Abstract
Objective
Current advice for patients being discharged from hospital suggests a body mass index of 18.5 to 24 kgm−2, although this aspirational target may often not be achieved. We examined the relationship between body mass index on discharge from hospital and subsequent mortality over a maximum follow-up of 3.8 years.
Design
We conducted a survival analysis using linked hospital records data with national hospital episode statistics and national death certification data.
Participants & Setting
The analysis included adult patients who were admitted to University Hospitals Birmingham NHS Foundation Trust for a period of over 24 h during 2011, excluding day cases and regular day case attenders.
Main outcome measures
The relationship between body mass index and mortality at medium term was estimated separately in both men and women, after accounting for case-mix.
Results
For both males and females, the relationship between body mass index at discharge and the loge hazard of death was strongly non-linear (p = 0.0002 for females and p < 0.0001 for males) and predictive (both p < 0.0001). In all models, the optimal body mass index range associated with best survival was 25 to 35 kgm−2, with a sharp increase in risk for lower body mass index.
Conclusions
There was little evidence to support current aspirational body mass index targets in the discharge population. Hospitals should ensure adequate nutrition especially among those with a reduced body mass index.
Keywords: Evidence-based practice, nutrition, metabolism
Introduction
The evidence that being overweight or obese predict poor health outcomes such as diabetes is strong,1 yet the relationship between mortality risk and body mass index (BMI, defined as weight in kilograms divided by height in metres squared) remains controversial. With an estimated 1.5 billion overweight or obese adults worldwide, this has substantial clinical and public health implications.
In a recent systematic review of 2.9 million people which adjusted for smoking status and chronic illness, only severely obese individuals (BMI > 35) were at increased risk of death from any cause compared to those with a BMI in the normal range (BMI 18–25) and overweight individuals (BMI 25–30) were at lower risk of death.2 By contrast, population-based studies of healthy adult non-smokers in middle age have shown a strong relationship between being overweight or obese and increased mortality, in both Western and non-Western populations.3,4 Smoking, chronic illness and increasing age are important modifiers of the relationship between BMI and mortality and this is compounded by variation in BMI-based weight categorisation, selection of different reference categories and the duration of study follow-up. In specific groups such as the elderly, BMI may be poorly discriminatory because the distribution of adipose tissue changes with increasing age.5
Patients on discharge from hospital are a population for whom there is an opportunity to provide advice on nutrition and calorie intake. In the UK, patients at discharge from hospital are normally recommended to maintain a BMI between 20 kgm−2 and 30 kgm−2,6 although the evidence base for this recommendation is unclear. For patients being discharged from hospital, the benefits of attaining a BMI value within the normal range may be negligible because these patients have comparatively high rates of smoking and chronic illness relative to the general population. In this study, we examined the relationship between BMI and mortality among patients discharged alive, using a unique holding of linked hospital and national records in order to inform clinical practice and guidance to patients.
Methods
Patients
University Hospital Birmingham NHS Foundation Trust (UHB) is a leading university teaching hospital and is one of the most consistently high-performing trusts in the NHS.7 UHB captures and holds a large amount of clinical data on its patients in a variety of different systems electronically. Through linking these datasets together, we can build a detailed description of patient status and assess and evaluate outcomes. For a number of years, UHB has held linked electronic data records on all patients treated in the hospital trust, a holding which includes prescribing, clinical observations, assessments, laboratory results, long-term outcome, demographics and admission history. We included patients admitted to UHB for a period of over 24 h during 2011, excluding day cases, regular day-case attenders and patients aged less than 18 years. For patients who were admitted more than once in 2011, only the first admission was retained for analysis.
Data sources
We accessed linked data from patients discharged alive from UHB, including: BMI; diagnosis,8 optimally grouped into disease areas based upon the Summary Hospital-level Mortality Indicator (SHMI) groupings9 and further clinical advice; age; sex; ethnicity; deprivation score (Index of Multiple Deprivation, IMD);10 admission source; admission urgency; number of urgent admissions and total number of complex admissions in five years prior to index admission; number of different drugs prescribed in inpatient spell; whether antibiotics were prescribed; whether intravenous drugs were given; whether immunosuppressant drugs were given; current smoking status; values for sodium, albumin, urea, white cell count, platelets, estimated glomerular filtration rate (eGFR); death indicator; and date of death after discharge. Information on death was retrieved from the Office for National Statistics mortality database.
Statistical analysis
We developed multivariable prognostic Cox proportional hazards models,11 examining the relationship between BMI at discharge and survival, accounting for case-mix. The candidate explanatory variables listed above were identified as a result of having a known impact on patient outcomes. Their initial inclusion was the product of considerable thought and discussion among the co-authors. The final model was then further reduced using backwards elimination. Continuous predictors were included into the model using restricted cubic splines to allow for non-linear effects where these substantially improved model fit.12 Comparisons between models were made using the Akaike’s Information Criterion.13 We tested for departures from the Cox model’s proportional hazards assumption by including interactions between a function of time and the covariates. Several functions of time were considered: a linear function, loge() and step functions of time. We also examined residual plots of the main models.
A number of the items included as candidate explanatory variables were not fully observed. In particular, the blood test results were likely to be missing not at random as doctors tend to request a blood test when they judge that the test value would be abnormal. White and Carlin14 have clearly showed via a simulation study that the regression coefficient estimates from a complete records analysis have negligible bias if, conditional on the model’s predictors, the missing data process does not depend on the outcome. We believe that this conditional independence assumption is likely to hold in our analysis. In other words, we expect that after adjusting for the model’s covariates (patient’s diagnosis, admission urgency and source, etc.) the probability for a patient of not getting a blood test is not related to his or her own survival time. We therefore undertook a complete case analysis and carried out sensitivity analyses to examine the robustness of our assumptions.
The principal analysis included all the patients who met the inclusion/exclusion criteria. Further sub-analyses were conducted in patients with cardiovascular or oncological diagnoses, which were identified using ICD10 diagnostic coding. In addition, since there were no censored observations before two years post discharge, a supportive analysis was carried out using a logistic model with the two-year mortality indicator as the response variable.
All statistical analyses were performed using Stata 13 (StataCorp LP, College Station, TX, USA) and SAS 9.4 (SAS Institute; Cary, NC, USA). The study was registered with the Audit Department of UHB.
Results
We identified a total of 19,528 adult patients who were admitted to UHB for at least 24 h during 2011 and who were discharged alive. Around 19% of these patients had more than one admission in 2011.
Table 1 reports summary statistics by gender for the overall data and for the subset of records with complete information on the variables included in the analysis. There were 7.3% of admissions with missing values for BMI, 3.2% for IMD, 3% observations had no information on diagnosis and 7.8% had none of the targeted reported laboratory test results. Overall, around 30% of patients had incomplete data and were not included in the main analysis.
Table 1.
Summary statistics for the full data and for the subset of records with complete information on the variables included in the analysis.
| Full dataset |
Complete records |
|||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| No. of patients (% of the full dataset) | 10,571 (100%) | 8957 (100%) | 7391 (69.9%) | 6283 (70.2%) |
| No. of deaths (%) | 2258 (21.4%) | 1977 (22.1%) | 1761 (23.8%) | 1559 (24.8%) |
| No. of cancer patients | 1662 | 1284 | 1187 | 915 |
| No. of patients with cardiovascular diseases | 2197 | 1454 | 1693 | 1088 |
| Age | ||||
| Median (IQR) | 61 (43–74) | 63 (45–78) | 63 (47–75) | 65 (48–79) |
| BMI | ||||
| Median (IQR) | 25.9 (22.8–29.2) | 25.8 (22.2–30.5) | 26 (22.9–29.3) | 25.8 (22.1–30.4) |
| Missing values | 721 (6.8%) | 708 (7.9%) | – | – |
| Deprivation IMD score | ||||
| Median (IQR) | 25.4 (15.3–43.6) | 27.4 (16.4–44.1) | 25.4 (15.3–43.6) | 27.2 (16.2–43.7) |
| Missing values | 452 (4.3%) | 167 (1.9%) | – | – |
| Admission via A&E (%) | 3128 (29.6%) | 3149 (35.2%) | 2230 (30.2%) | 2230 (35.5%) |
| Emergency admission (%) | 6649 (62.9%) | 5911 (66%) | 4847 (65.6%) | 4440 (70.7%) |
| Smokers (%) | 2822 (26.7%) | 1665 (18.6%) | 2026 (27.4%) | 1147 (18.3%) |
| No. complex admissions in last 5 years | ||||
| Median (IQR) | 2 (1–5) | 3 (1–6) | 2 (1–6) | 3 (1–7) |
| No. emergency admissions in last 5 years | ||||
| 0 admissions | 8880 (84%) | 7110 (79.4%) | 6221 (84.2%) | 4990 (79.4%) |
| 1–5 admissions | 1642 (15.5%) | 1774 (19.8%) | 1136 (15.4%) | 1236 (19.7%) |
| 6–10 admissions | 44 (0.4%) | 54 (0.6%) | 29 (0.4%) | 41 (0.7%) |
| >10 admissions | 5 (0.05%) | 19 (0.2%) | 5 (0.1%) | 16 (0.2%) |
| No. patients who received i.v. drugs (%) | 8737 (82.7%) | 7317 (81.7%) | 6340 (85.8%) | 5350 (85.2%) |
| No. patients who received Immunosuppressant drugs (%) | 1960 (18.5%) | 1835 (20.5%) | 1503 (20.3%) | 1437 (22.9%) |
| Min albumin | ||||
| Median (IQR) | 37 (31–42) | 37 (31–41) | 37 (31–42) | 36 (31–41) |
| Missing values (%) | 1843 (17.4%) | 1662 (18.6%) | – | – |
| Min platelets | ||||
| Median (IQR) | 204 (153–255) | 232 (176–292) | 202 (150–254) | 230 (174–289) |
| Missing values (%) | 1401 (13.3%) | 1358 (15.2%) | – | – |
| Peak sodium | ||||
| Median (IQR) | 142 (139–144) | 141 (139–143) | 142 (140–144) | 142 (139–143) |
| Missing values (%) | 1354 (12.8%) | 1359 (15.2%) | – | – |
| Peak urea | ||||
| Median (IQR) | 6.6 (5–9.8) | 6 (4.4–9.1) | 6.9 (5.2–10.3) | 6.2 (4.5–9.4) |
| Missing values (%) | 1237 (11.7%) | 1240 (13.8%) | – | – |
| Peak white blood cell count | ||||
| Median (IQR) | 10.6 (8–14.3) | 10.6 (7.9–14.3) | 10.8 (8.2–14.6) | 10.8 (8–14.6) |
| Missing values (%) | 1394 (13.2%) | 1356 (15.1%) | – | – |
| Peak EGFR | ||||
| <30 (%) | 546 (5.2%) | 434 (4.8%) | 461 (6.2%) | 347 (5.5%) |
| 30–59 (%) | 1047 (9.9%) | 1159 (12.9%) | 800 (10.8%) | 862 (13.7%) |
| 60–89 (%) | 3002 (28.4%) | 2573 (28.7%) | 2143 (29%) | 1903 (30.3%) |
| ≥90 (%) | 5066 (47.9%) | 3896 (43.5%) | 3987 (53.9%) | 3171 (50.5%) |
| Missing values (%) | 910 (8.6%) | 895 (10%) | – | – |
| Clinical diagnostic codes | ||||
| Missing values | 1 | 2 | – | – |
Patients accrued a median 3.1 years (minimum 1 day, maximum 3.8 years) follow-up to either death or censorship. There were 4235 (21.7%) deaths post discharge, and 1011 (5.2%) died during the first 90 days post discharge. The final statistical model was fitted separately for men and women and included BMI, indicators of the clinical diagnostic categories; age; smoking status; loge(1 + number of urgent admissions in last five years); loge(1 + total number of complex admissions during the last five years); minimum albumin; peak urea; peak white blood cell count; peak sodium; minimum platelet count; indicators for the four-category eGFR (<30, 30–59, 60–89, 90+); Index of Multiple Deprivation; whether immunosuppressants were prescribed; whether the admission was via A&E; main effects and interaction between whether admission was an emergency and whether intravenous drugs were given; and time-varying effects as interactions with loge(time) for emergency, age, minimum albumin, peak urea, peak white blood cell count, peak sodium, minimum platelet count, eGFR indicators and loge(1 + number of urgent admissions in last five years). Owing to substantial improvement in the model fit the main effects of BMI, age, albumin, urea, sodium, white blood cell count, platelets and IMD were included in the model using restricted cubic splines with four degrees of freedom for BMI and three for the other variables. Internal knots were placed at the quartiles for BMI and at the 33th and 67th centiles for the other covariates. In addition, boundary knots were placed at the extreme values of the covariate.
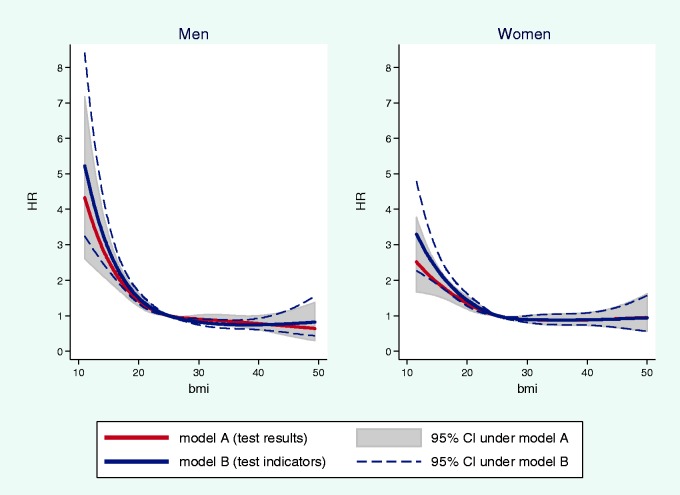
For both men and women, the relationship between BMI at discharge and the loge hazard of death was strongly non-linear (p = 0.0002 for women and p < 0.0001 for men) and predictive (both p < 0.0001). No evidence was found for a time-varying effect of BMI (p = 0.4 for both men and women). Figure 1 shows the estimated gender-specific hazard ratio curves and 95% CIs for BMI. The reference BMI value was set to 25 in order to illustrate the effects of being considered overweight. For both genders, the hazard ratio steeply decreases for BMIs up to 25 and then levels off, although the curve below a BMI of 20 kgm−2 for men is much steeper than the corresponding curve for women. For women, the best fit hazard ratio curve begins to increase gently above a BMI of about 40 kgm−2 while the corresponding curve for men continues to fall over all values of BMI over 25 kgm−2.
Figure 1.
Gender-specific hazard ratio curves and 95% confidence intervals for BMI (reference BMI value = 25).
The analysis was then repeated separately for younger (age < 65 years) and older (age ≥ 65 years) patients to evaluate whether there might be a differential effect of BMI on mortality by age group. No evidence was found of an interaction between BMI and age group.
In order to include into the analysis as many patients as possible we carried out a further sensitivity analysis where we used the blood test indicators (i.e. whether the patient had the blood test or not) instead of the observed blood test values. This allowed us to include 3848 additional records: 2028 for men and 1820 for women. Figure 2 compares the hazard ratios for BMI and their 95% CIs obtained from the models with either the blood test results or the blood test indicators. The two modelling strategies provided similar results.
Figure 2.
Gender-specific hazard ratio curves and 95% confidence intervals for BMI (reference BMI value = 25) obtained from the models with either the blood test results or the blood test indicators.
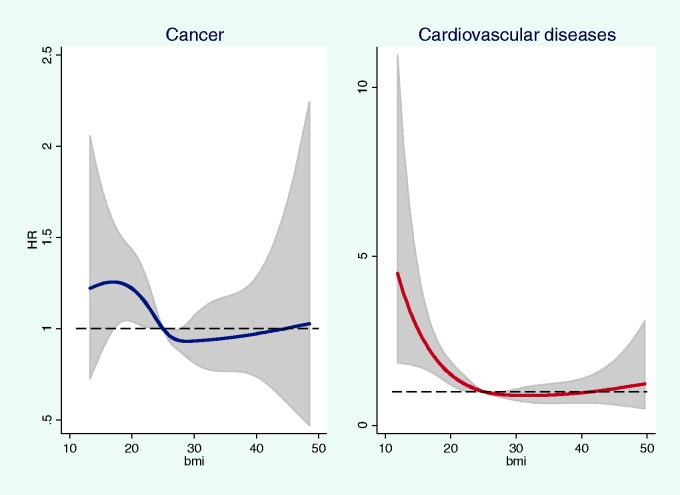
For patients with a cancer-related admission, the model provided no evidence of increased risk, with BMI over 25 kgm−2 being on average protective and lower BMI being associated with a poor outcome (Figure 3). For patients with a cardiovascular-related admission, there was no evidence of increased risk associated with BMI > 25 kgm−2 and the curve only recrossed 1 at a BMI of about 40 kgm−2. Patients with a BMI < 25 kgm−2 were at markedly increasing risk of death (Figure 3).
Figure 3.
Hazard ratios and 95% confidence intervals for BMI in cancer patients and in patients with cardiovascular diseases (reference BMI value = 25).
Conclusions
There is little evidence from our study to support current aspirational BMI targets for patients being discharged from hospital. Lower BMI on discharge is associated with a substantially increased hazard of death. For all patients, and for the subgroup with a diagnosis of cancer, there is no evidence of an increased risk of death at higher BMI on discharge, although there is increasing uncertainty at higher BMI levels. For cardiovascular disease, we observed a small increase in the risk of death with higher BMI values, although this did not become apparent until above about 40 kgm−2 and was not statistically convincing. Our study suggests that the current advice for patients discharged from an acute hospital should be updated as, contrary to the current national BAPEN guidance,6 optimal BMI for patients across all disease groups and for specific disease cohorts is higher than currently advocated.
Across all disease cohorts, a J-shaped relationship was observed between BMI and the relative hazard of death, indicating that higher BMI values did not pose any greater hazard of death compared to current perceived optimal BMI values. Even for cardiac disease groups, there was only a slight and uncertain elevation of risk above 25 kgm−2 with increasing BMI. Our work replicates the findings for patients with coronary artery disease and importantly extends the findings from Romero-Corral et al.15 from patients with coronary artery disease to all patients admitted to hospital, representing about 15.5 million admissions per year in England in 2013–2014.16
Most studies of the relationship between BMI and mortality have focused on the general population and emphasised the role of smoking and chronic illness as potential sources of bias.2,3 This has led some authors to exclude patients with these characteristics from their analyses to demonstrate a strong association between overweight, BMI and mortality,17 and these findings have been generalised to the whole population as the basis for nutritional guidance.
Compared to the general population, patients in our study were older (median age 60 years versus 40 years for the UK population) and less overweight with a median BMI of 26. Study participants often had multiple morbidities, demonstrated by the frequency of complex hospital admissions in the prior five years. About one-quarter of patients died during follow-up. Population-based estimates of the mortality risk associated with being overweight and obese are unlikely to be generalisable to patients in hospital for whom achieving a BMI target within the normal range may confer little benefit.
The protective effect of overweight and obesity in patients admitted to hospital may reflect the benefits of higher metabolic reserves,18 particularly for patients with prolonged hospital stay or those admitted to intensive care where weight loss is common. We reported the last BMI recorded in hospital rather than self-reported values of weight and height to reduce systematic error and bias.
Strengths
The linked data upon which our study is based are extensive and high quality, representing a unique holding in the UK. They reflect real-world patient experience in a multicultural setting with mortality data derived from the Office of National Statistics death certification records. We had access to very detailed information with which to address case-mix including the nature of the admission and previous NHS admissions, diagnosis, prescribing test results and investigations, and social deprivation. In addition, there were few missing data for BMI and for other explanatory variables individually. We undertook extensive supportive/sensitivity analyses and all provided similar results for the relationship between BMI and the risk of death in follow-up.
Limitations
As an observational analysis, the study reflects the outcome for patients when they are discharged at a given BMI. It could be argued that the relationship between lower weight and higher mortality risk reflected severity of disease and weight loss during admission, with weight being a marker of severity or frailty, and not becoming ‘otherwise ignorable’ after conditioning in the full model. Nonetheless, our models provide little evidence of higher risk even for obese individuals. The median follow-up period for study participants was 3.1 years, so we were unable to assess whether a BMI value within the normal range was associated with accrued health benefits in the longer term. However, our objective was to determine whether aspirational BMI targets are justified for patients discharged from hospital; given that one-quarter of these individuals will die within the three years following discharge from hospital.
In our study, the incompleteness in the blood tests variables depends on the unobserved values of the variables themselves. We excluded patients with missing data and this is likely to have excluded healthier patients because those who are less unwell have fewer clinical investigations. However, we argue that in our setting, conditional on the model’s predictors, it is plausible to assume independence between the missingness and the outcome. Under this conditional independence assumption, White and Carlin14 showed that complete records analysis delivers valid estimates of the regression coefficients. The robustness of our conclusions was corroborated by sensitivity analyses.
In conclusion, our study found no support for low, aspirational, BMIs among adult patients on discharge from hospital after a full admission. BMI below 25 kgm−2 was always associated with and increased risk of poor outcomes in our study, and for such patients adequate hospital nutrition should be ensured.
Declarations
Competing Interests
None declared.
Funding
This paper presents independent research which is funded in part by the National Institute for Health Research (NIHR)’s School for Public Health Research (SPHR), which funds MF and contributes to NF. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Ethical approval
Registered as an Audit at University Hospital Birmingham NHS Trust.
Guarantor
NF
Contributorship
NF had the original idea, conducted the statistical analyses and wrote the first draft of the paper; DR helped design the study, facilitated access to the linked data sets and reviewed the final version of the paper; MF conducted statistical analyses and revised the paper; DM helped design the study, facilitated access to the linked data sets and reviewed the final version of the paper; LS helped design the analysis and provided clinical input to the design and presentation of the results, and reviewed the final version of the paper; JW helped design and interpret the statistical analyses, and reviewed the final version of the paper; DP helped design the study, helped interpret the clinical implications and reviewed the final version of the paper.
Acknowledgements
None
Provenance
Not commissioned; the article was revised in accordance with peer review comments from a previous submission to another journal.
References
- 1.Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess 2004; 8: iii–iv, 1–182–iii–iv, 1–182. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013; 309: 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763–778. [DOI] [PubMed] [Google Scholar]
- 4.Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in Korean men and women. N Engl J Med 2006; 355: 779–787. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index to diagnose obesity in the US adult population. Int J Obes 2008; 32: 959–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.British Association for Parenteral and Enteral Nutrition. See http://www.bapen.org.uk/pdfs/must/bmi-weight-loss-charts/must-table-up-to-100kg.pdf (last checked 27 February 2016).
- 7.NHS Choices. See http://www.nhs.uk/Services/Trusts/Overview/DefaultView.aspx?id=1470 (last checked 27 February 2016).
- 8.Clinical Classification System Group. See http://www.hcup-us.ahrq.gov/toolssoftware/icd_10/ccs_icd_10.jsp (last checked 27 February 2016).
- 9.Clinical Indicators Team. Indicator Specification: Summary Hospital Level Mortality Indicator, London, UK: The Information Centre for Health and Social Care, Department of Health, 2012. [Google Scholar]
- 10.Department for Communities and Local Government (2011). The English Indices of Deprivation 2010. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/6320/1870718.pdf (last checked 27 February 2016).
- 11.Cox DR. Regression models and life tables. J R Stat Soc 1972; 34: 187–220. [Google Scholar]
- 12.Harrell FE., Jr Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis, New York, NY: Springer, 2001. [Google Scholar]
- 13.Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control 1974; 19: 716–723. [Google Scholar]
- 14.White IR, Carlin JB. Bias and efficiency of multiple imputation compared with complete-case analysis for missing covariate values. Stat Med 2010; 28: 2920–2931. [DOI] [PubMed] [Google Scholar]
- 15.Romero-Corral A, Montori VA, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 2006; 368: 666–678. [DOI] [PubMed] [Google Scholar]
- 16.Health and Social Care Information Centre. See http://www.hscic.gov.uk/article/2021/Website-Search?productid=16572&q=Health+survey+for+England+&sort=Relevance&size=10&page=1&area=both#top (last checked 27 February 2016).
- 17.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan PHL, MacInnis RJ, et al. Body mass index and mortality among 1.46 million white adults. N Engl J Med 2010; 363: 2211–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese—a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol 2010; 65: 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]