Abstract
Objectives
Despite increased hospice use over the last decade, end-of-life care intensity continues to increase. To understand this puzzle, we sought to examine regional variation in intensive end-of-life care and determine its associations with hospice use patterns.
Methods
Using Medicare claims for decedents age ≥ 66 years in 2011, we assessed end-of-life care intensity in the last 6 months of life across hospital referral regions (HRRs) as measured by proportion of decedents per HRR experiencing hospitalization, emergency department (ED) use, intensive care unit (ICU) admission, and number of days spent in hospital (hospital-days) and ICU (ICU-days). Using hierarchical generalized linear models and adjusting for patient characteristics, we examined whether these measures were associated with overall hospice use, very short (≤ 7 days), medium (8–179 days), or very long (≥180 days) hospice enrollment, focusing on very short stay.
Results
End-of-life care intensity and hospice use patterns varied substantially across HRRs. Regional-level end-of-life care intensity was positively correlated with very short hospice enrollment. Comparing HRRs in the highest versus the lowest quintiles of intensity in end-of-life care, regions with more intensive care had higher rates of very short hospice enrollment, with adjusted odds ratios [AOR] 1.14 (99% confidence interval [CI]: 1.04–1.25) for hospitalization; 1.23 (CI: 1.12–1.36) for ED use; AOR 1.25 (CI: 1.14–1.38) for ICU admission; AOR 1.10 (CI: 1.00–1.21) for hospital-days and AOR 1.20 (CI: 1.08–1.32) for ICU-days.
Conclusions
At the regional level, increased end-of-life care intensity was consistently associated with very short hospice use.
Keywords: Medicare Hospice Benefit, health services research, geographic variation, end-of-life care
Introduction
For decades, research has documented extensive Medicare spending for beneficiaries in their last year of life.1 Approximately 5% of Medicare enrollees who died in a chosen calendar year accounted for 25.1% of total Medicare annual spending.2 More than 70% of all terminal-year expenses occurred during the last 6 months of life.3,4 Furthermore, such intensity of care is not always aligned with patient and family preferences5–7 and is not associated with better quality of care.8
Hospice programs have expanded markedly in recent decades.9,10 Previous research demonstrated that rising trends in hospice use corresponded with a decreased likelihood of dying in the hospital;11,12 however, the intensity of care at the end of life is still increasing.11,12 To explain this puzzling finding, researchers have speculated that hospice use may be an “add-on” to a growing pattern of more utilization of intensive end-of-life care, after finding that there has also been a recent increase in the number of short hospice stays following a hospitalization.11 Yet previous studies have not empirically examined whether areas with higher rates of more intensive end-of-life care also have higher rates of very short hospice enrollments. The issue of appropriate timing of hospice referral is of great of interest:13 for instance, very short hospice enrollment (i.e., within 7 days of death) has been proposed as a measure of poor quality of end-of-life care, 14 as short length of hospice enrollment has been linked to fewer hospice services received, increased unmet need, and clinical depression among family members.15,16 Evidence of strong correlation between end-of-life care intensity and hospice use (no hospice vs. any hospice), as well as length of hospice use (very short, medium, and very long), may help explain the persistent trends of increasing end-of-life care intensity while hospice use is also expanding nationally. As hospice use has been embraced as the end-of-life care standard, it is imperative to know about how end-of-life care intensity relates to hospice use patterns.
Accordingly, we sought to examine the association between intensity of care in the last 6 months of life and hospice use patterns. We take advantage of regional-level variation in patterns of end-of-life care using data from Medicare fee-for-service decedents. We examined not only overall hospice use but also the length of hospice use, with the hypothesis that an increase in intensity of care in the last 6 months of life may be associated with increased very short hospice use. Findings from this study may provide a more nuanced view of hospice use, recognizing that increases in some types of hospice use (i.e., short-duration) may paradoxically co-occur with increases in intensity of care at the end of life.
Methods
Study design and sample
We conducted a retrospective analysis of all inpatient care and hospice fee-for-service Medicare claims in the 6 months prior to death among all decedents older than 66 years who died between July 1, 2011, and December 31, 2011. We limited our sample to beneficiaries who were enrolled in Medicare Parts A and B 6 months before death. We conducted hospital referral region (HRR)-level analyses so that we could have sufficient sample size (number of HRR=306) and adequate number of decedents in each HRR. The study was reviewed by the Institutional Review Board of Yale University and was exempt from full review.
Measurement
End-of-life care intensity
The measures of end-of-life care intensity were chosen based on prior literature and data availability.17–19 We included the HRR-level percentage of patients having any hospitalizations, the percentage of patients having any hospitalizations through ED visits, the percentage of patients having any ICU admissions, the number of days spent in hospital (“hospital days”), and the number of days spent in ICUs (“ICU days”). Hospitalization represented a composite measure as it encompasses hospitalization through ED use, and ICU admission. To ascertain these data, we used any revenue center code values of 0450–0459 (emergency room) and 0981 (professional fees—emergency room) in the Medicare claims to capture ED visits. Any revenue center code values of 0200–0219 (excluding 0204, 0205, and 0215) in the inpatient claims were used to determine ICU admission. Given the nature of regional-level analyses, we calculated the proportion of decedents who used intensive care in each HRR and the mean number of days spent in hospital or ICU in each HRR. For each intensive end-of-life care, we assigned the HRRs to 5 quintiles, where quintile 1 represents HRRs with the lowest end-of-life care intensity and quintile 5 those with the highest.
Hospice use
We created a set of binary variables to indicate use of hospice, as well as lengths of hospice use. For the decedents who enrolled with a hospice, we created three binary measures to indicate the following: the decedent experienced very short hospice enrollment (enrollment of 7 days or less), medium-length hospice enrollment (enrollment between 8 and 179 days), or very long hospice enrollment (enrollment of 180 days or longer). Very short hospice enrollment indicated hospice use for ≤7 days of enrollment and that the last hospice enrollment had been initiated ≤7 days prior to death.20
Covariates
We included as candidate covariates patient age (categorized as 66–69 years, 70–74 years, 75–79 years, 80–84 years, and ≥85 years), gender, and race/ethnicity (non-Hispanic white, black, Hispanic, and other). We ascertained chronic conditions using data from the Master Beneficiary Summary File, including heart disease (acute myocardial infarction, heart failure, and ischemic heart disease), Alzheimer’s disease or dementia, kidney disease, diabetes, chronic obstructive pulmonary disease or asthma, depression, stroke, and cancer (breast, colorectal, prostate, lung, and endometrial). In addition, we used zip code information to identify the county of residence and the HRR for each beneficiary. We then used data pertaining to the county in which the patient resided using the Area Resource File (ARF), which included median county-level income and the percentage of adults in the county with a high school education or less, the percentage of individuals in health maintenance organizations (HMOs) in the county, and the number of physicians, hospital beds, skilled nursing facility beds, hospices, and home health agencies per 1,000 people 65 years and older in the county.
Statistical analysis
Analyses were performed separately based on overall hospice use, very short hospice use, medium-length hospice use, and very long hospice use. We calculated intensive end-of-life care measures, for the total sample and for strata defined by type of hospice use (no hospice, any hospice, very short, medium, and very long hospice enrollments). We compared intensive end-of-life care measures between decedents who did not use hospice and the other groups, using x2 test for proportion measures and paired t-test for continuous measures.
In the HRR-level analyses, we calculated the proportions of decedents in each HRR who received intensive end-of-life care as we defined above during the study period, as well as the average length of stay in hospital or ICU in each HRR. We also determined the proportion of decedents who used hospice in each HRR and the proportion of hospice users with very short hospice use, medium-length hospice use, and very long hospice use. Correlations between hospital-based service utilization and hospice hospice-use patterns across HRR-level measures were tested using the Pearson correlation coefficient.
In the adjusted analyses, we used 2-level hierarchical generalized linear models (HGLMs) to examine the HRR-level associations between end-of-life care intensity and hospice use patterns. We included a HRR-level covariate according to the proportion of decedents who used any intensive end-of-life care (categorized by quintile) in multivariable analyses. Our HGLMs allowed us to estimate the associations between end-of-life care intensity and hospice use pattern at the HRR level while simultaneously adjusting for patient characteristics and market factors and accounting for the structure that patients were clustered within HRRs. Using each hospice use pattern as the dependent variable, we evaluated risk estimates across quintiles. For analyses of overall hospice use, all decedents were included. Analyses of length of hospice use were limited to hospice users. All statistical analyses were completed using SAS, version 9.3 (SAS Institute, Cary, NC). To account for multiple comparisons in our study, we applied a Bonferroni correction; thus, a two-tailed p < 0.01 was used to define statistical significance. We reported adjusted odds ratios (AORs) with 99% confidence intervals (CIs).
Results
Patient characteristics
The full study sample consisted of 660,132 decedents enrolled in fee-for-service Medicare during the last 6 months of life. Characteristics of decedents are summarized in Table 1. Approximately 45% of decedents were 85 years or older, 55% were female, and the majority were white. Most had chronic conditions such as heart disease (75.4%), chronic lung disease (48.1%), and diabetes (44.3%).
Table 1.
Characteristics of the beneficiaries
| Characteristics | Patients (n=660,132) |
|---|---|
| Demographic factors | |
| Age: 66–69 | 58,473 (8.9) |
| Age: 70–74 | 80,087 (12.1) |
| Age: 75–79 | 96,973 (14.7) |
| Age: 80–84 | 127,998 (19.4) |
| Age: 85+ | 296,601 (44.9) |
| Gender: female | 362,101 (54.9) |
| Race/ethnicity: non-Hispanic white | 558,223 (84.6) |
| Race/ethnicity: black | 55,332 (8.4) |
| Race/ethnicity: Hispanic | 28,352 (4.3) |
| Race/ethnicity: other | 18,225 (2.8) |
| Geographic factors | |
| Metropolitan statistical area (missing n=936) | |
| No | 63,662 (9.7) |
| Micropolitan | 91,388 (13.9) |
| Metropolitan | 504,146 (76.5) |
| County-level education (>=high school; missing n=936) | |
| < 60% | 905 (0.1) |
| 60–70% | 14,075 (2.1) |
| 70–80% | 106,969 (16.2) |
| 80–90% | 407,381 (61.8) |
| ≥ 90% | 129,866 (19.7) |
| County-level median household income (missing n=936) | |
| < $33,000 | 7,843 (1.2) |
| $33,000–$39,999 | 132,944 (20.2) |
| $40,000–$49,999 | 242,445 (36.8) |
| $50,000–$62,999 | 177,606 (26.9) |
| ≥ $63,000 | 98,358 (14.9) |
| Chronic conditions | |
| Heart disease | 497,492 (75.4) |
| Alzheimer’s disease/dementia | 273,967 (41.5) |
| Kidney disease | 274,100 (41.5) |
| Diabetes | 292,473 (44.3) |
| Lung disease | 317,553 (48.1) |
| Depression | 277,173 (42.0) |
| Stroke | 194,040 (29.4) |
| Cancer | 159,513 (24.2) |
Values are numbers (percentages).
A total of 348,519 (52.8%) decedents did not use hospice in the last 6 months of life, 68.4% of them had been hospitalized with mean hospital days of 12.3 days (Table 2). Compared with decedents who did not use hospice, hospice users were less likely to be hospitalized (66.1%, P-value < .001). Among those hospice users, 32.4% had very short hospice enrollments, and they were significantly more likely to experience hospitalization than decedents who did not use hospice (83.5%, P-value < .001); 57.6% had medium-length hospice use, and they were less likely than decedents without hospice use to incur intensive end-of-life care (P-value < .001 for all measures); and decedents with very long hospice enrollments were significantly less likely to receive intensive end-of-life care with hospitalization rate of 8.3% in the last 6 months of life (P-value < .001).
Table 2.
End-of-life care intensity in the last 6 months of life according to hospice use patterns
| Pattern of hospice use | Total Sample | All decedents | Any hospice | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | No hospice | Any hospice | P-value | Very short (≤7 days) | Medium | Very long (≥180 days) | ||||
| N (%) | N (%) | N (%) | P-value | N (%) | P-value | N (%) | P-value | |||
| No of patients | 659494 (100%) |
348,519 (52.8%) |
310,975 (47.2%) |
100,830 (32.4%) |
179,243 (57.6%) |
30,902 (9.9%) |
||||
| End-of-life care | ||||||||||
| Hospitalized | 443,881 (67.3) |
238,344 (68.4) |
205,537 (66.1) |
<.001 | 84,258 (83.6) |
<.001† | 118,715 (66.2) |
<.001† | 2,564 (8.3) |
<.001 |
| ED | 382172 (57.9) |
202,845 (58.2) |
179,327 (57.8) |
<.001 | 75,043 (74.4) |
<.001† | 102,058 (56.9) |
<.001† | 2,226 (7.2) |
<.001† |
| ICU | 265,367 (40.2) |
157,841 (45.3) |
107,526 (34.6) |
<.001† | 50,502 (50.1) |
<.001† | 56,173 (31.3) |
<.001† | 851 (2.8) |
<.001 |
| Hospital days* | 11.3 (16.7) |
12.3 (18.4) |
10.2 (14.4) |
<.001 | 14.3 (16.5) |
<.001 | 9.6 (13.4) |
<.001† | 0.5 (2.2) |
<.001 |
| ICU days* | 3.0 (7.6) |
3.7 (8.8) |
2.3 (5.9) |
<.001† | 3.7 (7.5) |
0.08† | 1.8 (5.1) |
<.001† | 0.1 (0.7) |
<.001 |
Values are number (percentage) unless stated otherwise. The reference group for comparison is decedents with no hospice use.
Values in parentheses are standard deviations.
Results were still significant in fully adjusted model.
Regional-level end-of-life care intensity
The average proportion of decedents in an HRR who had at least one hospitalization in the last 6 months of life was 66.4% (standard deviation [SD]=5.5%), ranging from 48.6% to 81.9% (Figure 1A). The average percentage of hospitalization through ED visits in the last 6 months was 55.8% (SD=9.1%; from 26.1% to 75.4%); the percentage of ICU admissions in the last 6 months was 35.5% (SD=8.5%; from 15.4% to 66.4%); the average number of days spent in hospital in the last 6 months was 10.6 (SD=2.9; from 4.3 days to 21.9 days); and the average number of ICU days was 2.8 (SD=1.2; from 0.7 days to 8.6 days). Overall hospice use among decedents and hospice use patterns among hospice users also varied substantially across HRRs (Figure 1B).
Figure 1.
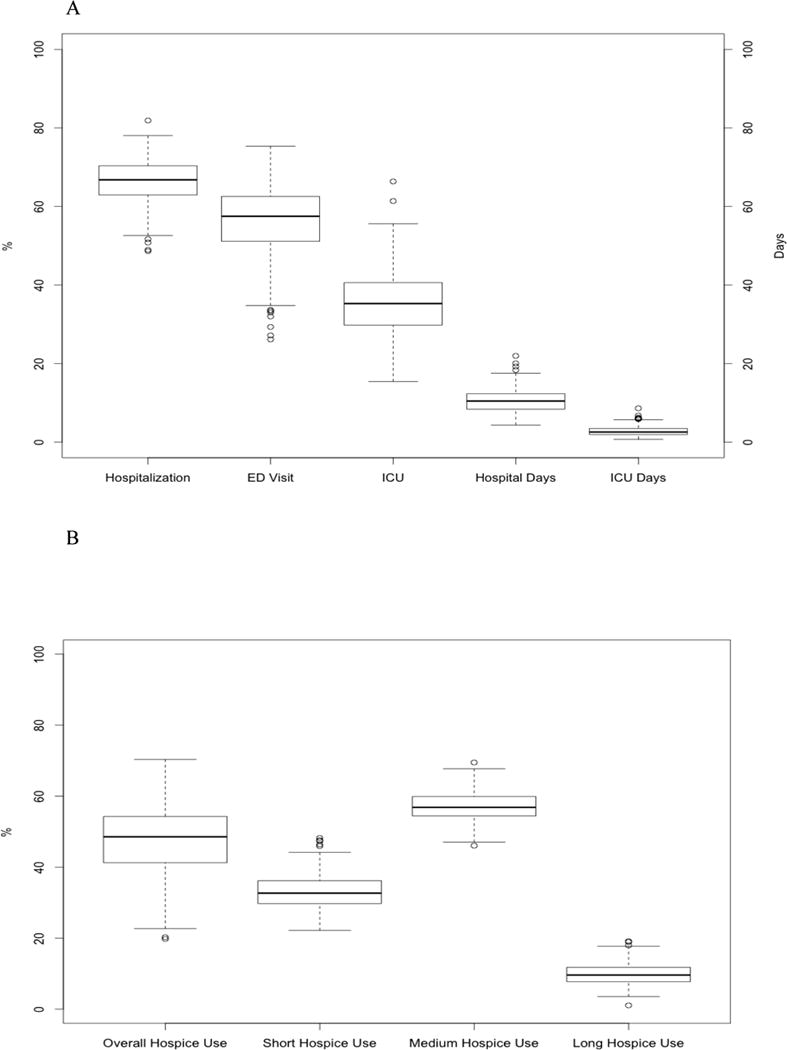
HRR-level variation in end-of-life care intensity (A) and hospice use patterns (B) in the last 6 months of life
HRR-level intensity of end-of-life care and hospice-use patterns
In unadjusted analyses, all measures of HRR-level end-of-life care intensity were significantly associated with increased proportions of decedents having very short hospice enrollment (Table 3). End-of-life care intensity was also significantly negatively correlated with the proportions of hospice users who had medium-length hospice enrollment. At the HRR-level, none of the measures of care intensity was significantly correlated with the overall proportion of decedents who used hospice, except a positive correlation between ICU admission and the proportion having used hospice at all.
Table 3.
HRR-level correlations between end-of-life care intensity and hospice use patterns*
| Hospitalization among decedents in the last 6 months | Hospitalization through ED use among decedents in the last 6 months | ICU among decedents in the last 6 months | Hospital days among decedents in the last 6 months | ICU days among decedents in the last 6 months | |
|---|---|---|---|---|---|
| Hospice use among decedents in the last 6 months | −0.090 (.116) |
0.060 (.298) |
0.165 (.004) |
−0.145 (.011) |
0.076 (.183) |
| Very short hospice enrollment (≤ 7 days) among hospice users in the last 6 months |
0.244 (<.001) |
0.211 (<.001) |
0.203 (<.001) |
0.164 (.004) |
0.205 (<.001) |
| Medium hospice enrollment (8–179 days) among hospice users in the last 6 months | −0.368 (<.001) |
−0.305 (<.001) |
−0.318 (<.001) |
−0.259 (<.001) |
−0.316 (<.001) |
| Very long hospice enrollment (≥ 180 days) among hospice users in the last 6 months | −0.026 (.649) |
0.087 (.131) |
0.119 (.037) |
0.100 (.080) |
0.113 (.048) |
The unit of analysis is HRR. Values in parentheses are p-values.
ED: Emergency department; ICU: Intensive care unit. Numbers in bold indicate significance where p-value < .01.
HRRs in the highest compared with the lowest quintile of hospitalization did not differ significantly in rates of overall hospice use with AOR of 1.05 (99% CI: 0.89–1.25); but had significantly elevated rates of very short hospice use with AOR of 1.14 (99% CI: 1.04–1.25; Table 4). For nearly all other measures of intensive end-of-life care, HRRs in the highest compared with lowest quintile of end-of-life care intensity had significantly higher rates of very short hospice use: AOR 1.23 (99% CI: 1.12–1.36) for hospitalization through ED use; AOR 1.25 (99% CI: 1.14–1.38) for ICU admission; and AOR 1.20 (99% CI: 1.08–1.32) for ICU-days. The exception to this is hospital-days: marginally significant with AOR 1.10 (99% CI: 1.00–1.21). HRRs with increased intensive end-of-life care also had significantly lower rates of hospice users with medium-length enrollments. Most of the associations between end-of-life care intensity and very long hospice use were statistically insignificant.
Table 4.
Adjusted odds of hospice use patterns as associated with regions in the highest quintile of end-of-life care intensity versus the lowest quintile*
| Care intensity measure | Mean percentage of intensive care | Hospice use patterns | |||
|---|---|---|---|---|---|
| Overall hospice use | Very short hospice use | Medium-length hospice use | Very long hospice use | ||
| Hospitalization | Q1: 60.0 | Reference | Reference | Reference | Reference |
| Q5: 73.0 | 1.05 (0.89, 1.25) | 1.14 (1.04, 1.25) | 0.90 (0.84, 0.97) | 0.95 (0.82, 1.09) | |
| ED visits | Q1: 45.0 | Reference | Reference | Reference | Reference |
| Q5: 66.8 | 0.94 (0.78, 1.12) | 1.23 (1.12, 1.36) | 0.88 (0.82, 0.95) | 0.83 (0.72, 0.96) | |
| ICU admission | Q1: 28.6 | Reference | Reference | Reference | Reference |
| Q5: 52.2 | 1.37 (1.15, 1.65) | 1.25 (1.14, 1.38) | 0.81 (0.75, 0.87) | 1.02 (0.88, 1.20) | |
| Hospital days | Q1: 7.6† | Reference | Reference | Reference | Reference |
| Q5: 15.4† | 1.00 (0.99, 1.20) | 1.10 (1.00, 1.21) | 0.91 (0.84, 0.98) | 1.04(0.90, 1.21) | |
| ICU days | Q1: 1.5† | Reference | Reference | Reference | Reference |
| Q5: 4.9† | 1.24 (1.02, 1.50) | 1.20 (1.08, 1.32) | 0.83 (0.77, 0.89) | 1.09 (0.93, 1.27) | |
Values are adjusted odds ratios (99% confidence intervals).
Q1: Quintile 1 (lowest quintile of end-of-life care intensity); Q5: Quintile 5 (highest quintile of end-of-life care intensity)
Quintiles are defined by proportion of decedents experiencing intensive end-of-life care.
Mean number of days spent in hospital or ICU in quintiles 1 and 5.
Discussion
We found that approximately two-thirds of Medicare beneficiaries who died in 2011 used hospital, ED, or ICU services in the last 6 months of life, a proportion that varied substantially across HRRs nationally. Additionally, of the decedents who enrolled in hospice, 32% of hospice users had very short enrollments, versus 58% with medium-length and 10% with very long enrollments. Notably, HRRs with greater intensity of end-of-life care also had significantly higher proportions of decedents with very short hospice enrollments before death. These associations remained statistically significant after adjusting for individual patient characteristics and regional health-care supply factors. Previous data have documented substantial increases in hospice use, short hospice enrollments, and ICU admissions during the last 6 months of life.11 Our results help resolve the puzzle of increasing end-of-life care intensity while at the same time having increased hospice use by demonstrating that certain patterns of hospice use are linked to higher end-of-life care intensity. The finding supports the idea that much of the increases in hospice, especially the 30% of very short hospice use, may be as an “add on” to an otherwise high intensity course of care.11 Our findings are important for policy decision-making, especially in regions with high end-of-life care intensity. Efforts that aim only at increasing the number of individuals who access hospice, without attention to factors that influence the timeliness of hospice enrollment, may miss opportunities to leverage the benefits of hospice care in mitigating high end-of-life care intensity.
The differences in end-of-life care intensity among groups experiencing different lengths of hospice enrollment are particularly intriguing. While decedents who used hospice were significantly less likely to use intensive end-of-life care, the differences were not substantial except with regard to the measures of ICU use. In our study, more than four-fifths of very short hospice users were hospitalized, approximately three-fourths had an ED visit, and one half had an ICU admission—all of which are proportions demonstrating that very short hospice users experienced more intensive care than that experienced by non-hospice users. In fact, non-hospice users and very short hospice users experienced more intensive end-of-life care than medium or very long hospice users did. These findings suggest that non-hospice users and users of very short hospice may have important factors in common (e.g. absences in end-of-life planning), which could in turn drive both more intensive care and difficulty in timing hospice enrollment. In contrast, minimal proportions of very long hospice users incurred intensive care in the last 6 months. While these patients would have increased spending on hospice services, very long hospice use may decrease patient’s suffering where end-of-life care intensity is concerned. Nonetheless, our results underscore the necessity to identify and address regional factors that may be affecting both timely hospice enrollment and intensity of end-of-life care.
The existing literature is mixed on whether hospice use serves as a complement to or a substitution for hospital-based services at the end of life.2 Wennberg and colleagues have found that hospice use was inversely correlated with hospital stays in the last 6 months of life, suggesting substitution effects between hospice and hospital care;19 however, increased numbers of very short hospice enrollments following a hospitalization has suggested that hospice and hospital-based care may be complements, 11 a suggestion that is consistent with data that end-of-life care in the United States remains highly intensive, even as hospice use has dramatically expanded in recent decades.12,21 Our results imply that both complementary and substitutional effects may exist. For some beneficiaries, timely hospice use may decrease hospital-based services; while for others, hospice use may be used as an “add-on” to conventional hospital-based services.
Prior literature has shown that intensity of health care at the end of life varies widely across the United States.8 There is growing concern about regional variation in end-of-life care intensity as high-intensity care appears misaligned with patient preferences and may represent inefficient or poor-quality care.21 The Dartmouth Atlas of Health Care, for instance, has reported the intensity of hospital resource utilization.21 Our measures differ from the Dartmouth measures because we included all decedents regardless of hospitalization status and conditions, whereas the cohort in the Dartmouth Atlas is restricted to beneficiaries with at least 1 hospital admission for 1 of 11 diagnoses that were known to confer a high risk of inpatient mortality.22 Building upon prior research, our study provided a more comprehensive picture regarding geographic variation of care intensity at the end of life in the United States.
Our findings should be interpreted in light of several limitations. First, our focus was on associations between end-of-life care intensity and hospice use pattern across HRRs, which was different from individual-level analyses. For example, researchers found that the growth in hospice care for nursing home residents was associated with less aggressive care near death.23 However, our findings are informative to policy makers and may facilitate their efforts on monitoring, benchmarking, and improving end-of-life care quality at the population level. Second, although our model adjusted for chronic conditions, we did not know the severity of disease, nor did we have information regarding patient preference of hospice use and end-of-life care. Nonetheless, prior literature has shown that patient preferences explain little of regional variation in end-of-life health care utilization.7 Third, we did not have complete cost information and thus could not include cost in our measures. Future research is needed. Finally, as a cross-sectional study, our research cannot be interpreted to make causal inferences. Future research using longitudinal data and econometric models is needed.
In conclusion, we provided contemporary data on regional-level variation in end-of-life care intensity, as well as its associations with overall hospice use and lengths of hospice use. Our study demonstrated that, at the regional level, associations between end-of-life care intensity and overall hospice use were not straightforward. In contrast, increased end-of-life care intensity was consistently associated with very short hospice use. Effective efforts reduce hospitalization and intensive care at the end of life would benefit from focusing not only on the use of hospice, but on earlier introduction of hospice in the course of care.
Acknowledgments
Funding: This study was supported by grant 1R01CA116398-01A2 from the National Cancer Institute (Drs. Aldridge and Bradley); the John D. Thompson Foundation (Dr. Bradley); grant 1R01NR013499-01A1 from the National Institute of Nursing Research (Dr. Aldridge); and grant 1K01HS023900-01 from the Agency for Healthcare Research and Quality (Dr. Wang).
Dr. Gross receives support from Medtronic, Inc., Johnson & Johnson, Inc., Pfizer, Inc., and 21st Century Oncology. These sources of support were not used for any portion of the current manuscript.
Footnotes
Financial Disclosures: None of the other coauthors have conflicts to report.
References
- 1.Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328(15):1092–6. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- 2.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45(2):565–76. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoover DR, Crystal S, Kumar R, Sambamoorthi U, Cantor JC. Medical expenditures during the last year of life: findings from the 1992–1996 Medicare current beneficiary survey. Health Serv Res. 2002;37(6):1625–42. doi: 10.1111/1475-6773.01113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scitovsky AA. “The high cost of dying”: what do the data show? 1984. Milbank Q. 2005;83(4):825–41. doi: 10.1111/j.1468-0009.2005.00402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–73. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Int Med. 2000;132(10):825–32. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 7.Barnato AE, Herndon MB, Anthony DL, Gallagher PM, Skinner JS, Bynum JP, et al. Are regional variations in end-of-life care intensity explained by patient preferences? A Study of the US Medicare Population Med Care. 2007;45(5):386–93. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Int Med. 2003;138(4):273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 9.While number of patients receiving hospice care increases, larger percentage have short length of service [news release] Alexandria, VA: National Hospice and Palliative Care Organization; Nov 27, 2012. http://www.nhpco.org/press-room/press-releases/hospice-facts-figures. Accessed October 27, 2014. [Google Scholar]
- 10.Aldridge MD, Canavan M, Cherlin E, Bradley EH. Has Hospice Use Changed? 2000–2010 Utilization Patterns. Med Care. 2015;53(1):95–101. doi: 10.1097/MLR.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–7. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright AA, Hatfield LA, Earle CC, Keating NL. End-of-life care for older patients with ovarian cancer is intensive despite high rates of hospice use. JCO. 2014;32(31):3534–9. doi: 10.1200/JCO.2014.55.5383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teno JM, Gozalo PL. Quality and costs of end-of-life care: the need for transparency and accountability. JAMA. 2014;312(18):1868–9. doi: 10.1001/jama.2014.14949. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Clinical Oncology. Summary of Current QOPI Measures. Available at http://www.asco.org/institute-quality/summary-current-qopi-measures (Assessed on August 25, 2015)
- 15.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families’ perceptions of services: are earlier hospice referrals better? J Am Geriatr Soc. 2005;53(5):819–23. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 16.Bradley EH, Prigerson H, Carlson MD, Cherlin E, Johnson-Hurzeler R, Kasl SV. Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry. 2004;161(12):2257–62. doi: 10.1176/appi.ajp.161.12.2257. [DOI] [PubMed] [Google Scholar]
- 17.Hospital Care Intensity - Dartmouth Atlas of Health Care. Available at www.dartmouthatlas.org/tools/care.aspx. Assessed May 23, 2015.
- 18.Blecker S, Anderson GF, Herbert R, Wang NY, Brancati FL. Hospice care and resource utilization in Medicare beneficiaries with heart failure. Med Care. 2011;49(11):985–91. doi: 10.1097/MLR.0b013e318235c221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328(7440):607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang SY, Aldridge MD, Canavan M, Cherlin E, Johnson-Hurzeler R, Bradley EH. Geographic Variation of Hospice Use Patterns at the End of Life. J Palliat Med. 2015;18(9):771–780. doi: 10.1089/jpm.2014.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morden NE, Chang CH, Jacobson JO, Berke EM, Bynum JP, Murray KM, et al. End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Aff (Millwood) 2012;31(4):786–96. doi: 10.1377/hlthaff.2011.0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnato AE, Farrell MH, Chang CC, Lave JR, Roberts MS, Angus DC. Development and validation of hospital “end-of-life” treatment intensity measures. Med care. 2009;47(10):1098–105. doi: 10.1097/MLR.0b013e3181993191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gozalo P, Plotzke M, Mor V, Miller SC, Teno JM. Changes in Medicare costs with the growth of hospice care in nursing homes. N Engl J Med. 2015;372(19):1823–31. doi: 10.1056/NEJMsa1408705. [DOI] [PMC free article] [PubMed] [Google Scholar]


