Abstract
Introduction
Pharmacy is a very dynamic profession and the role of the pharmacist is improving with the expansion of the scope of services and the introduction of new subspecialties over time. Moving from being medication dispensers to outcome-oriented and patient-focused care providers; pharmacists will carry more responsibility and commitment to improve their knowledge and practice.
Being updated and evidence-based is a key tool to achieve effective pharmaceutical care services. The primary purpose of this article is to highlight the concept of “evidence based pharmaceutical care” as professional practice to improve the quality of pharmaceutical care.
Methods
Literature for relevant evidence was searched by Medline (through PubMed), Cochrane library using the keywords: pharmaceutical care, evidence-based and pharmacy practice. Also a manual search through major journals for articles referenced in those located through PubMed was done.
Results and discussion
There is strong data showing that pharmaceutical care lead to improvement in health outcomes and cost-effective therapy. More efforts, policies and qualified staff are needed to establish the “evidence-based pharmaceutical care” as new daily professional practice. Evidence to support pharmacists in their emerging role as care providers is available to improve the efficacy and quality of pharmaceutical care. Education and specialized training practicing evidence based approach are vital to prepare pharmacists to provide high quality pharmaceutical care.
Conclusion
As care providers, pharmacists are effective in providing high quality patient care and being members in multidisciplinary clinical teams is needed to give them the opportunity. Evidence based pharmaceutical care is a natural and logical emerging concept in the modern pharmacy practice to achieve high quality and more effective pharmaceutical care but still more efforts and resources are needed to promote new attitude toward more professional career.
Keywords: Evidence-based pharmacy, Patient care, Pharmacist, Pharmaceutical care, Pharmacy practice
1. Introduction
Personal experience or expert opinion alone is not enough to support health care decision. High quality research is the most accurate source of scientific evidence that can be used to identify and meet the patient health needs. In a recent survey of pharmacists, 90% held positive attitudes toward evidence based practice and 84% thought research findings were important to daily practice (Burkiewicz and Zgarrick, 2005). These results reflect the awareness of the pharmacists toward their profession as evidence-based practice and the desire to expand their role as researchers.
Pharmacy profession has improved to include the provision of cognitive services in addition to the traditional role of medication dispensing. Establishing evidence-based practice is important for pharmaceutical care services to be effective, updated and relevant to patients. Pharmacists must accept and actively participate in the research needed to establish the required evidence-base pharmaceutical care.
1.1. What is “pharmaceutical care”?
According to the definition of Hepler & Strand pharmaceutical care is “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life” (Hepler and Strand, 1990). Pharmaceutical care is based on a relationship between the patient and the healthcare providers who accept responsibility to provide care to the patients. Pharmaceutical care involves the active participation of both the patient and the health care provider in drug therapy decisions.
Pharmaceutical care involves three major functions: identifying potential and actual drug related problems; resolving actual drug-related problems; and preventing drug related problems. Although there are different trends, such as clinical pharmacy services, cognitive services, medication management, medication review, they all share the same philosophy and objectives, namely “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life” (Roughead et al., 1990).
Pharmaceutical care activities include medication dispensing, providing drug information, patient counseling, drug monitoring, parenteral nutrition preparation, adverse drug reaction monitoring, medication reconciliation, drug protocol/guideline development, medical rounding with the health care team, and performing admission drug histories. Practicing these activities by evidence-based approach will improve the quality of the provided services.
Pharmacists need training and support to develop and improve their practical skills to provide comprehensive pharmaceutical care (Schommer and Cable, 1996).
To be effective, pharmaceutical care needs to be adopted by majority of pharmacists in their daily work. Many barriers limit the implementation of the pharmaceutical care principles. To identify and solve these barriers well designed research is needed (Farris and Kirking, 1993a, Farris and Kirking, 1993b).
1.2. Evidence based practice
There is an increasing awareness of the need for healthcare professionals to adopt an evidence-based approach to their daily practice. Practicing pharmacy in an evidence based manner will enhance professional skills of the pharmacist with improved patient care. The concept of evidence-based pharmaceutical care requires training and education starting from undergraduate level. Pharmacy students need to be educated how to professionally apply science in patient care. Special training on research principles, literature review and evidence based approaches is very important to prepare the pharmacists to practice the evidence based pharmaceutical care efficiently.
2. Methods
A literature review was performed by searching Medline database through PubMed for relevant articles including meta-analyses, systematic reviews, review articles, randomized and non-randomized trials, as well as case reports. Search keywords were as follows: evidence-based pharmacy, patient care, pharmacist, pharmaceutical care, and pharmacy practice. Web-based searching and backward citation tracking were conducted for context and additional citations.
3. Results and discussion
3.1. Search results
There are strong data showing that pharmaceutical care is effective and led to improved patient care with more cost-effective therapy in both in- and outpatient settings. Many studies and reviews demonstrated the efficacy of the pharmaceutical care programs as described below. Research describing the term “evidence-based pharmaceutical care” is limited in the literature.
3.2. Data findings
3.2.1. Inpatient pharmaceutical care
The literature proving the beneficial role of the pharmacist in inpatient care is strong and abundant (Shekelle et al., 2013). A comprehensive systematic review of inpatient pharmacy services was conducted and summarized in a Technology Assessment report in 2013 by the Agency for Healthcare Research and Quality titled, “Making Healthcare Safer II: an Updated Critical Analysis of the Evidence for Patient Safety Practices”.
The report stated that the totality of the literature (delineated in evidence tables) shows that pharmacist-provided care enhances the patient safety and improves outcomes. Later in the report, they focus on medication reconciliation and found that pharmacists significantly decreased emergency department visits and hospitalizations within 30 days of discharge (Shekelle et al., 2013).
Services provided by pharmacists in hospitals were found to be highly cost-effective in a database analysis of 1016 hospitals (Bond et al., 2000). In all, 6 services significantly reduced costs, including drug use evaluation, drug information, adverse drug reaction monitoring, drug protocol/guideline development, medical rounding with the health care team, and performing admission drug histories. As staffing was increased for clinical pharmacists, total cost of care decreased (Bond et al., 2000).
3.2.2. Outpatient pharmaceutical care
In 2010, a comprehensive systematic review of 298 studies evaluating the impact of pharmacist-provided direct patient care in ambulatory settings found significant benefits in achieving hemoglobin A1c, LDL cholesterol, and blood pressure targets in addition to reducing adverse drug events (Chisolm-Burns et al., 2010). These intermediate health outcome benefits result from enhanced patient knowledge about medications, increased medication adherence, and improved quality of life as a result of pharmacist-provided services (Chisolm-Burns et al., 2010).
In a systematic review of 15 randomized controlled trials in 9111 outpatients with diabetes published in 2012, the use of pharmacist medication management, educational interventions, feedback to providers, and patient reminders had a significant effect on systolic blood pressure, diastolic blood pressure, total cholesterol, LDL cholesterol, and body mass index versus standard of care (Santschi et al., 2012).
Similar benefits were seen in a systematic review of hyperlipidemia patients treated by pharmacists, where markers of lipid control were markedly improved (Charrois et al., 2012). In July 2013, the impact of pharmacists, specifically on geriatric care, was assessed in a meta-analysis of 20 studies (Lee et al., 2013). Pharmacist-provided care resulted in significant improvements in hospitalizations, medication adherence, combined therapeutic outcomes (blood pressure, INRs, etc), and combined safety end points (falls, adverse events, and number of unnecessary drugs being used) (Lee et al., 2013).
3.2.3. Evidence-based pharmaceutical care
The concept “evidence-based pharmaceutical care” has been mentioned as a term in 2008 (Gaebelein and Gleason, 2008) and it has been defined in 2009 as ‘‘the responsible provision of evidence-based medication-related care for the purpose of achieving definite outcomes that improve patients’ quality of life” (Aburuz, 2015). EBPC evolves the application of the current best up to date pharmacy research to provide effective pharmaceutical services to patients. Like other health care disciplines, implementation of EBPC mainly involves four sequential steps (Weng et al., 2013): first, framing a clear question based on a clinical problem; second, searching for relevant evidence in the literature; third, critically appraising the validity of contemporary research; and fourth, applying the findings to clinical decision-making.
4. Discussion
From the literature review results it is clear that pharmaceutical care achieves a brilliant and innovative step in improving the pharmacy practice to be more professional and effective health care service. Changing practice from dispensing to care providing system requires major changes in education and training of the pharmacists that should be started early from undergraduate level and continues throughout their carrier.
Commitment and dedication of the pharmacists toward self improvement and professionalism should be enforced and encouraged since this will build up the future of the pharmacy practice.
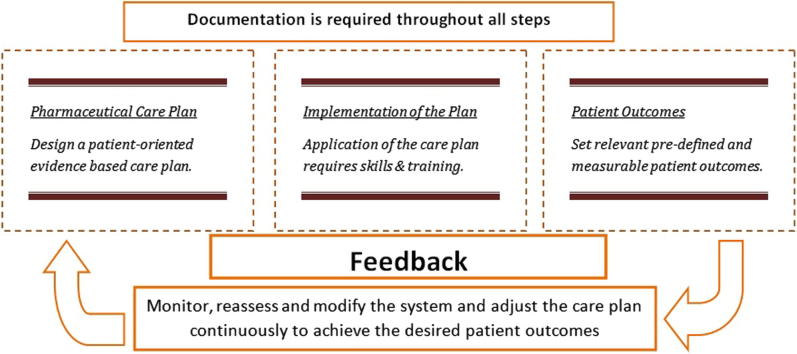
As any other health care discipline to be effective, pharmaceutical care needs to be evidence-based practice that is systemic, well organized and updated. Being systemic implies input, process and output. This flow will also be subjected to continuous corrections and modifications through feedback step (pharmacists need to measure and monitor their contribution to health care for the ultimate benefit of the patient). In order to ensure standards of practice, pharmacists must be willing to assess their knowledge and audit their practice to determine the effectiveness of their interventions.
Evidence-based pharmaceutical care is a dynamic daily practice that is updated according to new and emerging evidence of high quality research and this represents the feedback loop in this system.
To simplify the concept; pharmaceutical care services can be subdivided into direct services that are provided directly to the patient (ex. patient counseling) and indirect services like any other pharmacy service that eventually will help the patient (ex. therapeutic drug monitoring).
4.1. Example
In the anti-coagulation clinic the pharmacist is in direct contact with the patients who are treated with warfarin. Pharmacists are using written brochures to counsel the patients about the proper use of warfarin but during the routine patient satisfaction survey it had been noticed that some patients still do not understand the basic information regarding warfarin use.
Now we have identified the problem, the root cause analysis would be a good option or we can use the PICO method. The next step is to review the literature to figure out the best evidence based approach to be applied in order to achieve effective and convenient patient counseling. By literature search it was found that there is evidence suggesting that weekly scheduled phone consultations increased awareness regarding warfarin use and this resulted in decreased risk of hospitalization for an adverse event associated with anticoagulation (Ibrahim and Saber-Ayad, 2013). Consequently the pharmacy team decided to apply the weekly phone consultations as warfarin counseling tool in addition to the conventional written (warfarin booklet) educational brochures, and to follow the effect of the new counseling program on the proper usage and understanding of warfarin using patient satisfaction measurement tool. In this example evidence-based approach is used to provide pharmaceutical care to patient on warfarin.
Implementation of EBPC can improve the quality of the pharmaceutical care services and encourage the pharmacists to be involved in the health care systems as both practitionersc107 and researchers. Barriers to the implementation of the use of evidence in clinical decision-making can generally be summarized as problems in identifying, assessing, interpreting, and applying best evidence to practice.
Some potential barriers may hinder the implementation of an evidence base approach; these barriers can be categorized as personal or environmental factors. Personal factors include: Attitude and perception toward EBPC, time (due to a heavy clinical load), basic knowledge, skills in critical appraisal, skills in literature searching, clinical incorporation. Environmental factors are those barriers related to system adopted by the health institution like lack of support and reward, inadequate library and evidence based resources and lack of specialized training courses (Weng et al., 2013).
5. Conclusion
Health care interventions can no longer be based on opinion or individual experience alone. Scientific evidence, built up from good quality research, is used as a guide, and adapted to each individual patient’s circumstances. As a new innovative concept evidence-based pharmaceutical care seems promising practice to improve the quality of the pharmaceutical care. We encourage all health system pharmacists to adapt, disseminate and promote this new concept to improve the pharmacy profession. More focused studies are needed to establish and market this concept as a daily pharmacy practice.
Disclosure
The author declares no conflicts of interest.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aburuz S. The case for evidence-based pharmaceutical care. Res. Social Adm. Pharm. 2015;11(3):e146–e147. doi: 10.1016/j.sapharm.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Bond C.A., Raehl C., Franke T. Clinical pharmacy services, pharmacy staffing, and the total cost of care in the United States. Pharmacotherapy. 2000;20:609–621. doi: 10.1592/phco.20.7.609.35169. [DOI] [PubMed] [Google Scholar]
- Burkiewicz J.S., Zgarrick D.P. Evidence-based practice by pharmacists: utilization and barriers. Ann. Pharmacother. 2005;39(7–8):1214–1219. doi: 10.1345/aph.1E663. (Epub 2005, Jun 14.) [DOI] [PubMed] [Google Scholar]
- Charrois T.L., Zolezzi M., Koshman S.L. A systematic review of the evidence for pharmacist care of patients with dyslipidemia. Pharmacotherapy. 2012;32:222–233. doi: 10.1002/j.1875-9114.2012.01022.x. [DOI] [PubMed] [Google Scholar]
- Chisolm-Burns M.A., Lee J.K., Spivey C.A. US pharmacists’ effect as team members on patient care: systematic review and meta-analysis. Med. Care. 2010;48:923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- Farris K.B., Kirking D.M. Assessing the quality of pharmaceutical care I. One perspective of quality. Ann. Pharmacother. 1993;27:68–73. doi: 10.1177/106002809302700116. [DOI] [PubMed] [Google Scholar]
- Farris K.B., Kirking D.M. Assessing the quality of pharmaceutical care II. Application of concepts of quality assessment from medical care. Ann. Pharmacother. 1993;27:215–222. doi: 10.1177/106002809302700218. [DOI] [PubMed] [Google Scholar]
- Gaebelein C.J., Gleason B.L. first ed. Lippincott Williams & Wilkins; Philadelphia: 2008. Contemporary Drug Information: An Evidence-based Approach (In chapter 1) [Google Scholar]
- Hepler C.D., Strand L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Pharm. Educ. 1990;53(Suppl.):7S–15S. [PubMed] [Google Scholar]
- Ibrahim R., Saber-Ayad M. Continuous outpatient warfarin counseling and its effects on adherence. Asian J. Pharm. Clin. Res. 2013;6(2):101–104. [Google Scholar]
- Lee J., Slack M.K., Martin J., Ehrman C., Chisolm-Burns M. Geriatric patient care by US pharmacists in healthcare teams: systematic review and meta-analyses. J. Am. Geriatr. Soc. 2013;61:1119–1127. doi: 10.1111/jgs.12323. [DOI] [PubMed] [Google Scholar]
- Roughead L., Semple S., Vitry A. University South of Australia; Adelaide: 2002. The Value of Pharmacist Professional Services in the Community Setting. A Systematic Review of the Literature 1990–2002. [Google Scholar]
- Santschi V., Cholero A., Paradis G., Colosimo A.L., Burnand B. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes. Diabetes Care. 2012;35:2706–2717. doi: 10.2337/dc12-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schommer Jon C., Cable Gerald L. Current status of pharmaceutical care practice. Strategies for education. Am. J. Pharm. Educ. 1996;vol. 60 Spring. [Google Scholar]
- Shekelle, P.G., Wachter, R.M., Pronovost, P.J., et al., 2013. Making healthcare safer: II. An updated critical analysis of the evidence for patient safety practices. <http://www.ahrq.gov/research/findings/evidence-based-ports/ptsafetysum.pdf>. Accessed August 1. [PMC free article] [PubMed]
- Weng Y.H. Implementation of evidence-based practice across medical, nursing, pharmacological and allied healthcare professionals: a questionnaire survey in nationwide hospital settings. Implement. Sci. 2013;8:112. doi: 10.1186/1748-5908-8-112. [DOI] [PMC free article] [PubMed] [Google Scholar]