Abstract
BACKGROUND:
Incidence of postoperative pulmonary complications (PPC) in patients undergoing non-cardiothoracic surgery remains high and the occurrence of these complications has enormous implications for the patient and the health care system.
AIM:
The aim of the study was to identify risk factors for PPC in patients undergoing abdominal surgical procedures.
MATERIALS AND METHODS:
A prospective cohort study in abdominal surgical patients, admitted to the emergency and surgical ward of the UHC of Tirana, Albania, was conducted during the period: March 2014-March 2015. We collected data on the occurrence of a symptomatic and clinically significant PPC using clinical, laboratory, and radiology data. We evaluated the relations between PPCs and various pre-operative or intra-operative factors to identify risk factors.
RESULTS:
A total of 450 postoperative patients admitted to the surgical emergency and surgical ward were studied. The mean age were 59.85 ±13.64 years with 59.3% being male. Incidence of PPC was 27.3% (123 patients) and hospital length of stay was 4.93 ± 4.65 days. Length of stay was substantially prolonged for those patients who developed PPC (7.48 ± 2.89 days versus 3.97± 4.83 days, p < 0.0001. PPC were identified as risk factors for mortality, OR: 21.84; 95% CI: 11.66-40.89; P < 0.0001. The multivariate regression analysis identified as being independently associated with an increased risk of PPC: age ≥ 65 years (OR 11.41; 95% CI: 4.84-26.91, p < 0.0001), duration of operation ≥ 2.5 hours (OR 8.38; 95% CI: 1.52-46.03, p = 0.01, history of previous pulmonary diseases (OR 11.12; 95% CI: 3.28-37.65, P = 0.0001) and ASA > 2 (OR 6.37; 95% CI: 1.54-26.36, P = 0.01).
CONCLUSION:
We must do some efforts in reducing postoperative pulmonary complications, firstly to identify which patients are at increased risk, and then following more closely high-risk patients because those patients are most likely to benefit.
Keywords: postoperative, pulmonary, complications, risk factor, abdominal surgery
Introduction
Incidence of postoperative pulmonary complications in patients undergoing non-cardiothoracic surgery remains high [1] and the occurrence of these complications has enormous implications for the patient and the health care system [2].
Postoperative pulmonary complications (PPC) occur in 2% to 40% of patients and are associated with increased morbidity, mortality, and length of hospital stay [2-4].
In our country, there is no study about the incidence and risk factors for PPC. Previous international studies demonstrated that the majority of risk factors for PPC can be intervened and improved, [5, 6] so identifying which patients are at increased risk, we can reduce postoperative pulmonary complications. Studies have shown that pulmonary complications make the second most serious morbidity after cardiovascular event, one in four deaths occurring within a week of surgery is related to pulmonary complications [7]. Already has been explored that identifying perioperative risk factors of PPC is an important step toward improving quality of care in surgical patients [8-10]. The National Surgical Quality Improvement Program that compared hospitalization costs and length of stay among patients with various postoperative complications found that pulmonary complications were by far most costly [4]. So identifying patients at risk for pulmonary complications and developing a strategy to reduce the risk is clearly worthwhile [11].
The aim of the study was to identify risk factors for postoperative pulmonary complications in patients undergoing abdominal surgical procedures.
Materials and Methods
Study design and patient population
A prospective cohort study in abdominal surgical patients, admitted to the emergency and surgical ward of the University Hospital Centre “Mother Teresa” of Tirana, Albania, was conducted during the period: March 2014-March 2015. Throughout this period, consecutive patients aged > 18 years that underwent abdominal surgery and stayed in the hospital for more than 24 hours were enrolled in the study. The exclusion criteria: pregnancy, patients with preoperatively intubated trachea, and patients who underwent thoracoabdominal incision.
This study was approved by the Ethics Committee of the University of Medicine, Tirana, Albania. It has been performed in accordance with the ethical standards displayed in the 1964 Declaration of Helsinki and its later amendments. Data were made anonymous for analysis.
Demographic and medical information
Demographic and medical information including sex, age, date of hospital admission, diagnosis, and type of hospital admission (emergency or elective) ASA (American Society of Anesthesiologists) class were collected [12]. The ASA classification is a general index of overall morbidity that ranges from class 1 (normal healthy patient) to class 5 (moribund patient who is not expected to survive without the operation) and class 6 (declared brain-dead patient whose organs are being removed for donor purposes). We recorded history of chronic obstructive pulmonary disease (COPD) and history of asthma as preexistence of pulmonary diseases.
Postoperative pulmonary complications
We collected data on the occurrence of a symptomatic and clinically significant postoperative pulmonary complication using clinical, laboratory, and radiology data. These included: respiratory failure requiring mechanical ventilation, pneumonia. [13], macroscopic atelectasis (by chest radiography), and pneumothorax, mass pleural effusion requiring percutaneous intervention.
Length of hospital stay was measured in days, from the day of hospital admission to the time of discharge or death.
Data were collected prospectively to determine ICU admission and stay, and mortality.
We evaluated the relations between PPCs and various pre-operative or intra-operative factors to identify risk factors.
Statistical analysis
Continuous variables were presented as the mean ± SD (standard deviation). Categorical variables were expressed as actual numbers (n) and percentages (%). Linear and logistic regression was conducted to test the relation between the postoperative pulmonary complications (PPC) and other variables. Multivariate analysis was conducted using a logistic regression model in which “postoperative pulmonary complication” was used as the dependent variable. Only the variables associated with PPC that yielded P-values lower than 0.10 in the initial analysis were used in the stepwise logistic regression analysis. Odds ratios (OR) and 95% confidence intervals (95% CIs) were used to estimate the association between PPC and other variables.
Also, this model was used to analyze the effect of PPC on the length of hospital stay and mortality. Chi-square analysis was applied to compare frequencies between subgroups, and Student’s t-tests, or non-parametric tests when necessary, were employed for quantitative variable analysis.
Statistical significance was considered at the level of p ≤ 0.05. All tests were two tailed. SPSS 15.0 statistical package used to analyze the data.
Results
A total of 450 postoperative patients admitted to the surgical emergency and surgical ward were studied. The mean age was 59.85 ± 13.64 years (range: 27-86) with 59.3% (n = 267) being male.
Incidence of PPC was 27.3% (123 patients) and hospital length of stay was 4.93 ± 4.65 days. Length of hospital stay was substantially prolonged for those patients who developed postoperative pulmonary complications (7.48 ± 2.89 days versus 3.97 ± 4.83 days, p < 0.0001, (Figure 1).
Figure 1.
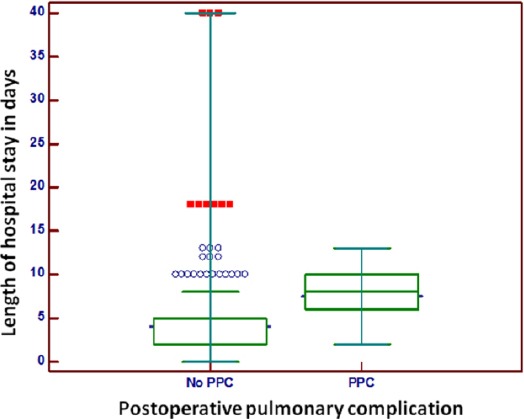
Length of hospital stay in days according to the developing of postoperative pulmonary complications (PPC).
Average age was significantly higher in those with PPC compared to those without (64.93 ± 13.87 and 59.68 ± 15.37, respectively) (Figure 2).
Figure 2.
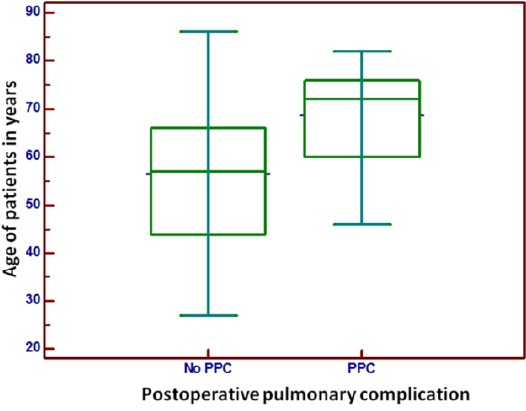
Incidence of postoperative pulmonary complications (PPC) according to the age of patients in years.
Seventy five (75) patients (16.7%) were deemed by the anesthesiologist to be American Society of Anesthesiologists (ASA) class 3 or 4, with increasing of ASA class level was increased the incidence of PPC (Table 1 and Figure 3).
Table 1.
Postoperative pulmonary complications according to the level ASA class of the patients
| ASA class 1 No of patients | ASA class 2 No of patients | ASA class 3 No of patients | ASA class 4 No of patients | |
|---|---|---|---|---|
| Patients without PPC | 219 | 96 | 12 | 0 |
| Patients with PPC | 24 | 36 | 60 | 3 |
Figure 3.
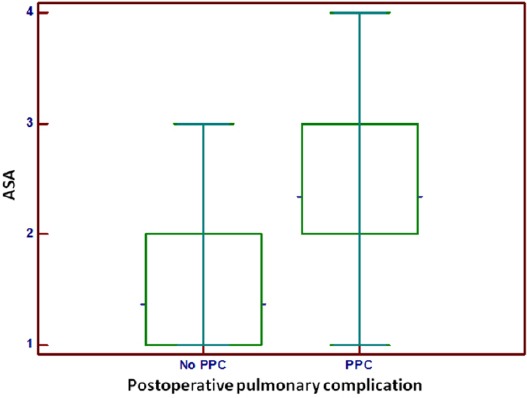
Incidence of postoperative pulmonary complications (PPC) according to the ASA class of the patients preoperatively.
The results of univariate analyses are outlined in Table 2. 90 patients (73.17% of the patients who developed postoperative pulmonary complications) were transferred to the Intensive Care Unit. Hospital mortality was 17.3% (n = 78) and 60 patients (48.78%) of the patients who developed postoperative pulmonary complications died.
Table 2.
Results of univariate analysis for significant risk factors for PPC
| Variable | No. of patients (%) | No. of patients with particular finding | OR (95% CI) | P Value |
|---|---|---|---|---|
| Male gender | 267 (59.3%) | 84 | 1.69 (1.09-2.62) | 0.018 |
| Age ≥ 65 yr | 180 (40%) | 87 | 6.08 (3.85-9.60) | < 0.0001 |
| Emergency admission | 63 (14%) | 63 | 687.47 (41.96-11262.8) | < 0.0001 |
| Current smoking | 153 (34%) | 60 | 2.39 (1.56-3.67) | 0.0001 |
| Presence of malignant disease | 138 (30.7%) | 66 | 4.10 (2.63-6.37) | < 0.0001 |
| Preexistence of pulmonary diseases | 60 (13.3%) | 51 | 25.02 (11.78-53) | < 0.0001 |
| ASA class > 2 | 75 (16.7%) | 63 | 27.56 (14.01-54.2) | < 0.0001 |
| Estimated bleeding during surgical procedure ≥ 500 mL | 63 (14%) | 39 | 5.86 (3.33-10.29) | < 0.0001 |
| Pre-operative blood transfusion | 33 (7.3%) | 24 | 8.56 (3.85-19.03) | < 0.0001 |
| Intra and post-operative blood transfusion | 72 (16%) | 45 | 6.41 (3.74-10.98) | < 0.0001 |
| Duration of operation ≥ 2.5 hours | 162 (36%) | 90 | 9.65 (5.99-15.56) | < 0.0001 |
| Perioperative nasogastric tube | 358 (79.6%) | 118 | 8.55 (3.38-21.63) | < 0.0001 |
PPC: post-operative pulmonary complication; OR: odds ratio; CI: confidence interval
PPC were identified as risk factors for mortality, OR: 21.84; 95%CI: 11.66-40.89; P < 0.0001. The multivariate regression analysis identified as being independently associated with an increased risk of postoperative pulmonary complications: age ≥ 65 years (OR 11.41; 95% CI: 4.84-26.91, p < 0.0001), duration of operation ≥ 2.5 hours (OR 8.38; 95%CI: 1.52-46.03, p = 0.01, history of previous pulmonary diseases (OR 11.12; 95%; CI: 3.28-37.65, P = 0.0001) and ASA class 3, or ASA class 4 (OR 6.37; 95% CI: 1.54-26.36, P = 0.01).
Discussion
The present study found that there was high incidence of PPC. This incidence is comparable with the incidence of PPC in high risk patients, because we excluded patients that stayed < 24 hour in the hospital. However, respiratory complications occur within 48-72 h following surgery [14].
Perioperative variables associated with postoperative pulmonary complications were: male gender, age ≥ 65 years, emergency admission, current smoking, presence of malignant disease, preexistence of pulmonary diseases, estimated bleeding during surgical procedure ≥ 500 mL, perioperative blood transfusion, duration of operation ≥ 2.5 hours and perioperative placement of nasogastric tube. However, only four of these variables were independently associated with increased risk after multivariate analysis: age ≥ 65 years, duration of operation ≥ 2.5 hours, history of previous pulmonary diseases and ASA > 2.
As it has been reported, we found significant associations between age, history of previous pulmonary disease and postoperative pulmonary complications [9, 14]. Although those are unmodifiable risk factors, a post-operative meticulous management can prevent progression to severe complications in these patients.
Our findings showed that ASA > 2 is a risk factor [15]. Several studies have shown that duration of surgery is an independent risk predictor for PPC, and the present study confirmed this finding [2, 16-18].
In our study we found that a previous pulmonary disease is a risk factor for PPC. Our findings are consistent with other studies that have shown a correlation between COPD, asthma and PPC [17].
PPC occur more often in males than in females, a possible explanation being that men tend to breathe more with their diaphragm and women more with their thorax; thus when the movements of the diaphragm are restricted after upper abdominal operations the males suffer more from lack of expansion of the lungs [19].
In our clinical practice we use routine nasogastric decompression. Our study, like other studies, [2, 20, 21] showed that placement of a nasogastric tube perioperatively increases the risk of pulmonary complications. These findings supports the selective nasogastric decompression only when it is judged to be necessary on clinical grounds [2], leading to the reduction of PPC [6].
The present study showed that smoking history correlates with pulmonary complications. [9, 14, 16, 22]. The presence of PPC lead to prolonged hospital stay and increased mortality rate, as in other studies [2, 23].
One limitation of the study was that we didn’t evaluate the risk factors for PPC independently for each type of surgery.
In conclusion, the present study found that there was high incidence of PPC which increased hospital length of stay and hospital mortality in the abdominal surgery. We identified twelve factors associated with the occurrence of PPC. We must do some efforts in reducing postoperative pulmonary complications, firstly to identify which patients are at increased risk, and then following more closely high-risk patients because those patients are most likely to benefit. We have demonstrated some perioperative factors that can be used to identify patients at increased risk for postoperative pulmonary complications after abdominal surgery.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Rock P, Rich PB. Postoperative pulmonary complications. Curr Opin Anaesthesiol. 2003;16:123–31. doi: 10.1097/00001503-200304000-00004. http://dx.doi.org/10.1097/00001503-200304000-00004 . PMid: 17021450. [DOI] [PubMed] [Google Scholar]
- 2.McAlister FA, Bertsch K, Man J, Bradley J, Jacka M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. The American Journal of Respiratory and Critical Care Medicine. 2005;171(5):514–517. doi: 10.1164/rccm.200408-1069OC. http://dx.doi.org/10.1164/rccm.200408-1069OC . PMid: 15563632. [DOI] [PubMed] [Google Scholar]
- 3.Shander A, Fleisher LA, Barie PS, Bigatello LM, Sladen RN, Watson CB. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Critical Care Medicine. 2011;39(9):2163–2172. doi: 10.1097/CCM.0b013e31821f0522. http://dx.doi.org/10.1097/CCM.0b013e31821f0522 . PMid: 21572323. [DOI] [PubMed] [Google Scholar]
- 4.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. http://dx.doi.org/10.1016/j.jamcollsurg.2004.05.276 . PMid: 15454134. [DOI] [PubMed] [Google Scholar]
- 5.Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Annals of Internal Medicine. 2006;144(8):575–580. doi: 10.7326/0003-4819-144-8-200604180-00008. http://dx.doi.org/10.7326/0003-4819-144-8-200604180-00008 . PMid: 16618955. [DOI] [PubMed] [Google Scholar]
- 6.Lawrence VA, Cornell JE, Smetana GW. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Annals of Internal Medicine. 2006;144:596–608. doi: 10.7326/0003-4819-144-8-200604180-00011. http://dx.doi.org/10.7326/0003-4819-144-8-200604180-00011 . PMid: 16618957. [DOI] [PubMed] [Google Scholar]
- 7.Fischer SP, Bader AM, Sweitzer BJ. Miller’s Anaesthesia. 7th ed. Ch. 34. New York: Churchill Livingstone; 2010. Preoperative evaluation; pp. 1019–22. http://dx.doi.org/10.1016/b978-0-443-06959-8.00034-0 . [Google Scholar]
- 8.Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–1350. doi: 10.1097/ALN.0b013e3181fc6e0a. http://dx.doi.org/10.1097/ALN.0b013e3181fc6e0a . PMid: 21045639. [DOI] [PubMed] [Google Scholar]
- 9.Arozullah AM, Khuri SF, Henderson WG, Daley J for the Participants in the National Veterans Affairs Surgical Quality Improvement Program. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Annals of Internal Medicine. 2001;135:847–857. doi: 10.7326/0003-4819-135-10-200111200-00005. http://dx.doi.org/10.7326/0003-4819-135-10-200111200-00005 . PMid: 11712875. [DOI] [PubMed] [Google Scholar]
- 10.Canet J, Gallart L. Predicting postoperative pulmonary complications in the general population. Current Opinion in Anaesthesiology. 2013;26(2):107–115. doi: 10.1097/ACO.0b013e32835e8acd. http://dx.doi.org/10.1097/ACO.0b013e32835e8acd . PMid: 23407154. [DOI] [PubMed] [Google Scholar]
- 11.Smetana GW. Postoperative pulmonary complications: An update on risk assessment and reduction. Cleveland Clinic Journal Of Medicine. 2009;76(Supplement 4):S60–S65. doi: 10.3949/ccjm.76.s4.10. http://dx.doi.org/10.3949/ccjm.76.s4.10 . PMid: 19880838. [DOI] [PubMed] [Google Scholar]
- 12.ASA Physical Status Classification System. American Society of Anesthesiologists. Available at https://www.asahq.org/For-Members/Clinical-Information/ASA-Physical-Status-Classification-System.aspx .
- 13.Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections. In: Olmsted RN, editor. APIC Infection Control and Applied Epidemiology: Principles and Practice. St. Louis: Mosby; 1996. pp. A–7. [Google Scholar]
- 14.Arozullah AM, Daley J, Henderson WG, Khuri SF for the National Veterans Administration Surgical Quality Improvement Program. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. Ann Surg. 2000;232:242–253. doi: 10.1097/00000658-200008000-00015. http://dx.doi.org/10.1097/00000658-200008000-00015 . PMid: 10903604 PMCid: PMC1421137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roizen MF, Fleisher LA. Anaesthetic implications of concurrent disease. In: Miller R, editor. Miller’s Anaesthesia. 7th ed. Ch. 35. New York: Churchill Livingstone; 2010. pp. 1103–11. [Google Scholar]
- 16.Toori KU, Khan JS, Nomani AZ, Hussain SW, Hashmi S. A prospective study of factors predicting PPC in patients undergoing non cardiothoracic surgery under general anaesthesia in developing country. Anaesth Pain Intensive Care. 2012;16:252–6. [Google Scholar]
- 17.Mark A. Yoder, Sat Sharma. William A, editor. [Last updated on 2013 Oct 2];Schwer, Medscape - Perioperative pulmonary management: e-medicine. Medscape.com/article 284983. [Google Scholar]
- 18.Smetna G. Preoperative pulmonary evaluation – Current concepts – A review article. N Engl J Med. 1999;340:937–44. doi: 10.1056/NEJM199903253401207. http://dx.doi.org/10.1056/NEJM199903253401207 . PMid: 10089188. [DOI] [PubMed] [Google Scholar]
- 19.Rosa Maria Salani Motab, Carvalhedo de Bruin PF, et al. Risk factors for pulmonary complications after emergency abdominal surgery. Respiratory Medicine. 2007;101:808–813. doi: 10.1016/j.rmed.2006.07.015. http://dx.doi.org/10.1016/j.rmed.2006.07.015 . PMid: 16963245. [DOI] [PubMed] [Google Scholar]
- 20.Sircar BN, Boston FK. Post-operative pulmonary complications. The British Medical Journal. 1940;82 doi: 10.1136/bmj.2.4150.82. http://dx.doi.org/10.1136/bmj.2.4150.82 . PMid: 20783206 PMCid: PMC2178986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall JC, Tarala RA, Hall JL. Respiratory insufficiency after abdominal surgery. Respirology. 1996;1:133–138. doi: 10.1111/j.1440-1843.1996.tb00022.x. http://dx.doi.org/10.1111/j.1440-1843.1996.tb00022.x . PMid: 9434329. [DOI] [PubMed] [Google Scholar]
- 22.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. http://dx.doi.org/10.1097/01.sla.0000133083.54934.ae . PMid: 15273542 PMCid: PMC1360123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell CK, Smoger SH, Pfeifer MP, Vogel RL, Pandit MK, Donnelly PJ, Garrison RN, Rothschild MA. Multivariate analysis of factors associated with postoperative pulmonary complications following general elective surgery. Arch Surg. 1998;133:194–198. doi: 10.1001/archsurg.133.2.194. http://dx.doi.org/10.1001/archsurg.133.2.194 . PMid: 9484734. [DOI] [PubMed] [Google Scholar]


