ainamo J. Frequency of gingival lesions after standardized brushing as related to stiffness of toothbrush and abrasiveness of dentifrice. J Clin Periodontol. 1984;11(4):254–61. doi: 10.1111/j.1600-051x.1984.tb02215.x. [DOI] [PubMed] [Google Scholar]
- 17.Rajapakse PS, McCracken GI, Gwynnett E, et al. Does tooth brushing influence the development and progression of non-inflammatory gingival recession? A systematic review. J Clin Periodontol. 2007;34(12):1046–61. doi: 10.1111/j.1600-051X.2007.01149.x. [DOI] [PubMed] [Google Scholar]
- 18.Campbell A, Moore A, Williams E, Stephens J, Tatakis DN. Tongue piercing: impact of time and barbell stem length on lingual gingival recession and tooth chipping. J Periodontol. 2002;73(3):289–97. doi: 10.1902/jop.2002.73.3.289. [DOI] [PubMed] [Google Scholar]
- 19.Robertson PB, Walsh M, Greene J, et al. Periodontal effects associated with the use of smokeless tobacco. J Periodontol. 1990;61(7):438–43. doi: 10.1902/jop.1990.61.7.438. [DOI] [PubMed] [Google Scholar]
- 20.Wennstrom JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14(3):121–9. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 21.Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134(5):652–6. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- 22.Renkema AM, Fudalej PS, Renkema A, Bronkhorst E, Katsaros C. Gingival recessions and the change of inclination of mandibular incisors during orthodontic treatment. Eur J Orthod. 2013;35(2):249–55. doi: 10.1093/ejo/cjs045. [DOI] [PubMed] [Google Scholar]
- 23.Aziz T, Flores-Mir C. A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Aust Orthod J. 2011;27(1):33–9. [PubMed] [Google Scholar]
- 24.Vasconcelos G, Kjellsen K, Preus H, Vandevska-Radunovic V, Hansen BF. Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatment. Angle Orthod. 2012;82(1):42–7. doi: 10.2319/021411-108.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Renkema AM, Fudalej PS, Renkema AA, et al. Gingival labial recessions in orthodontically treated and untreated individuals: a case - control study. J Clin Periodontol. 2013;40(6):631–7. doi: 10.1111/jcpe.12105. [DOI] [PubMed] [Google Scholar]
- 26.Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13(3):127–41. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 27.Kloukos D, Eliades T, Sculean A, Katsaros C. Indication and timing of soft tissue augmentation at maxillary and mandibular incisors in orthodontic patients. A systematic review. Eur J Orthod. 2014;36(4):442–9. doi: 10.1093/ejo/cjt073. [DOI] [PubMed] [Google Scholar]
- 28.Lindhe J, Nyman S, Karring T. Scaling and root planing in shallow pockets. J Clin Periodontol. 1982;9(5):415–8. doi: 10.1111/j.1600-051x.1982.tb02054.x. [DOI] [PubMed] [Google Scholar]
- 29.Beck JD, Koch GG. Characteristics of older adults experiencing periodontal attachment loss as gingival recession or probing depth. J Periodontal Res. 1994;29(4):290–8. doi: 10.1111/j.1600-0765.1994.tb01224.x. [DOI] [PubMed] [Google Scholar]
- 30.Baker DL, Seymour GJ. The possible pathogenesis of gingival recession. A histological study of induced recession in the rat. J Clin Periodontol. 1976;3(4):208–19. doi: 10.1111/j.1600-051x.1976.tb00040.x. [DOI] [PubMed] [Google Scholar]
- 31.Smukler H, Landsberg J. The toothbrush and gingival traumatic injury. J Periodontol. 1984;55(12):713–9. doi: 10.1902/jop.1984.55.12.713. [DOI] [PubMed] [Google Scholar]
- 32.Baker P, Spedding C. The aetiology of gingival recession. Dent Update. 2002;29(2):59–62. doi: 10.12968/denu.2002.29.2.59. [DOI] [PubMed] [Google Scholar]
- 33.Miller PD., Jr Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int J Periodontics Restorative Dent. 1985;5(2):14–37. [PubMed] [Google Scholar]
- 34.Zaher CA, Hachem J, Puhan MA, Mombelli A. Interest in periodontology and preferences for treatment of localized gingival recessions. J Clin Periodontol. 2005;32(4):375–82. doi: 10.1111/j.1600-051x.2005.00690.x. [DOI] [PubMed] [Google Scholar]
- 35.Nieri M, Pini Prato GP, Giani M, et al. Patient perceptions of buccal gingival recessions and requests for treatment. J Clin Periodontol. 2013;40(7):707–12. doi: 10.1111/jcpe.12114. [DOI] [PubMed] [Google Scholar]
- 36.Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent. 1984;51(1):24–8. doi: 10.1016/s0022-3913(84)80097-9. [DOI] [PubMed] [Google Scholar]
- 37.West NX. Dentine hypersensitivity: preventive and therapeutic approaches to treatment. Periodontol 2000. 2008;48:31–41. doi: 10.1111/j.1600-0757.2008.00262.x. [DOI] [PubMed] [Google Scholar]
- 38.Douglas de Oliveira DW, Oliveira-Ferreira F, Flecha OD, Goncalves PF. Is surgical root coverage effective for the treatment of cervical dentin hypersensitivity? A systematic review. J Periodontol. 2013;84(3):295–306. doi: 10.1902/jop.2012.120143. [DOI] [PubMed] [Google Scholar]
- 39.Acharya AB, Surve SM, Thakur SL. A clinical study of the effect of calcium sodium phosphosilicate on dentin hypersensitivity. J Clin Exp Dent. 2013;5(1):e18–22. doi: 10.4317/jced.50955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cortellini P, Tonetti M, Baldi C, et al. Does placement of a connective tissue graft improve the outcomes of coronally advanced flap for coverage of single gingival recessions in upper anterior teeth? A multi-centre, randomized, double-blind, clinical trial. J Clin Periodontol. 2009;36(1):68–79. doi: 10.1111/j.1600-051X.2008.01346.x. [DOI] [PubMed] [Google Scholar]
- 41.Clauser C, Nieri M, Franceschi D, Pagliaro U, Pini-Prato G. Evidence-based mucogingival therapy. Part 2: Ordinary and individual patient data meta-analyses of surgical treatment of recession using complete root coverage as the outcome variable. J Periodontol. 2003;74(5):741–56. doi: 10.1902/jop.2003.74.5.741. [DOI] [PubMed] [Google Scholar]
- 42.Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontol. 2008;35(8 Suppl):136–62. doi: 10.1111/j.1600-051X.2008.01267.x. [DOI] [PubMed] [Google Scholar]
- 43.Greenwell H, Fiorellini J, Giannobile W, et al. Oral reconstructive and corrective considerations in periodontal therapy. J Periodontol. 2005;76(9):1588–600. doi: 10.1902/jop.2005.76.9.1588. [DOI] [PubMed] [Google Scholar]
- 44.Serino G, Wennstrom JL, Lindhe J, Eneroth L. The prevalence and distribution of gingival recession in subjects with a high standard of oral hygiene. J Clin Periodontol. 1994;21(1):57–63. doi: 10.1111/j.1600-051x.1994.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 45.Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control. I. As observed in human biopsy material. J Periodontol. 1978;49(1):1–8. doi: 10.1902/jop.1978.49.1.1. [DOI] [PubMed] [Google Scholar]
- 46.Silness J. Fixed prosthodontics and periodontal health. Dent Clin North Am. 1980;24(2):317–29. [PubMed] [Google Scholar]
- 47.Valderhaug J, Birkeland JM. Periodontal conditions in patients 5 years following insertion of fixed prostheses. Pocket depth and loss of attachment. J Oral Rehabil. 1976;3(3):237–43. doi: 10.1111/j.1365-2842.1976.tb00949.x. [DOI] [PubMed] [Google Scholar]
- 48.Zlataric DK, Celebic A, Valentic-Peruzovic M. The effect of removable partial dentures on periodontal health of abutment and non-abutment teeth. J Periodontol. 2002;73(2):137–44. doi: 10.1902/jop.2002.73.2.137. [DOI] [PubMed] [Google Scholar]
- 49.Wright PS, Hellyer PH. Gingival recession related to removable partial dentures in older patients. J Prosthet Dent. 1995;74(6):602–7. doi: 10.1016/s0022-3913(05)80312-9. [DOI] [PubMed] [Google Scholar]
- 50.Tatakis DN, Chambrone L, Allen EP, et al. Periodontal soft tissue root coverage procedures: a consensus report from the AAP regeneration workshop. J Periodontol. 2015;86(2 Suppl):S52–5. doi: 10.1902/jop.2015.140376. [DOI] [PubMed] [Google Scholar]
- 51.Oates TW, Robinson M, Gunsolley JC. Surgical therapies for the treatment of gingival recession. A systematic review. Ann Periodontol. 2003;8(1):303–20. doi: 10.1902/annals.2003.8.1.303. [DOI] [PubMed] [Google Scholar]
- 52.Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: a systematic review. J Clin Periodontol. 2002;29(Suppl 3):178–94. doi: 10.1034/j.1600-051x.29.s3.11.x. discussion 95–6. [DOI] [PubMed] [Google Scholar]
- 53.Chambrone L, Sukekava F, Araujo MG, et al. Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol. 2010;81(4):452–78. doi: 10.1902/jop.2010.090540. [DOI] [PubMed] [Google Scholar]
- 54.Thoma DS, Benic GI, Zwahlen M, Hammerle CH, Jung RE. A systematic review assessing soft tissue augmentation techniques. Clin Oral Implants Res. 2009;20(Suppl 4):146–65. doi: 10.1111/j.1600-0501.2009.01784.x. [DOI] [PubMed] [Google Scholar]
- 55.Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(2 Suppl):S8–51. doi: 10.1902/jop.2015.130674. [DOI] [PubMed] [Google Scholar]
- 56.McGuire MK, Scheyer ET, Schupbach P. Growth factor-mediated treatment of recession defects: a randomized controlled trial and histologic and microcomputed tomography examination. J Periodontol. 2009;80(4):550–64. doi: 10.1902/jop.2009.080502. [DOI] [PubMed] [Google Scholar]


