Abstract
Our report describes an unusual radiological presentation of optic nerve sheath meningioma. The classic radiological appearance of optic nerve thickening with enhancement and calcification within the tumor was not seen; instead, an elongating gadolinium enhancing band-like area adjacent to the superomedial aspect of the left optic nerve sheath was identified. The diagnosis was confirmed on histopathology. Our report adds to the spectrum of presentations of this relatively common clinical entity.
Keywords: Optic nerve sheath meningioma, Radiology, MRI, Histopathology
Introduction
Optic nerve sheath meningiomas (ONSM) account for 2% of all orbital tumors.1 They are the second most common optic nerve tumor after gliomas and represent 1–2% of all meningiomas.2, 3 Without treatment, continued growth of ONSM results in progressive loss of visual acuity, color blindness and eventually complete loss of vision.1 No tumor-related deaths have been reported.3 Radiological findings are usually of an enlarged optic canal, optic nerve thickening and enhancement and calcification within the tumor.2 Definitive treatment of ONSM is controversial. Fractionated radiotherapy is often first choice in an attempt to control the ONSM growth rate and to preserve vision if the diagnosis is not in question.3 Surgery remains best-treatment in cases with blindness, severe proptosis and in patients with intracranial extension.3
Case report
A 57-year-old female doctor presented with a 1-year history of blurred vision and visual field changes in her left eye. She had a history of a pituitary adenoma 30 years previously, treated by open craniotomy and post-operative radiotherapy (4200 rad over 20 treatments). She was otherwise well.
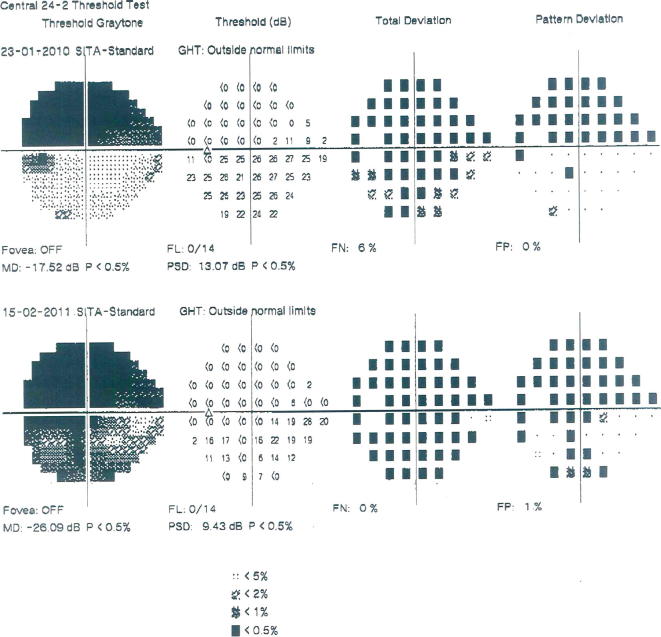
Examination revealed visual acuity of 20/17 on the right and 20/120 on the left. There was left relative afferent pupillary defect and left sided brightness desaturation. No proptosis was noted and the patient had a full range of ocular movements. Anterior segment examination was unremarkable, while fundal examination showed disk pallor of the left optic nerve head without disk swelling. There was progression of inferior visual field loss (Humphrey Field Analyzer; Zeiss, Germany) between January 2010 and February 2011 as shown in Fig. 1.
Figure 1.
Humphrey visual field of the left eye. Clear progression is visible with inferior visual field involvement over a year.
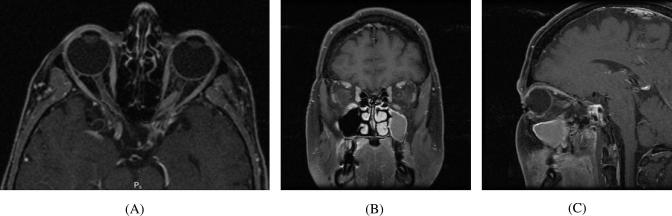
A Magnetic Resonance (MR) scan of the brain and orbits was performed (Fig. 2), which showed an elongating gadolinium enhancing band-like area adjacent to the superomedial aspect of the left optic nerve sheath measuring 13.4 × 3.5 mm, compressing and displacing the optic nerve inferolaterally. The optic nerve did not appear to be involved. The mass extended posteriorly to the level of the optic foramen. A cerebral angiogram was performed, which did not show a carotid cavernous fistula or aneurysms. The differential diagnosis was an ONSM, a diffuse glioma of the optic nerve, or less likely, an atypical recurrence of pituitary adenoma.
Figure 2.
T1 weighted magnetic resonance image with gadolinium enhancement of the optic nerve sheath meningioma (A) transverse view, (B) coronal view and (C) sagittal view. Note the elongating gadolinium enhancing band-like area adjacent to the superomedial aspect of the left optic nerve sheath compressing and displacing the optic nerve inferolaterally.
With her previous history of pituitary adenoma with radiation treatment, progressing symptoms and the uncertainty of the diagnosis, the patient expressed a strong preference for surgical exploration and removal of the lesion with division of the optic nerve rather than further radiation therapy. She was aware that surgical exploration would leave her with no light perception vision post-operatively.
A stereotactically guided resection of tumor was performed through an orbitozygomatic craniotomy. The left frontal lobe was gently retracted to expose the superior orbit. The roof of the orbit was decompressed to 6 mm anterior to the optic canal. After opening the periorbita and exposing the muscle cone, the supraorbital nerve was mobilized laterally. The optic nerve was localized behind the globe and the optic nerve was full inside the dura. A band-like structure was not identified; instead, a macroscopically normal-looking nerve was found surrounded by soft red/brown material. Resection of the optic nerve over a 16 mm distance was performed and sent for histopathology.
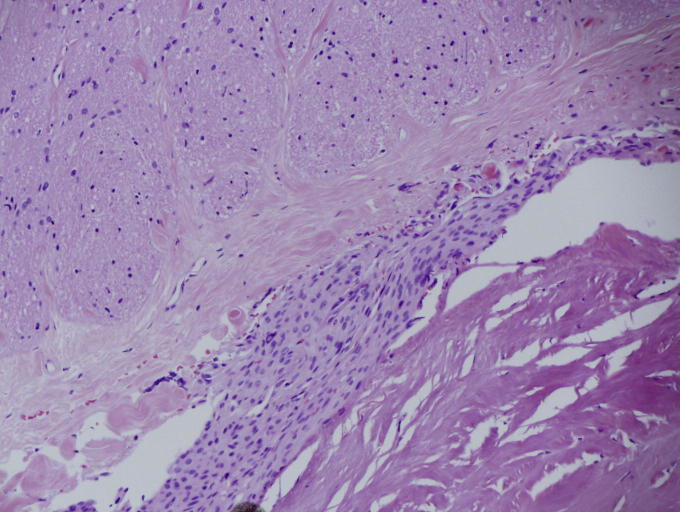
Histopathology (Fig. 3) showed fibrous thickening of the dura and arachnoid around the nerve with large collections of meningiothelial cells between the two layers with occasional psammoma bodies within the cellular collections. The meningiothelial cells show immunoperoxidase staining for progesterone receptors with a negligible proliferation rate with virtually no staining for Ki67. Taken altogether, this was consistent with an ONSM. No invasion of the optic nerve was noted. No subdural involvement of the meningioma was seen at either end of the nerve segment. Thus far, the patient has been followed up over a 12 month period and is recovering well.
Figure 3.
Histological appearance of the optic nerve sheath meningioma. The meningiothelial cells do not invade the pial/arachnoid tissue. (Hematoxylin and eosin stain.)
Discussion
Our case demonstrated unusual radiological features of a histologically confirmed ONSM. The largest case series on record of ONSM describes five radiological patterns commonly encountered.2 The commonest pattern identified was tubular (62% of cases), with subgroups of diffuse (45%), apical expansion (15%) and anterior expansion (3%), which had minimal widening of the optic nerve and more frequent evidence of calcification.2 The second group was globular tumors (23%) where growth was outside the dural sheath causing significant proptosis. 11% displayed a fusiform pattern and 4% had a focal enlargement of the optic nerve.2 The radiological appearance of the ONSM in our case did not conform to any of the known patterns; rather, it appeared as a distinct band-like structure that displaced the optic nerve.
Previous ionizing radiation is a known cause of ONSM.4, 5 Such secondary meningiomas tend to present at a younger age, present with multiple lesions commonly arising from the sphenoid ridge, tuberculum sellae or olfactory groove and demonstrate a higher recurrence rate.4, 6, 7 Histopathology also suggests that they tend to be more aggressive, with a higher tendency toward malignancy in patients who had high nose radiation therapy.4, 8 This knowledge played a role in the decision made by our well-informed patient.
Canalicular ONSM can often pose a diagnostic challenge for clinicians as very small lesions can compress the optic nerve and cause significant and progressive visual symptoms because the bony canal walls limit expansion. Reports have shown diagnostic delays of greater than 1 year due to this variability in radiological appearance.4 It is strongly recommended that all cases of progressive visual loss be investigated by high-spatial-resolution MR of the orbit before and after contrast enhancement in combination with fat suppression.4, 5
Recent literature reviews support the safety of fractionated radiotherapy in the treatment of ONSM.2, 3
Patient consent
The patient has consented to the submission of the case report for submission to the journal.
Conflict of interests and source of funding
The authors declared that there is no conflict of interest or funding source for any authors.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Wright J., McNab A., McDonald W. Primary optic nerve sheath meningioma. Br J Ophthalmol. 1989;73:7. doi: 10.1136/bjo.73.12.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saeed P., Rootman J., Nugent R. Optic nerve sheath meningiomas. Ophthalmology. 2003;110:12. doi: 10.1016/S0161-6420(03)00787-5. [DOI] [PubMed] [Google Scholar]
- 3.Pacelli R., Cella L., Conson M., Tranfa F., Strianese D., Liuzzi R. Fractionated stereotactic radiation therapy for orbital optic never sheath meningioma – a single institution experience and a short review of the literature. J Radiat Res. 2011;52:6. doi: 10.1269/jrr.10139. [DOI] [PubMed] [Google Scholar]
- 4.Mansouri A., Badhiwala J., Mansouri S., Zadeh G. The evolving role of radiosurgery in the management of radiation-induced meningiomas: a review of current advances and future directions. BioMed Res Int. 2014;2014:107526. doi: 10.1155/2014/107526. PubMed PMID: 25136551. Pubmed Central PMCID: 4124844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shenoy S.N., Munish K.G., Raja A. High dose radiation induced meningioma. Br J Neurosurg. 2004 Dec;18(6):617–621. doi: 10.1080/02688690400022789. PubMed PMID: 15799195. [DOI] [PubMed] [Google Scholar]
- 6.Kondziolka D., Kano H., Kanaan H., Madhok R., Mathieu D., Flickinger J.C. Stereotactic radiosurgery for radiation-induced meningiomas. Neurosurgery. 2009;64(3):463–469. doi: 10.1227/01.NEU.0000336765.85922.D9. discussion 9-70. PubMed PMID: 19240608. [DOI] [PubMed] [Google Scholar]
- 7.Miller N.R. Primary tumours of the optic nerve and its sheath. Eye (London, England) 2004;18(11):1026–1037. doi: 10.1038/sj.eye.6701592. PubMed PMID: 15534587. [DOI] [PubMed] [Google Scholar]
- 8.Sadetzki S., Flint-Richter P., Ben-Tal T., Nass D. Radiation-induced meningioma: a descriptive study of 253 cases. J Neurosurg. 2002;97(5):1078–1082. doi: 10.3171/jns.2002.97.5.1078. PubMed PMID: 12450029. [DOI] [PubMed] [Google Scholar]