Abstract
Purpose
This prospective observational study aims to evaluate the accuracy of dead-space fraction derived from the ventilator volumetric capnography (volumetric CO2) or a prediction equation to predict the survival of mechanically ventilated patients with acute respiratory distress syndrome (ARDS).
Methods
Consecutive VD/VT measurements were obtained based upon a prediction equation validated by Frankenfield et al for dead-space ventilation fraction: VD/VT = 0.320 + 0.0106 (PaCO2-ETCO2) + 0.003 (RR) + 0.0015 (age) in adult patients who had infection-related severe pneumonia and were confirmed as having ARDS. Here PaCO2 is the arterial partial pressure of carbon dioxide in mmHg; ETCO2, the end-tidal carbon dioxide measurement in mmHg; RR, respiratory rate per minute; and age in years. Once the patient had intubation, positive end expiratory pressure was adjusted and after Phigh reached a steady state, VD/VT was measured and recorded as the data for the first day. VD/VT measurement was repeated on days 2, 3, 4, 5 and 6. Meanwhile we collected dead-space fraction directly from the ventilator volumetric CO2 and recorded it as Vd/Vt. We analyzed the changes in VD/VT and Vd/Vt over the 6-day period to determine their accuracy in predicting the survival of ARDS patients.
Results
Overall, 46 patients with ARDS met the inclusion criteria and 24 of them died. During the first 6 days of intubation, VD/VT was significantly higher in nonsurvivors on day 4 (0.70 ± 0.01 vs 0.57 ± 0.01), day 5 (0.73 ± 0.01 vs. 0.54 ± 0.01), and day 6 (0.73 ± 0.02 vs. 0.54 ± 0.01) (all p = 0.000). Vd/Vt showed no significant difference on days 1–4 but it was much higher in nonsurvivors on day 5 (0.45 ± 0.04 vs. 0.41 ± 0.06) and day 6 (0.47 ± 0.05 vs. 0.40 ± 0.03) (both p = 0.008). VD/VT on the fourth day was more accurate to predict survival than Vd/Vt. The area under the receiver-operating characteristic curve for VD/VT and Vd/Vt in evaluating ARDS patients survival was day 4 (0.974 ± 0.093 vs. 0.701 ± 0.023, p = 0.0024) with the 95% confidence interval being 0.857–0.999 vs. 0.525–0.841.
Conclusion
Compared with Vd/Vt derived from ventilator volumetric CO2, VD/VT on day 4 calculated by Frankenfield et al's equation can more accurately predict the survival of ARDS patients.
Keywords: Respiratory distress syndrome, adult; Respiration, artificial; Pulmonary dead-space fraction; Survival; Volumetric capnography
Introduction
Acute respiratory distress syndrome (ARDS) is a life-threatening condition, which presents as progressive hypoxemia and difficulty in breathing following diffuse pulmonary interstitial and alveolar edema due to pulmonary capillary endothelial cell damage. Patients with ARDS are often critical and accompanied by other diseases or major injuries, for example, severe infection, shock, trauma and burns, etc.1 Although medical rescue is enhancing unceasingly, the mortality rate of critical patients has not been greatly decreased. Previous studies have shown the importance of physiologic dead space and its evolution in predicting mortality in critical patients.2, 3, 4, 5, 6 In clinical practice, we can directly read pulmonary dead-space fraction on the ventilator screen (in this study we recorded it as Vd/Vt), which may change a lot and sometimes contradictory or nonsensitive due to numerous interference factors, including high positive end-expiratory pressure (PEEP), administration of sedatives or muscle relaxants, etc. Therefore its accuracy to predict survival should be studied further. The equation VD/VT = 0.320 + 0.0106 (PaCO2-ETCO2) + 0.003 (RR) + 0.0015 (Age) proposed by Frankenfield et al7 (in this study we recorded it as VD/VT) has been shown to calculate pulmonary dead-space fraction precisely and without bias, eliminating the abovementioned disturbing factors. In this study, we compared VD/VT with Vd/Vt to evaluate their prediction accuracy of survival of ARDS patients.
Methods
Patient selection
This was a prospective observational cohort study conducted in the intensive care unit (ICU) of Tianjin Third Central Hospital, Tianjin, China. All the protocols have been approved by the Institutional Committee on Human Research, and informed consents have been obtained from the patients or their relatives. All patients with ARDS admitted to the adult ICU of our hospital between January 2014 and January 2015 were eligible for this study. Inclusion criteria were adult patients (≥18 years old) who were diagnosed as having ARDS based on the Berlin Definition for ARDS8 and required positive pressure mechanical ventilation via an endotracheal tube. Vd/Vt was directly read from the Dräger XL ventilator (Dräger Medical, Germany) volumetric CO2. Patients were excluded if they have pulmonary thromboembolism (PTE), history of chronic obstructive pulmonary disease (COPD), bronchiectasis or interstitial lung disease. Of 58 patients with ARDS, 46 were included in this study.
Clinical data collection
Baseline characteristics, demographic data and relevant physiologic data were recorded on the first day of study (defined as the moment when PEEP has been well adjusted and Phigh reached a steady state after intubation). Acute physiology and chronic health evaluation (APACHE) II score and lung-injury score at the time of enrollment were calculated. The primary etiology of ARDS was assessed based on a detailed review of the clinical history. Finally, we recorded the information about the survival condition of patients within 28 days.
Measurement of dead-space fraction
Initial VD/VT measurements were obtained on the first day. VD/VT was serially measured on days 2, 3, 4, 5 and 6 following the equation: VD/VT = 0.320 + 0.0106 (PaCO2-ETCO2) + 0.003 (RR) + 0.0015 (Age). At the same time, we recorded Vd/Vt directly from breath-by-breath volumetric CO2. We also recorded the arterial blood gas values, PaO2/FiO2, PEEP and FiO2. Breath-by-breath volumetric CO2 and analysis of ETCO2 were obtained by the mainstream CO2 sensor of a Dräger XL ventilator based on the non-dispersive infrared absorption principle. The machine was placed between the ventilator circuit and the patient. Measurement of dead-space fraction was conducted at the same time of arterial blood sampling, which was analyzed by a Radiometer ABL800 arterial blood gas analyzer (Radiometer, Bronshøj, Denmark). Modality of mechanical ventilation of all patients were bilevel positive airway pressure. Data were read when the patient were observed to be calm with complete respiratory rhythm.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (Version 17.0, SPSS Inc, Chicago, Illinois, USA) and Med Calc statistical software (V.15.6.1). Parametric and nonparametric values were expressed as mean ± SEM, and distance between median and quartile respectively. Comparison of sampled ratios were explored by using χ2 test. Student t test were used to compare mean values. Paired comparisons were conducted by using the Mann-Whitney test. Receiver operating characteristic (ROC) curves were obtained for the prognostic value of VD/VT and Vd/Vt, respectively. The area under the ROC curves of VD/VT and Vd/Vt were compared with Med Calc statistical software. A simple Pearson correlation was used to compare the relation of VD/VT to PEEP and PaO2/FiO2. A logistic regression was used to determine the association of VD/VT with mortality as the outcome. All tests were two sided and considered significant at p < 0.05.
Results
Baseline characteristics
A total of 46 patients with ARDS were enrolled in this study, including 18 females and 28 males with the mean age of (55.71 ± 3.01) years. Etiology of ARDS was pneumonia in 26 patients (57%), sepsis in 12 (25%), aspiration in 4 (9%) and trauma or others in 4 (9%). Of the 46 patients enrolled, 24 (52%) died and 22 (48%) survived. The demographics data, APACHE II score and lung-injury score are summarized in Table 1. Differences in PEEP and PaO2/FiO2 are summarized in Table 2. In this study, PEEP and FiO2 were adjusted based upon a target PaO2 ≥ 60 mmHg and low tidal volume. PEEP showed no significant difference at the first 5 days, but it was much lower in survivors on day 6 (9.2 ± 0.10 vs. 14.3 ± 0.08, p < 0.001). PaO2/FiO2 was significantly higher among survivors on day 4 (273 ± 11 vs. 182 ± 56), day 5 (289 ± 20 vs. 172 ± 15) and day 6 (305 ± 29 vs. 174 ± 40, p = 0.000 for all).
Table 1.
Baseline data and clinical characteristics of 46 patients (mean ± SEM).
| Group | Age (yr) | Female percentage | APACHE II score | Lung-injury score |
|---|---|---|---|---|
| Survivors (n = 22) | 43.84 ± 3.35 | 32% | 25 ± 0.5 | 2.60 ± 0.7 |
| Non-survivor (n = 24) | 66.59 ± 2.94 | 45% | 28 ± 0.4 | 2.7 ± 0.6 |
| Examining value | t = −3.342 | χ2 = 0.947 | U = −2.846 | U = −1.78 |
| p value | 0.003 | 0.378 | 0.004 | 0.076 |
Table 2.
Differences in PEEP and PaO2/FiO2 during the first 6 days between survivors (n = 22) and nonsurvivors (n = 24).
| Physiologic variables | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 |
|---|---|---|---|---|---|---|
| PEEP (cmH2O) | ||||||
| S | 12.3 ± 0.06 | 11.6 ± 0.04 | 12.8 ± 0.12 | 11.8 ± 0.14 | 10.9 ± 0.04 | 10.2 ± 0.10 |
| NS | 12.4 ± 0.06 | 12.6 ± 0.06 | 13.2 ± 0.12 | 13.8 ± 0.09 | 13.3 ± 0.10 | 15.3 ± 0.08 |
| U | −0.16 | −1.53 | −1.13 | −1.77 | −1.63 | −5.50 |
| P | 0.875 | 0.127 | 0.261 | 0.077 | 0.104 | <0.001 |
| PaO2/FiO2(mmHg) | ||||||
| S | 166 ± 13 | 172 ± 26 | 171 ± 16 | 273 ± 11 | 289 ± 20 | 305 ± 29 |
| NS | 157 ± 21 | 161 ± 10 | 169 ± 22 | 182 ± 56 | 172 ± 15 | 174 ± 40 |
| U | −1.22 | −1.706 | −0.76 | −5.62 | −5.77 | −5.81 |
| P | 0.222 | 0.088 | 0.448 | 0.000 | 0.000 | 0.000 |
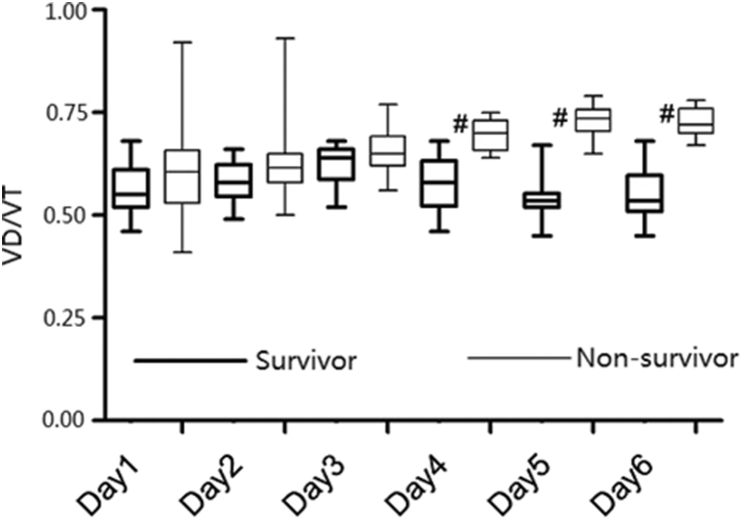
Comparison of VD/VT and Vd/Vt between survivors and nonsurvivors
The mean VD/VT was significantly higher in nonsurvivors than in survivors from the fourth day of mechanical ventilation (p < 0.05, Fig. 1). As for Vd/Vt, nonsurvivors had a slightly higher mean value (0.40–0.47). However, the difference between two groups was significant only on day 5 and day 6. During the whole study period (6 days of mechanical ventilation), the mean Vd/Vt for all the patients was consistently lower than 0.5 (Fig. 2).
Fig. 1.
Changes of VD/VT during the first 6 days of intubation. #p < 0.001 represents the significant differences between survivors and nonsurvivors on the same day.
Fig. 2.
Changes of Vd/Vt during the first 6 days of intubation. *p < 0.05 represents the significant differences between survivors and nonsurvivors on the same day.
ROC curves for the prognosis of patients
The mean VD/VT was significantly higher in nonsurvivors than in survivors from the fourth day of mechanical ventilation. So VD/VT and Vd/Vt on the fourth day as a survival predictor of ARDS patients was compared using the area under the ROC curve, which showed a much larger area of VD/VT (0.974 ± 0.093, 95% CI: 0.857–0.999) than that of Vd/Vt (0.701 ± 0.023, 95% CI: 0.525–0.841) (Z = 3.302, p = 0.0024). Therefore, VD/VT calculated by Frankenfield et al's prediction formula has a higher prognostic value of patients with ARDS on the fourth day.
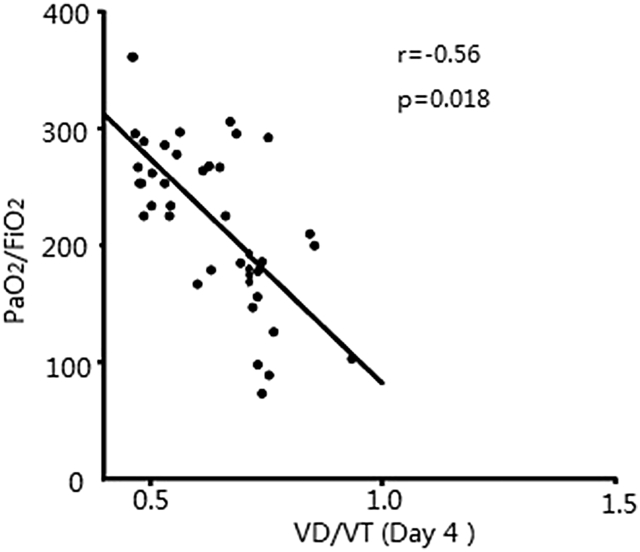
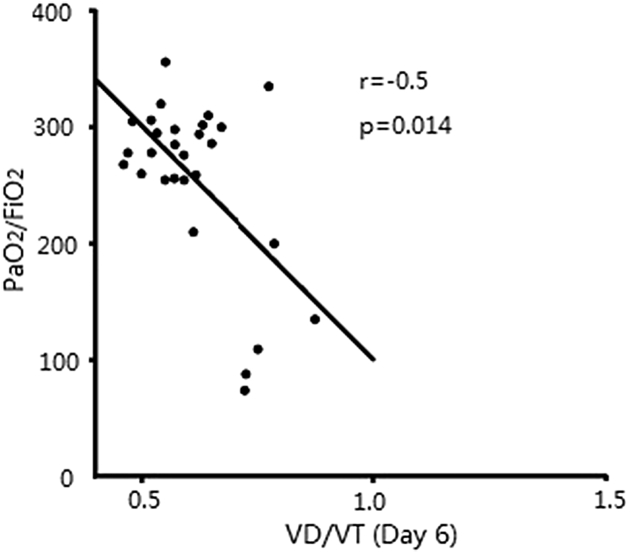
Correlation analysis between VD/VT and PEEP & PaO2/FiO2
VD/VT has no correlation with PEEP in statistics at the study period of mechanical ventilation (p > 0.05). At the first three days, there was no correlation between VD/VT and PaO2/FiO2 neither, but they were positively related on day 4 (r = −0.56, p = 0.018), day 5 (r = −0.58, p = 0.01), and day 6 (r = −0.50, p = 0.014). Statistic analysis was shown in Fig. 3, Fig. 4, Fig. 5.
Fig. 3.
Scatter plot of VD/VT and PaO2/FiO2 on day 4. There was statistically significant correlation between VD/VT and PaO2/FiO2.
Fig. 4.
Scatter plot of VD/VT and PaO2/FiO2 on day 5. There was statistically significant correlation between VD/VT and PaO2/FiO2.
Fig. 5.
Scatter plot of VD/VT and PaO2/FiO2 on day 6. There was statistically significant correlation between VD/VT and PaO2/FiO2.
The strength analysis of association between VD/VT and mortality
In the analysis of correlation between VD/VT and mortality, the odds ratio (OR) was calculated for every increase of 0.05 in VD/VT. The ORs for death in the unadjusted logistic regression model were statistical significant from day 4. They were still consistently >2.55 after the combined analysis of age, PaO2/FiO2, and APACHE II score. Moreover we found that age and APACHE II score were independent death risk factors (p < 0.05). PaO2/FiO2 in the adjusted logistic regression model reached statistic significance on days 4, 5 and 6. Because significant difference of VD/VT between survivors and nonsurvivors appeared on the fourth day, we only list detailed data on days 4, 5, and 6 in Table 3.
Table 3.
Unadjusted and adjusted logistic analyses of VD/VT and mortality on days 4, 5 and 6.
| Day 4 |
Day 5 |
Day 6 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Unadjusted model | |||||||||
| VD/VT | 3.06 | 1.77–5.3 | 0.000 | 3.23 | 1.82–5.61 | 0.000 | 5.37 | 1.83–15.69 | 0.002 |
| Adjusted model | |||||||||
| VD/VT | 2.82 | 1.35–5.88 | 0.006 | 3.02 | 1.63–5.29 | 0.028 | 5.52 | 1.16–26.22 | 0.031 |
| PaO2/FiO2 | 0.98 | 0.97–1 | 0.044 | 0.97 | 0.96–1.00 | 0.034 | 0.97 | 0.94–1.003 | 0.037 |
| Age | 1.08 | 1.01–1.16 | 0.025 | 1.07 | 0.98–1.16 | 0.086 | 1.07 | 0.99–1.16 | 0.087 |
| APACHE II score | 2.18 | 1.19–3.98 | 0.011 | 2.23 | 1.15–4.08 | 0.013 | 2.55 | 1.09–5.94 | 0.03 |
Discussion
Pulmonary dead-space ventilation i.e. the tidal volume that does not participate in gas exchange was first described and calculated by the Bohr equation in 1891. Later the Bohr's formula was simplified as dead-space fraction = (PACO2 − P CO2)/PACO2, where PACO2 represents the mean alveolar partial pressure of CO2 during expiration9 and P CO2 is defined as mixed expired partial pressures of CO2. In 1938, Bohr equation was modified by Enghoff. Physiologic dead-space fraction is consisted of anatomic or airway dead space and alveolar dead space.10, 11
Recently, due to the advanced technology, the ratio of physiologic dead space to tidal volume can be obtained directly by using forced expiratory volumetric CO2 concentration. The Dräger XL ventilator is equipped with integrated CO2 sensor and has this capability. ARDS patients were clinically managed with lung-protective ventilation and sufficient lung recruitment maneuvers. For example, ARDS patients received a high PEEP and low tidal volume ventilation, and some of them were injected sedative drugs or muscle relaxants. In this condition, patients cannot breathe evenly or reach forced respiration, resulting in inaccurate measurement of ETCO2. Therefore, the concentration curve of expiratory volumetric CO2 may have poor stability. In this study, VD/VT has a much larger areas under the ROC curve than Vd/Vt as a survival predictor on the fourth day. The result indicates that Vd/Vt may be highly variable or nonsensitive. As a result, Vd/Vt, when applied to evaluate clinical therapeutic effect and prognosis of patients, may be unreliable.
The prediction equation constructed by Frankenfield DC et al7 for dead space fraction has been proved to be capable of avoiding the abovementioned disturbances. In fact, most pioneering studies have found that the dead space fraction can reliably predict the threshold values for prognosis (i.e. >60%).2, 3, 4, 6, 12, 13, 14 However, we found that the mean Vd/Vt among survivors was volatile and consistently <0.50. From a clinical viewpoint, Vd/Vt may mislead clinicians to make inaccurate judgment. Our result indicates that VD/VT has a greater value in predicting the survival of ARDS patients than Vd/Vt. But our study is potentially limited by its relatively small size, thus requiring a larger sample clinical research for further study.
In our study, VD/VT has no correlation with PEEP during the first 6 days of ARDS. In ARDS, PEEP has a bidirectional variable influence on VD/VT: alveolar recruitment decreases dead-space while alveolar over-distension increases it.15 It is hard to predict the effect of PEEP because both phenomena may occur at the same time. We designed the research based on previous studies and showed prognostic value of pulmonary dead-space fraction among ARDS patients by the strength analysis of relationship between VD/VT and mortality. At present, PaO2/FiO2 and APACHE II score have been proved to be capable of predicting mortality in ARDS patients. But because of numerous interference factors, PaO2/FiO2 and APACHE II score alone can not be treated as a prognostic indicator. Complications and extrapulmonary organ failure also have important influence on the prognosis of patients with ARDS.
This study is a further confirmation and supplement of Robert et al's result.16 In conclusion, on the fourth day of mechanical ventilation for patients with ARDS, compared with Vd/Vt derived from ventilator volumetric CO2, VD/VT calculated by a prediction equation constructed by Frankenfield et al7 is more accurate to estimate patients' survival.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Fukuda Y. Acute lung injury/acute respiratory distress syndrome: progress in diagnosis and treatment. Topics: I. Pathogenesis and pathophysiology: 4. Pathophysiology and histopathology of ALI/ARDS. Nihon Naika Gakkai Zasshi. 2011;100:1536–1540. doi: 10.2169/naika.100.1536. [DOI] [PubMed] [Google Scholar]
- 2.Nuckton T.J., Alonso J.A., Kallet R.H. Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med. 2002;346:1281–1286. doi: 10.1056/NEJMoa012835. [DOI] [PubMed] [Google Scholar]
- 3.Kallet R.H., Alonso J.A., Pittet J.F. Prognostic value of the pulmonary dead-space fraction during the first 6 days of acute respiratory distress syndrome. Respir Care. 2004;49:1008–1014. [PubMed] [Google Scholar]
- 4.Cepkova M., Kapur V., Ren X. Pulmonary dead space fraction and pulmonary artery systolic pressure as early predictors of clinical outcome in acute lung injury. Chest. 2007;132:836–842. doi: 10.1378/chest.07-0409. [DOI] [PubMed] [Google Scholar]
- 5.Phua J., Badia J.R., Adhikari N.K. Has mortality from acute respiratory distress syndrome decreased over time?: a systematic review. Am J Respir Crit Care Med. 2009;179:220–227. doi: 10.1164/rccm.200805-722OC. [DOI] [PubMed] [Google Scholar]
- 6.Raurich J.M., Vilar M., Colomar A. Prognostic value of the pulmonary dead-space fraction during the early and intermediate phases of acute respiratory distress syndrome. Respir Care. 2010;55:282–287. [PubMed] [Google Scholar]
- 7.Frankenfield D.C., Alam S., Bekteshi E. Predicting dead space ventilation in critically ill patients using clinically available data. Crit Care Med. 2010;38:288–291. doi: 10.1097/CCM.0b013e3181b42e13. [DOI] [PubMed] [Google Scholar]
- 8.Ranieri V.M., Rubenfeld G.D., Thompson B.T. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 9.Dubois A.B., Britt A.G., Fenn W.O. Alveolar CO2 during the respiratory cycle. J Appl Physiol. 1952;4:535–548. doi: 10.1152/jappl.1952.4.7.535. [DOI] [PubMed] [Google Scholar]
- 10.Siobal M.S., Ong H., Valdes J. Calculation of physiologic dead space: comparison of ventilator volumetric capnography to measurements by metabolic analyzer and volumetric CO2 monitor. Respir Care. 2013;58:1143–1151. doi: 10.4187/respcare.02116. [DOI] [PubMed] [Google Scholar]
- 11.Tusman G., Sipmann F.S., Bohm S.H. Rationale of dead space measurement by volumetric capnography. Anesth Analg. 2012;114:866–874. doi: 10.1213/ANE.0b013e318247f6cc. [DOI] [PubMed] [Google Scholar]
- 12.Kallet R.H., Siobal M.S. Measuring dead space: does it really matter? or, what are we waiting for? Respir Care. 2010;55:350–352. [PubMed] [Google Scholar]
- 13.Lucangelo U., Bernabè F., Vatua S. Prognostic value of different dead space indices in mechanically ventilated patients with acute lung injury and ARDS. Chest. 2008;133:62–71. doi: 10.1378/chest.07-0935. [DOI] [PubMed] [Google Scholar]
- 14.Siddiki H., Kojicic M., Li G. Bedside quantification of dead-space fraction using routine clinical data in patients with acute lung injury: secondary analysis of two prospective trials. Crit Care. 2010;14:R141. doi: 10.1186/cc9206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kallet R.H., Zhuo H., Liu K.D. The association between physiologic dead-space fraction and mortality in subjects with ARDS enrolled in a prospective multi-center clinical trial. Respir Care. 2014;59:1611–1618. doi: 10.4187/respcare.02593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vender R.L., Betancourt M.F., Lehman E.B. Prediction equation to estimate dead space to tidal volume fraction correlates with mortality in critically ill patients. J Crit Care. 2014;29:e311–e313. doi: 10.1016/j.jcrc.2013.12.009. [DOI] [PubMed] [Google Scholar]