Abstract
Objective
To compare the knowledge and use of recommendations for the management of sport-related concussion (SRC) among sport and exercise medicine physicians (SEMPs) and emergency department physicians (EDPs) to assess the success of SRC knowledge transfer across Canada.
Design
A self-administered, multiple-choice survey accessed via e-mail by SEMPs and EDPs. The survey had been assessed for content validity.
Setting
Canada.
Participants
The survey was completed between May and July 2012 by SEMPs who had passed the diploma examination of the Canadian Academy of Sport and Exercise Medicine and by EDPs who did not hold this diploma.
Main outcome measures
Knowledge and identification of sources of concussion management information, use of concussion diagnosis strategies, and whether physicians use common and consistent terminology when explaining cognitive rest strategies to patients after an SRC.
Results
There was a response rate of 28% (305 of 1085). The SEMP and EDP response rates were 41% (147 of 360) and 22% (158 of 725), respectively. Of the responses, 41% of EDPs and 3% of SEMPs were unaware of any consensus statements on concussion in sport; 74% of SEMPs used the Sport Concussion Assessment Tool, version 2 (SCAT2), “usually or always,” whereas 88% of EDPs never used the SCAT2. When queried about how cognitive rest could best be achieved after an SRC, no consistent answer was documented.
Conclusion
Differences and a lack of consistency in the implementation of recommendations for SRC patients were identified for SEMPs and EDPs. It appears that the SCAT2 is used more in the SEMP setting than in the emergency context. Further knowledge transfer efforts and research should address the barriers to achieving more consistent advice given by physicians who attend SRC patients.
Knowledge transfer (KT) efforts play an integral role in educating Canadian physicians about changes in best practices for sport-related concussion (SRC) management.1 This has been emphasized in the 2012 Concussion in Sport Group’s (CISG’s) fourth consensus document, published in March 2013.2 This committee of worldwide experts formulated their consensus statements based on the proceedings at concussion management conferences. The CISG’s 2004 consensus statement was published in specialty journals3 and their 2008 consensus statement was simultaneously published in 5 sport medicine and neurosurgery journals.4 In 2006, members of the ThinkFirst Canada Concussion Education and Awareness Committee recognized a need to educate a larger group of physicians and published an article in Canadian Family Physician to inform primary care physicians about the new consensus statement.5 ThinkFirst Canada (now part of Parachute) has also led this KT effort during the past decade, delivering current and practical management recommendations for SRC to physicians across Canada.6 Timelines for selected KT efforts aimed at Canadian physicians up to 2012 (including this survey) are summarized in Table 1.2–8 Since that time, other useful Canadian websites and guidelines have appeared.9–12 However, the outcome of KT efforts in Canada has not been formally measured and published. The CISG’s 2012 consensus document stresses the importance of appraising current KT efforts in order to construct a comprehensive plan that takes into account different target populations’ specific needs.2
Table 1.
Timeline for selected KT efforts
| KT EFFORT | LOCATION | DATE | KEY FEATURE |
|---|---|---|---|
| First International Conference on Concussion in Sport and consensus statement8 | Vienna | 2001 | Eliminated concussion grading 6-step return to play |
| Second International Conference on Concussion in Sport and consensus statement3 | Prague | 2004 | SCAT Emphasis on cognitive rest |
| ThinkFirst Canada website and resources6 | Canada | 2003–2012 | Lectures and road shows in many Canadian cities |
| Summary of Second International Conference on Concussion in Sport and consensus statement5 | Canada | 2006 | Summary for Canadian family physicians |
| Canadian pediatric concussion guideline7 | Canada | 2006 | Focus on SRC in children |
| Third International Conference on Concussion in Sport and consensus statement4 | Zurich | November 2008 | SCAT2 |
| Current survey of Canadian physicians | Canada | Spring and summer 2012 | Assessment of the success of KT efforts |
| Fourth International Conference on Concussion in Sport and consensus statement2 | Zurich | November 2012 | SCAT3 and Child SCAT3 Greater emphasis on return to school after an SRC |
KT—knowledge transfer, SCAT—Sport Concussion Assessment Tool, SRC—sport-related concussion.
Knowledge transfer research indicates that merely publishing a guideline, although important, has minimal effect on practice.13,14 Investigators have identified 4 types of barriers to guideline dissemination: barriers related to the evidence, the clinician, the consumer, and the context.15 These barriers vary by practice setting and between family physicians and other specialists.16 Health care leaders can address these barriers using a range of activities, from targeting individuals (through increasing the accessibility of information, education, leadership, and competency development) to working with practising professionals and health care teams.14 However, the effectiveness of guideline dissemination and implementation strategies varies across settings.17 Thus, before undertaking further KT efforts, guideline use by physicians needs to be investigated to develop an informed and evidence-based targeted KT strategy.
Although many SRC patients experience timely improvement of symptoms, an unknown percentage have a longer recovery period. In adults with SRCs, brain dysfunction can persist for longer than the usual 7 to 10 days in 10% to 20% of cases.2 Indeed, there is evidence to suggest that younger athletes require a longer recovery period than the typical 7 to 10 days. A study of concussions in high school football players showed that 25% of these young athletes might require 4 weeks for full recovery.18 This proportion of patients who have a longer SRC recovery is potentially affected by the variation in the quality and consistency of the management advice given by physicians early in the postconcussion treatment course.
A chart review of SRC patients led the authors to question why emergency department physician (EDP) management of SRC did not appear to be consistent from one case to the next.19 Our expectation was that sport and exercise medicine physicians (SEMPs) across Canada had SRC management expertise and used this in a consistent manner. We wanted to inquire whether EDPs truly do employ similar SRC management strategies. This study reports on the second arm of our group’s validated survey of Canadian physicians regarding the consistency of SRC management. The first arm surveyed family physicians, EDPs, and pediatricians in the greater Toronto area.20 This second arm compared the knowledge and use of SRC recommendations by SEMPs and EDPs to assess the success of SRC management KT efforts throughout Canada. Specifically, we wanted to determine whether KT efforts have allowed Canadian SEMPs and EDPs to give consistent SRC management advice.
METHODS
A 19-question, multiple-choice survey was created using a modified Dillman approach.21 The survey was sent to 10 methodologists and 10 typical participants for content validation. An iterative process was used to ensure question relevance and clarity. Ethics approval was obtained (both before and after validation) from the research ethics board at Toronto East General Hospital in Ontario. Pilot testing was done with family medicine residents at the teaching units of 2 Toronto-area hospitals.
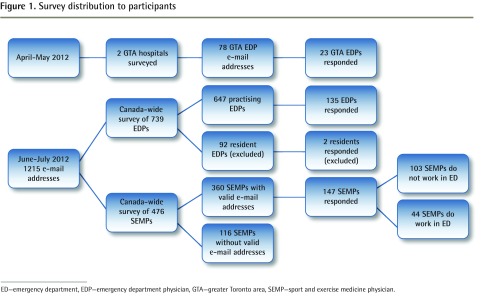
Figure 1 shows a flow diagram of survey distribution to participants. The survey was accessed via e-mail between May and July 2012 by SEMPs who had passed the diploma examination of the Canadian Academy of Sport and Exercise Medicine and EDPs in clinical practice on the Canadian Association of Emergency Physicians (CAEP) e-mail list. This EDP group was solicited through 1 e-mail blast directly from CAEP. In addition, EDPs on staff at 2 community teaching hospitals in the greater Toronto area were surveyed. The chiefs of each hospital department forwarded a link via e-mail to their department members. Physicians were excluded if they had invalid e-mail addresses or if they were residents. This latter criterion excluded 13% of the physicians on the CAEP e-mail list. The principal investigator (J.D.C.) sent an e-mail once per week for 3 sequential weeks to the SEMPs. Anonymity was retained in all follow-up e-mails.
Figure 1.
Survey distribution to participants
ED—emergency department, EDP—emergency department physician, GTA—greater Toronto area, SEMP—sport and exercise medicine physician.
One subset of physicians could have fit into either group. We decided that physicians who practise both sport medicine and emergency medicine would have increased opportunities to learn about SRC management. Thus, we included these physicians in the SEMP group rather than the EDP group.
All survey answers were collected anonymously, and data were analyzed using SPSS. Frequencies and percentages were calculated along with cross-tabulations by specialty, and χ2 tests were done to determine whether there were any statistically significant differences between groups.
RESULTS
The survey was sent to 1293 physicians. Of the 1085 eligible physicians, 360 (33%) held a Canadian Academy of Sport and Exercise Medicine diploma and 725 did not. There was a response rate of 28%, with 305 physicians responding. The SEMP and EDP response rates were 147 of 360 (41%) and 158 of 725 (22%), respectively. The survey elicited information on the usefulness of various SRC information sources in the past 5 years. Table 2 displays, in frequencies, how each group viewed the effectiveness of selected sources. More than 86% of EDPs found their SRC-related continuing medical education (CME) to be very or fairly useful. Respondents were asked to rate the usefulness of the 2008 Zurich statement on SRC. Overall, 41% of EDPs were unaware of any consensus statements on concussion in sport (Table 3).3,8
Table 2.
Usefulness of SRC information sources according to each physician group: Of the respondents, 158 were EDPs and 147 were SEMPs.
| SOURCE | USEFULNESS, N (%) | ||||
|---|---|---|---|---|---|
|
| |||||
| VERY USEFUL | FAIRLY USEFUL | NOT VERY USEFUL | NOT AT ALL USEFUL | NOT APPLICABLE, BLANK, OR OTHER | |
| Emergency medicine journal articles | |||||
| • EDPs | 53 (34) | 87 (55) | 9 (6) | 3 (2) | 6 (4) |
| • SEMPs | 8 (5) | 23 (16) | 24 (16) | 1 (1) | 91 (62) |
| Sport medicine journal articles | |||||
| • EDPs | 8 (5) | 18 (11) | 14 (9) | 2 (1) | 116 (73) |
| • SEMPs | 100 (68) | 39 (26) | 2 (1) | 0 (0) | 6 (4) |
| Emergency medicine CME conference presentations | |||||
| • EDPs | 51 (32) | 85 (54) | 9 (6) | 2 (1) | 11 (7) |
| • SEMPs | 11 (7) | 22 (15) | 13 (9) | 5 (3) | 96 (65) |
| Sport medicine CME conference presentations | |||||
| • EDPs | 5 (3) | 9 (6) | 7 (4) | 1 (1) | 136 (86) |
| • SEMPs | 94 (64) | 34 (23) | 2 (1) | 1 (1) | 16 (11) |
| ThinkFirst Canada website | |||||
| • EDPs | 29 (18) | 14 (9) | 4 (3) | 1 (1) | 110 (70) |
| • SEMPs | 41 (28) | 42 (29) | 9 (6) | 3 (2) | 52 (35) |
CME—continuing medical education, EDP—emergency department physician, SEMP—sport and exercise medicine physician, SRC—sport-related concussion.
Table 3.
Usefulness of the Fourth International Conference on Concussion in Sport (Zurich 2008) statement: Of the respondents, 150 were EDPs and 145 were SEMPs.
| RESPONDENT GROUP | USEFULNESS, N (%) | KNOW OF ONLY 20043 OR 20018 VERSION, N (%) | DO NOT KNOW ANY VERSION, N (%) | P VALUE | |
|---|---|---|---|---|---|
|
| |||||
| EXTREMELY OR VERY USEFUL | SOMEWHAT, OCCASIONALLY, OR RARELY USEFUL | ||||
| EDPs | 35 (23) | 34 (23) | 20 (13) | 61 (41) | < .0001* |
| SEMPs | 106 (73) | 33 (23) | 2 (1) | 4 (3) | |
EDP—emergency department physician, SEMP—sport and exercise medicine physician.
Fisher exact test.
The survey assessed use of tools in diagnosing SRC. In total, 74% of SEMPs and 12% of EDPs said they “usually or always” use the Sport Concussion Assessment Tool (SCAT), version 2 (P < .0001), while 88% of EDPs never use the SCAT2. Physicians were asked how they advise patients to use various treatment strategies for SRC. Sport and exercise medicine physicians are far less likely to advise taking nonnarcotic analgesics and nonsteroidal anti-inflammatory drugs than EDPs are (Table 4) (P < .0001). Sport and exercise medicine physicians are significantly more likely to recommend cognitive rest than EDPs are (P = .0002), and 77% of SEMPs usually advise time off of work or school after an SRC, while 75% of EDPs do likewise (Table 5).
Table 4.
Frequency of prescribing nonnarcotic analgesics and NSAIDS: N = 294.
| MEDICATION | SOMETIMES, RARELY, OR NEVER, N (%) | USUALLY OR ALWAYS, N (%) | P VALUE |
|---|---|---|---|
| Nonnarcotic analgesics | < .0001* | ||
| • EDPs | 44 (29) | 106 (71) | |
| • SEMPs | 101 (70) | 43 (30) | |
| NSAIDs | < .0001* | ||
| • EDPs | 53 (35) | 97 (65) | |
| • SEMPs | 118 (82) | 26 (18) |
EDP—emergency department physician, NSAID—nonsteroidal anti-inflammatory drug, SEMP—sport and exercise medicine physician.
χ2 test.
Table 5.
Frequency of advising cognitive rest, physical rest, and time off of school or work
| ADVICE | SOMETIMES, RARELY, OR NEVER, N (%) | USUALLY OR ALWAYS, N (%) | P VALUE |
|---|---|---|---|
| Cognitive rest (N = 293) | .0002* | ||
| • EDPs | 30 (20) | 120 (80) | |
| • SEMPs | 8 (6) | 135 (94) | |
| Physical rest (N = 293) | .3785† | ||
| • EDPs | 8 (5) | 141 (95) | |
| • SEMPs | 4 (3) | 140 (97) | |
| Time off school or work (N = 294) | .6284* | ||
| • EDPs | 38 (25) | 112 (75) | |
| • SEMPs | 33 (23) | 111 (77) |
EDP—emergency department physician, SEMP—sport and exercise medicine physician.
χ2 test.
Fisher exact test.
No statistically significant difference was found between how SEMPs and EDPs advise patients to achieve cognitive rest following an SRC (P = .067). However, differences did emerge, with twice as many SEMPs as EDPs finding no option appealing (Table 6). Slightly more than one-quarter of both groups agree that decreasing the number of activities that require high concentration is the best advice. Emergency department physicians are more likely than SEMPs are to suggest engaging in regular activities, only stopping if they aggravate symptoms (17% and 9%, respectively) .
Table 6.
Favoured choice of advice given to SRC patients regarding how cognitive rest can best be achieved
| CHOICE | EDP, N (%) | SEMP, N (%) |
|---|---|---|
| Decrease the number of activities that require lots of concentration and take breaks between such activities. Breaks can slowly decrease as symptoms slowly decrease | 39 (26) | 40 (28) |
| Engage in regular everyday activities, but if they aggravate symptoms refrain from participation in these activities | 25 (17) | 13 (9) |
| An increase in thinking will lead to an increase in symptoms. An increase in rest will lead to a decrease in recovery time. You should rest as much as possible until your symptoms resolve | 34 (23) | 30 (21) |
| Engage in total rest from all activities, in a room with very little light, noise, or distractions. If you do this for a short amount of time, you will feel much better | 27 (18) | 26 (18) |
| “Go to jail” in your own bedroom with only bathroom and food breaks for 2 full days. Turn off all electronics and music and avoid watching television, reading, or having conversations | 8 (5) | 4 (3) |
| None of the above appeal to me | 15 (10) | 30 (21) |
EDP—emergency department physician, SEMP—sport and exercise medicine physician, SRC—sport-related concussion.
DISCUSSION
We have determined that KT efforts have been only somewhat successful in allowing SEMPs and EDPs to give consistent SRC management advice. It must be emphasized that most EDPs and SEMPs consistently advise cognitive rest after an SRC. Advice regarding time off school or work is less consistent (approximately three-quarters of each group) than for cognitive rest after SRC. However, this is not surprising, as return-to-learn concepts were only widely introduced with the fourth CISG consensus in 2012.2 Yet, beyond these simple SRC management strategies, consistent advice appears to be lacking. This is not isolated to just one area of the SRC clinical scenario. Indeed, SRC information use, assessment, diagnosis, and management advice given all appear inconsistent among these Canadian physician groups. This survey was conducted more than 3 years after the 2008 CISG consensus statement was published simultaneously in 5 journals worldwide.4 While several consensus statements have been published and websites now exist with high-quality, up-to-date information, many of our physicians surveyed in 2012 were simply not aware of where to access high-quality SRC management information. Many EDPs had no knowledge of any published SRC consensus statements, and many doctors remain either unaware of the ThinkFirst website6 or do not find it useful in clinical practice. Now, in 2016, there is no tangible indication that this situation has improved.
There appear to be differences in the assessment and diagnosis of SRC among SEMPs and EDPs. Patients, their family members, and their family physicians assume that emergency physicians give comprehensive SRC management advice. However, in the context of an emergency department, time constraints and traditional focus on the exclusion of more severe traumatic brain injury might constitute barriers to the implementation of more comprehensive concussion advice practices.22 The SCAT2 tool was rarely used in the emergency department setting, which might be attributed to the time constraints on EDPs, but might also reflect inability to use and interpret the results.22 We assume that the more current SCAT3 and Child SCAT3 will have similar usefulness, although this study did not evaluate these newer tools. Another possibility is that the SCAT3 might be perceived as more appropriately designed for field evaluation or follow-up visits for return-to-play decisions, contexts that are more typical of SEMP practices. Knowledge transfer efforts should include educating EDPs on the diagnostic value of tools such as the SCAT3. The reason for the lack of use of the SCAT2 in the emergency department should be further investigated to better understand how KT efforts might be adapted to better meet the needs of that environment and result in more comprehensive and consistent concussion advice.
Rest is the key first step in acute SRC management. The quality and quantity of rest required to optimally reduce SRC symptoms has been debated at the most recent CISG conference.2 In this study, most EDPs and SEMPs recommended cognitive and physical rest, but variation in the perception of how cognitive rest should be described to patients was documented. The varied responses to the questions regarding what a physician should optimally recommend suggest that there is limited consistency regarding how the “optimal rest” messages are conveyed to SRC patients. There was uniform distribution for each option, with none emerging as a clear favourite for either group. This might reflect the fact that concussion consensus publications have not been specific on this issue.2 As graduated steps for return to learn23,24 are being developed to complete the well-established gradual steps for return to play,2 KT efforts need to focus on ensuring that proper cognitive and physical rest strategies are being developed and successfully implemented in the different environments that characterize our health care system. Ultimately, improved implementation of consistent and evidence-based advice can be expected to decrease the number of patients suffering from extended SRC symptoms.
Limitations
A limitation of this study was its focus upon the CISG’s and ThinkFirst’s efforts without directly referencing other guidelines or KT organizations in our survey. There was a large group of potential SEMP participants who could not be contacted, as we did not have valid e-mail addresses for them. Further, the group of EDPs who responded differed from those who stated to CAEP that they would welcome surveys. In addition, with almost double the response rate for SEMPs compared with EDPs, this raises further questions regarding whether the EDP responses are adequately reflected, rendering these data difficult to generalize. Finally, the data collected were not specific regarding which CME courses physicians had attended. This does not adequately address how good EDP CME is at providing SRC management information.
Conclusion
Large knowledge gaps and inconsistencies in the implementation of the recommendations outlined in the CISG 2008 international consensus statement have been identified. Recommendations for SRC patients given by SEMPs and EDPs lack consistency. Each tool developed by the CISG has generally been highly regarded by the sport medicine community, yet this has not translated into consistent use in a variety of clinical settings. The reasons might be multifactorial, including the perceived barrier of the time required to administer the tools. As SRC management continually evolves, efforts to design and critically evaluate KT strategies will be important to implement better practices by all categories of clinicians involved with SRC management.
Acknowledgments
We thank the 20 people who participated in the validation of our survey.
EDITOR’S KEY POINTS
The Sport Concussion Assessment Tools developed by the Concussion in Sport Group have generally been highly regarded by the sport medicine community, yet this has not translated into their consistent use in a variety of clinical settings. The reasons might be multifactorial, including the perceived barrier of the time required to administer the tools.
Beyond cognitive rest, there is a lack of consistent advice given to patients with sport-related concussions.
There are large knowledge gaps and inconsistencies in the implementation of the recommendations outlined in the Concussion in Sport Group international consensus statements. Recommendations for patients with sport-related concussions given by sport and exercise medicine physicians and emergency department physicians lack consistency.
Footnotes
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de juin 2016 à la page e346.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Provvidenza CF, Johnston KM. Knowledge transfer principles as applied to sport concussion education. Br J Sports Med. 2009;43(Suppl 1):i68–75. doi: 10.1136/bjsm.2009.058180. [DOI] [PubMed] [Google Scholar]
- 2.McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorák J, Echemendia RJ, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250–8. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 3.McCrory P, Johnston K, Meeuwisse W, Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, et al. Consensus statement on concussion in sport—the Third International Conference on Concussion in Sport held in Zurich, November 2008. Phys Sportsmed. 2009;37(2):141–59. doi: 10.3810/psm.2009.06.1721. [DOI] [PubMed] [Google Scholar]
- 5.Carson J, Tator C, Johnston K, Kissick J, Purcell L, Hunt B, et al. New guidelines for concussion management. Based on the second International Conference on Concussion in Sport. Can Fam Physician. 2006;52:756–7. [PubMed] [Google Scholar]
- 6.Parachute Canada [website] ThinkFirst Canada is now part of Parachute. Toronto, ON: Parachute; Available from: www.parachutecanada.org/thinkfirstcanada. Accessed 2015 Feb 9. [Google Scholar]
- 7.Purcell L, Canadian Paediatric Society, Healthy Active Living and Sports Medicine Committee Identification and management of children with sport-related concussion. Paediatr Child Health. 2006;11(7):420–8. [Google Scholar]
- 8.Aubry M, Cantu R, Dvorak J, Graf-Baumann T, Johnston K, Kelly J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001. Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Concussion Awareness Training Tool [website] Vancouver, BC: British Columbia Injury Research and Prevention Unit; 2014. Available from: www.cattonline.com. Accessed 2015 Feb 9. [Google Scholar]
- 10.Concussions Ontario [website] Toronto, ON: Ontario Neurotrauma Foundation; 2015. Available from: www.concussionsontario.org. Accessed 2015 Feb 9. [Google Scholar]
- 11.Concussions Ontario [website] Guidelines for pediatric concussion. Toronto, ON: Ontario Neurotrauma Foundation; 2014. Available from: www.concussionsontario.org/guidelines-for-pediatric-concussion. Accessed 2015 Feb 9. [Google Scholar]
- 12.Purcell LK, Canadian Paediatric Society, Healthy Active Living and Sports Medicine Committee Evaluation and management of children and adolescents with sports-related concussion. Paediatr Child Health. 2012;17(1):31–4. doi: 10.1093/pch/17.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halbert RJ, Isonaka S. International Primary Care Respiratory Group (IPCRG) guidelines: integrating diagnostic guidelines for managing chronic respiratory diseases in primary care. Prim Care Respir J. 2006;15(1):13–9. doi: 10.1016/j.pcrj.2005.12.001. Epub 2006 Jan 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kendall E, Sunderland N, Muenchberger H, Armstrong K. When guidelines need guidance: considerations and strategies for improving the adoption of chronic disease evidence by general practitioners. J Eval Clin Pract. 2009;15(6):1082–90. doi: 10.1111/j.1365-2753.2009.01147.x. [DOI] [PubMed] [Google Scholar]
- 15.Majumdar SR, McAlister FA, Furberg CD. From knowledge to practice in chronic cardiovascular disease: a long and winding road. J Am Coll Cardiol. 2004;43(10):1738–42. doi: 10.1016/j.jacc.2003.12.043. [DOI] [PubMed] [Google Scholar]
- 16.Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997;157(4):408–16. [PMC free article] [PubMed] [Google Scholar]
- 17.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6):iii–iv. 1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 18.Lovell MR, Fazio V. Concussion management in the child and adolescent athlete. Curr Sports Med Rep. 2008;7(1):12–5. doi: 10.1097/01.CSMR.0000308671.45558.e2. [DOI] [PubMed] [Google Scholar]
- 19.Carson JD, Lawrence DW, Kraft SA, Garel A, Snow CL, Chatterjee A, et al. Premature return to play and return to learn after a sport-related concussion. Physician’s chart review. Can Fam Physician. 2014;60:e310–5. Available from: www.cfp.ca/content/60/6/e310.full.pdf+html. Accessed 2016 Apr 20. [PMC free article] [PubMed] [Google Scholar]
- 20.Stoller J, Carson JD, Garel A, Libfeld P, Snow CL, Law M, et al. Do family physicians, emergency department physicians, and pediatricians give consistent sport-related concussion management advice? Can Fam Physician. 2014;60:548–52. [PMC free article] [PubMed] [Google Scholar]
- 21.Dillman DA, Smyth JD, Christian LM. Internet, mail, and mixed-mode surveys. The tailored design method. 3rd ed. Hoboken, NJ: John Wiley and Sons; 2009. [Google Scholar]
- 22.Carson JD, Rendely A, Lebrun CM, Warden J, Arcand A. Family physicians can champion sport-related concussion management. It’s about time. Can Fam Physician. 2014;60:505–7. (Eng), 515–7 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 23.Nationwide Children’s Hospital [website] An educator’s guide to concussions in the classroom. 2nd ed. Columbus, OH: Nationwide Children’s Hospital; Available from: www.nationwidechildrens.org/concussions-in-the-classroom. Accessed 2015 Feb 9. [Google Scholar]
- 24.Sady MD, Vaughan CG, Gioia GA. School and the concussed youth: recommendations for concussion education and management. Phys Med Rehabil Clin N Am. 2011;22(4):701–19. ix. doi: 10.1016/j.pmr.2011.08.008. Epub 2011 Sep 25. [DOI] [PMC free article] [PubMed] [Google Scholar]