Abstract
Purpose
Measurement of intraocular pressure (IOP) is one of the basic investigations in a general ophthalmic workup. In this study, we attempt to determine the agreement in the measurement of IOP obtained by Perkin’s applanation tonometer, noncontact tonometer and Schiotz indentation tonometer in patients attending general ophthalmology OPD in a tertiary care centre in South India and its use in a community ophthalmology setting.
Methods
A cross-sectional analytical study in which IOP was measured in patients using the three tonometers. Central corneal thickness (CCT) was measured using Ultrasonic pachymetry. Bland Altman analysis was done to evaluate the agreement between instruments.
Results
800 eyes of 400 patients were included in the study. By Bland Altman method, Schiotz indentation tonometer was found to have better correlation to IOP obtained by Perkin’s applanation tonometer. Schiotz indentation tonometer was found to be most accurate when CCT was in the range of 501–550 μm and noncontact tonometer was found to be least accurate when CCT was greater than 600 microns. On comparing correlation at different age groups, both the methods had better correlation at <40 years age group.
Conclusion
Both the tonometers showed a significant correlation with the gold standard technique (Perkin’s applanation tonometer) over a range of IOP and CCT with the Schiotz tonometer better than the NCT. This study proves that Schiotz tonometer can be recommended as a reliable screening tool in community outreach ophthalmology services. The twin advantages of portability and availability make the Schiotz tonometer a popular choice among ophthalmology trainees and optometrists in a developing country like India.
Keywords: Perkin’s tonometer, Noncontact tonometer (NCT), Schiotz indentation tonometer, Intraocular pressure (IOP), Tonometry, Central corneal thickness (CCT)
Introduction
Worldwide, Glaucoma is the second most common cause of irreversible visual loss, with its prevalence in South India varying between 1.62% and 2.6%.1, 2
A chronic optic neuropathy with characteristic structural and functional changes in the optic nerve head, an important risk factor for glaucoma is increased Intraocular pressure (IOP). A normal intraocular pressure is essential to maintain the shape of the eye and visual function with prolonged elevation in IOP resulting in irreversible damage to the retinal ganglion cells and postganglionic nerve fibres.3 Detecting the IOP is essential in not only initiating treatment, but also in monitoring the response to treatment.4 The past few decades have seen a rapid evolution of tonometry instrumentation to ensure more accurate measurement of IOP. However, both ocular and nonocular factors often exert confounding influences in the accurate measurement of the IOP and complicate the treatment.5
Public sector health institutions in India primarily serve the underprivileged sections of the society and rural camps are the most effective measures to screen the population for debilitating vision disorders. In population screenings and rural camp settings for glaucoma detection, the ease of operability and cost significantly influence the selection of the tonometer. Also, in many instances, absence of sufficient manpower requires the services of an optometrist to perform a quick IOP measurement. However, the accuracy of such cheap and user-friendly tonometer may be called into question in comparison with the gold standard. It, therefore, becomes essential to determine the reliability of these tonometers and also to determine their usefulness in special situations.
In this study we aimed to evaluate the efficacy of Schiotz indentation tonometer and Non-contact tonometer (NCT) in measuring the IOP as compared to Perkins handheld applanation tonometer (handheld model of Goldman applanation tonometer (GAT- the gold standard)) and to determine the inter-instrument agreement of these tonometers with Perkins tonometer over a range of central corneal thickness (CCT). The reliability of these tonometers with Perkins tonometer during mass screening of IOP in rural and community outreach eye camps was also analysed.
Materials and method
This study was approved by the Institute Research Board and Ethical Committee. Over a 4 month period (January–April 2013), patients of both sexes between the ages of 20–80 years attending the outpatient services were randomly screened and included in this study. Patients with pre-existing corneal pathologies and nystagmus were excluded from the study. The IOP was measured by a single investigator using the Noncontact Tonometer, Perkin’s applanation tonometer and Schiotz indentation tonometer in that order to prevent lowering of IOP induced by contact. In all cases, a 5 min interval was ensured between any two methods of IOP measurement and an average of three measurements was taken as the final IOP obtained by that method. CCT was measured with the Altair Ultrasonic pachymeter after tonometric measurements had been completed.
First, the patient was seated at the tabletop model of Canon TX-10 Noncontact Tonometer (Canon USA Inc, USA) and asked to fix at the target. The examiner aligned the cornea by superimposing the reflection of the target from the patient’s cornea on a stationary ring. An air puff was automatically triggered when alignment was satisfactory.
Then, the patient’s cornea was anaesthetized with topical application of 0.5% proparacaine hydrochloride and the tear film stained with sodium fluorescein using paper strips impregnated with fluorescein. With the patient in a sitting position, under cobalt blue light illumination, the biprism of Perkin’s tonometer (Haag-Streit, USA) was brought into gentle contact with the centre of the cornea. The fluorescein semicircles were viewed through the biprism, and the calibrated dial was adjusted till the inner edges overlapped. The reading on the dial was multiplied by ten for the IOP value.
Finally, the patient was placed in a supine position and asked to fix at a target. Zero error of Schiotz indentation tonometer (Medetz Surgical, USA) was taken by placing the footplate on the test block provided. The eyelids were separated by hand without exerting pressure on the globe, and the tonometer foot plate was placed on the anaesthetized cornea so that the plunger moved freely vertically. The scale reading was noted. The 5.5 gram weight was initially used, but if scale reading was four or less additional weights were added to the plunger. The subsequent readings were taken with additional weights to overcome the influence of sclera rigidity. These readings were converted to IOP measurement in mm of Hg by using Friedenwald’s table.
Following the completion of IOP measurements, the ultrasonic pachymetry probe (Optikon 2000 S.p.A, Altair, Rome, Italy) was placed on the centre of the anaesthetized cornea. Three consecutive readings were taken and averaged to get the central corneal thickness. CCT values were categorized as per the findings of the Los Angeles Latino Eye Study Group.6
The results of all four diagnostic investigations were analysed by Microsoft Excel Program for frequency distribution and computed in percentages.
Statistical analyses were performed using MedCalc for Windows, version 13.3.1 (MedCalc Software, Ostend, Belgium). IOP measurements were compared to those obtained by the Perkin’s handheld applanation tonometer which was assumed to be the gold standard (Sensitivity, specificity, positive and negative predictive values). Regression Analysis was also performed to determine any causal relationship (Dependant variable -Perkin’s Tonometer IOP; Independent variables- Noncontact tonometer IOP, Schiotz tonometer IOP, age, gender and CCT). A Bland–Altman plot was constructed to investigate the existence of any systematic difference between the different tonometry methods.
Results
Both the eyes of all included patients have been studied. Therefore for our analysis, background characteristics were calculated based on sample size of 400 patients while the remaining analysis was based on 800 eyes.
The study population comprised of 36 per cent males with mean age of 54 years (95% CI 52.8–55.5, range 26–78 years) and 64 per cent females with mean age of 55.6 years (95% CI 54.7–56.7, range 20–80 years). The mean age of all patients in this study was 55.1 years (95% CI 54.3–55.9 years).
The mean CCT was 527.5 microns (μm) (95% CI 524.6–530.5) ranging between 360 μm and 646 μm. Maximum eyes (n = 423) had CCT in the range of 501–550 μm and only 48 eyes had CCT above 600 μm.
The mean of IOP measured by Perkin’s Tonometer, Noncontact Tonometer and Schiotz Tonometer was 13.8 mmHg (95% CI 13.5–14.2), 13.9 mmHg (95% CI 13.5–14.2) and 14.97 mmHg (95% CI 14.7–15.3) respectively. Most eyes (n = 497) had values between 11 and 20 mmHg while only 8.5% eyes (n = 68) had IOP of more than 21 mm Hg. On evaluating the validity of the IOP measurements, both NCT and Schiotz Tonometer were found to have high specificity and negative predictive value (Table 1).
Table 1.
Noncontact tonometer and Schiotz Tonometer when compared with the gold standard Perkin’s tonometer.
| Parameters | NCT Vs Perkin’s Tonometer | Schiotz Tonometer Vs Perkin’s Tonometer |
|---|---|---|
| Sensitivity | 50% (95% CI: 37.6–62.3) | 42.7% (95% CI: 30.7–55.2) |
| Specificity | 98.9% (95% CI: 97.9–99.5) | 99.5% (95% CI: 98.6–99.8) |
| Positive predictive value | 80.9% (95% CI: 65.9–91.4) | 87.8% (95% CI: 71.8–96.6) |
| Negative predictive value | 95.5% (95% CI: 93.8–96.9) | 94.9% (95% CI: 93.1–96.4) |
NCT- Noncontact Tonometer.
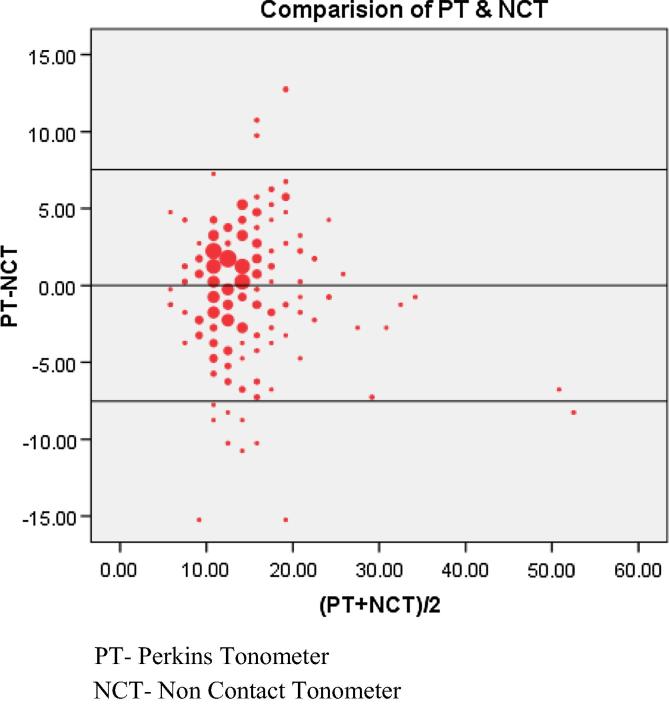
According to the Bland Altman plot, the mean (±S.D.) measurement for Perkins tonometer was 13.8 mmHg (±5.2) compared with 13.9 mmHg (±5.2) for the Noncontact Tonometer method. The bias of the method was −0.02 (95% CI −0.29, −0.26) and precession was 3.9 (95% CI = −7.67, 7.64) (Chart 1).
Chart 1.
Bland–Altman plot: Perkin’s tonometer and Noncontact Tonometer.
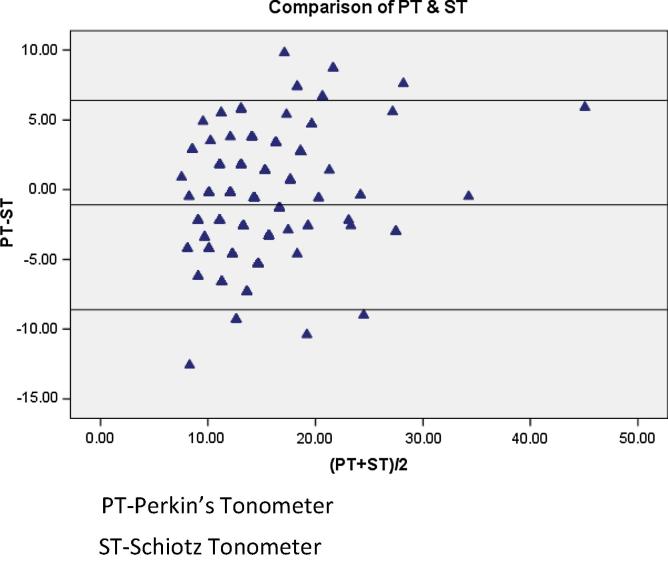
The mean (±S.D) measurement for Perkins tonometer was 13.8 mmHg (±5.2) compared with 14.97 mmHg (±4.1) for the Schiotz Tonometer method. The bias of the method was – 1.1 (95% CI = 1.39, −0.85) and precession was 3.88 (95% CI = −8.7, 6. 4) (Chart 2).
Chart 2.
Bland–Altman plot: Perkin’s tonometer and Schiotz tonometer.
Bland–Altman plot indicated that while both the Schiotz tonometer and Noncontact tonometer correlated with Perkin’s handheld applanation tonometer, the former was found to correlate marginally better (SD of 3.87 for Schiotz tonometer versus SD of 3.91 for NCT when compared to Perkin’s tonometer).
When compared over different CCT ranges, the Schiotz and Noncontact tonometers were most accurate when the CCT was in the range of 501–550 microns. This correlation was significant at p value of 0.01 level (2-tailed) in almost all cases. However, the accuracy of the Noncontact tonometer was poor when the CCT was greater than 600 μm (Pearson’s correlation 0.22).
On comparing correlation at different age groups, both the tonometers had significant correlation with Perkin’s tonometer (significant at p value of 0.01 level, 2-tailed), with maximum correlation at <40 years group. Regression analysis with a standard error of 3.14 indicated that the independent variables could explain 57% of variation in IOP by Perkin’s tonometer (R square: 0.57) (Table 2).
Table 2.
Regression analysis.
| Coefficients | P-value | |
|---|---|---|
| Intercept | 2.8 | 0.1 |
| Noncontact tonometer | 0.5 | 2.28E−40 |
| Schiotz tonometer | 0.4 | 7.33E−17 |
| Age | 0.01 | 0.4 |
| Gender | 0.8 | 0.00 |
| Central corneal thickness | −0.01 | 0.02 |
| Laterality of eye | −0.63 | 0.01 |
Dependent variable- IOP by Perkin’s tonometer.
Independent variable-IOP by NCT, Schiotz tonometer, age, gender, central corneal thickness and laterality of eye.
Discussion
Population screening for glaucoma based solely on IOP may not be necessarily identifying all patients due to variable response of the human eye to the changing IOP. Although multiple risk factors can account for the susceptibility to glaucomatous damage, the IOP is the only risk factor that is amenable to treatment by pharmacological and surgical measures.4 Baseline values of the IOP will help the clinician in monitoring progress of the disease and response to treatment. While a number of tonometers are available for measuring the IOP, each has its own advantages and disadvantages. The increased costs and the need for specialized training for optimal utilization of modern tonometers preclude the use of such tonometers in the rural camp setting and outreach mass screening programmes.
Applanation tonometry is the method of measuring IOP with instruments that flatten the corneal apex. The Goldman applanation tonometer (GAT) is regarded as the gold standard, and the Perkins tonometer is the portable version of the GAT. However, the GAT has certain disadvantages. Firstly, the probe of the instrument contacts the cornea that can result in corneal abrasions and cross infection. Secondly, the requirement of local anaesthesia makes it unpopular among patients unwilling to permit or tolerate drug application. Thirdly, while the accuracy of measurement is dependent on the amount of fluorescein in the cul de sac, other factors such as the CCT, corneal curvature, axial length and the structural rigidity of the cornea are well-known sources of error in conventional applanation tonometry.7, 8, 9, 10 And finally, the GAT does not permit its use in the rural mass screening programmes that are required in a country like India.
The Perkins tonometer, albeit, being an excellent alternative to the GAT is prohibitively expensive ($1400 approx) for use in a community screening setting. Further, the Perkins handheld applanation tonometer requires a trained ophthalmologist for accurate measurements and needs to be sterilized after each reading.
The Noncontact tonometer (NCT) is a user-friendly instrument that lends well to use by the ophthalmology trainee as well as by the optometrist. The NCT has the potential advantage that it uses an air puff to indent the cornea thereby reducing the possible risk of epithelial trauma and cross infection which can be of tremendous advantage while in use in mass screening camp setting.11 Nevertheless, the use of the NCT by an ophthalmology trainee in a community screening is deterred by its cost ($2000/-approx). The NCT is often difficult to perform in patients with poor fixation and has also been found to significantly underestimate GAT measurements at lower IOP and to overestimate those at higher IOP.12
The Schiotz tonometer is another user-friendly instrument available for use by both the ophthalmology trainee and the optometrist with twin advantages of portability and affordability ($300/approx). However, the results of Schiotz tonometry are known to be affected by factors such as scleral rigidity, compressibility of the vascular content of the eye, the ease with which the fluid is expressed through the drainage channels and “Moses effect”13 With the advent of applanation tonometers, there has been some doubt on the accuracy of the Schiotz tonometer. Several workers have compared the efficacy of tonometers with some showing good correlation between applanation tonometers and indentation tonometers and others finding only a moderate agreement between NCT and applanation tonometer.14, 15
In this study, we have compared both Schiotz indentation tonometer and NCT to Perkin’s tonometer in the same set of patients and determined their respective agreement to Perkin’s by Bland–Altman method.16 Surprisingly, the Schiotz indentation tonometer was found to agree better with Perkins than NCT suggesting that the IOP measurements by the Schiotz indentation tonometer are still clinically acceptable. The bias on comparing the two tonometers to Perkins was found to be clinically acceptable, thereby permitting either one to be used in lieu of the Perkins Tonometer for measuring IOP.
In outreach community ophthalmology camp settings, where a large number of patients are to be screened within a short period of time, the NCT and Schiotz tonometer serve as acceptable devices. The results of our study support the use of Schiotz tonometer as a screening tool for elevated IOP in a community ophthalmology setting. In most outreach camps, a major part of the screening will be done by either the ophthalmology trainee or the optometrist due to resource and manpower constraints. The relative ease of use and the reasonable cost make the Schiotz tonometer a readily available screening tool for community screening programmes. Though, this tonometer needs repeated sterilization of the instrument tip with ether or sodium hypochlorite after each case, not much time is lost.
In this study, both the methods had a better correlation at <40 years age group. Change in CCT with age can affect IOP as measured by Perkin’s tonometer.17 Age-related changes in corneal resistance to applanation has also been documented and could have affected the IOP values in the >40 years age group.18 Our finding that NCT was found to be least accurate when CCT was greater than 600 μm is similar to the observation of Tonnu et al that the readings by NCT are far more affected by changes in CCT than those of GAT.19
The majority of patients who reported for the screening belong to the lower socioeconomic status. This is akin to the patient population catered to the public health institution in which this study was performed. Post-LASIK patient reporting is almost never seen. This has resulted with only subjects with corneal thickness close to normal being included in the study although no conscious decision was taken to make corneal thickness or post-LASIK as part of inclusion or exclusion criteria. Also, the role of refractive error on IOP measurements by different methods could not be analysed as most patients included were diagnosed with significant bilateral cataracts.20 The use of both eyes for analysis can result in a Type I error (rejecting a true null hypothesis) and can be minimized with the use of a mixed model approach.21 Also, during analysis the data were found to be slightly skewed, but, the sample size was large enough to follow a normal distribution for analysis.
Conclusion
Both the tonometers showed a significant correlation with the gold standard technique (Perkin’s applanation tonometer) over a range of IOP and CCT with the Schiotz tonometer performing better than the NCT. For early detection, it is recommended that those above the age of 40 years reporting to ophthalmic services be screened for glaucoma. Limitation of resources and poor access to specialized ophthalmic services may justify the use of the more economical Schiotz tonometer along with evaluation of the optic disc as the screening test for glaucoma. The high specificity seen with Schiotz tonometer in this study indicates that this tonometer can be recommended as a reliable screening tool in community outreach ophthalmology services. However, prudency demands that those patients with a provisional diagnosis of abnormal IOP must be further subjected to GAT, visual fields and examination of the optic nerve head for confirmation and follow-up.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Stevens G.A., White R.A., Flaxman S.R., Price H., Jonas J.B., Keeffe J. Vision Loss Expert Group. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990–2010. Ophthalmology. 2013;120:2377–2384. doi: 10.1016/j.ophtha.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 2.Vijaya L., George R., Paul P.G., Baskaran M., Arvind H., Raju P. Prevalence of open-angle glaucoma in a rural south Indian population. Invest Ophthalmol Vis Sci. 2005;46:4461–4467. doi: 10.1167/iovs.04-1529. [DOI] [PubMed] [Google Scholar]
- 3.Quyang P.B., Li C.Y., Zhu X.H., Duan X.C. Assessment of intraocular pressure measured by Reichert ocular response analyzer, Goldmann applanation tonometry, and dynamic contour tonometry in healthy individuals. Int J Ophthalmol. 2012;5:102–107. doi: 10.3980/j.issn.2222-3959.2012.01.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medeiros F.A., Alencar L.M., Sample P.A., Zangwill L.M., Susanna R., Jr., Weinreb R.N. The relationship between intraocular pressure reduction and rates of progressive visual field loss in eyes with optic disc hemorrhage. Ophthalmology. 2010;117:2061–2066. doi: 10.1016/j.ophtha.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Chui W.S., Lam A., Chen D., Chiu R. The influence of corneal properties on rebound tonometry. Ophthalmology. 2008;115:80–84. doi: 10.1016/j.ophtha.2007.03.061. [DOI] [PubMed] [Google Scholar]
- 6.Francis B.A., Hsieh A., Lai M.Y., Chopra V., Pena F., Azen S. Los Angeles Latino Eye Study Group; Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology. 2007;114:20–26. doi: 10.1016/j.ophtha.2006.06.047. [DOI] [PubMed] [Google Scholar]
- 7.Whitacre M.M., Stein R. Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol. 1993;38:1–30. doi: 10.1016/0039-6257(93)90053-a. [DOI] [PubMed] [Google Scholar]
- 8.Doughty M.J., Zaman M.L. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000;44:367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 9.Hagishima M., Kamiya K., Fujimura F., Morita, Shoji N., Shimizu K. Effect of corneal astigmatism on intraocular pressure measurement using ocular response analyzer and Goldmann applanation tonometer. Graefes Arch Clin Exp Ophthalmol. 2010;248:257–262. doi: 10.1007/s00417-009-1202-7. [DOI] [PubMed] [Google Scholar]
- 10.Whitacre M.M., Stein R.A., Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993;115:592–596. doi: 10.1016/s0002-9394(14)71455-2. [DOI] [PubMed] [Google Scholar]
- 11.Walia J.S., Chronister C.L. Possible iatrogenic transmission of Creutzfeldt-Jakob disease via tonometer tips: a review of the literature. Optometry. 2001;72:649–652. [PubMed] [Google Scholar]
- 12.Tonnu P.A., Ho T., Sharma K., White E., Bunce C., Garway-Heath D. A comparison of four methods of tonometry: method agreement and interobserver variability. Br J Ophthalmol. 2005;89:847–850. doi: 10.1136/bjo.2004.056614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel H., Gilmartin B., Cubbidge R.P., Logan N.S. In vivo measurement of regional variation in anterior scleral resistance to Schiotz indentation. Ophthalmic Physiol Opt. 2011;31:437–443. doi: 10.1111/j.1475-1313.2011.00840.x. [DOI] [PubMed] [Google Scholar]
- 14.Krieglstein G.K., Waller W.K. Goldmann applanation versus hand-applanation and schiotz indentation tonometry. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975;194:11–16. doi: 10.1007/BF00408271. [DOI] [PubMed] [Google Scholar]
- 15.Chiara G.F., Semes L.P., Potter J.W., Cutter G.R., Tucker W.R. Portable tonometers: a clinical comparison of applanation and indentation device. J Am Optom Assoc. 1989;60:105–110. [PubMed] [Google Scholar]
- 16.Bland J.M., Altman D.G. Measuring agreement in method comparison studies. Stat Meth Med Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 17.Vijaya L., George R., Arvind H., Ve Ramesh S., Baskaran M., Raju P. Central corneal thickness in adult South Indians: the Chennai Glaucoma Study. Ophthalmology. 2010;117:700–704. doi: 10.1016/j.ophtha.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Malik N.S., Moss S.J., Ahmed N., Furth A.J., Wall R.S., Meek K.M. Ageing of the human corneal stroma: structural and biochemical changes. Biochim Biophys Acta. 1992;1138:222–228. doi: 10.1016/0925-4439(92)90041-k. [DOI] [PubMed] [Google Scholar]
- 19.Tonnu P.A., Ho T., Newson T., El Sheikh A., Sharma K., White E. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. Br J Ophthalmol. 2005;89:851–854. doi: 10.1136/bjo.2004.056622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Del Buey M.A., Lavilla L., Ascaso F.J., Lanchares E., Huerva V., Cristóbal J.A. Assessment of corneal biomechanical properties and intraocular pressure in myopic spanish healthy population. J Ophthalmol. 2014;2014:905129. doi: 10.1155/2014/905129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barleon L., Hoffmann E.M., Berres M., Pfeiffer N., Grus F.H. Comparison of dynamic contour tonometry and Goldmann applanation tonometry in glaucoma patients and healthy subjects. Am J Ophthalmol. 2006;142:583–590. doi: 10.1016/j.ajo.2006.05.030. [DOI] [PubMed] [Google Scholar]