Abstract
Purpose
The optimal surgical treatment of displaced type B and C fractures of the proximal humerus in the elderly remains controversial. Good clinical results have been reported by plating these fractures as well as a high rate of complications. Our retrospective study aims to evaluate clinical recovery and complications using the S3 locking plate in elderly patients.
Methods
Fifty-one patients older than 65 years of age, with a complex proximal humeral fracture type B or C (AO classification system), were included. Patients have been followed up for a minimum of 12 months. We assessed callus formation, radiological results, clinical outcome (according to the Constant Shoulder Score System) and complications. Any difference in the clinical recovery among the 2 types of fracture pattern (B and C) was investigated.
Results
The mean time of fracture healing was 12.4 weeks. The mean Constant score at 3, 6 and 12 months was 68, 73 and 75 respectively. No statistically significant difference in the clinical outcome was observed between the B and C fracture patterns (p > 0.05). We noticed an overall of 5 complications (9.8%). There was no need to revision any of the implants.
Conclusion
Anatomic reduction and proper plate positioning are essential for minimizing implant-related complications. In our experience the S3 angular stability system offers a proper osteosyntesis and a good clinical recovery with a low rate of complications.
Keywords: Shoulder fractures, Bone plates, Humerus, Aged
Introduction
Fractures of the proximal humerus represent about 5% of all fractures, being the third most common fracture among elderly patients.1, 2, 3 According to Palvanen et al,3 the gross incidence, the age adjusted and the number of proximal humeral fractures have tripled during the last three decades. Approximately 75% of these fractures undergo a conservative treatment resulting in non-displaced or minimally displaced results.4, 5
On the other hand, an increasing number of specific devices have been made available such as pinning,6 intramedullary nails,7 1/3 tubular plates, cloverleaf plates,8, 9 angular stability plates,10, 11 as well as early shoulder hemiarthroplasty.12, 13 Neer criteria14 and the AO/ASIF classification system15 represent the most common tools used as a decision-making guide for treatment. As an articular fracture, proximal humerus requires the best anatomic reduction and stable fixation for an early joint mobilization, leading to a better functional outcome.16
However, open reduction and internal fixation (ORIF) has been correlated to various complications17, 18 such as hardware failure, intra-articular screw perforation, avascular necrosis, subacromial impingement, frozen shoulder, and fracture re-displacement.
The aim of the present study, using the S3 locking plate for treatment of complex proximal humeral fractures in elderly patients, was to evaluate retrospectively the clinical efficacy and complication rate.
Materials and methods
The S3 fixation plate was used in our Institution for ORIF of closed, displaced proximal humeral fractures in 90 cases from December 2005 to December 2011. This is a retrospective analysis of 51 patients who met the inclusion criteria and underwent surgery within 7 days after trauma, having a minimum follow-up of 12 months (range 12–30, mean 16 months). Four patients presenting other associated injuries of the upper limb were excluded, as well as five patients with previous shoulder injuries. Twenty-one patients with a type A fracture (according to AO classification) and nine patients with a follow-up of less than 12 months were also excluded. Subsequently, a retrospective analysis of the data was carried out. Dominant arm was involved in 55% of the cases. The mean age of patients was 70.7 years ranging from 65 to 84 years (9 males and 42 females). Most cases (45/51) had a low energy trauma. Fractures were rated according to AO/ASIF classification system15 based on AP (90° to the scapular plane), lateral and axillary (when possible) radiograms.
A CT scan was implemented when the X-ray was not suitable for a correct preoperative planning and there was discordance between the observers in classifying a fracture. The distribution of the fractures patterns, according to AO/ASIF classification, showed 31 type B and 20 type C fractures.
Considering the most important predictors of humeral head ischemia reported by Hertel et al,19 20 patients were found to have a calcar length <8 mm attached to the head (type C fractures). In addition, the medial hinge was disrupted (>2 mm) in five cases among these patients (type C2 patterns).
Despite the high risk of avascular necrosis described by Hertel, we preferred to proceed with osteosynthesis. Operation was performed under regional anesthesia with inter-scalenic nerve blocking, associated with general anesthesia when needed.
A standard delto-pectoral approach was performed with the patient placed in a beach-chair position. Reduction was surgically achieved and confirmed under fluoroscopy. All fractures were stabilized using the S3 locking plate introducing all the proximal cephalic pegs/screws and at least three distal screws. This device, designed to fit at about 3 cm distal to the greater humeral tuberosity, provides an angular stability fixation. Distal positioning of the implant should prevent any subacromial impingement. Moreover, the 4 mm proximal pegs should achieve a more stable fixation in a highly cancellous bone, and meanwhile prevent perforation of the humeral head.
After surgery, the arm was positioned in a sling. Physical therapy was performed according to Hughes and Neer rehabilitation program,20 with passive assisted movements beginning from 2nd day after surgery.
Radiographic and clinical assessment was performed by a single orthopedic consultant according to the Constant Shoulder Score (CS)21 at 3, 6 and 12 months for all patients after surgery. CS score was also calculated for the different fracture patterns alone (type B and C fractures).
This is a retrospective, observation study of our cohort and no sample size was calculated prior to the investigation. CS scores obtained showed an abnormal distribution. The median, mean values and inter-quartile ranges (IQR) were reported. The IQR is between 75th and 25th percentiles and indicates that 50% of the values are in this range. Differences of CS score between type B and C fracture groups at the different time frames (3, 6, 12 months) were investigated for statistical significance by an unpaired Mann–Whitney t-test. Significance of CS score improvement within the two fracture patterns during the follow-up was calculated by the Wilcoxon test. The SPSS statistical program was used for the analysis. For all tests p values < 0.05 were considered significant.
Results
At follow-up, the mean CS score at 3, 6 and 12 months was 68 (IQR 64 to 72), 73 (IQR 70 to 78.5) and 75 (IQR 72.5 to 80) and the median was 69, 74 and 77 respectively. In the type B fracture group, the mean CS score was 68 (IQR 64.5 to 73), 74 (IQR 70 to 79), and 76 (IQR 72.5 to 81). The median was found to be 69.5, 75.5, 79.5 respectively. In the type C fracture group the mean CS was 67 (IQR 64 to 71), 72 (IQR 68 to 75) and 75 (IQR 73 to 79). The median was 69, 72 and 75 respectively.
No variation was detected in 43 (43/51) patients during a 20 months follow-up. No statistical significance was found (p = 0.46, 0.15, 0.16 respectively) between groups B and C at 3, 6 and 12 months after surgery (Table 1). The Wilcoxon test showed a statistical significance in the CS score improvement within the groups among the different time frames (p = 0.001) when investigating the outcome between the consecutive follow-up. In 2 cases of type B1, in 1 case of type B3 and in 1 case of type C1 fracture, radiographic results were poor but the clinical outcome obtained at the final follow-up was satisfactory.
Table 1.
Median (Interquartile range) CS score at 3,6,12 months for all patients and for the B and C fracture pattern alone. No significant difference was found comparing the 2 groups (p > 0.05) with an unpaired Mann–Whitney t-test.
| Postoperation | All patients | Type B fractures | Type C fractures | p value |
|---|---|---|---|---|
| 3 months | 69 (IQR 64–72) | 69.5 (IQR 64.5–73) | 69 (IQR 64–71) | 0.46 |
| 6 months | 74 (IQR 70–78.5) | 75.5 (IQR 70–79) | 72 (IQR 68–75) | 0.155 |
| 12 months | 77 (IQR 72.5–80) | 79.5 (IQR 72.5–81) | 75 (IQR 73–79) | 0.162 |
We observed 5 complications (9.8%) among the 51 patients reported in our study. No cases of deep infections occurred. One case (1.96%) of superficial infection was detected and resolved in 2 weeks by oral antibiotic therapy. No cases of early avascular necrosis were detected during the minimum follow-up period of 12 months in our cohort. There were no neurovascular injuries prior to surgery or any iatrogenic damages following the surgical procedure.
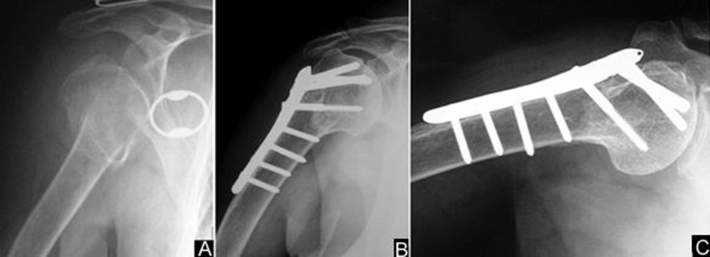
Fracture healing was achieved with the evidence of sufficient callus formation and cortex continuity in the standard X-ray films, with no cases of pseudoarthrosis. The mean time to fracture healing was 12.4 weeks (range 8–16 weeks). There were 4 cases (7.8%) of primary subacromial impingement of the plate due to a varus inclination of the humeral head <120°and malreduction >5° in all cases (Fig. 1). Among these fractures (type 2B1, 1B2 and 1C1 fractures), all patients were 67 years old or older (mean 71 years).
Fig. 1.
A 78 years old woman with a type B1 fracture: (A) preoperative X-ray; (B, C) postoperative X-ray at 12 months showing fracture healing and evidence of subacromial impingement in abduction as a result of a varus inclination of the humeral head.
None of these patients developed a varus displacement in the postoperative follow-up. No other implant-related complications such as hardware breakage, implant dislocation, cut-out, and intra-articular screw perforation were detected. In one case the tip of the drill was broken and left into the bone, resulting in no interference with implant fixation and bone healing.
All 4 patients presenting subacromial impingement refused a reoperation for implant removal, having a satisfactory clinical outcome. To date, 3 implants have been removed after patients' request without beneficial clinical outcome.
Discussion
Decision making for the treatment of proximal humeral fractures includes various parameters, such as patients' age, general medical conditions, daily activities before injury, and the fracture pattern.
Conservative treatment remains the gold standard for non-displaced or minimal displaced fractures of the proximal humerus with satisfactory results.5, 17 Furthermore, surgical treatment of displaced fractures remains a challenge. Thus, radiological imaging including AP and axillary views is necessary. If not possible, when the only emergency AP view is available (Fig. 1A), a CT scan is necessary for better defying the fracture pattern. Subsequently, a multiplanar reconstruction (MPR) could be used for a detailed preoperative planning. Aiming to anatomic reduction and stable fixation, any device resulting in a better clinical outcome could be used to allow early mobilization.16
Considering preoperative activities of the patient and bone quality, ORIF seems highly recommended in young patients with displaced fractures of the proximal humerus.22 Physician should offer, to the aged but still active patient, a proper treatment that could turn in delaying any type of one way surgery, such as shoulder hemiarthroplasty. However, vascular supply of the humeral head is the key point in such cases and the preoperative planning should be addressed not only to select the optimal implant but also to understand if the present fracture is to be fixed or to be treated by prosthesis. Particular emphasis should be given for a proper support of the proximal medial part of the humeral metaphisis.19, 23
In our cohort, we preferred to perform osteosyntesis even in those patterns rated as a high risk of avascular necrosis, giving particular emphasis on an accurate reduction of the medial metaphyseal extension of the fracture. However 8 patients with a calcal segment <8 mm and head-splitting (type C3 fractures not included in this study) were treated by a shoulder hemiarthroplasty or an inverse prosthesis, considering the poor reduction likely achieve.
Various types of plates have been used for ORIF during the past years and mostly good results were reported, especially when adopting angle-stabilizing plates. Despite the good results reported, ORIF has been correlated, in a significant number of papers, with a high number of subacromial impingement, screw penetration of the humeral head, loss of reduction, avascular necrosis, and infections.11, 18, 24, 25
Gille et al26 presented preliminary results of five proximal humeral fractures treated with the S3 locking plate. Aksu et al27 adopted this plate in 10 out of 107 patients treated over a four years period, reporting only one complication. They considered that the S3 locking plate is placed in a lower position than that of the PHILOS plate, therefore it is less likely to result in impingement syndrome.
To our knowledge, our retrospective study reports the higher number of patients treated with the S3 locking plate. Our patients experienced a very good clinical recovery with a mean CS score of 75 at the final follow-up and 5 complications (9.8%). We compared our results with studies adopting other locking plate systems and found similar or better clinical outcomes and less complications.
Helwig et al24 conclude that even using fixed-angle implants, fractures of the proximal humerus are associated with a high complication rate and sometimes poor outcome. Solberg et al28 experienced more complications among the 70 years old patients with three and four part fractures as compared with our study. They concluded that Neer 3- and 4-part proximal humeral fractures in older patients with initial varus angulation of the humeral head had a significantly worse clinical outcome and a higher complication rate than similar fracture patterns with initial valgus angulation. Schliemann et al29 found satisfactory or good clinical outcomes after treating complex proximal humeral fractures in elder patients and a high complication rate. Leonard et al30 also report good functional results, thus, giving emphasis on the high potential for reoperations following various complications.
Screw perforation and loss of reduction are the most frequent problems among these papers followed by avascular necrosis. The restricted number of implant-related complications in our study could be the result of specific features of this fixation plate. All cases of subacromial impingement (4/51) of the plate adopted in this study were the result of improper reduction and a varus inclination (<120°, malreduction >5°) of the humeral neck (Fig. 1B, C). Varus malreduction (>5°) is considered to be common among varus impacted fractures with a higher possibility of mechanical disadvantages and failure of the implant.28
When anatomic reduction is achieved, the S3 plate can prevent any impingement (fitting 3 cm distally to the great tuberosity, Fig. 2). The absence of any protrusion through the articular surface and no loss of reduction or implant breakage are in our opinion the advantage of the blunt-tipped subchondral support pegs. Huff et al31 compared the mechanical stability of the S3 and the Synthes fixation plate in bending and torsion in synthetic and cadaveric speciments. They concluded that the S3 plate was stiffer than the Synthes plate in terms of varus and valgus bending, as well as in torsion. However, Schumer et al,32 using threaded screws and smooth pegs in post-mortem proximal humeral specimens, evaluated differences in the biomechanical properties of locking plates. They concluded that there was no statistically significant difference between the 2 types of fixation.
Fig. 2.
A 70 years old woman with a type C1 fracture: (A) preoperative X-ray; (B, C) postoperative X-rays at 6 months showing bone healing.
In conclusion, further investigation by prospective randomized trials is necessary to compare with other fixation techniques. A long term follow-up of these patients could be also useful to identify patients with secondary painful arthrosis and eventually late avascular necrosis. The limited number of patients included represents a limit of this study.
Anatomic reduction and proper plate positioning are essential for minimizing hardware-related complications. Due to the particular bone and vascular structure of this area, a detailed preoperative study of the fracture pattern, especially regarding a possible blood supply impairment is essential. In our opinion osteosynthesis should be tempted every time and a satisfactory reduction could be achieved in order to delay any type of a one-way surgery, such as shoulder hemiarthroplasty.
Our results suggest that the S3 locking plate system represents a valid alternative for ORIF of proximal humeral fractures. It can offer a favorable clinical recovery in the elderly, with a restricted number of complications.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Habermeyer P., Schweiberer L. Fractures of the proximal humerus. Othopade. 1989;18:200–207. [PubMed] [Google Scholar]
- 2.Bengner U., Johnell O., Redlund-Johnell I. Changes in the incidence of fracture of the upper end of the humerus during a 30-year period. A study of 2125 fractures. Clin Orthop Relat Res. 1988;231:179–182. [PubMed] [Google Scholar]
- 3.Kannus P., Palvanen M., Niemi S. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970-1998 and alarming projections for the new millennium. Acta Orthop Scand. 2000;71:465–470. doi: 10.1080/000164700317381144. [DOI] [PubMed] [Google Scholar]
- 4.Lill H., Bewer A., Korner J. Conservative treatment of dislocated proximal humeral fractures. Zentralbl Chir. 2001;126:205–210. doi: 10.1055/s-2001-12495. [DOI] [PubMed] [Google Scholar]
- 5.Neer C.S., 2nd Displaced proximal humeral fractures. Ⅱ. Treatment of three-part and four-part displacement. J Bone Jt Surg Am. 1970;52:1090–1103. [PubMed] [Google Scholar]
- 6.Fenichel I., Oran A., Burstein G. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop. 2006;30:153–157. doi: 10.1007/s00264-005-0058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koike Y., Komatsuda T., Sato K. Internal fixation of proximal humeral fractures with a Polarus humeral nail. J Orthop Traumatol. 2008;9:135–139. doi: 10.1007/s10195-008-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esser R.D. Treatment of three- and four-part fractures of the proximal humerus with a modified cloverleaf plate. J Orthop Trauma. 1994;8:15–22. doi: 10.1097/00005131-199402000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Sehr J.R., Szabo R.M. Semitubular blade plate for fixation in the proximal humerus. J Orthop Trauma. 1988;2:327–332. doi: 10.1097/00005131-198802040-00010. [DOI] [PubMed] [Google Scholar]
- 10.Siwach R., Singh R., Rohilla R.K. Internal fixation of proximal humeral fractures with locking proximal humeral plate (LPHP) in elderly patients with osteoporosis. J Orthop Traumatol. 2008;9:149–153. doi: 10.1007/s10195-008-0014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bjorkenheim J.M., Pajarinen J., Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand. 2004;75:741–745. doi: 10.1080/00016470410004120. [DOI] [PubMed] [Google Scholar]
- 12.Robinson C.M., Page R.S., Hill R.M. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Jt Surg Am. 2003;85:1215–1223. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Zyto K., Wallace W.A., Frostick S.P. Outcome after hemiarthroplasty for three- and four-part fractures of the proximal humerus. J Shoulder Elb Surg. 1998;7:85–89. doi: 10.1016/s1058-2746(98)90215-4. [DOI] [PubMed] [Google Scholar]
- 14.Neer C.S., 2nd Displaced proximal humeral fractures: Ⅰ. Classification and evaluation. J Bone Jt Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 15.Müller M.E., Nazarian S., Koch P. 1st ed. Heidelberg; Berlin: 1990. The Comprehensive Classification of Fractures of Long Bones. [Google Scholar]
- 16.Hintermann B., Trouillier H.H., Schafer D. Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Jt Surg Br. 2000;82:1107–1112. doi: 10.1302/0301-620x.82b8.10330. [DOI] [PubMed] [Google Scholar]
- 17.Wachtl S.W., Marti C.B., Hoogewoud H.M. Treatment of proximal humerus fracture using multiple intramedullary flexible nails. Arch Orthop Trauma Surg. 2000;120:171–175. doi: 10.1007/s004020050037. [DOI] [PubMed] [Google Scholar]
- 18.Zyto K., Ahrengart L., Sperber A. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Jt Surg Br. 1997;79:412–417. doi: 10.1302/0301-620x.79b3.7419. [DOI] [PubMed] [Google Scholar]
- 19.Hertel R., Hempfing A., Stiehler M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elb Surg. 2004;13:427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 20.Hughes M., Neer C.S., 2nd Glenohumeral joint replacement and postoperative rehabilitation. Phys Ther. 1975;55:850–858. doi: 10.1093/ptj/55.8.850. [DOI] [PubMed] [Google Scholar]
- 21.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 22.Williams G.R., Wong K.L. Two part and three part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin North Am. 2000;31:1–21. doi: 10.1016/s0030-5898(05)70124-3. [DOI] [PubMed] [Google Scholar]
- 23.Gardner M.J., Weil Y., Barker J.U. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21:185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 24.Helwig P., Bahrs C., Epple B. Does fixed-angle plate osteosynthesis solve the problems of a fractured proximal humerus? A prospective series of 87 patients. Acta Orthop. 2009;80:92–96. doi: 10.1080/17453670902807417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sadowski C., Riand N., Stern R. Fixation of fractures of the proximal humerus with the planttan humerus fixator plate: early experience with a new implant. J Shoulder Elb Surg. 2003;12:148–151. doi: 10.1067/mse.2003.11. [DOI] [PubMed] [Google Scholar]
- 26.Gille J., Schulz A.P., Queitsch Ch. Initial results of the S3-humerus plate. Open Orthop J. 2008;2:133–136. doi: 10.2174/1874325000802010133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aksu N., Göğüş A., Kara A.N. Complications encountered in proximal humerus fractures treated with locking plate fixation. Acta Orthop Traumatol Turc. 2010;44:89–96. doi: 10.3944/AOTT.2010.2313. [DOI] [PubMed] [Google Scholar]
- 28.Solberg B.D., Moon C.N., Franco D.P. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23:113–119. doi: 10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 29.Schliemann B., Siemoneit J., Theisen Ch. Complex fractures of the proximal humerus in the elderly–outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96:S3–S11. doi: 10.1007/s12306-012-0181-8. [DOI] [PubMed] [Google Scholar]
- 30.Leonard M., Mokotedi L., Alao U. The use of locking plates in proximal humeral fractures: comparison of outcome by patient age and fracture pattern. Int J Shoulder Surg. 2009;3:85–89. doi: 10.4103/0973-6042.63214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huff L.R., Taylor P.A., Jani J. Proximal humeral fracture fixation: a biomechanical comparison of two constructs. J Shoulder Elb Surg. 2013;22:129–136. doi: 10.1016/j.jse.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 32.Schumer R.A., Muckley K.L., Markert R.J. Biomechanical comparison of a proximal humeral locking plate using two methods of head fixation. J Shoulder Elb Surg. 2010;19:495–501. doi: 10.1016/j.jse.2009.11.003. [DOI] [PubMed] [Google Scholar]