Abstract
BACKGROUND
Atrial fibrillation after cardiac surgery is associated with increased rates of death, complications, and hospitalizations. In patients with postoperative atrial fibrillation who are in stable condition, the best initial treatment strategy — heart-rate control or rhythm control — remains controversial.
METHODS
Patients with new-onset postoperative atrial fibrillation were randomly assigned to undergo either rate control or rhythm control. The primary end point was the total number of days of hospitalization within 60 days after randomization, as assessed by the Wilcoxon rank-sum test.
RESULTS
Postoperative atrial fibrillation occurred in 695 of the 2109 patients (33.0%) who were enrolled preoperatively; of these patients, 523 underwent randomization. The total numbers of hospital days in the rate-control group and the rhythm-control group were similar (median, 5.1 days and 5.0 days, respectively; P = 0.76). There were no significant between-group differences in the rates of death (P = 0.64) or overall serious adverse events (24.8 per 100 patient-months in the rate-control group and 26.4 per 100 patient-months in the rhythm-control group, P = 0.61), including thromboembolic and bleeding events. About 25% of the patients in each group deviated from the assigned therapy, mainly because of drug ineffectiveness (in the rate-control group) or amiodarone side effects or adverse drug reactions (in the rhythm-control group). At 60 days, 93.8% of the patients in the rate-control group and 97.9% of those in the rhythm-control group had had a stable heart rhythm without atrial fibrillation for the previous 30 days (P = 0.02), and 84.2% and 86.9%, respectively, had been free from atrial fibrillation from discharge to 60 days (P = 0.41).
CONCLUSIONS
Strategies for rate control and rhythm control to treat postoperative atrial fibrillation were associated with equal numbers of days of hospitalization, similar complication rates, and similarly low rates of persistent atrial fibrillation 60 days after onset. Neither treatment strategy showed a net clinical advantage over the other. (Funded by the National Institutes of Health and the Canadian Institutes of Health Research; ClinicalTrials.gov number, NCT02132767.)
In recent years, much research has focused on the prevention of atrial fibrillation after cardiac surgery, but highly effective interventions are lacking. Thus, postoperative atrial fibrillation remains the most common complication after cardiac surgery, with an incidence of 20 to 50%.1–4 This complication has major adverse consequences for patients and the health care system, including increased rates of death, complications, and hospitalizations and inflated costs.1–9 Therefore, efforts to determine the most effective preventive strategies and management practices are important. There are two general approaches to managing postoperative atrial fibrillation: heart-rate control (hereafter “rate control”) and rhythm control with the use of antiarrhythmic drugs, direct-current cardioversion, or both.
In the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) trial, in which investigators studied the use of rate control versus rhythm control in nonsurgical patients with atrial fibrillation, the use of rhythm control was shown to offer no survival advantage but was associated with more frequent hospitalizations and adverse drug effects.10 However, some studies involving patients with postoperative atrial fibrillation after cardiac surgery have suggested that rhythm control may offer advantages over rate control, although the evidence is inconclusive.3,11–13
The lack of consensus regarding best practices for the management of atrial fibrillation after cardiac surgery has led to major variations in practice patterns.1,3,14–16 Treatment approaches aim to reduce the severity of associated symptoms, limit adverse hemodynamic effects, decrease the length of hospital stay, prevent read-missions, and improve survival. Advocates of a rhythm-control strategy contend that a more rapid conversion to sinus rhythm might reduce thromboembolic risk, minimize exposure to anticoagulation, and restore functional capacity more quickly than rate control. Proponents of rate control counter that this approach averts the potential adverse effects of antiarrhythmic drugs and complications associated with cardioversion.
Determining the risks and benefits of rate control versus rhythm control for postoperative atrial fibrillation may provide information to improve clinical decision making and resource utilization for this highly prevalent condition. The Cardiothoracic Surgical Trials Network (CTSN), therefore, conducted a randomized trial to evaluate the effectiveness and safety of rate control versus rhythm control for new-onset atrial fibrillation or atrial flutter after cardiac surgery.
METHODS
TRIAL DESIGN AND OVERSIGHT
This trial was conducted at 23 sites in the United States and Canada; the institutional review board at each site approved the protocol. A coordinating center, independent adjudication committee, and data and safety monitoring board oversaw the progress of the trial. The investigators vouch for the fidelity of this report to the trial protocol, which is available with the full text of this article at NEJM.org.
PATIENTS AND INTERVENTIONS
The trial enrolled adult patients in hemodynamically stable condition who were undergoing elective cardiac surgery to treat coronary artery disease or heart-valve disease; none of the patients had a history of atrial fibrillation (see the eligibility criteria in the Supplementary Appendix, available at NEJM.org). All the patients provided written informed consent.
The patients were enrolled in the study and underwent randomization if they had postoperative atrial fibrillation that persisted for more than 60 minutes or recurrent episodes of atrial fibrillation during the index hospitalization (≤7 days after surgery). Patients with a history of atrial fibrillation were excluded to avoid making changes to their established preoperative medication regimen for atrial fibrillation and anticoagulation.
Patients in the rate-control group received medications to slow the heart rate, with a goal of achieving a resting heart rate of less than 100 beats per minute. Patients in whom sinus rhythm did not return after an initial strategy of rate control could be switched to rhythm control if their provider thought that such treatment was necessary to improve their hemodynamic status or alleviate symptoms.
Patients in the rhythm-control group were treated with amiodarone with or without a rate-slowing agent. If atrial fibrillation persisted for 24 to 48 hours after randomization, direct-current cardioversion was recommended. The recommended dose of amiodarone was the equivalent of 3 g of oral amiodarone before hospital discharge, with a maintenance dose of 200 mg per day or less if direct-current cardioversion was successful. It was recommended that the use of amiodarone be extended for 60 days, but discontinuation was allowed for amiodarone-related adverse events (e.g., symptomatic bradycardia, a corrected QT interval of >480 msec, or neuropathy).
If patients remained in atrial fibrillation or had recurrent atrial fibrillation 48 hours after randomization, anticoagulation with warfarin (target international normalized ratio, 2 to 3) was recommended, and bridging with low-molecular-weight heparin was allowed. Anticoagulation was recommended to be continued for 60 days, unless complications occurred.
To control for noncardiovascular reasons for hospitalization, we defined readiness for discharge from an atrial fibrillation perspective. For patients in the rate-control group with continuing atrial fibrillation, the readiness-for-discharge criteria included a target resting heart rate of less than 100 beats per minute. Patients in the rhythm-control group met the discharge criteria if they received a full amiodarone loading dose and were either free of atrial fibrillation for more than 24 hours and had no atrial fibrillation at the time of discharge or remained in atrial fibrillation after treatment with amiodarone for at least 48 hours or received direct-current cardioversion with adequate control of rate.
TRIAL END POINTS
The primary end point was the total number of days in the hospital (including emergency department visits) within 60 days after randomization. Secondary end points included the duration of the hospital stay from randomization to the time of eligibility for discharge on the basis of criteria regarding atrial fibrillation, the length of the index hospitalization, the need for readmission, heart rhythm and time to conversion to a sustained stable rhythm without atrial fibrillation, the need for permanent placement of a pacemaker, and the rates of death and adverse events. The status of patients with respect to atrial fibrillation was determined by means of telemetry during the first 7 days and by means of electrocardiography at the time of hospital discharge and at 30 days and 60 days. (Details about trial end points are provided in the Supplementary Appendix.) Follow-up assessments were performed 30 days and 60 days after randomization.
STATISTICAL ANALYSIS
The primary null hypothesis of the trial was that there would be no between-group difference in the total number of days of hospitalization at 60 days after randomization. The sample size was based on estimates of the length of hospital stay and rate of rehospitalization,17 in addition to a blinded reestimation of sample size. Using a conservative estimate of a standard deviation of 6.3 days for the primary end point, we determined that enrollment of 520 patients assigned in a 1:1 ratio to one of the two groups would give the study 90% power to detect a difference of 2.0 days between the groups. We tested the primary end point in an intention-to-treat analysis using a two-tailed Wilcoxon rank-sum test with an alpha level of 0.05. The test accommodated nonignorable missing outcomes because of death by assigning such patients the worst ranks on the basis of the date of death. We used Poisson regression to analyze rates of adverse events and Kaplan–Meier analysis and the log-rank test to assess the time until conversion to a sustained, stable heart rhythm without atrial fibrillation. Sensitivity analyses to determine the influence of treatment nonadherence were performed with the use of an instrumental variable approach with the randomization assignment as the instrument.
RESULTS
PATIENTS
From May 2014 through May 2015, a total of 2109 patients met the eligibility criteria and were enrolled preoperatively (Fig. S1 in the Supplementary Appendix). Among these patients, postoperative atrial fibrillation developed in 695 (33.0%); 523 of these patients underwent randomization. The characteristics of the two groups were similar at baseline (Table 1). The mean age was 68.8±9.1 years, and 24% of the patients were women. Isolated coronary-artery bypass grafting (CABG) was performed in approximately 40%, isolated valve surgery in 40%, and both procedures in 20%. The proportion of patients in whom postoperative atrial fibrillation developed was 28.1% among those who had undergone isolated CABG, 33.7% among those who had undergone isolated valve surgery, and 47.3% among those who had undergone combined procedures.
Table 1.
Characteristics of the Patients and Procedures at Baseline.*
| Characteristic | Rate Control (N = 262) |
Rhythm Control (N = 261) |
Overall (N = 523) |
|---|---|---|---|
| Age — yr | 69.2±9.8 | 68.4±8.4 | 68.8±9.1 |
| Male sex — no. (%) | 197 (75.2) | 199 (76.2) | 396 (75.7) |
| Race or ethnic group — no. (%)† | |||
| Hispanic | 10 (3.8) | 12 (4.6) | 22 (4.2) |
| White | 242 (92.4) | 250 (95.8) | 492 (94.1) |
| Median body-mass index (IQR)‡ | 27.6 (25.1–30.9) | 28.5 (25.4–31.9) | 28.0 (25.2–31.5) |
| Medical history — no. (%) | |||
| Diabetes | 82 (31.3) | 79 (30.3) | 161 (30.8) |
| Heart failure | 35 (13.4) | 33 (12.6) | 68 (13.0) |
| Hypertension | 193 (73.7) | 198 (75.9) | 391 (74.8) |
| Previous myocardial infarction | 50 (19.1) | 48 (18.4) | 98 (18.7) |
| Stroke | 17 (6.5) | 15 (5.7) | 32 (6.1) |
| Previous revascularization | 46 (17.6) | 40 (15.3) | 86 (16.4) |
| Valve disease | 140 (53.4) | 148 (56.7) | 288 (55.1) |
| Medication — no. (%) | |||
| ACE inhibitor | 89 (34.0) | 84 (32.2) | 173 (33.1) |
| ARB | 51 (19.5) | 47 (18.0) | 98 (18.7) |
| Beta-blocker | 162 (61.8) | 145 (55.6) | 307 (58.7) |
| Calcium-channel blocker | 52 (19.8) | 58 (22.2) | 110 (21.0) |
| Diuretic | 79 (30.2) | 81 (31.0) | 160 (30.6) |
| Nitrate | 60 (22.9) | 55 (21.1) | 115 (22.0) |
| Index surgical procedure | |||
| CABG only — no. (%) | 112 (42.7) | 100 (38.3) | 212 (40.5) |
| Valve repair only — no. (%) | 39 (14.9) | 43 (16.5) | 82 (15.7) |
| CABG plus valve repair — no. (%) | 10 (3.8) | 7 (2.7) | 17 (3.3) |
| Valve replacement only — no./total no. (%) | 60/262 (22.9) | 66/261 (25.3) | 126/523 (24.1) |
| Aortic and mitral valve | 5/60 (8.3) | 4/66 (6.1) | 9/126 (7.1) |
| Aortic valve only | 44/60 (73.3) | 52/66 (78.8) | 96/126 (76.2) |
| Mitral valve only | 11/60 (18.3) | 9/66 (13.6) | 20/126 (15.9) |
| Tricuspid valve only | 0 | 1/66 (1.5) | 1/126 (0.8) |
| CABG plus valve replacement — no./total no. (%) | 41/262 (15.6) | 45/261 (17.2) | 86/523 (16.4) |
| CABG plus aortic and mitral valve | 2/41 (4.9) | 1/45 (2.2) | 3/86 (3.5) |
| CABG plus aortic valve only | 35/41 (85.4) | 36/45 (80.0) | 71/86 (82.6) |
| CABG plus mitral valve only | 4/41 (9.8) | 8/45 (17.8) | 12/86 (14.0) |
| Median bypass time (IQR) — min§ | 95.0 (73.5–127.5) | 94.0 (78.0–126.0) | 95.0 (76.0–127.0) |
| Median aortic cross-clamp time (IQR) — min¶ | 73.5 (53.5–96.0) | 73.0 (57.5–93.5) | 73.0 (55.0–94.5) |
Plus–minus values are means ±SD. ACE denotes angiotensin-converting enzyme, ARB angiotensin-receptor blocker, CABG coronary-artery bypass grafting, and IQR interquartile range.
Race and ethnic group were self-reported, and patients could report both categories.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
A total of 505 patients were included in the analysis of bypass time.
A total of 500 patients were included in the analysis of cross-clamp time.
Approximately 24% of the patients in the rhythm-control group did not complete the full course of amiodarone and received beta-blockers, calcium-channel blockers, or both (Table 2). Among the patients in the rate-control group, 26.7% received amiodarone or direct-current cardioversion. The majority of patients who discontinued or switched therapy did so for protocol-specified clinical reasons (80.0% in the rate-control group and 64.5% in the rhythm-control group). The timing of such changes in therapy differed between the groups, with more patients in the rate-control group than in the rhythm-control group changing therapy during the index hospitalization (83% vs. 48%). Overall, 60 patients (11.5%) received direct-current cardioversion (9.2% in the rate-control group and 13.8% in the rhythm-control group).
Table 2.
Reasons for and Timing of Nonadherence to Treatment Assignment.*
| Variable | Rate Control (N = 70) |
Rhythm Control (N = 62) |
|---|---|---|
| no. (%) | ||
| Reason for nonadherence | ||
|
| ||
| Preference of patient or provider | 14 (20) | 22 (35) |
|
| ||
| Side effects of heart-rate drug | 20 (29) | NA |
|
| ||
| Ineffectiveness of heart-rate drug | 36 (51) | NA |
|
| ||
| Side effects of rhythm drug | NA | 40 (65) |
|
| ||
| Timing of nonadherence | ||
|
| ||
| Before index-hospital discharge | 58 (83) | 29 (47) |
|
| ||
| Between hospital discharge and 30 days | 8 (11) | 18 (29) |
|
| ||
| After 30 days | 4 (6) | 15 (24) |
NA denotes not applicable.
HOSPITALIZATION DAYS
The primary outcome, the number of hospital days from randomization until 60 days, did not differ significantly between the rate-control group and the rhythm-control group (mean, 6.4 days and 7.0 days, respectively; median, 5.1 days and 5.0 days, respectively; P = 0.76) (Table 3). The mean length of stay for the index hospitalization after randomization was 5.5 days in the rate-control group and 5.8 days in the rhythm-control group (median, 4.3 in each group; P = 0.88). A sensitivity analysis to determine the influence of treatment nonadherence confirmed the results of the intention-to-treat analysis (P = 0.51 for the total hospital stay, P = 0.72 for the index hospital stay). (Details regarding the sensitivity analysis are provided in the Supplementary Appendix.) When the length of stay for the index hospitalization was adjusted for discharge readiness on the basis of status regarding atrial fibrillation, the mean length of stay was 5.0 days in the rate-control group and 5.2 in the rhythm-control group, with a median of 4.0 days in each group (P = 0.99).
Table 3.
Hospitalization and Readmission.
| Variable | Rate Control (N = 262) |
Rhythm Control (N = 261) |
P Value |
|---|---|---|---|
| median (IQR) | |||
| Hospitalization | |||
|
| |||
| No. of days in hospital from randomization to 60 days | 5.1 (3.0–7.4) | 5.0 (3.2–7.5) | 0.76 |
|
| |||
| After isolated CABG | 4.8 (3.0–7.7) | 5.1 (3.1–6.8) | 0.96 |
|
| |||
| After isolated valve repair or replacement | 5.0 (2.6–7.1) | 4.4 (3.1–7.0) | 0.76 |
|
| |||
| After CABG plus valve repair or replacement | 5.3 (4.2–8.4) | 7.1 (4.4–9.7) | 0.11 |
|
| |||
| No. of days of index hospitalization after randomization | 4.3 (2.9–6.6) | 4.3 (3.0–7.0) | 0.88 |
|
| |||
| No. of days from randomization to eligibility for cardiac discharge* | 4.0 (2.0–6.0) | 4.0 (3.0–6.0) | 0.99 |
|
| |||
| No. of days in hospital after discharge from index hospitalization | 2.2 (0.6–5.0) | 2.1 (1.0–4.7) | 0.82 |
|
| |||
| no. of events (rate/100 patient-mo) | |||
|
| |||
| Readmission | |||
|
| |||
| Any cause | 79 (18.5) | 80 (18.5) | 0.99 |
|
| |||
| Emergency department visit | 28 (6.5) | 24 (5.6) | 0.55 |
|
| |||
| Hospital stay of <24 hr | 5 (1.2) | 4 (0.9) | 0.73 |
|
| |||
| Rehospitalization | 46 (10.8) | 52 (12.0) | 0.58 |
|
| |||
| Cardiovascular cause | 29 (6.8) | 35 (8.1) | 0.48 |
|
| |||
| Treatment of atrial fibrillation | 11 (2.6 ) | 17 (3.9) | 0.27 |
|
| |||
| Other cardiovascular reason | 18 (4.2) | 18 (4.2) | 0.97 |
|
| |||
| Noncardiovascular cause | 50 (11.7) | 45 (10.4) | 0.57 |
To control for noncardiovascular reasons for hospitalization, eligibility for cardiac discharge was defined according to the atrial fibrillation status.
During the study period, there were 159 hospital readmissions, including emergency department visits, with no significant between-group difference in the rate per 100 patient-months (Table 3). Rates of readmission for cardiovascular causes were 6.8 per 100 patient-months in the rate-control group and 8.1 per 100 patient-months in the rhythm-control group (P = 0.48); readmission rates for the treatment of atrial fibrillation were 2.6 and 3.9 per 100 patient-months, respectively (P = 0.27). The proportion of patients who were readmitted within 30 days after hospital discharge was 22.8% in the rate-control group and 21.4% in the rhythm-control group (P = 0.71).
TIMING OF ONSET AND RESOLUTION OF ATRIAL FIBRILLATION
The average time to the onset of postoperative atrial fibrillation was 2.4 days (range, 0 to 7) after surgery. A total of 46.2% of the patients in the rate-control group and 31.8% of those in the rhythm-control group met the protocol-specified indications for the initiation of anticoagulation. At the time of hospital discharge, warfarin had been prescribed for 42.7% of the patients in the rate-control group and for 43.3% of those in the rhythm-control group, with an average duration of anticoagulation of 44.8 days and 44.9 days, respectively.
A total of 89.9% of the patients in the rate-control group and 93.5% of those in the rhythm-control group had a stable, sustained heart rhythm without atrial fibrillation at hospital discharge (P = 0.14). At 60 days, a stable heart rhythm without atrial fibrillation had been achieved for the previous 30 days in 93.8% of the patients in the rate-control group and in 97.9% of those in the rhythm-control group (P = 0.02); from discharge to 60 days, the percentages were 84.2% in the rate-control group and 86.9% in the rhythm-control group (P = 0.41) (Fig. 1).
Figure 1. Patients with No Atrial Fibrillation at 7 Days and Status at 30 Days and 60 Days.
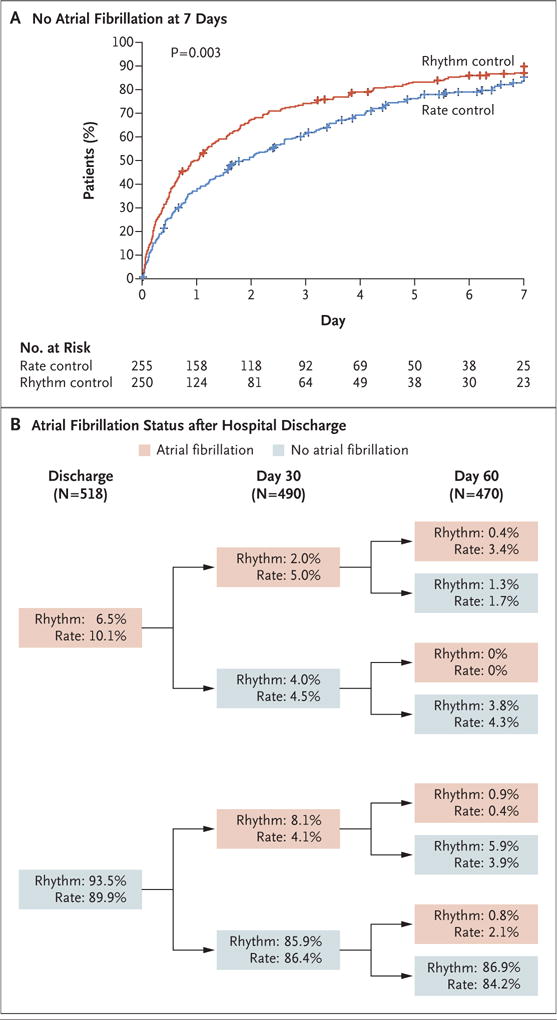
Panel A shows the proportion of patients undergoing cardiac surgery who had a stable heart rhythm without atrial fibrillation during the first week after randomization in the rate-control group and the rhythm-control group. Panel B shows the status with respect to atrial fibrillation at the time of discharge from the index hospitalization, at 30 days, and at 60 days, according to treatment group. The pink boxes denote patients in atrial fibrillation, and the blue boxes denote patients with a stable heart rhythm without atrial fibrillation. The patients’ status with respect to atrial fibrillation was determined by means of electrocardiography at the time of hospital discharge and at 30 days and 60 days. The accounting for atrial fibrillation included patients who had recurrent atrial fibrillation (as adjudicated by the clinical events committee) or who were readmitted to the hospital for recurrent atrial fibrillation during the interval periods. Overall, 11.5% of patients underwent direct-current cardioversion (9.2% in the rate-control group and 13.8% in the rhythm-control group). Of the direct-current cardioversions, 85% occurred during the index hospitalization. Among the patients who were discharged from the hospital with atrial fibrillation, direct-current cardioversion was performed during the index hospitalization in 3 of 26 patients (12%) in the rate-control group and in 7 of 17 patients (41%) in the rhythm-control group.
DEATH AND ADVERSE EVENTS
At 60 days, five patients had died: three in the rate-control group and two in the rhythm-control group (P = 0.64). There were no significant differences in the overall rates of serious adverse events between the rate-control group and the rhythm-control group (24.8 per 100 patient-months and 26.4 per 100 patient-months, respectively; P = 0.61) (Table 4). The overall rates of cerebrovascular thromboembolism (0.8 per 100 patient-months in the rate-control group and 0.4 per 100 patient-months in the rhythm-control group) and noncerebral thromboembolism (0.6 per 100 patient-months and 0.2 per 100 patient-months) were low and did not differ significantly between the two groups (P = 0.40 for the cerebrovascular thromboembolism comparison and P = 0.31 for the noncerebral thromboembolism comparison). The rates of serious bleeding (a score of ≥3 on the Bleeding Academic Research Consortium scale, with scores ranging from 0 [no bleeding] to 5 [fatal bleeding]) were 2.2 per 100 patient-months in the rate-control group and 1.2 per 100 patient-months in the rhythm-control group (P = 0.21). The most common protocol-defined adverse events (either serious or nonserious) were major infections (9.3 per 100 patient-months in the rate-control group and 6.6 per 100 patient-months in the rhythm-control group, P = 0.13), cardiac arrhythmias (4.7 and 6.2 per 100 patient-months, respectively; P = 0.30), and pleural effusions (3.0 and 4.8 per 100 patient-months, respectively; P = 0.16).
Table 4.
Serious and Protocol-Defined Adverse Events.*
| Event | Serious Adverse Events
|
Nonserious Adverse Events
|
Total Events
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Rate Control | Rhythm Control | P Value | Rate Control | Rhythm Control | P Value | Rate Control | Rhythm Control | P Value | |
|
no. of events (rate/100 patient-mo) |
no. of events (rate/100 patient-mo) |
no. of events (rate/100 patient-mo) |
|||||||
| Any | 122 (24.8) | 132 (26.4) | 0.61 | 33 (6.7) | 28 (5.6) | 0.48 | 155 (31.5) | 160 (32.0) | 0.88 |
|
| |||||||||
| Bleeding | 11 (2.2) | 6 (1.2) | 0.21 | 2 (0.4) | 2 (0.4) | 0.99 | 13 (2.6) | 8 (1.6) | 0.26 |
|
| |||||||||
| Anemia | 0 | 3 (0.6) | 0.08 | NA | NA | NA | 0 | 3 (0.6) | 0.08 |
|
| |||||||||
| Cardiac arrhythmia | 21 (4.3) | 23 (4.6) | 0.80 | 2 (0.4) | 8 (1.6) | 0.06 | 23 (4.7) | 31 (6.2) | 0.30 |
|
| |||||||||
| Sustained supraventricular | 13 (2.6) | 16 (3.2) | 0.61 | 0 | 3 (0.6) | 0.08 | 13 (2.6) | 19 (3.8) | 0.31 |
|
| |||||||||
| Sustained ventricular | 0 | 0 | 0 | 1 (0.2) | 0 | 0.32 | 1 (0.2) | 0 | 0.32 |
|
| |||||||||
| Conduction abnormality | |||||||||
|
| |||||||||
| With pacemaker placement | 5 (1.0) | 7 (1.4) | 0.58 | 0 | 0 | 0 | 5 (1.0) | 7 (1.4) | 0.59 |
|
| |||||||||
| Without pacemaker placement | 2 (0.4) | 0 | 0.16 | 0 | 0 | 0 | 2 (0.4) | 0 | 0.16 |
|
| |||||||||
| Corrected QT interval >500 msec | 1 (0.2) | 0 | 0.32 | 1 (0.2) | 5 (1.0) | 0.10 | 2 (0.4) | 5 (1.0) | 0.27 |
|
| |||||||||
| Cerebrovascular thromboembolism | 4 (0.8) | 2 (0.4) | 0.40 | 0 | 0 | 0 | 4 (0.8) | 2 (0.4) | 0.40 |
|
| |||||||||
| Stroke | 4 (0.8) | 1 (0.2) | 0.18 | 0 | 0 | 0 | 4 (0.8) | 1 (0.2) | 0.18 |
|
| |||||||||
| Transient ischemic attack | 0 | 1 (0.2) | 0.32 | 0 | 0 | 0 | 0 | 1 (0.2) | 0.32 |
|
| |||||||||
| Noncerebral thromboembolism | 3 (0.6) | 1 (0.2) | 0.31 | 0 | 0 | 0 | 3 (0.6) | 1 (0.2) | 0.31 |
|
| |||||||||
| Heart failure | 9 (1.8) | 9(1.8) | 0.97 | 0 | 0 | 0 | 9(1.8) | 9(1.8) | 0.97 |
|
| |||||||||
| Major infection | 28 (5.7) | 22 (4.4) | 0.37 | 18 (3.7) | 11 (2.2) | 0.18 | 46 (9.3) | 33 (6.6) | 0.13 |
|
| |||||||||
| Renal event | 5 (1.0) | 6 (1.2) | 0.78 | 4 (0.8) | 6 (1.2) | 0.54 | 9(1.8) | 12 (2.4) | 0.53 |
|
| |||||||||
| Respiratory failure | 5 (1.0) | 8 (1.6) | 0.42 | 0 | 0 | 0 | 5 (1.0) | 8 (1.6) | 0.42 |
|
| |||||||||
| Warfarin toxic effect | 1 (0.2) | 1 (0.2) | 0.99 | NA | NA | NA | 1 (0.2) | 1 (0.2) | 0.99 |
|
| |||||||||
| Hypotension or syncope | 6 (1.2) | 4 (0.8) | 0.51 | NA | NA | NA | 6 (1.2) | 4 (0.8) | 0.51 |
|
| |||||||||
| Amiodarone toxic effect | 0 | 2 (0.4) | 0.16 | NA | NA | NA | 0 | 2 (0.4) | 0.16 |
|
| |||||||||
| Pericardial-fluid collection | 2 (0.4) | 0 | 0.16 | 0 | 0 | 0 | 2 (0.4) | 0 | 0.16 |
|
| |||||||||
| Pleural effusion | 10 (2.0) | 23 (4.6) | 0.03 | 5 (1.0) | 1 (0.2) | 0.10 | 15 (3.0) | 24 (4.8) | 0.16 |
|
| |||||||||
| Other | 17(3.5) | 22 (4.4) | 0.45 | 2 (0.4) | 0 | 0.16 | 19 (3.9) | 22 (4.4) | 0.67 |
NA denotes not applicable.
DISCUSSION
Our findings confirm that new-onset atrial fibrillation remains a common complication after cardiac surgery. More than 30% of the patients who underwent cardiac surgery in our trial had either sustained or recurrent postoperative atrial fibrillation. These rates approached 50% among patients who underwent combined CABG and valve surgery. Postoperative atrial fibrillation is associated with several adverse consequences and independently predicts increased rates of death and complications, including stroke, heart failure, and infection.1,2,6,8 Moreover, postoperative atrial fibrillation after cardiac surgery significantly increases the length of hospital stay, readmission risk, and resource utilization. Estimates of the average annual cost of treatment of postoperative atrial fibrillation and its sequelae approach $1 billion in the United States.1,18,19
Despite the importance of postoperative atrial fibrillation, the most effective management strategy for this common surgical complication remains uncertain, a factor that had led to a substantial variation in treatments. The joint guidelines of the American College of Cardiology, American Heart Association, and Heart Rhythm Society, which were published when our trial was far along in enrollment, recommend rate control with beta-blockers as the first-line therapy in patients whose condition is hemodynamically stable (i.e., class I, level of evidence A).20 These recommendations are based partly on studies regarding the prevention of atrial fibrillation after cardiac surgery and extrapolation from the AFFIRM trial, which compared rate control with rhythm control in nonsurgical patients with atrial fibrillation. The AFFIRM trial showed that management of nonsurgical atrial fibrillation with rhythm control offered no survival advantage over rate control and that patients who were treated with a rhythm-control strategy were more likely to require hospitalization and have adverse drug effects than were those who were treated with a rate-control strategy.10 By comparison, rigorous evidence in the cardiac surgical setting is sparse and limited to several retrospective, observational studies and one pilot randomized trial comparing rate control with rhythm control in 50 patients.5–9,11,13
In our trial, in which the number of patients enrolled was 10 times that in the previous studies, we discovered important insights into the benefits and risks of rate control versus rhythm control for the treatment of postoperative atrial fibrillation after cardiac surgery. We found no significant difference between treatment strategies with respect to the primary end point, the total number of hospital days, including the primary admission and any subsequent readmissions occurring within 60 days after randomization. Postoperative atrial fibrillation is usually a transient condition that resolves spontaneously but that may have hemodynamic consequences and result in treatment-related adverse events, such as bleeding, thromboembolic complications, drug-related toxic effects, and complications related to the use of direct-current cardioversion, events that may in turn lead to prolonged hospitalizations and repeat admissions. The primary end point that we used in this trial captures the short-term effect of a very diverse set of adverse events. Moreover, further insight into the trade-offs between rate control and rhythm control can help improve clinical decision making and resource utilization. The importance of this end point is reflected in the finding that the rate of hospital readmission at 30 days was more than 28%, with nearly one fifth of such readmissions resulting from recurrent atrial fibrillation.
Patients in the rhythm-control group achieved a stable heart rhythm without atrial fibrillation earlier than those in the rate-control group. In addition, the proportion of patients who were free of atrial fibrillation between day 30 and day 60 was significantly lower in the rhythm-control group than in the rate-control group. However, the overall proportion of patients who were free of atrial fibrillation between hospital discharge and 60 days was much lower than the proportion who were free of atrial fibrillation between 30 days and 60 days, but the between-group difference was not significant. Although we did not compare strategies for anticoagulation in patients with postoperative atrial fibrillation, the results provide data that may inform clinical decision making. The protocol specified that anticoagulation therapy should be initiated in patients who had atrial fibrillation for more than 48 hours and those who had more than a single episode of atrial fibrillation during the index hospitalization. More patients in the rate-control group than in the rhythm-control group met this indication (46.2% vs. 31.8%). However, the proportions of patients who were prescribed warfarin at discharge were similar in the two groups, which may reflect additional considerations regarding the need for anticoagulation. The median duration of anticoagulation was approximately 45 days in each group.
With the anticoagulation strategy used in this trial, the incidence of serious thromboembolic events (2%) was low overall and did not differ significantly between the two groups. The overall percentage of patients with serious bleeding was approximately 3%, a frequency that did not differ significantly between the two groups. Nearly 90% of the bleeding events occurred in patients who were receiving anticoagulation. Thus, the relatively low incidence of thromboembolic events came at the expense of serious bleeding, which suggests the need to further study the trade-off between the risks and benefits of anticoagulation for atrial fibrillation after cardiac surgery.
In this comparative effectiveness trial, we evaluated an initial strategy of rate control versus rhythm control in a clinical context in which changes in the status of patients can prompt alterations in the treatment regimen. Approximately 25% of the patients could not adhere to the assigned treatment strategy. Among the patients in the rate-control group, 26.7% received amiodarone or direct-current cardioversion, and 23.8% of the patients in the rhythm-control group did not complete the full course of amiodarone. The majority of treatment nonadherence occurred for prespecified clinical indications. Deviation from rate control was largely a result of drug ineffectiveness, whereas amiodarone was discontinued mostly due to drug-related toxic effects. In the AFFIRM trial, investigators noted crossover rates of 15 to 38% during the course of the trial in nonsurgical patients who were not as acutely ill as those in our trial.10
Our study has several limitations. First, the primary end point was a proxy for important clinical outcomes, such as stroke and serious bleeding. A randomized trial with the power to detect differences in these end points would have required the enrollment of thousands of patients. Second, the results of our trial pertain only to patients with new-onset postoperative atrial fibrillation. Third, there was a relatively high rate of treatment discontinuation, but in sensitivity analyses we confirmed the results of the intention-to-treat analysis. Fourth, we did not include quality-of-life measures because of the short duration of the trial and the likelihood that the effects of surgery would overshadow the effects of postoperative atrial fibrillation on quality of life. However, the inclusion of such measures might have provided insights into the burden of treatment and its trade-offs. Finally, we did not assess postoperative atrial fibrillation by means of continuous home monitoring, an approach that might have led to an underestimation of its prevalence.
Postoperative atrial fibrillation is common after cardiac surgery and amenable to either a rate-control or rhythm-control strategy. Approximately 85% of the patients in our trial had a stable heart rhythm without atrial fibrillation from the time of hospital discharge onward, and about 95% were free of atrial fibrillation by the end of the study. Anticipating this result, we chose an end point that was related to resource utilization and the experience of patients: days in the hospital after randomization. The study-group assignments did not influence this end point. However, we did observe clinical differences between the two approaches. An initial strategy of rate control averted much of the toxic effects and side effects associated with amiodarone but was associated with a slower resolution of atrial fibrillation, thereby leading to a greater need for anticoagulation (with its attendant risks) and a slightly higher prevalence of atrial fibrillation during follow-up. The faster resolution of atrial fibrillation in the rhythm-control group came at the price of amiodarone-related side effects in many patients, often necessitating discontinuation of amiodarone after hospital discharge. In patients with postoperative atrial fibrillation who are in hemodynamically stable condition, one strategy does not appear to have a net clinical advantage over the other. In such cases, the preferences of patients and physicians should dictate whether a rhythm-control approach that uses amiodarone with or without direct-current cardioversion is worth the benefit over a rate-control approach.
Supplementary Material
Acknowledgments
Supported by a cooperative agreement (U01 HL088942) funded by the National Heart, Lung, and Blood Institute and the National Institute of Neurological Disorders and Stroke of the National Institutes of Health, Bethesda, MD, and the Canadian Institutes of Health Research.
APPENDIX
The authors’ full names and academic degrees are as follows: A. Marc Gillinov, M.D., Emilia Bagiella, Ph.D., Alan J. Moskowitz, M.D., Jesse M. Raiten, M.D., Mark A. Groh, M.D., Michael E. Bowdish, M.D., Gorav Ailawadi, M.D., Katherine A. Kirkwood, M.S., Louis P. Perrault, M.D., Michael K. Parides, Ph.D., Robert L. Smith II, M.D., John A. Kern, M.D., Gladys Dussault, R.N., Amy E. Hackmann, M.D., Neal O. Jeffries, Ph.D., Marissa A. Miller, D.V.M., Wendy C. Taddei-Peters, Ph.D., Eric A. Rose, M.D., Richard D. Weisel, M.D., Deborah L. Williams, B.S.N., M.P.H., Ralph F. Mangusan, R.N., Michael Argenziano, M.D., Ellen G. Moquete, R.N., Karen L. O’Sullivan, M.P.H., Michel Pellerin, M.D., Kinjal J. Shah, P.A., James S. Gammie, M.D., Mary Lou Mayer, B.S.N., Pierre Voisine, M.D., Annetine C. Gelijns, Ph.D., Patrick T. O’Gara, M.D., and Michael J. Mack, M.D.
The authors’ affiliations are as follows: the Department of Thoracic and Cardiovascular Surgery, Cleveland Clinic Foundation, Cleveland (A.M.G.); the International Center for Health Outcomes and Innovation Research, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai (E.B., A.J.M., K.A.K., M.K.P., D.L.W., E.G.M., K.L.O., K.J.S., A.C.G.), Department of Cardiac Surgery, Mount Sinai Health System (E.A.R.), and Division of Cardiothoracic Surgery, Department of Surgery, College of Physicians and Surgeons, Columbia University (M.A.) — all in New York; Department of Anesthesiology and Critical Care, University of Pennsylvania (J.M.R.), and Department of Surgery, Division of Cardiovascular Surgery, University of Pennsylvania School of Medicine (M.L.M.) — both in Philadelphia; Cardiovascular and Thoracic Surgery, Mission Health and Hospitals, Asheville, NC (M.A.G., R.F.M.); Department of Surgery, Keck School of Medicine of USC, University of Southern California, Los Angeles (M.E.B., A.E.H.); Division of Thoracic and Cardiovascular Surgery, University of Virginia School of Medicine, Charlottesville (G.A., J.A.K.); Montreal Heart Institute, Université de Montréal, Montreal (L.P.P., M.P.), Institut Universitaire de Cardiologie et de Pneumologie de Québec, Hôpital Laval, Quebec, QC (G.D., P.V.), and Peter Munk Cardiac Centre and Division of Cardiovascular Surgery, Toronto General Hospital, University Health Network and the Division of Cardiac Surgery, University of Toronto, Toronto (R.D.W.) — all in Canada; Department of Cardiovascular Surgery, Heart Hospital Baylor Plano, Baylor Health Care System, Plano, TX (R.L.S., M.J.M.); Office of Biostatistics Research (N.O.J.) and Division of Cardiovascular Sciences (M.A.M., W.C.T.-P.), National Heart, Lung, and Blood Institute, Bethesda, and Department of Surgery, University of Maryland Medical Center, Baltimore (J.S.G.) — both in Maryland; and the Cardiovascular Division, Brigham and Women’s Hospital, Boston (P.T.O.).
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51:793–801. doi: 10.1016/j.jacc.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 2.Jongnarangsin K, Oral H. Postoperative atrial fibrillation. Cardiol Clin. 2009;27:69–78, viii. doi: 10.1016/j.ccl.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Nair SG. Atrial fibrillation after cardiac surgery. Ann Card Anaesth. 2010;13:196–205. doi: 10.4103/0971-9784.69047. [DOI] [PubMed] [Google Scholar]
- 4.Chelazzi C, Villa G, De Gaudio AR. Postoperative atrial fibrillation. ISRN Cardiol. 2011;2011:203179. doi: 10.5402/2011/203179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imazio M, Belli R, Brucato A, et al. Rationale and design of the COlchicine for Prevention of the Post-pericardiotomy Syndrome and Post-operative Atrial Fibrillation (COPPS-2 trial): a randomized, placebo-controlled, multicenter study on the use of colchicine for the primary prevention of the postpericardiotomy syndrome, postoperative effusions, and postoperative atrial fibrillation. Am Heart J. 2013;166:13–9. doi: 10.1016/j.ahj.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. JAMA. 1996;276:300–6. [PubMed] [Google Scholar]
- 7.Lee JK, Klein GJ, Krahn AD, et al. Rate-control versus conversion strategy in postoperative atrial fibrillation: a prospective, randomized pilot study. Am Heart J. 2000;140:871–7. doi: 10.1067/mhj.2000.111104. [DOI] [PubMed] [Google Scholar]
- 8.Mathew JP, Fontes ML, Tudor IC, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–9. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 9.Ozaydin M, Icli A, Yucel H, et al. Metoprolol vs. carvedilol or carvedilol plus N-acetyl cysteine on post-operative atrial fibrillation: a randomized, double-blind, placebo-controlled study. Eur Heart J. 2013;34:597–604. doi: 10.1093/eurheartj/ehs423. [DOI] [PubMed] [Google Scholar]
- 10.The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825–33. doi: 10.1056/NEJMoa021328. [DOI] [PubMed] [Google Scholar]
- 11.Lee JK, Klein GJ, Krahn AD, et al. Rate-control versus conversion strategy in postoperative atrial fibrillation: trial design and pilot study results. Card Electrophysiol Rev. 2003;7:178–84. doi: 10.1023/a:1027428003609. [DOI] [PubMed] [Google Scholar]
- 12.Mayson SE, Greenspon AJ, Adams S, et al. The changing face of postoperative atrial fibrillation prevention: a review of current medical therapy. Cardiol Rev. 2007;15:231–41. doi: 10.1097/CRD.0b013e31813e62bb. [DOI] [PubMed] [Google Scholar]
- 13.Al-Khatib SM, Hafley G, Harrington RA, et al. Patterns of management of atrial fibrillation complicating coronary artery bypass grafting: results from the PRoject of Ex-vivo Vein graft ENgineering via Transfection IV (PREVENT-IV) Trial. Am Heart J. 2009;158:792–8. doi: 10.1016/j.ahj.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell LB, Crystal E, Heilbron B, Pagé P. Atrial fibrillation following cardiac surgery. Can J Cardiol. 2005;21(Suppl B):45B–50B. [PubMed] [Google Scholar]
- 15.Fuster V, Rydén LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(7):e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 16.Fuster V, Rydén LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123(10):e269–367. doi: 10.1161/CIR.0b013e318214876d. [DOI] [PubMed] [Google Scholar]
- 17.Gelijns AC, Moskowitz AJ, Acker MA, et al. Management practices and major infections after cardiac surgery. J Am Coll Cardiol. 2014;64:372–81. doi: 10.1016/j.jacc.2014.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aranki SF, Shaw DP, Adams DH, et al. Predictors of atrial fibrillation after coronary artery surgery: current trends and impact on hospital resources. Circulation. 1996;94:390–7. doi: 10.1161/01.cir.94.3.390. [DOI] [PubMed] [Google Scholar]
- 19.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics — 2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 20.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199–267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


