Highlights
-
•
Malignant Peripheral Nerve Sheath Tumor is a rare type of soft tissue malignant tumor that occurs in only 5% of cases.
-
•
Among mediastinal tumors, only 18.8% occur primarily in the nerves, and of these, only 10.3% are malignant.
-
•
We studied six cases of mediastinal primary malignant peripheral nerve sheath tumors in which surgery was carried out.
-
•
Nerve sheath tumors localized within the membrane offer good long-term prognosis even if malignant.
-
•
Furthermore, long-term survival is possible even if the tumor has invaded neighboring organs, provided it can be completely excised.
Keywords: Malignant peripheral nerve sheath tumor, MPNST, Surgery, Malignant schwannoma, Mediastinal tumor
Abstract
Introduction
Malignant Peripheral Nerve Sheath Tumor is a rare type of soft tissue malignant tumor that occurs in only 5% of cases. It tends to occur in the arms and legs and trunk of the body, with mediastinal occurrence in only a few cases. Among mediastinal tumors, only 18.8% occur primarily in the nerves, and of these, only 10.3% are malignant, with very few reports indicating the long-term progress of patients with MPNST of the mediastinum.
Case presentation
We studied six cases of mediastinal primary malignant peripheral nerve sheath tumors in which surgery was carried out at this Center between 1977 and 2000. Four of the cases were men and two were women. The period of observation was between 14 and 277 months and the median follow-up time was 119.5 months. The tumors were contained in a membrane and completely excisable in three cases, with the patient demonstrating long-term survival with no recurrence in each case. The remaining three cases were not completely excisable due to invasion into the aorta. In two cases, the patients were treated post-surgically with chemotherapy; however, in all three cases the patient died as a result of the original condition.
Discussion and conclusions
Nerve sheath tumors localized within the membrane offer good long-term prognosis even if malignant. Furthermore, long-term survival is possible even if the tumor has invaded neighboring organs, provided it can be completely excised. In cases where complete excision is difficult, a multidisciplinary approach including radiotherapy and anti-cancer drug treatment may contribute to improved prognosis but this is a subject that requires further study.
1. Introduction
Malignant Peripheral Nerve Sheath Tumor (MPNST) is a rare type of soft tissue malignant tumor that occurs in only 5% of cases [1]. It tends to occur in the arms and legs and trunk of the body, with mediastinal occurrence in only a few cases [1]. Among mediastinal tumors, only 18.8% occur primarily in the nerves, and of these, only 10.3% are malignant, with very few reports indicating the long-term progress of patients with MPNST of the mediastinum [2]. In this study, the authors considered the long-term surgical results of six cases of MPNST treated surgically at this hospital.
2. Presentation of cases
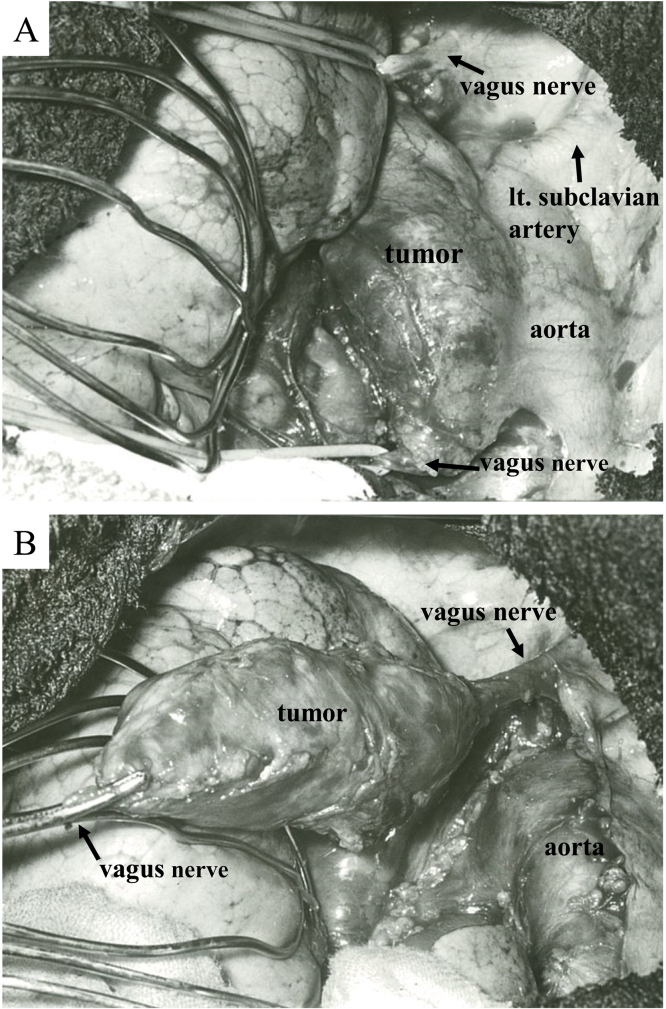
We studied the long-term progress of six patients undergoing surgery at this Center between 1977 and 2000 for mediastinal primary malignant peripheral nerve sheath tumors. Four of the patients were men and two were women. Their ages ranged from 17 to 72 years (averaging 51 years). The primary location was the anterior mediastinum in three cases, middle mediastinum in one case and superior mediastinum in two cases. The tumor diameter was between 70 and 150 mm (average 101.8 mm). (Table 1) The period of observation was between 14 and 277 months and the median follow-up time was 119.5 months. None of the cases had a diagnosis prior to surgery; however, swift diagnosis during surgery led to suspicion of a malignant nerve sheath tumor. In three of the six cases (Cases 2, 4 and 5) the tumor was enclosed in a membrane, with no invasion of the surrounding area, enabling complete excision thereof (Fig. 1). Cases 2 and 4 were treated with surgery alone, while Case 5 went on to undergo radiotherapy. All three of these cases went on to have long-term survival of ten years or more with no recurrence. The remaining three cases (Cases 1, 3 and 6) involved invasion into the aorta and could not be completely excised. In Case 6, the lung and aorta were also excised, but surgical margins were positive. In Cases 1 and 3, the patients were post-surgically treated with chemoradiotherapy, but in Case 6, no further treatment was carried out because of the poor physical state of the patient. All three of these patients died from the original condition (Table 2).
Table 1.
Mediastinal MPNST:characteristics.
| Case | Age | Sex | Symptoms | Location | Size(mm) | Preoperative diagnosis |
|---|---|---|---|---|---|---|
| 1 | 17 | M | Back pain, Cough | P | 150 | Neurogenic tumor |
| 2 | 65 | M | – | S | 75 | Mediastinal tumor |
| 3 | 50 | M | Back pain | P | 70 | Neurogenic tumor |
| 4 | 45 | F | Chest oppression, Cough | M | 86 | Lung tumor |
| 5 | 55 | F | – | S | 110 | Mediastinal tumor |
| 6 | 72 | M | Back pain | P | 120 | Schwannoma |
P: posterior mediastinum, S: superior mediastinum, M, middle mediastinum.
Fig. 1.
(A) Intraoperative image of case 4. The tumor originated from the vagus nerve. (B) Intraoperative image of case 4. The tumor could be smoothly detached from the aorta.
Table 2.
Treatment and outcome.
| Case | Surgical approach | Surgical treatment | CT | RT | Recurrence | Follow-up (months) |
|---|---|---|---|---|---|---|
| 1 | PL | Extirpation (incomplete) | + | 40 | Local, brain | 69, death |
| 2 | MS | Extirpation | − | − | − | 170, deatha |
| 3 | PL | Exploratory thoracotomy | + | 70 | 14, death | |
| 4 | PL | Extirpation | − | − | − | 277, alive |
| 5 | MS | Extirpation | − | 46 | − | 255, alive |
| 6 | PL | Extirpation | − | − | local | 18, death |
CT: Chemotherapy, RT: Radiotherapy, PL: posterolateral, MS: median sternotomy.
Died of other disease.
3. Discussion
The five-year survival rate for MPNST is between 34 and 43.7%. Localized recurrence after excision is 46–65%, with the distal metastasis rate considered between 40 and 68% [3], [4], [5]. Factors in poor prognosis include: 1. Age at onset of 30 or lower; 2. Large tumor diameter; 3. Occurrence inside the trunk; 4. Complicated by nerve fiber tumor type 1; and 5. Incomplete excision, with the three cases in this study that died having factors 2, 3 and 5 [3], [4], [6]. During treatment of MPNST, it is important to completely surgically excise the tumor. In the cases in this study, the three patients whose tumors were enclosed in a membrane and could be completely excised all survived with no recurrence. Many tumors occur on the surface of the limbs or trunk, allowing them to be discovered early and completely excised; however, those occurring inside the chest or abdomen take longer for the symptoms to express and in many cases discovery is delayed, meaning that the tumor grows and in many cases can no longer be completely excised upon discovery, or may be inoperable. Chemotherapy or radiotherapy has conventionally been implemented on cases in which complete excision cannot be performed, or inoperable cases; however, the results are insufficiently effective. More recently, however, reports note cases in which high dose Ifosfamide, vincristine, doxorubicin, cyclophosphamide have been notably effective, as well as cases in which post-surgery high dose radiation was effective, and those in which boron neutron capture therapy has been effective [7], [8], [9]. In the future, further studies need to be conducted to establish the effectiveness of these therapies. In Case 1 in this study, the patient was post-surgically treated with 60 Gy radiotherapy and cyclophosphamide, along with the anticancer drug cisplatin, which yielded temporary results, achieving survival for 69 months.
4. Conclusion
This study considered the long-term surgical results in six cases of mediastinally occurring MPNST treated at this hospital. MPNST localized within the membrane, which can be completely excised, offer good long-term prognosis. Furthermore, long-term survival is possible even if the tumor has invaded neighboring organs, providing it can be completely excised. In cases where complete excision is difficult, a multidisciplinary approach including radiotherapy and anti-cancer drug treatment may contribute to improved prognosis but this is a subject that requires further study.
Conflict of interest
The authors report no conflict of interest.
Funding
None.
Consent
Informed and written consent has been given by patients.
References
- 1.Lewis J.J., Brennan M.F. Soft tissue sarcomas. Curr. Probl. Surg. 1996;33:817–872. [PubMed] [Google Scholar]
- 2.Wada H., Teramatsu T. Mediastinal tumors—a statistical nationwide report of 1546 cases between July, 1975 and May, 1979 in Japan. Gen. Thorac. Cardiovasc. Surg. 1982;30:374–378. [PubMed] [Google Scholar]
- 3.Ducatman B.S., Scheithauer B.M., Piepgras D.G., Reiman H.M., Ilstrup D.M. Malignant peripheral nerve sheath tumors: a clinicopathologic study of 120 cases. Cancer. 1986;57:2006–2021. doi: 10.1002/1097-0142(19860515)57:10<2006::aid-cncr2820571022>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Wanebo J.E., Malik J.M., VandenBerg S.R., Wanebo H.J., Driesen N. Malignant peripheral sheath tumors A clinicopathologic study of 28 cases. Cancer. 1993;71:1247–1252. doi: 10.1002/1097-0142(19930215)71:4<1247::aid-cncr2820710413>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 5.Weiss S.W., Goldblum J.R. 4th ed. Mosby; St. Louis: 2001. Enzinger and Weiss’s Soft Tissue Tumors. [Google Scholar]
- 6.Meis J.M., Enzinger F.M., Martz K.L., Neal J.A. Malignant peripheral nerve sheath tumors (malignant schwannomas) in children. Am. J. Surg. Pathol. 1992;16:694–702. doi: 10.1097/00000478-199207000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Masui F., Yokoyama S., Beppu Y., Asanuma K., Fujii K. A malignant peripheral nerve-sheath tumor responding to chemotherapy. J. Bone Joint Surg. Br. 2004;86-B:113–115. [PubMed] [Google Scholar]
- 8.Yone K., Ijiri K., Hayashi K., Yokouchi M., Takenouchi T. Primary malignant peripheral nerve sheath tumor of the cauda equina in a child case report. Spinal Cord. 2004;42:199–203. doi: 10.1038/sj.sc.3101567. [DOI] [PubMed] [Google Scholar]
- 9.Inoue M., Lee C.M., Ono K., Suzuki M., Tokunaga T. Clinical effectiveness of boron neutron capture therapy for a recurrent malignant peripheral nerve sheath tumor in the mediastinum. J. Thorac. Oncol. 2010;5 doi: 10.1097/JTO.0b013e3181f1cd86. 2037–2010. [DOI] [PubMed] [Google Scholar]