Abstract
Introduction
Postpartum telogen effluvium (PPTE) is a commonly described entity, but few studies deal with the real incidence and pathogenesis of this claimed common disease.
Objective
To analyze the objective data published and to define the real incidence of the so-called PPTE.
Method
A retrospective review of the published data was conducted.
Results
No statistically significant data were found in any of the papers reviewed, which could support the conclusion that the amount of hair shedding between pregnant and postpartum women is different.
Conclusion
PPTE is not a well-defined entity, and the exact incidence is unknown. From our literature review, we could state that the frequency of PPTE is so low and undefined that we dare say that PPTE does not exist.
Key Words: Postpartum telogen effluvium, Pregnancy, Hormones, Hair loss, Lactation
Introduction
The hair cycle is a complex biological process of partially unknown signals by which human hair follicles undergo three main stages: growth (anagen phase), apoptosis-driven regression (catagen phase) and the quiescent state (telogen phase). The phases last approximately 2-6 years, 2-3 weeks and 3 months, respectively. The normal hair cycle replaces each hair on the scalp every 3-5 years. Some of the biological cascade signals by which the anagen phase shifts to the catagen and telogen phases remain unclear [1,2,3]. The phases are not equal in duration, and the biological pathways by which one phase switches to the next are not yet well understood [4].
Telogen effluvium (TE) is a diffuse hair pattern loss which occurs 3 months after a triggering event and is self-limited in time [3]. Different types of stresses have been related to TE, such as febrile states, stress, major surgery, an increase in androgen and estrogen hormones, hyperthyroidism and many others [3]. It is well studied that hormone levels during and after pregnancy are dramatically distinct. During pregnancy, there is a peak of human chorionic gonadotropin at 2 months, a 9-fold gradual increase in progesterone and an 8-fold increase in estrogens [4]. Once the placenta is removed at birth, the levels of progesterone and estrogens return to normal within 2-4 days [5,6]. Prolactin also rises gradually during pregnancy, reaching a 20-fold increase at term [7]. It is believed that TE can be explained with these variations in hormone levels in postpartum women.
Postpartum TE (PPTE) is usually reported as hair loss after delivery [1,2,3]. Many patients, if asked, would state that they have the impression that their hair falls out a few months after delivery, but it is not a consistent observation throughout the entire postpartum group, and it might be overestimated by many due to the psychological stress of their body changes. PPTE has not been the focus of vigorous and serious research, and only two studies have been conducted until today. In the 1960s, Lynfield [1] was the first to investigate this phenomenon, performing a trichogram of the temporal scalp, and ever since, PPTE had been considered by many as a confirmed incident. In 2013, Ekmekci et al. [2] tried to study PPTE with a more sophisticated tool: the trichoscan [2,8]. Both articles wanted to demonstrate that this phenomenon [1,2], namely that the hair of women falls out in a higher quantity after delivery, is true and notable.
In this review, we analyze the data gathered to date in order to have a clear idea of what is happening to these postpartum women and if PPTE is actually relevant in this population.
Methods
We have retrospectively reviewed the literature in search of PPTE evidence and compared the two papers which confront PPTE with a scientific approach. The paper of Lynfield [1] in 1960 and that of Ekmekci et al. [2] in 2013 have been carefully analyzed and the clinical data discussed in order to give a clear understanding of PPTE [1,2].
Results
The study of Lynfield was conducted with 26 pregnant women in total; they were analyzed during pregnancy every 3 months, and three more times postpartum, and the clinical hair loss was analyzed in some of them. The respective results are shown in table 1.
Table 1.
Age, anagen rates in all 26 patients and clinical hair loss [1]
| Age, years | 1st trimester | 2nd trimester | 3r trimester | 1 week PP | 6 weeks PP | 3 weeks PP | Clinical hair loss |
|---|---|---|---|---|---|---|---|
| 25 | 96 | 94 | 97 | 74 | 74 | 4–6 months PP | |
| 24 | 93 | 88 | 70 | 1–10 weeks PP | |||
| 20 | 86 | 56 | no | ||||
| 38 | 87 | 91 | 91 | no | |||
| 32 | 98 | 100 | 97 | 65 | no | ||
| 26 | 98 | 99 | 89 | 54 | no | ||
| 25 | 98 | 97 | 89 | no | |||
| 23 | 96 | 94 | 92 | 77 | no | ||
| 29 | 84 | unreported | |||||
| 21 | 87 | unreported | |||||
| 22 | 89 | unreported | |||||
| 24 | 81 | unreported | |||||
| 25 | 83 | unreported | |||||
| 29 | 95 | unreported | |||||
| 26 | 93 | unreported | |||||
| 21 | 91 | unreported | |||||
| 23 | 95 | unreported | |||||
| 24 | 98 | unreported | |||||
| 34 | 90 | unreported | |||||
| 26 | 91 | yes | |||||
| 17 | 97.5 | 95 | unreported | ||||
| 23 | 94 | 92 | unreported | ||||
| 31 | 97.5 | 95 | 73 | unreported | |||
| 29 | 77 | yes | |||||
| 38 | 72 | unreported | |||||
| 21 | 77 | unreported | |||||
PP = Postpartum.
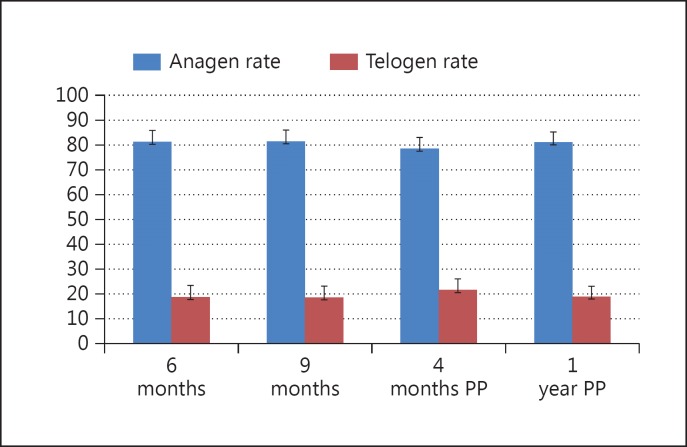
The study of Ekmekci et al. was conducted with 116 women, distributed into 4 different stages: at 6 and 9 months of pregnancy, and at 4 and 12 months postpartum. Data were collected once from each woman, and the results obtained were compared with all the interpersonal differences. They demonstrated a difference between all the groups and the 4-month postpartum group, in which the anagen phase decreased and the telogen phase increased. These results are shown in table 2 and figure 1 to better capture the difference stated by the authors (the graph places differences into a better perspective, which the numbers cannot hold up).
Table 2.
Mean age and anagen and telogen rates in the four groups studied [2]
| At 6 months of pregnancy (n = 28) | At 9 months of pregnancy (n = 30) | At 4 months PP (n = 29) | At 1 year PP (n = 29) | p value | |
|---|---|---|---|---|---|
| Age, years | 29.07 ± 4.19 | 27.43 ± 5.24 | 27.43 ± 3.18 | 27.17 ± 4.13 | 0.325 |
| Anagen rate | 81.24 ± 4.63 | 81.43 ± 4.55 | 78.47 ± 4.51 | 81.05 ± 4.14 | 0.042 |
| Telogen rate | 18.76 ± 4.63 | 18.57 ± 4.55 | 21.53 ± 4.51 | 18.94 ± 4.14 | 0.042 |
PP = Postpartum.
Fig. 1.
Anagen versus telogen rates during pregnancy and postpartum periods. Lactation seemed to have some influence on the anagen rate since there were statistically significant data between the women who did not breastfeed and those who did, measured at 4 months postpartum.
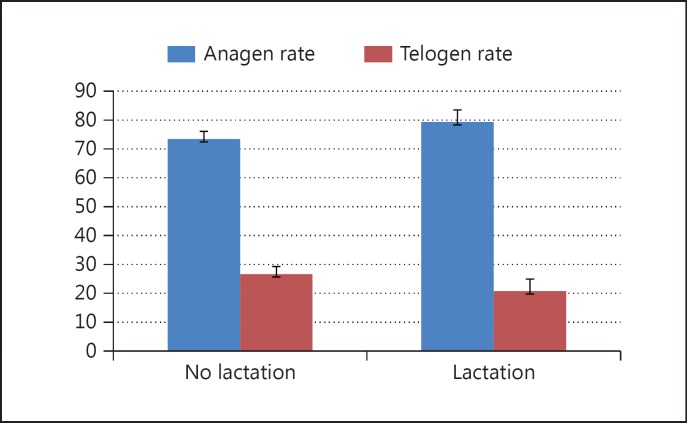
Lactation seemed to have some influence on the anagen rate since there were statistically significant data between women who did not breastfeed and those who did, measured at 4 months postpartum. The results are shown in table 3 and figure 2, in which the stated difference can be appreciated more clearly.
Table 3.
Four months postpartum: no lactation versus lactation [2]
| No lactation | Lactation | p value | |
|---|---|---|---|
| (n = 4) | (n = 5) | ||
| Anagen rate | 73.37±2.63 | 79.28±4.22 | 0.014 |
| Telogen rate | 26.62±2.63 | 20.72±4.22 | 0.014 |
Fig. 2.
Four months postpartum: no lactation versus lactation [2].
Discussion
The study of Lynfield [1] was conducted with 26 pregnant women in total, but only 10 women were examined at 6 weeks postpartum and 5 women at 3 months postpartum; the rest were examined during pregnancy or 1 week postpartum. The data gathered before and after pregnancy were not from the same women. Only the data of 9 women were collected during the 3rd trimester as well as at 6 weeks or 3 months postpartum. Of these 9 women, 7 showed an increase in the telogen phase and a decrease in the anagen phase after their pregnancy at 6 weeks or 3 months postpartum with the trichogram. Out of the 26 women, only 4 reported clinical hair loss, whereas 6 did not state any clinical hair loss. The remaining women were not assessed. There are many hormonal, nutritional and uncontrolled factors which vary among women, and the fact that the data are from different women at different stages of their pregnancy or postpartum cannot be biologically comparable. Also, the authors mixed the data collected from the same woman and data from different women and compared all of them during a final statistical exam, testing for significance. Moreover, their method used is observer dependent since counting 100 hairs of each patient under the microscope might be tricky. The study is not blinded to remove possible unconscious counting bias since the same researcher also states the hair phases. Unfortunately, not many patients have been analyzed nor was the same patient analyzed during different stages of pregnancy and postpartum. A better approach should have been used, and additional research should have been done in order to confirm TE after the pregnancy.
From the paper of Ekmeci et al. [2], we concluded that there are statistically significant differences between the 4-month postpartum group and any of the other groups. The mean difference was an anagen rate of 78.47 at 4 months postpartum and of 81.43 in the other periods, approximately. However, a small difference exists between the groups as represented in figure 1; there is a surprisingly statistically significant difference between pregnancy and 4 months postpartum.
The authors did not state precisely in which period of the year the data were collected for each woman in the study, adding a seasonal shedding factor that could play a role in the group differences reported. Ekmekci et al. affirm that summer time was excluded from the study, but there is still a big hair shedding in autumn and spring that might have had an effect on the increase in the telogen rate. It is well known that the seasons have an effect on the hair cycle, and thus, may increase TE [3].
When comparing lactating with non-lactating groups of women, the authors found a statistically significant difference. However, the number of non-lactating women analyzed was only 4 and that of lactating women was 25. The few included non-lactating women could lead to wrong assumptions.
The number of women analyzed by Ekmekci et al. [2] was 4 times higher than that analyzed by Lynfield [1], and the method used was more consistent and avoided observer bias by using a trichoscan. Still, the data were collected from different women at different pregnancy or postpartum stages; also, the number of non-lactating women was 4, which is too small a number to make any assumptions about the effect of lactation on women's hair health. Lastly, the subjective information of whether every patient felt that PPTE was occurring to them and when could also be useful to help understand if this rate difference actually matches the women's clinical shedding sensation.
PPTE might be a clinically valid observation or a simple overestimation of what really occurs, enhanced by the psychological stress that translates assuming all the body changes right after delivery. As our revision demonstrates, PPTE has not been supported by serious evidence in any of the studies analyzed. Therefore, we could affirm that PPTE seems to be overestimated by some women.
Conclusions
Although in most dermatological textbooks PPTE occupies a paragraph in the hair section, our literature review shows that there are no well-performed clinical studies that could claim the existence of PPTE.
In order to clarify the real incidence of PPTE, further studies including a higher number of patients under the same biological conditions and a better follow-up would give light to this unsolved question.
Statement of Ethics
We ensure the quality and integrity of our review, in which the entire scientific literature has been analyzed thoroughly and all the papers studying PPTE were considered in the same manner. No patients were used to write this paper, and thus, no informed consent or money of any sort was needed to conduct this research.
Disclosure Statement
In accordance with Universitat Internacional de Catalunya policies and procedures, and our ethical obligation as researchers, we are reporting that we do not have financial and/or business interests that may be affected by the research reported in the enclosed paper. Our interest in this publication is to bring a new perspective into the so-called PPTE, in order to call for more evidence before we affirm this phenomenon.
References
- 1.Lynfield YL. Effect of pregnancy on the human hair cycle. J Invest Dermatol. 1960;35:323–327. doi: 10.1038/jid.1960.54. [DOI] [PubMed] [Google Scholar]
- 2.Ekmekci TR, et al. The changes in the hair cycle during gestation and the post-partum period. J Eur Acad Dermatol Venereol. 2014;28:878–881. doi: 10.1111/jdv.12188. [DOI] [PubMed] [Google Scholar]
- 3.Malkud S. Telogen effluvium: a review. J Clin Diagn Res. 2015;9:9. doi: 10.7860/JCDR/2015/15219.6492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piérard GE. The hair eclipse phenomenon: sharpening the focus on the hair cycle chronobiology. Int J Cosmet Sci. 2003;25:295–299. doi: 10.1111/j.1467-2494.2003.00198.x. [DOI] [PubMed] [Google Scholar]
- 5.Tulchinsky D, Hobel CJ, Yeager E, Marshall JR. Plasma estrone, estradiol, estriol, progesterone, and 17-hydroxyprogesterone in human pregnancy. Am J Obstet Gynecol. 1972;112:1095–1100. doi: 10.1016/0002-9378(72)90185-8. [DOI] [PubMed] [Google Scholar]
- 6.Hendrick V, Altshuler LL, Suri R. Hormonal changes in the postpartum and implications for postpartum depression. Psychosomatics. 1998;39:93–101. doi: 10.1016/S0033-3182(98)71355-6. [DOI] [PubMed] [Google Scholar]
- 7.Ostrom KM. A review of the hormone prolactin during lactation. Prog Food Nutr Sci. 1990;14:1–43. [PubMed] [Google Scholar]
- 8.Hoffman R. Trichoscan: what is new? Dermatology. 2005;211:54–62. doi: 10.1159/000085581. [DOI] [PubMed] [Google Scholar]