Abstract
Objectives
Compare expenditures of fall-related injuries (FRIs) using several methods to identify FRIs in administrative claims data.
Research Design
Using 2007-2009 Medicare claims and 2008 Health and Retirement Survey data, FRIs were identified using external-cause-of-injury (e-codes 880/881/882/884/885/888) only, e-codes plus a broad set of primary diagnosis codes, and a newer approach using e-codes and diagnostic and procedural codes. Linear regression models adjusted for sociodemographic, health, and geographic characteristics were used to estimate per-FRI, service component, patient cost share, expenditures by type of initial FRI treatment (inpatient, ED only, outpatient) and total annual FRI-related Medicare expenditures.
Subjects
The analysis included 5,497 community-dwelling adults ≥65 (228 FRI, 5,269 non-FRI individuals) with continuous Medicare coverage and alive during the 24-month study.
Results
The 3 FRI identification methods produced differing distributions of index FRI type and varying estimated expenditures: $12,171 (95% CI: $4,662-$19,680), $5,648 (95% CI: $3,819-$7,476), and $9,388 (95% CI: $5,969-$12,808). In all models, most spending occurred in hospital, outpatient, and SNF settings, but greater proportions of SNF and outpatient spending were observed with commonly used FRI identification methods. Patient cost-sharing was estimated at $691 to $1,900 across the three methods. Inpatient-treated index FRIs were more expensive than ED and outpatient-treated FRIs across all methods, but were substantially higher when identifying FRI using only e-codes. Estimated total FRI-related Medicare expenditures were highly variable across methods.
Conclusion
FRIs are costly, with implications for Medicare and its beneficiaries. However, expenditure estimates vary considerably based on the method used to identify FRIs.
Keywords: Fall injury, Economics, Medicare
INTRODUCTION
Fall-related injuries (FRIs) are the most likely cause of injury-related emergency department (ED) visits and hospitalization among seniors, with over 2 million annual FRI-related ED visits.1 As many as 30% of ED visits result in hospitalization,1 with 630,000 hospitalizations for non-fatal falls in 2011.2 A 2010 systematic review assessing the burden of falls among older adults observed considerable differences in costs per individual who falls (“faller”) ($2,000 to $26,000), per fall ($1,059 to $10,913) and for fall-related hospitalization ($5,654 to $42,840).3 Costs per faller in U.S. studies examining older adults from all settings (including institutionalized adults) ranged from $3,766 to $25,955 while costs per faller involving only community-dwelling older adults ranged from $2,310 to $24,140.3
Prior studies vary in terms of the population examined, the type of information used to identify a fall, cost data used, and study design/model specification (see Appendix A, Table A1). Of particular importance is the approach to identifying FRIs. Most FRI costing studies have used administrative data, involving ICD-9 diagnosis codes and external cause-of-injury codes (“e-codes”). Studies have also varied in terms of study design, with studies making use of “cohort,” “case-crossover,” and “case control” designs,4-6 while employing differing model specifications. However, the effect of different approaches on cost estimates is unknown.
Table 1.
Three Methods to Identify Fall-related Injuries (FRI) in Medicare Claims Data: Codes and Claims Data Used, Sample Size, and Sensitivity and Specificity of Methods
| Codes Used | Claims Used | Sample Size |
Sensitivity and Specificity | |
|---|---|---|---|---|
| 1. E-code Only (“ECO”) Method |
E-codes 880, 881, 882, 884, 885, and 888. | Inpatient (IP), outpatient (OP), skilled nursing facility (SNF) |
55 FRI, 5,463 non-FRI (1% FRI) |
Insensitive (does not adequately identify as fallers those respondents who experienced an FRI) but highly specific (correctly identifies as non- fallers those individuals who did not fall). |
| 2. E-code and Broad Diagnostic Code (“ECDC”) Method |
E-codes 880, 881, 882, 884, 885, and 888; ICD- 9 diagnostic codes 800-848, 850-854, and 920- 924. |
IP, OP, Carrier File (PB), SNF |
705 FRI, 4,774 non-FRI (13% FRI) |
Highly sensitive but non-specific, as this method broadly ascribes falls to individuals. |
| 3. Adapted UCLA/RAND (“AUR”) Method |
Inpatient e-codes 880, 881, 882, 884, 885, and 888; primary or secondary inpatient ICD-9 diagnoses of hip fracture (820), other fracture a (807-810, 812-817, 821-824), head injury (800- 804, 850-854), or joint dislocation (831-833, 836); (a) fracture repairs indicated by CPT codesb for hip fractures and other fractures, face injuries, and joint dislocations and (b) fracture repairs that occurred on same day as outpatient ICD-9 diagnosis codes identified as FRIs; (a) multiple outpatient ICD-9 diagnosis codes or an imaging CPT code plus an outpatient ICD-9 diagnosis code that occurred on separate days but <10 days apart or (b) one outpatient e-code; e-codes 806, 812-814, 867, 878, 879, 915, 916, 930-936, 942-949, and 980 resulted in non- qualification unless an FRI-identifying e-code is also listed. |
IP, OP, Carrier File (PB), SNF |
228 FRI, 5,269 non-FRI (4% FRI) |
Potentially more sensitive than the e- code only method (Method #1) and as sensitive as the e-code and broad diagnostic code method (Method #2). Less specific than the first method and potentially more specific than the second method. |
Other fractures include fractures of the pelvis, neck/trunk, clavicle, humerus, radius and ulna, carpal, hand, femur/tibia, fibula, patella, or ankle).
Please contact authors for additional information regarding CPT codes used to identify repair and imaging procedures.
Methods Used to Identify FRIs
FRIs are most commonly identified using claims data e-codes, which assess the place and mechanism of an injury. However, e-codes are commonly missing in claims data.7-9 Authors of one study found that only 7% of hip or femur fractures among older adults had e-codes for their injuries.10 The accuracy of e-codes (the percentage of e-codes that are in agreement when abstracting patient records) was 66% and 73% in two studies.11-13 There is also an absence of quality assurance activities aimed at monitoring the completeness and validity of e-codes.14 Missingness in records could be due to certain states not having a statewide database for collecting injury information (a number of states are not mandated to collect e-code information) and because, among states collecting such information, there are differences in the number of fields available for inputting e-codes in the databases; further, some states are unable to identify a first hospital visit for patients hospitalized more than one time for an injury.7
Accordingly, this method is likely insensitive (i.e., does not adequately identify as fallers those respondents who experienced an FRI) but highly specific (i.e., correctly identifies as non-fallers those individuals who did not fall). Moreover, the method likely identifies fallers as those individuals experiencing the most serious (and thus most costly) falls, resulting in higher cost estimates but lower FRI prevalence than other methods.
Another approach uses e-codes plus ICD-9 diagnosis codes for fractures, dislocations/sprains and strains, intracranial injuries, and contusions.4,5,10 This method is highly sensitive, but non-specific, as it broadly ascribes falls to individuals. Thus, the average cost of a fall observed is likely to be low since individuals are considered fallers even if they had treatment for an injury due to an incident less serious than a fall. But, the prevalence of fallers identified should be higher compared to that obtained using only e-codes.
A more recently introduced approach using e-codes, inpatient ICD-9 diagnostic, and outpatient procedural codes to assess whether claims data reflected a serious fall injury.15, 51 Cases can qualify according to receipt of treatment for diagnoses in inpatient settings, including the hospital and skilled nursing facilities (SNFs), or by receipt of procedures (within certain time periods following initial treatment) performed in outpatient settings. This method may be more sensitive than the first and is potentially as sensitive as the second method; it is also potentially more specific than the second method. Resultant cost estimates may be lower than with the first and higher than with the second method; also, the prevalence of fallers using this method may be higher and lower compared to the first and second methods, respectively.
The current study uses these three FRI identification methods to estimate annual per-FRI episode, service component, patient cost-share, and total Medicare FRI-related expenditures. The study objective is to inform whether the widespread use of e-codes in falls surveillance and cost-of-falls analyses provides similar estimates to other FRI identification methods.
METHODS
Data and Study Population
This study uses the Area Health Resource File (AHRF), the 2008 Medicare Impact File, and the 2008 Health and Retirement Study (HRS) (with interviews conducted from 2/2008-2/2009) data linked to 2007-2009 Medicare claims data—which includes Beneficiary Summary, Carrier, Denominator, Inpatient, Outpatient, Durable Medical Equipment (DME), Home Health Agency (HHA), SNF, Hospice, and MedPAR Standard Analytic Files. Participants were included if they were ≥65 years old, not living in a nursing home at the time of interview, alive during the full follow-up period (which is 12 months from the date of the index admission date, or the first qualifying FRI, as discussed below), and had continuous Parts A/B coverage.
Methods for Identifying FRIs
Three separate methods are used to identify FRIs in the claims data. Method 1 (the e-code only, or “ECO” method) is the one commonly used to identify FRIs in claims data and typically involves the ICD-9 e-codes 880, 881, 882, 884, 885, or 888.3,6,10,16-20 Method 2 (e-code and diagnostic code, or “ECDC” method) uses the above e-codes plus a broad set of primary inpatient diagnostic codes indicating fractures, dislocations, sprains, strains, head injuries, and contusions (ICD-9 diagnostic codes 800-848, 850-854, and 920-924).4,5,10 Method 3 (the adapted UCLA/RAND, or “AUR” method) employs an adaptation of the algorithm that identified ICD-9 inpatient primary diagnosis codes (for hip fractures, other nonvertebral fractures, head trauma, joint dislocations, and injuries identified by the above e-codes) as well as outpatient Current Procedural Terminology (CPT) codes (for imaging and repair procedures) as fall injuries.15, 51 To identify index FRIs, each of the three methods uses e-codes from inpatient, outpatient, and SNF claims data; the ECDC method and AUR methods additionally use ICD-9 codes from the Carrier file while the AUR method further uses CPT codes from outpatient settings. See Table 1 for additional details, including analytic sample sizes and size of FRI cohort using each identification method; note that differing total sample sizes resulted from use of the “washout” period—or 12-month period of time without an FRI required for inclusion in either of the cohorts—that excluded different numbers of respondents using each FRI identification method.
Study Design
This study uses a “case-crossover” design to isolate per-FRI episode expenditures (hereafter referred to as “per-FRI expenditures”) using a pre-post analysis with a comparison group. An FRI and non-FRI cohort were created using the three FRI identification methods described above and then pooled for analysis. The FRI cohort included those with a first FRI in 2008 but no FRIs during the 12 months prior to a given individual’s specific date of index admission (a first qualifying FRI) and the non-FRI cohort included those with no FRIs in 2007, 2008, or the first half of 2009. FRI cohort individuals received an index date—the date of their first qualifying FRI in 2008. Non-FRI cohort individuals received an index date that was the midpoint of the year during which FRI cohort index admissions were observed, 7/1/2008.
Medical expenditures for both cohorts were measured during the year prior to (“pre-index”) and following the index date (“post-index”). Expenditures were defined as total, direct, medical expenditures from the perspective of the Medicare program and Medicare beneficiary, excluding Medicaid, private supplemental insurance policies and other third-party payers. Medical expenditures include the amount Medicare paid to the institutional provider, physician, or supplier for the services covered by the claim record plus beneficiary out-of-pocket (OOP) expenditures.
The main expenditure outcome is expenditures in the post period minus expenditures in the pre period (“expenditures change score”) and the predictor of interest is an indicator for whether the observation is from the FRI vs. non-FRI cohort. The estimated marginal effect of this indicator therefore reflects a “difference-in-differences” estimate, i.e., the differential change in expenditures experienced over time between individuals who did and did not have an FRI. Because this methodology (which is akin to controlling for person-level fixed effects) controls for measurable and unmeasurable confounders that do not vary within an individual over time, the difference in change scores can be interpreted as the incremental expenditures associated with an FRI during the year after falling.
Descriptive statistics are provided. An ordinary least squares specification was chosen given that change scores were normally distributed:
where, for respondent i, ΔExpendi is the expenditure change from the pre- to post-baseline period, FRIi is the FRI cohort, Healthi are health variables and Areai are contextual variables, discussed below. Using each FRI identification method, expenditures were estimated (in separate models) by service category (hospital, outpatient/carrier, SNF, HH, DME, hospice) and for patient OOP expenditures. Expenditures were also estimated by type of treatment initially received—inpatient (hospital/SNF including admission from ED ≤10 days of discharge), ED-only, or outpatient (in a model identical to that shown above but that included dummy variables for each treatment type rather than a dichotomous variable indicating whether an FRI occurred).6 Total Medicare expenditures were computed using estimated per-FRI expenditures, fall prevalence, and the number of older Medicare beneficiaries in 2008 (34.3 million).21
Risk Adjustment Variables
The study controlled for individual and contextual factors that are associated with falls in the falls literature and health services’ price and/or quantity and thus might confound the falls-cost relationship.22 To control for potential confounders of the falls-expenditure relationship, individual and contextual factors that have been associated with falls and/or health care expenditures were included. These were individuals’ age at the index date,22,23 self-reported gender,22,23 race/ethnicity (White, Black, Hispanic, Asian/Pacific Islander, Other),23,24 educational level (less than high school, high school, some college, college or beyond), and total household income and wealth (the latter three of which may affect the home environment, which has been associated with fall risk).25 Self-reported health-related characteristics were included to account for differential demand for care: number of chronic health conditions23,26-28 (an index scored from 0-5 for osteoarthritis, stroke, heart disease, high blood pressure, and diabetes), functional limitations (an index scored from 0-12 for reported difficulties with activities such as walking several blocks),22,23,28,29 and self-rated eyesight (1-6 where 1=legally blind and 6=excellent)23,28,30 and hearing (1-5, where 1= poor and 5 = excellent);30,31-33 low cognitive status22,23,28,30 was measured using a score of ≤6 on the Telephone Interview of Cognitive Status (range of 0-15);34 and disability indicating that a respondent reported applying for SSI or SSDI (reflecting diminished physical status, which is a risk factor for falls).22,23 The model also included self-reported use of psychiatric medications23,27,30 and, to account for the likelihood of accessing services, supplemental Medicaid coverage. To measure the area-level availability and price of medical care, a county’s number of non-federal physicians/100,000 older adults and Medicare wage index were included.
RESULTS
Unadjusted Results
Characteristics of study respondents in the FRI cohort were generally similar across methods (See Table 2). Pre- and post-index expenditures for the non-FRI cohort were similar across methods (~$7,500 and ~$9,500, respectively; Table 3). However, for the FRI cohort, there was significant variation across methods in pre-index expenditures (from $9,461 to $14,040) and post-index expenditures (from $16,899 to $28,883). Accordingly, expenditure changes also ranged broadly for the FRI cohort.
Table 2.
Comparison of Fall-related Injury (FRI) Identification Methods for Unadjusted Descriptive Statistics for Older Medicare Beneficiaries, 2007-9
| 1. E-code Only (“ECO”) (n = 5,518) |
2. E-code and Broad Diagnostic Code (“ECDC”) (n = 5,479) |
3. Adapted UCLA/ RAND (“AUR”) (n = 5,497) |
||||
|---|---|---|---|---|---|---|
|
| ||||||
| FRI Cohort |
Non-FRI Cohort |
FRI Cohort |
Non-FRI Cohort |
FRI Cohort |
Non-FRI Cohort |
|
| Characteristics of Individuals in FRI Cohort | ||||||
| Age | 81 (8) | 81 (8) | 77 (7) | 76 (7) | 78 (7) | 76 (7) |
| Male (%) | 36 | 42 | 33 | 43 | 32 | 42 |
| Race/ethnicity (%) | ||||||
| White | 85 | 82 | 85 | 82 | 86 | 82 |
| African-American | 11 | 11 | 8 | 11 | 7 | 11 |
| Hispanic | 0 | 4 | 5 | 4 | 3 | 4 |
| Other | 4 | 3 | 3 | 3 | 4 | 3 |
| Education (%) | ||||||
| < high school | 22 | 22 | 22 | 22 | 23 | 22 |
| High school | 37 | 37 | 39 | 37 | 36 | 37 |
| Some college | 13 | 20 | 18 | 20 | 15 | 20 |
| College | 22 | 21 | 21 | 21 | 26 | 20 |
| Income ($1,000) | 44 (45) | 55 (110) | 61 (211) | 54 (86) | 54 (73) | 55 (111) |
| Wealth ($1,000) | 499 (1,000) | 562 (1,307) | 563 (1,099) | 562 (1,327) | 635 (1,200) | 559 (1,311) |
| Eyesight (1-6) | 3 (1) | 3 (1) | 3 (1) | 3 (1) | 3 (1) | 3 (1) |
| Hearing (1-5) | 3 (1) | 3 (1) | 3 (1) | 3 (1) | 3 (1) | 3 (1) |
| Cognitive impairment (%) | 5 | 2 | 3 | 2 | 3 | 2 |
| No. of functional limitations (0-12) | 7 (3) | 4 (3) | 5 (3) | 4 (3) | 6 (3) | 4 (3) |
| No. of chronic conditions (0-6) | 3 (1) | 2 (1) | 2 (1) | 2 (1) | 2 (1) | 2 (1) |
| Psychiatric medication (%) | 15 | 9 | 12 | 9 | 13 | 9 |
| Disability (%) | 22 | 12 | 12 | 12 | 13 | 12 |
| Medicaid (%) | 11 | 9 | 10 | 9 | 8 | 9 |
| Area wage index | 0.92 (0.16) | 0.96 (0.15) | 0.97 (0.15) | 0.96 (0.14) | 0.96 (0.16) | 0.96 (0.15) |
| Physicians/10,000 older adults | 147 (94) | 188 (141) | 191 (153) | 188 (140) | 181 (133) | 188 (141) |
Table 3.
Comparison of Fall-related Injury (FRI) Identification Methods for Unadjusted Expenditures for Older Medicare Beneficiaries, 2007-9
| Method 1 (n = 5,518) |
Method 2 (n = 5,479) |
Method 3 (n = 5,497) |
|
|---|---|---|---|
|
|
|||
| Index FRI Type | |||
| Inpatient | 12 (22%) | 13 (2%) | 25 (11%) |
| ED Only | 30 (55%) | 80 (11%) | 58 (25%) |
| Outpatient | 13 (24%) | 612 (87%) | 145 (64%) |
|
|
|||
| Expenditures ($) (SD) | |||
| Pre-index | 8,003 (14,893) | 7,650 (14,619) | 7,801 (14,682) |
| FRI cohort | 14,040 (18,827) | 9,461 (16,059) | 11,575 (18,960) |
| Non-FRI cohort | 7,942 (14,838) | 7,383 (14,376) | 7,638 (14,448) |
| Post-index | 10,099 (19,906) | 10,035 (19,479) | 10,081 (19,826) |
| FRI cohort | 28,883 (28,004) | 16,899 (24,008) | 23,151 (25,977) |
| Non-FRI cohort | 9,909 (19,720) | 9,021 (18,506) | 9,515 (19,321) |
| Change Score | 2,096 (20,023) | 2,394 (19,427) | 2,280 (19,880) |
| FRI cohort | 14,843 (28,654) | 7,437 (23,621) | 11,577 (26,329) |
| Non-FRI cohort | 1,967 (19,878) | 1,638 (18,616) | 1,878 (19,457) |
Note: Method 1 involves the use of e-codes (880, 881, 882, 884, 885, or 888) only. Method 2 uses the same e-codes plus primary inpatient diagnostic codes indicating fractures, dislocations, sprains, strains, head injuries, and contusions (ICD-9 diagnostic codes 800-848, 850-854, and 920-924). Method 3 involves FRIs identified using the adapted UCLA/RAND algorithm15 in which FRIs are identified using inpatient (hospital and SNF) ICD-9 primary diagnoses and the same e-codes plus outpatient diagnoses and procedural codes. The change score is the difference between pre- and post-index costs.
Adjusted Results
FRI Expenditure Estimates
While the expenditure estimate confidence intervals overlapped for the three methods, point estimates ranged considerably (Table 4). With the commonly used EOC method, expenditures were $12,171 (95% CI: $4,662-$19,680). The ECDC method (using e-codes and a broad set of diagnostic codes) and AUR (using e-codes, a more limited set of diagnostic codes, and procedural codes) estimated FRI expenditures 54% and 30% less than the ECO method, respectively: expenditures using ECDC were $5,648 (95% CI: $3,819-$7,476) and using AUR were $9,388 (95% CI: $5,969-$12,808) (Table 4).
Table 4.
Adjusted Annual Medicare Expenditures for Older Adults Experiencing a Fall-related Injury (FRI) Using Three Methods to Identify FRIs in Medicare Claims Data, 2007-9
| Method 1 |
Method 2 |
Method 3 |
|
|---|---|---|---|
| β (95% CI) a | β (95% CI) a | β (95% CI) a | |
| Post-baseline Expenditures | 15,797 (8,639-22,954)* | 7,123 (5,346-8,901)* | 12,215 (8,989-15,440)* |
| Pre-baseline Expenditures | 3,626 (−1,037-8,288) | 1,476 (268-2,684)* | 2,826 (469-5,183)* |
| Expenditures Change Score (Total Expenditures) | 12,171 (4,662-19,680)* | 5,648 (3,819-7,476)* | 9,389 (5,969-12,808)* |
| Patient Out-of-pocket Expenditures | |||
| Total | 1,900 (688-3,113)* | 691 (471-911)* | 1,363 (889-1,837)* |
| Deductible | 223 (−51-497) | 94 (35-154)* | 252 (134-371)* |
| Coinsurance | 1,677 (582-2,773)* | 597 (405-789)* | 1,111 (695-1,526)* |
| Expenditures by Initial Treatment Type | |||
| Inpatient | 33,418 (15,734-51,101)* | 22,749 (10,839-34,658)* | 21,441 (11,567-31,281)* |
| ED only | 6,128 (−1,416-13,673) | 5,405 (1,569-9,241)* | 6,142 (1,314-10,970)* |
| Outpatient | 6,549 (−10,243-23,340) | 5,327 (3,328-7,325)* | 8,622 (3,991-13,254)* |
p < 0.05
Note: The expenditure outcome is expenditures in the post period minus expenditures in the pre period (“expenditures change score”) and the predictor of interest is an indicator for whether the observation is from the FRI vs. non-FRI cohort. The estimated marginal effect of this indicator, or the beta coefficient, therefore reflects the differential change in expenditures experienced over time between individuals who did and did not have an FRI. Because this methodology controls for measurable and unmeasurable confounders that do not vary within an individual over time, the difference in change scores can be interpreted as the incremental expenditures associated with an FRI during the year after falling. The models control for baseline sociodemographic, health, and geographic characteristics. Method 1 involves the use of e-codes (880, 881, 882, 884, 885, or 888) only. Method 2 uses the same e-codes plus primary inpatient diagnostic codes indicating fractures, dislocations, sprains, strains, head injuries, and contusions (ICD-9 diagnostic codes 800-848, 850-854, and 920-924). Method 3 involves FRIs identified using the adapted UCLA/RAND algorithm15 in which FRIs are identified using inpatient (hospital and SNF) ICD-9 primary diagnoses and the same e-codes plus outpatient diagnoses and procedural codes. Models were estimated using OLS regression with robust standard errors. The respective analytic sample sizes for models estimated separated using FRI identification Methods 1-3 were 5,518, 5,479, and 5,497. The models do not include individuals who died during the post-index period. Separate models were estimated for each type of cost and for each payment source. A single model was estimated to assess costs associated with the FRI initial treatment type—dummy variables for each type were included (with outpatient only treatment as the reference category) and predicted costs were obtained from model estimates.
CI = confidence interval
b Percentages may not add up to 100% because several of the estimated expenditure components were negative.
Service Components and Out-of-Pocket (OOP) Expenditures
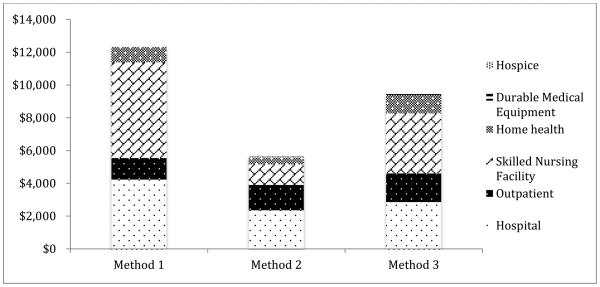
For each method, hospital, outpatient, and SNF expenditures comprised the majority of spending (Figure 1). Hospital expenditures were greatest for ECDC (42% vs. 35% and 31% for ECO and AUR, respectively) while SNF expenditures were greatest for ECO (48% vs. 22% and 39% for ECDC and AUR, respectively). Outpatient expenditures constituted 11%, 27%, and 18% of total estimated per-FRI expenditures for Methods 1-3, respectively (Table 4). OOP expenditures were greatest for ECO ($1,900) and lowest for ECDC ($691). Coinsurance represented the majority of OOP expenditures across all methods (88%, 86%, and 82%, respectively, for Models 1-3).
Figure 1. Adjusted Annual Medicare Expenditures by Service Category for Older Adults Experiencing a Fall-related Injury (FRI) Using Three Methods to Identify FRIs in Medicare Claims Data, 2007-9.
Note: The expenditure outcome is expenditures in the post period minus expenditures in the pre period (“expenditures change score”) and the predictor of interest is an indicator for whether the observation is from the FRI vs. non-FRI cohort. The estimated marginal effect of this indicator, or the beta coefficient, therefore reflects the differential change in expenditures experienced over time between individuals who did and did not have an FRI. Because this methodology controls for measurable and unmeasurable confounders that do not vary within an individual over time, the difference in change scores can be interpreted as the incremental expenditures associated with an FRI during the year after falling. The models control for baseline sociodemographic, health, and geographic characteristics. Method 1 involves the use of e-codes (880, 881, 882, 884, 885, or 888) only. Method 2 uses the same e-codes plus primary inpatient diagnostic codes indicating fractures, dislocations, sprains, strains, head injuries, and contusions (ICD-9 diagnostic codes 800-848, 850-854, and 920-924). Method 3 involves FRIs identified using the adapted UCLA/RAND algorithm15 in which FRIs are identified using inpatient (hospital and SNF) ICD-9 primary diagnoses and the same e-codes plus outpatient diagnoses and procedural codes. Models were estimated using OLS regression with robust standard errors. The respective analytic sample sizes for models estimated separated using FRI identification Methods 1-3 were 5,518, 5,479, and 5,497. The models do not include individuals who died during the post-index period. Separate models were estimated for each payment source. The percentage of total estimated expenditures across the three methods for hospital, outpatient, skilled nursing facility, home health, durable medical equipment, and hospice were: 35%, 11%, 48%, 8%, 0%, 0% (Method 1); 42%, 27%, 22%, 8%, 1%, 0% (Method 2); and 31%, 18%, 39%, 12%, 1%, 0% (Method 3).
Expenditures Associated with Initial Treatment for Index FRI
With respect to treatment for the index admission, inpatient FRI expenditures were lower in the ECDC and AUR methods—$22,749 and $21,424—compared to ECO ($33,418) (Table 4). However, ED-only and outpatient-treated FRIs were similar ($5,000-$6,000 and $5,000-$8,000, respectively) across the methods.
Total FRI-Related Medicare Expenditures
Total Medicare expenditures were highly sensitive to the FRI identification method used. Approximate, total Medicare expenditures were $4 (95% CI: $2-$7), $25 (95% CI: $17-$33), and $13 (95% CI: $9-$18) billion for Methods 1-3, respectively. Even though the per-FRI annual expenditure estimate was lower using AUR compared to ECO, the total Medicare expenditure was much greater due to the higher proportion of beneficiaries assumed to have fallen during the study period. There were more than three times as many beneficiaries in the FRI cohort using AUR compared to ECO (13% vs. 4%).
DISCUSSION
The study’s findings indicate that the method used to identify FRIs in claims data has important implications for annual per-FRI and, in particular, total Medicare expenditure estimates. Several FRI identification approaches were used because existing approaches vary in terms of sensitivity and specificity.15 The broadest approach (ECDC) produced the lowest per-FRI expenditure estimates, while the narrowest approach (EOC) and an adaptation of a method using e-codes, diagnostic, and procedural codes (AUR) produced relatively higher per-FRI expenditure estimates. The total annual Medicare FRI-related expenditures for older adults varied due to the difference in prevalence estimates for FRIs using each of the methods.
The study offers possible explanations for these expenditure discrepancies. First, differences in the distribution of FRIs across methods may affect expenditure estimates. The claims-based FRI identification method using e-codes only identified a relatively high proportion of index FRIs initially treated in the ED (55% compared to 11% and 25% for the ECDC and AUR methods, respectively), relative to inpatient or outpatient/physician care settings. It may be that e-codes for falls are more commonly documented in the ED compared to hospitals. Additionally, the ECO method (which assesses FRIs in outpatient settings with e-codes) may not be as sensitive to outpatient-treated FRIs as the other two methods, which identify FRIs involving outpatient/physician care using diagnosis (and additionally, in the AUR method, CPT procedure) codes. In the outpatient and Carrier files (the latter of which does not contain e-codes), there were 817,455 observations for 2007-2009, 599 of which had e-codes. Comparatively, Methods 1-3 identified 599 (0.07%), 24,374 (3.0%), and 7,404 (0.9%) FRIs, respectively. Compared to the ECO method, most additional FRIs in the adapted AUR method involved outpatient diagnosis codes. Also, the ECDC method identified outpatient expenditures as comprising a proportion of total expenditures nearly double that of the AUR method and triple those of the ECO method—presumably due to that method’s inclusion of sprains and strains that are not considered FRIs in the traditional and AUR methods. In all, the use of e-codes only to identify FRIs is problematic, as noted as well in prior analyses.8,11,13 One report noted the incompleteness of e-coding in most states, with 44% of states that evaluated hospital records also e-coding at least 90% of injury-related hospitalizations. Until injury reporting is improved with more thorough provider reporting of injuries, more complete sharing of injury data by certain states, as well as changes to state regulations regarding e-coding, the use of e-codes only for falls surveillance may continue to pose problems for researchers and policymakers—suggesting the need for alternative approaches such as those provided with ECDC and AUR.
Despite some relative benefits, however, using the ECDC method may also be problematic to an extent. That approach identified a number of minor outpatient injuries as FRIs, but it is questionable whether all such injuries are fall-related; for example, minor sprains treated in outpatient settings may not be uniformly attributable to FRIs. Overall, ECDC’s lack of specificity may overestimate the prevalence of fallers and underestimate expenditures, suggesting that prior studies using this method may have underestimated per-FRI episode expenditures (excepting other methodological choices that could have inflated those studies’ estimates).4,5,10 Also, because it identifies a much greater proportion of individuals with FRIs compared to other methods, it results in total annual FRI-related Medicare expenditure ranges ($17-33 billion) nearly twice those using the AUR method ($9-19 billion) and even greater relative to the EOC method ($2-$7 billion). In future analyses estimating annual expenditures, ECDC estimates might be standardized using other, lower-prevalence population FRI estimates.
The adapted UCLA/RAND method used in this study15, 51 provides an alternative with potential benefits, using an algorithm based in part upon a review of orthopedic literature to assess FRI qualification. This AUR method appears beneficial in identifying additional FRIs not apparent in e-codes while not overly broadly attributing FRIs to care episodes, such as those involving treatment for sprains and strains. The method produces per-FRI episode expenditure estimates that are in the middle of the range of expenditure estimates for hospitalized FRIs among prior studies.3 This suggests that some prior estimates are too high6,16,17,19,35,36 and that prior cost-effectiveness studies using earlier estimates may be similarly affected.37-42
Despite these potential advantages to using the AUR method, there remain issues of note for researchers to consider. For instance, evidence of scaphoid fractures (FRIs in the AUR) being fall-related43 relies on a study in which only six patients of the 158 assessed had a fracture resulting from a fall.44 Also, shoulder dislocations are considered fall-related based upon a study that observed that just 59% of 8,940 dislocations examined were the result of a fall.45 Yet, these dislocations may be due to motor vehicle injury2 rather than falls or may involve exertion by active, healthy older individuals—with different implications for falls prevention when compared to FRIs involving less active older adults. Clearly, no claims-based method of ascribing injury to fall is perfect. Nonetheless, these newer methods—AUR in particular—appear to be improvements over the traditional ECO approach.
The other findings of note are the distribution of expenditures across healthcare settings and incidence of costs for Medicare compared to the beneficiary. Expenditures were primarily associated with hospital, outpatient, and SNF treatment,5 but varied across identification methods. With ECDC, the distribution involved greater relative spending in the hospital versus outpatient and SNF settings; however, expenditures for those initially treated in the hospital were similar for beneficiaries using ECDC and AUR; thus, ECDC captures a greater proportion of less serious injuries than the other two methods. Relative to the traditional ECO method, the newer AUR method seems to also identify a cohort of less serious FRIs, but also to capture relatively costly outpatient injuries not observed using ECO. Also, the relative shares of DME and hospice expenditures were minimal compared to other spending across all methods. In all, AUR appears to present credible estimates of the prevalence of and expenditures (including the distribution across care settings) involving per-FRI episode and total annual FRI costs. This method is recommended for future FRI expenditure analyses.
Finally, patient out-of-pocket costs associated with FRIs were similar across the three methods, averaging 12-15% of total per-FRI episode expenditures. The financial burden of FRIs for older Medicare beneficiaries appears substantial. Roughly $700-$1,900 in annual patient contributions for each FRI episode is noteworthy given the prevalence of falls (including multiple falls) and FRIs among community-dwelling older adults.46-49
Limitations
Several limitations may apply to this analysis. First, because many fallers are admitted to a nursing facility,50 FRI-related expenditures are likely underestimated if a social planner, rather than Medicare, perspective is taken. Second, the findings may not be generalizable to the US older Medicare population, given the smaller sample size of the models and because the distribution of FRI types may not be the same as in the overall older Medicare population. However, similar results were obtained when using individual-level HRS survey weights in a sensitivity analysis. Third, results may be biased due to reverse causality because, given the choice of using 2008 HRS data, some individuals’ self-reported health may reflect a prior FRI. However, estimates were robust to models in which potentially endogenous regressors were controlled, among others (see Appendix B).
Conclusion
In summary, FRIs are costly events, with implications for beneficiaries in terms of out-of-pocket expenditures and the Medicare program. While these estimates may be useful to policymakers assessing the cost-benefit of Medicare falls prevention programs, this study also provides researchers with information about various methodological approaches to assessing FRI prevalence and expenditures. In future work, careful consideration should be given to the FRI identification algorithm; falls surveillance and Medicare expenditure estimates may improve accordingly, with potential implications for the health and safety of older adults.
Supplementary Material
Acknowledgments
Geoffrey J. Hoffman was supported by the NIH/National Center for Advancing Translational Science UCLA CTSI (No. TL1TR000121). Ron D. Hays was supported in part by grants from NCI (1 U2-CCA186878-01), the NIA (P30-AG021684), and the NIMHD (P20-MD000182).
Footnotes
No potential conflicts of interest for the authors exist pertaining to this work.
Contributor Information
Geoffrey J. Hoffman, Department of Systems, Populations and Leadership, University of Michigan School of Nursing 400 N. Ingalls Street, Room 4352, Ann Arbor, MI 48109.
Ron D. Hays, UCLA Division of General Internal Medicine and Health Services Research, University of California Los Angeles.
Martin Shapiro, Division of General Internal Medicine, David Geffen School of Medicine Professor, Department of Health Policy and Management, Fielding School of Public Health, University of California Los Angeles.
Steven P. Wallace, Department of Community Health Sciences, Fielding School of Public Health, University of California Los Angeles.
Susan L. Ettner, Division of General Internal Medicine and Health Services Research, David Geffen School of Medicine at UCLA, Department of Health Policy and Management, Fielding School of Public Health University of California Los Angeles.
References
- 1.Owens PL, Russo CA, Spector W, Mutter R. Healthcare Cost and Utilization (HCUP) Statistical Brief #80: Emergency department visits for injurious falls among the elderly, 2006. Agency for Health Care Policy and Research; Rockville: 2009. [PubMed] [Google Scholar]
- 2.Web-based Injury Statistics Query and Reporting System (WISQARS). Centers for Disease Control and Prevention: National Center for Injury Prevention and Control 2015 http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html Accessed April 3, 2015.
- 3.Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH. Cost of falls in old age: A systematic review. Osteoporos. Int. 2010;21(6):891–902. doi: 10.1007/s00198-009-1100-1. [DOI] [PubMed] [Google Scholar]
- 4.Bohl AA, Fishman PA, Ciol MA, Williams B, Logerfo J, Phelan EA. A longitudinal analysis of total 3-year healthcare costs for older adults who experience a fall requiring medical care. J. Am. Geriatr. Soc. 2010;58(5):853–860. doi: 10.1111/j.1532-5415.2010.02816.x. [DOI] [PubMed] [Google Scholar]
- 5.Bohl AA, Phelan EA, Fishman PA, Harris JR. How are the costs of care for medical falls distributed? The costs of medical falls by component of cost, timing, and injury severity. The Gerontologist. 2012;52(5):664–675. doi: 10.1093/geront/gnr151. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein EA, Chen H, Miller TR, Corso PS, Stevens JA. A comparison of the case-control and case-crossover designs for estimating medical costs of nonfatal fall-related injuries among older Americans. Med. Care. 2005;43(11):1087–1091. doi: 10.1097/01.mlr.0000182513.35595.60. [DOI] [PubMed] [Google Scholar]
- 7.Abellera J, Annest JL, Conn JM. How states are collecting and using cause of injury data: 2004 update to the 1997 report. Council of State and Territorial Epidemiologists;2004; Atlanta, GA: [Google Scholar]
- 8.Annest JL, Fingerhut LA, Gallagher SS, et al. Strategies to improve external cause-of-injury coding in state-based hospital discharge and emergency department data systems: Recommendations of the CDC Workgroup for Improvement of External Cause-of-Injury Coding. Morbidity and Mortality Weekly Report. 2008;57(RR-1):1–15. [PubMed] [Google Scholar]
- 9.Goldman LE, Chu PW, Prothro C, Osmond D, Bindman AB. Accuracy of condition present on admission, do not resuscitate, and e-codes in California patient discharge data. HSR. 2011;46(6 Pt 1):1946–1962. [Google Scholar]
- 10.Roudsari BS, Ebel BE, Corso PS, Molinari NA, Koepsell TD. The acute medical care costs of fall-related injuries among the U.S. older adults. Injury. 2005;36(11):1316–1322. doi: 10.1016/j.injury.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 11.LeMier M, Cummings P, West TA. Accuracy of external cause of injury codes reported in Washington State hospital discharge records. Injury Prevention. 2001;7(4):334–338. doi: 10.1136/ip.7.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langley J, Stephenson S, Thorpe C, Davie G. Accuracy of injury coding under ICD-9 for New Zealand public hospital discharges. Injury Prevention. 2006;12(1):58–61. doi: 10.1136/ip.2005.010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenzie K, Enraght-Moony EL, Walker SM, McClure RJ, Harrison JE. Accuracy of external cause-of-injury coding in hospital records. Injury Prevention. 2009;15(1):60–64. doi: 10.1136/ip.2008.019935. [DOI] [PubMed] [Google Scholar]
- 14.Annest JL, Fingerhut LA, Gallagher SS, et al. Strategies to improve external cause-of-injury coding in state-based hospital discharge and emergency department data systems: Recommendations of the CDC Workgroup for Improvement of External Cause-of-Injury Coding. MMWR Recomm Rep. 2008;57(RR-1):1–15. [PubMed] [Google Scholar]
- 15.Ganz DA, Kim S-B, Zingmond DS, et al. Effect of a falls quality improvement program on serious fall-related injuries. J Am Geriatr Soc. 2015;63(1):63–70. doi: 10.1111/jgs.13154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finkelstein E, Prabhu M, Chen H. Increased prevalence of falls among elderly individuals with mental health and substance abuse conditions. American Journal of Geriatric Psychiatry. 2007;15(7):611–619. doi: 10.1097/JGP.0b013e318033ed97. [DOI] [PubMed] [Google Scholar]
- 17.Hendrie D, Hall SE, Arena G, Legge M. Health system costs of falls of older adults in Western Australia. Australian Health Review. 2004;28(3):363–373. doi: 10.1071/ah040363. [DOI] [PubMed] [Google Scholar]
- 18.Mahoney JE, Glysch RL, Guilfoyle SM, Hale LJ, Katcher ML. Trends, risk factors, and prevention of falls in older adults in Wisconsin. WMJ : official publication of the State Medical Society of Wisconsin. 2005;104(1):22–28. [PubMed] [Google Scholar]
- 19.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj. Prev. 2006;12(5):290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization International statistical classification of diseases and related health problems 10th revision (ICD-10) version for 2010. 2010.
- 21.CMS . Medicare enrollment - aged beneficiaries as of July 2008. Washington, D.C: 2008. [Google Scholar]
- 22.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: A systematic review and meta-analysis. Epidemiology. 2010;21(5):658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 23.Currie L. Fall and Injury Prevention. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): 2008. [PubMed] [Google Scholar]
- 24.Ellis AA, Trent RB. Hospitalized fall injuries and race in California. Inj. Prev. 2001;7(4):316–320. doi: 10.1136/ip.7.4.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Letts L, Moreland J, Richardson J, et al. The physical environment as a fall risk factor in older adults: Systematic review and meta-analysis of cross-sectional and cohort studies. Aust. Occup. Ther. J. 2010;57(1):51–64. doi: 10.1111/j.1440-1630.2009.00787.x. [DOI] [PubMed] [Google Scholar]
- 26.Fauth EB, Zarit SH, Malmberg B, Johansson B. Physical, cognitive, and psychosocial variables from the Disablement Process Model predict patterns of independence and the transition into disability for the oldest-old. The Gerontologist. 2007;47(5):613–624. doi: 10.1093/geront/47.5.613. [DOI] [PubMed] [Google Scholar]
- 27.Tinetti ME. Prevention of falls among the elderly. N Engl J Med. 1989;348:1055–1059. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- 28.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J. Am. Geriatr. Soc. 1995;43(11):1214–1221. doi: 10.1111/j.1532-5415.1995.tb07396.x. [DOI] [PubMed] [Google Scholar]
- 29.Yamashita T, Noe DA, Bailer AJ. Risk factors of falls in community-dwelling older adults: Logistic regression tree analysis. The Gerontologist. 2012 doi: 10.1093/geront/gns043. [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME. Prevention of falls among the elderly. NEJM. 1989;348:1055–1059. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- 31.Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, Rubenstein LZ. Fall risk assessment measures: An analytic review. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;56(12):M761–766. doi: 10.1093/gerona/56.12.m761. [DOI] [PubMed] [Google Scholar]
- 32.AGS The American Geriatrics Society: Guidelines for prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–672. [PubMed] [Google Scholar]
- 33.Rubenstein LZ, Josephson KR. Falls. In: Kenny RA, editor. Syncope in the Older Patient. Chapman and Hall; London: 1996. pp. 283–297. [Google Scholar]
- 34.Dal Forno G, Chiovenda P, Bressi F, et al. Use of an Italian version of the telephone interview for cognitive status in Alzheimer's disease. Int. J. Geriatr. Psychiatry. 2006;21(2):126–133. doi: 10.1002/gps.1435. [DOI] [PubMed] [Google Scholar]
- 35.Gannon B, O'Shea E, Hudson E. Economic consequences of falls and fractures among older people. Ir. Med. J. 2008;101(6):170–173. [PubMed] [Google Scholar]
- 36.Mahoney JE, Glysch RL, Guilfoyle SM, Hale LJ, Katcher ML. Trends, risk factors, and prevention of falls in older adults in Wisconsin. Wmj. 2005;104(1):22–28. [PubMed] [Google Scholar]
- 37.Wu S, Keeler EB, Rubenstein LZ, Maglione MA, Shekelle PG. A cost-effectiveness analysis of a proposed national falls prevention program. Clin Geriatr Med. 2010;26(4):751–766. doi: 10.1016/j.cger.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Frick KD, Kung JY, Parrish JM, Narrett MJ. Evaluating the cost-effectiveness of fall prevention programs that reduce fall-related hip fractures in older adults. J Am Geriatr Soc. 2010;58(1):136–141. doi: 10.1111/j.1532-5415.2009.02575.x. [DOI] [PubMed] [Google Scholar]
- 39.Hendriks MR, Evers SM, Bleijlevens MH, van Haastregt JC, Crebolder HF, van Eijk JT. Cost-effectiveness of a multidisciplinary fall prevention program in community-dwelling elderly people: A randomized controlled trial. Int J Technol Assess Health Care. 2008;24(2):193–202. doi: 10.1017/S0266462308080276. [DOI] [PubMed] [Google Scholar]
- 40.Tinetti ME, Gordon C, Sogolow E, Lapin P, Bradley EH. Fall-risk evaluation and management: Challenges in adopting geriatric care practices. The Gerontologist. 2006;46(6):717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]
- 41.RAND . Falls prevention interventions in the Medicare population. The RAND Corporation, prepared for the U.S. Department of Health and Human Services; Baltimore, MD: 2003. [Google Scholar]
- 42.Fleurence RL. Cost-effectiveness of fracture prevention treatments in the elderly. Int J Technol Assess Health Care. 2004;20(2):184–191. doi: 10.1017/s0266462304000960. [DOI] [PubMed] [Google Scholar]
- 43.Adams JE, Steinmann SP. Acute scaphoid fractures. Orthopedic Clinics of North America. 2007;38(2):229–235. doi: 10.1016/j.ocl.2007.02.004. vi. [DOI] [PubMed] [Google Scholar]
- 44.Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. The Journal of Bone and Joint Surgery. 1984;66(1):114–123. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 45.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. Journal of Bone and Joint Surgery. 2010;92(3):542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 46.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 47.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002;18(2):141–158. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 48.Sleet DA, Moffett DB, Stevens J. CDC's research portfolio in older adult fall prevention: A review of progress, 1985-2005, and future research directions. J Safety Res. 2008;39(3):259–267. doi: 10.1016/j.jsr.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Kramer BJ, Vivrette RL, Rubenstein LZ. Engaging community-based organizations in fall prevention education. Gerontol Geriatr Educ. 2011;32(2):182–196. doi: 10.1080/02701960.2011.572209. [DOI] [PubMed] [Google Scholar]
- 50.Rizzo JA, Friedkin R, Williams CS, Nabors J, Acampora D, Tinetti ME. Health care utilization and costs in a Medicare population by fall status. Med. Care. 1998;36(8):1174–1188. doi: 10.1097/00005650-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 51.Kim SB, Zingmond DS, Keeler EB, et al. Development of an algorithm to identify fall-related injuries and costs in Medicare data. Inj Epidemiol. 2016;3:1. doi: 10.1186/s40621-015-0066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.