Abstract
Objectives
Health related quality of life (HRQoL) has been increasingly considered an endpoint in evaluations of treatment for substance use disorders. We aimed to characterize longitudinal patterns of HRQoL in individuals with opioid use disorder (OUD) and with a history of opioid agonist treatment (OAT) with methadone.
Methods
The EuroQol EQ-5D, a preference-weighted measure of HRQoL, was assessed in individuals with OUD and with a history of OAT enrolled in three prospective cohort studies between December 2011 and May 2014, with a maximum of five biannual assessments. We used latent class growth analysis to identify HRQoL trajectory classes and their association with self-reported current OAT receipt. Class assignment was derived from posterior probabilities and we explored time-invariant and time-varying determinants of trajectory class membership.
Results
Our study included 443 individuals (median age 47, 37% female); 24.6% reported use of illicit opioids at every follow-up, 69.1% during at least one follow-up. We identified three latent HRQoL trajectory classes that were stable regardless of current OAT receipt: stably high (n=107, 24.2%), stably moderate (n=260, 58.7%) and stably low HRQoL (n=76, 17.2%). A history of either a physical disability or of a mental health illness increased the probability of membership assignment to a lower HRQoL class.
Conclusions
The non-significant association of OAT with HRQoL may suggest that the modest immediate HRQoL gains after OAT engagement, observed in short-term studies, may not persist over time. Implications for cost-effectiveness analysis and clinical practice are discussed.
Keywords: Health related quality of life, longitudinal health utility, opioid agonist treatment, opioid use, stimulant use, treatment outcomes
1. INTRODUCTION
Drug dependence is recognized as a chronic, recurrent disease (McLellan, Lewis, O’Brien, & Kleber, 2000) and the assessment of health related quality of life (HRQoL) is increasingly considered an important endpoint in evaluations of treatment for substance use disorders (SUD) (De Maeyer, Vanderplasschen, & Broekaert, 2010; Miller & Miller, 2009; Veilleux, Colvin, Anderson, York, & Heinz, 2010). Treatment focused only on use reduction or cessation does not directly incorporate concerns for all dimensions of health, which can be problematic for treatment evaluation given the complex psychological and physical problems commonly present in individuals with SUD (Miller & Miller, 2009). Economic evaluations underlying many health policy decisions measure benefits through estimated quality-adjusted life year (QALY) (Caro, Briggs, Siebert, & Kuntz, 2012), an outcome capturing longevity and HRQoL. The use of self-reported HRQoL capturing the diverse domains of health important to the individual receiving treatment is therefore not only a useful clinical outcome but also an integral component of health economic evaluations that are executed to guide resource allocation decisions.
Opioid agonist treatment (OAT) with methadone has been shown to be effective in numerous randomized trials, meta-analyses, and large-scale longitudinal studies (Amato et al., 2005; Faggiano, Vigna-Taglianti, Versino, & Lemma, 2003; Mattick, Kimber, Breen, & Davoli, 2008). Beyond clinical and cost effectiveness, OAT has the potential to improve patients’ HRQoL through alleviation of withdrawal symptoms, reduction in risk of HIV infection and overdose, and decrease in harms resulting from drug-seeking behavior. If delivered according to best practice guidelines, OAT can further increase access to psychosocial and pharmacological treatment for co-morbid conditions as well as pain management (Health Canada, 2002; National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998).
Previous research assessing HRQoL over time for individuals with OUD has mostly been done in the context of treatment evaluations: some comparing OAT with methadone and buprenorphine (Giacomuzzi et al., 2003; Ponizovsky & Grinshpoon, 2007) or buprenorphine/naloxone (Nosyk, Bray, et al., 2015), others comparing OAT with methadone to prescribed heroin (Dijkgraaf et al., 2005; Karow et al., 2010; Nosyk et al., 2012) or to prescribed morphine (Winklbaur, Jagsch, Ebner, Thau, & Fischer, 2008). Otherwise, HRQoL has also been assessed in the context of buprenorphine/naloxone receipt concurrent with HIV care (Korthuis et al., 2011). These studies have ranged from 12 to 24 weeks (Giacomuzzi et al., 2003; Nosyk, Bray, et al., 2015; Winklbaur et al., 2008) up to 12 months (Dijkgraaf et al., 2005; Karow et al., 2010; Korthuis et al., 2011; Nosyk et al., 2012; Ponizovsky & Grinshpoon, 2007), and while many have used simple pre-post comparisons of HRQoL measures (Dijkgraaf et al., 2005; Giacomuzzi et al., 2003; Karow et al., 2010; Ponizovsky & Grinshpoon, 2007; Winklbaur et al., 2008), some have evaluated changes in HRQoL estimated with statistical analyses controlling for potential confounding (Korthuis et al., 2011; Nosyk, Bray, et al., 2015; Nosyk et al., 2012). For instance, a secondary analysis of two randomized controlled trials with up to a 6-month time horizon found immediate yet relatively small improvements in HRQoL, with diminishing, and possibly deteriorating benefits thereafter (Nosyk, Bray, et al., 2015). A prior study on individuals with OUD revealed moderate immediate HRQoL improvement that declined slightly over time during OAT. Critically, these gains were only observed in 61% of the study cohort, while 20% demonstrated low baseline HRQoL and no HRQoL response despite sustained engagement in treatment (Nosyk et al., 2011). While this growing body of evidence in recent years has indicated improvements in HRQoL in OAT for individuals with OUD, the estimated gains have been over short-term studies and modest in magnitude.
Confirmation of such findings over longer periods may have important implications for cost-effectiveness analyses (CEA) for the treatment of OUD. Indeed, evidence on longitudinal patterns of OAT utilization suggests that OUD is characterized by recurrent periods of treatment, relapse and abstinence (Bell, Burrell, Indig, & Gilmour, 2006; Nosyk et al., 2009). In the absence of longitudinal data, CEA implicitly assume that the observed short term improvements stemming from OAT engagement are persistent over time, and in repeated treatment admissions (Connock, Juarez-Garcia, Jowett, Frew, & Liu, 2007; Nosyk et al., 2012; Schackman, Leff, Polsky, Moore, & Fiellin, 2012). Past OAT evaluations have either lacked HRQoL data (Amato et al., 2005), using instead varying conceptualization of subjective quality of life outcomes (De Maeyer et al., 2010), or have had follow-up periods too short to capture the recurrent pattern of OUD. CEA adhering to best practice guidelines (Caro et al., 2012) require accurate characterization of health state-specific HRQoL measures over the long-term to estimate quality-adjusted life year (QALY) benefits in comparative analyses of competing treatment modalities and medications.
Individuals with OUD typically access OAT several times over their life trajectories of substance use (McLellan et al., 2000) and may follow heterogeneous long-term HRQoL trajectories. Models of group-based trajectories allow the identification of clusters of individuals with similar patterns over time. Using a modified version of the Lancashire Quality of Life Profile rather than a measure of HRQoL, De Maeyer et al. (2013) evaluated latent classes of quality of life among individuals with OUD five to ten years after initiating OAT and found three classes that did not differ in terms of drug use or alcohol consumption. However, both psychological and chronic medical comorbidities were associated with lower quality of life classes. These findings in addition to the aforementioned studies suggesting that short-term HRQoL benefits associated with OAT, when observed, appeared to diminish, and possibly decline (Nosyk, Bray, et al., 2015; Nosyk et al., 2012), led us to hypothesize that long-term HRQoL trajectories would display minimal variation over time.
The paucity of evidence on long-term patterns of HRQoL increases the importance of identifying these distinct trajectories and characterizing their relationship with OAT engagement. We undertook this study to characterize longitudinal patterns of HRQoL in individuals with OUD and with a history of OAT with methadone. Our secondary objective was to understand the effect of both time-varying and time-invariant attributes on HRQoL trajectories. Both outcomes will inform CEA and contribute to clinical efforts to develop treatment for those individuals with complex needs who will most benefit from comprehensive care over a long-term perspective.
2. METHODS
2.1 Study design and measurement
Longitudinal data were derived from a series of ongoing open prospective cohort studies undertaken in Vancouver, Canada involving illicit drug users, including the At-Risk Youth Study (ARYS), the AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS), and the Vancouver Injection Drug Users Study (VIDUS). The VIDUS study began enrollment in May 1996 and recruits individuals through word of mouth, street out-reach, and referrals. The original VIDUS cohort was divided into two separate studies in 2005: VIDUS now follows HIV-negative individuals and its sister study ACCESS follows HIV-positive drug users based in the Greater Vancouver area (Strathdee et al., 1997; E. Wood et al., 2009). The At-Risk Youth Study began in late 2005 and is made up of street-involved youth (aged 14–26) who report use of drugs other than or in addition to cannabis (E. Wood, Stoltz, Li, Montaner, & Kerr, 2006; E. Wood, Stoltz, Montaner, & Kerr, 2006).
Detailed sampling and follow-up methodologies have been described previously and were equivalent across cohorts to allow for pooled analyses (Strathdee et al., 1997; Tyndall et al., 2003; E. Wood, Stoltz, Li, et al., 2006; E. Wood, Stoltz, Montaner, et al., 2006). Participants complete an interviewer-administered questionnaire at baseline and receive $30 CAD for each visit. All studies have been approved by the University of British Columbia/Providence Health Care Research Ethics Board.
Items assessing HRQoL were first added to the follow-up study instrument for the cohort studies in November 2011. We considered baseline data captured between March 2005 and May 2013, with a maximum of five bi-annual assessments during the period of December 2011 and May 2014. All individuals who completed four consecutive follow-up assessments during this period and reported ever accessing OAT at the start of the study period were eligible for inclusion. Individuals were excluded if during the study period they reported neither any OAT receipt nor any illicit opioid use.
The primary outcome for this analysis was participants’ self-reported HRQoL, captured as a preference weighted multi-attribute measure derived from the EuroQol EQ-5D. The EQ-5D index value is derived from a short generic self-rated questionnaire where respondents choose 1 of 3 levels of severity of impairment in functioning in 5 items representing domains of health status (mobility, personal care, usual activities, pain/discomfort, and anxiety/depression) (Brooks, 1996; The EuroQol Group, 1990). The 5-dimension-by-3-level structure can describe 243 unique health states which are weighted using a set of preference values derived from general population surveys (Shaw, Johnson, & Coons, 2005). We used Canadian preference weights derived using the time trade-off method (Bansback, Tsuchiya, Brazier, & Anis, 2012), thus generating scores ranging from −0.34 to 1.0. The score is considered a measure of indirect health utility, as methods used to derive societal preference weights are grounded in expected utility theory, and such measures are designed to calculate QALYs for use in CEA. The EQ-5D score has been shown to be valid for individuals with OUD (van der Zanden et al., 2006) and more responsive to changes in drug use compared to the SF-6D (Nosyk et al., 2010).
We were primarily interested in assessing how current OAT receipt was associated with HRQoL patterns. In British-Columbia, Canada individuals prescribed OAT with methadone must meet DSM-IV-TR criteria for opioid use disorder (College of Physicians and Surgeons of British Columbia, 2014). We used self-reported current OAT receipt at the time of assessment as the EQ-5D questionnaire requests the participant to describe their own HRQoL that day. The question asked was: “Are you in a methadone treatment program right now?” While an indicator of OAT receipt might not be informative of other treatment context such as dosage, time from initiation or adherence, self-report of OAT receipt has been found to be associated with expected treatment outcomes of OAT in various studies (Palepu et al., 2006 ; Uhlmann et al., 2010; E Wood et al., 2005).
2.2 Statistical analysis
We used latent class growth analysis (LCGA) to disaggregate individuals into latent, or unobserved, HRQoL trajectory classes. LCGA is a semi-parametric mixture modeling method used to determine differences in longitudinal profiles among individuals. Rather than assuming individuals are drawn from a single homogeneous population, LCGA assumes that each individual may be regarded as a sample from one of an unknown or hypothesized number of hypothetical latent classes (Cameron & Trivedi, 2005). This allows for the estimation of class-specific HRQoL parameters and of the probability of class membership. The method and underlying statistical theory is described exhaustively elsewhere (Jones & Nagin, 2007; Jones, Nagin, & Roeder, 2001; Nagin, 2009).
As we had no a priori hypothesis regarding the number of classes, we considered models with up to five latent classes, and up to a cubic polynomial function for each class. The number of classes should be determined considering a combination of both statistical and theoretical criteria (Muthén, 2003; Nagin, 2009) and the Bayesian Information Criterion (BIC) has been shown to perform the best of all information criteria across mixture models (Nylund, Asparouhov, & Muthén, 2007; Yang, 2006). Our model for estimation was chosen from the lowest BIC. To assess the degree of evidence favoring our chosen model compared to a simpler model, we used the BIC log Bayes factor approximation, which is equal to two times the difference between the BIC of the more complex model less the simpler model. Values between two and six provide positive evidence of favoring the more complex model whereas values above six provide strong evidence for the more complex model (Jones et al., 2001). The model used in our analysis is a mixture of censored normal probability distributions with censorship point = 1, which is suitable given the EQ-5D score index is bounded at 1.
Using prior cross-sectional and longitudinal studies among individuals with OUD (Astals et al., 2008; Falck, Wang, Siegal, & Carlson, 2000; Kertesz et al., 2005; Millson et al., 2006; Puigdollers et al., 2004), we identified time invariant covariates hypothesized to be associated with class membership. Using latent group membership as the dependent variable in regression analysis to determine the effect of such hypothesized covariates would not account for the uncertainty associated with the assignment of class membership. Rather, time-invariant covariates are introduced in the LCGA estimation and thus their effect will account for the probabilistic assignment of class membership. Aside from vital demographic characteristics (age at baseline, gender, ethnicity), our analysis included time invariant self-reported indicators for physical disability (defined as reporting to have a physical disability limiting mobility), history of mental health conditions (defined as reporting ever being diagnosed with a mental health issue) as well as infectious disease status (HIV, HCV) at baseline.
Trajectories of HRQoL are defined over time yet they do not necessarily represent a deterministic function of time. As there is the potential for time-varying covariates to impact the observed trajectories, we also included time-varying covariates for daily or non-daily opioid and stimulant use, derived at every assessment on the basis of self-reported use in the past six months. Illicit opioids included heroin and the misuse of prescription opioids, methadone or morphine. Stimulants included crack, cocaine, and crystal methamphetamine.
To explicate individual longitudinal variation of the HRQoL score we identified one or two level deterioration, improvement or the absence of change for each of the 5 items representing domains of health status in the EQ-5D between each completed assessments. For instance, two-level changes captured a change from a response of having no problems to having extreme problems, or the converse.
Finally, we conducted two sensitivity analyses. First, we compared baseline characteristics of individuals included in our study compared to those that were excluded to address selectivity and generalizability issues. Second, we conducted our LCGA on the subset of individuals included in our study sample that did not report any illicit opioid use over the study period to assess if our findings differed for individuals with reported abstinence.
Statistical analyses were executed in SAS version 9.3 and Stata version 13.1 and figures were produced in R version 3.1.2.
3. RESULTS
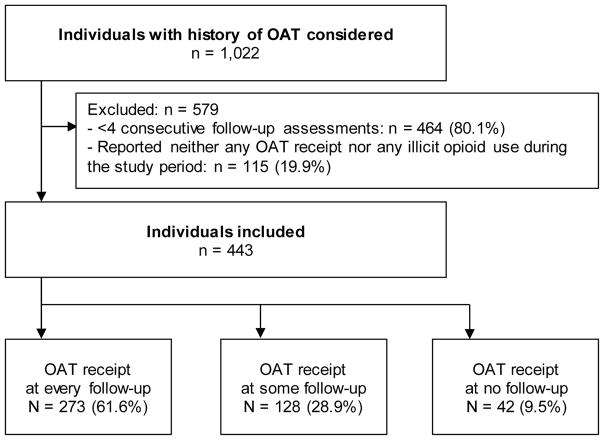
1,022 individuals recruited by the prospective cohort studies reporting a history of ever accessing OAT with methadone at study initiation were considered. Of the 558 with at least four follow-up assessments during our study period, 443 individuals met the inclusion and exclusion criteria (Figure 1). Our study sample had a median age of 47 and 36.8% were female. Prevalence of illicit opioid use at one follow-up or more was 69.1% and 90.5% reported current OAT receipt at least once during the study period (Table 1).
Fig. 1.
Study flow diagram. OAT: Opioid agonist treatment; OAT receipt based on self-report.
Table 1.
Descriptive characteristics of participants at baseline.
| %§
|
|
|---|---|
| Participants (N) | 443 |
| Age (Median [IQR]) | 47 [40, 52] |
| Male gender | 63.2 |
| Completed High School | 52.0 |
| Aboriginal | 32.5 |
| White | 63.0 |
| Ever been homeless | 92.8 |
| Ever been in jail | 39.5 |
| HIV+ | 37.7 |
| HCV+ | 92.1 |
| Any physical disability | 81.3 |
| Ever had mental illness diagnosed | 62.3 |
| Ever attempted suicide | 17.9 |
| Age of first injection drug use (Median [IQR]) | 18 [15, 25] |
| Ever overdosed | 63.9 |
| Longitudinal illicit opioid‡ use | |
| Reported at every follow-up | 24.6 |
| Reported at one follow-up or more | 69.1 |
| Not reported at any follow-up | 30.9 |
| Longitudinal stimulant¶ use | |
| Reported at every follow-up | 13.5 |
| Reported at one follow-up or more | 50.1 |
| Not reported at any follow-up | 49.9 |
| Longitudinal OAT receipt | |
| Reported at every follow-up | 61.6 |
| Reported at one follow-up or more | 90.5 |
| Not reported at any follow-up | 9.5 |
Percentage of study sample, unless otherwise noted.
IQR: interquartile range
HIV+: Human Immunodeficiency Virus positive
HCV+: Hepatitis C positive
Including heroin, morphine and prescription opioids
Including crack, cocaine, speed and methamphetamine
Results for the models we examined can be found in Table 2. The model with three HRQoL latent classes had the lowest absolute BIC value. As assessed using the BIC log Bayes factor approximation, we found very strong evidence favoring a three-class model over a two-class model (BIC log Bayes = 60.34) and results also favored a three-class model over a more complex four-class model (BIC log Bayes = −5.15). The shape of all three trajectories for the best fitting model was characterized by a constant term only. We thus selected a model with three constant classes in order to assign latent class membership to individuals. We defined these as: stably high, stably moderate and stably low HRQoL.
Table 2.
Bayesian Information Criterion values for model selection.
| BIC§ | Null Model | 2(ΔBIC)† | |
|---|---|---|---|
|
|
|||
| Number of Groups | |||
| 2 | −456.94 | ||
| 3 | −426.77 | 2 | 60.34 |
| 4 | −429.34 | 3 | −5.15 |
| 5 | −435.44 | 4 | −12.19 |
| Order of groups for model with 3 groups | |||
| 0 (Constant) | −426.77 | ||
| 1 (Linear) | −432.09 | 0 | −10.64 |
| 2 (Quadratic) | −439.63 | 1 | −15.08 |
| 3 (Cubic) | −447.56 | 2 | −15.86 |
BIC: Bayesian Information Criterion
2(ΔBIC) is the approximation of the BIC log Bayes factor, 2loge(B10)
Probabilistic class membership assignment resulted in the majority of individuals assigned to the stably moderate class (N=260, 58.7%) and almost a quarter of the individuals assigned to the stably high class (N=107, 24.2 %). The smallest class was the stably low (N=76, 17.2%). Detailed estimation results from the LCGA are presented in Table 3, which include estimates for the coefficients of time-varying covariates affecting HRQoL trajectory as well as the estimates for the log odds ratios of time-invariant covariates affecting class membership. While OAT receipt was not significantly associated with HRQoL trajectories across latent classes, stimulant use was significantly negatively associated with the stably high trajectory (Non-daily use coefficient: −0.109, standard error (SE): 0.041; daily use: −0.167, SE: 0.066). Further, daily illicit opioid use was also negatively associated with the stably moderate trajectory (−0.056, SE: 0.025). Time-invariant indicators of physical disability and a history of mental health were both significant in reducing the probability of assignment to a higher latent class. Using the stably moderate class as reference, a history of mental illness would increase threefold the probability of being assigned to the stably low latent class (Log odds ratio (Log OR): 1.184; SE: 0.519) and reduce by more than a factor of five the assignment to the stably high class (Log OR: −1.767; SE: 0.349). Similarly, having a physical disability would reduce by more than half the probability of being assigned to the stably high class (Log OR: −0.893; SE: 0.423). The estimated coefficient for physical disability in the stably low class was of very large magnitude in predicting assignment to the stably low class (Log OR: 2.800; SE: 1.977), yet it was not statistically significant. Given that all 76 individuals assigned to the stably low HRQoL class reported having a physical disability this estimation result is suggestive of insufficient observations for precise estimation as the association is clearly very strong.
Table 3.
Results from latent class growth analysis (LCGA) based on EQ-5D† score trajectories (N = 443).
|
|
||||||
|---|---|---|---|---|---|---|
| Latent HRQoL classes
|
||||||
| Stably High | Stably Moderate | Stably Low | ||||
|
|
|
|
||||
| Class assignment‡ | N | % | N | % | N | % |
|
|
|
|
||||
| 107 | 24.2 | 260 | 58.7 | 76 | 17.2 | |
| Parameter estimates of trajectories | β | S.E. | β | S.E. | β | S.E. |
|
|
|
|
||||
| Constant | 1.207* | (0.058) | 0.871* | (0.023) | 0.613* | (0.049) |
| OAT receipt | −0.027 | (0.047) | −0.017 | (0.021) | −0.023 | (0.040) |
| Illicit opioid use, non-daily | −0.040 | (0.040) | −0.023 | (0.019) | 0.035 | (0.031) |
| Illicit opioid use, daily | −0.084 | (0.053) | −0.056* | (0.025) | −0.014 | (0.045) |
| Stimulant use, non-daily | −0.109* | (0.041) | −0.029 | (0.018) | 0.023 | (0.032) |
| Stimulant use, daily | −0.167* | (0.066) | −0.059 | (0.033) | −0.020 | (0.054) |
| Class membership probability | Log OR | S.E. | Referent class | Log OR | S.E. | |
|
|
|
|
||||
| Age at baseline | 0.003 | (0.022) | - | 0.011 | (0.027) | |
| Gender | 0.021 | (0.364) | - | −0.108 | (0.407) | |
| White | −1.461* | (0.652) | - | 1.083 | (1.681) | |
| Aboriginal | −0.519 | (0.677) | - | 0.493 | (1.716) | |
| Physical disability | −0.893* | (0.423) | - | 2.800 | (1.977) | |
| Mental illness, ever | −1.767* | (0.349) | - | 1.184* | (0.519) | |
| HIV+ | 0.046 | (0.362) | - | 0.614 | (0.401) | |
| HCV+ | 0.119 | (0.625) | - | −0.824 | (0.671) | |
Statistically significant at the 5% level.
EQ-5D is a preference weighted multi-attribute index value for health utility.
Class assignment was based on posterior probability of membership.
N: Number of individuals
HIV+: Human Immunodeficiency Virus positive
HCV+: Hepatitis C positive
Log OR: Log odds ratio
S.E.: Standard Error
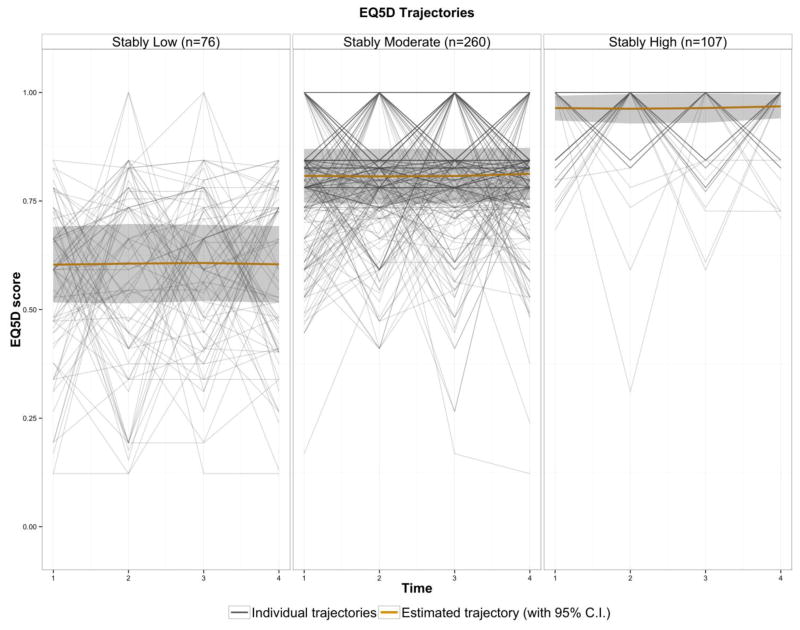
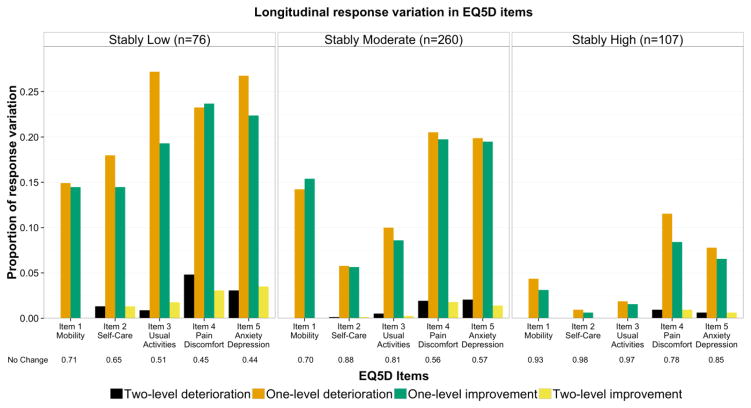
Figure 2 presents each of the three HRQoL latent classes’ estimated trajectory with 95% confidence intervals as well as individual trajectories. Crucially, none of the confidence intervals overlap indicating three clearly distinct estimated trajectory classes. Substantial individual longitudinal variation of the EQ-5D score was observed across classes and Figure 3 presents the cumulative variation in each EQ-5D item between each completed assessment. No change was most frequently observed and two-level changes were rare: maximum observed proportion of two-level deterioration was 4.8% for the domain capturing pain and/or discomfort in the stably low class and the maximum two-level improvement was 3.5% for the domain capturing anxiety and/or depression also in the stably low class. One level changes in the domain capturing pain and/or discomfort were present in each class with proportions generally twice as large for the stably low (one-level deterioration 23.2%; one-level improvement 23.7%) and stably moderate classes (20.5%; 19.7%) compared to the stably high class (11.5%; 8.4%); results for the domain capturing anxiety and/or depression for the stably low (26.7%; 22.4%) and stably moderate (19.9%; 19.5%) compared to the stably high (7.8%; 6.5%) were almost three times as large. The main differentiating domains between the stably low and stably moderate classes were those capturing difficulty with both self-care (one-level deterioration stably low class was 18.0% vs. 5.8% for the stably moderate class; one-level improvement 14.5% vs. 5.6%) and in the conducting of usual activities (27.2% vs. 10.0%; 19.3% vs. 8.6%).
Fig. 2.
Estimated HRQoL longitudinal trajectory, with shaded 95% confidence intervals (95% C.I.), for each of the latent classes. Despite the constant estimated HRQoL trajectories for each latent class, the figure highlights the heterogeneous individual EQ-5D trajectories composing each latent class. EQ-5D is a preference weighted multi-attribute index value for HRQoL
Fig. 3.
Proportion of response variation compared to previous assessment for every individual (N=443) in each health-related quality of life latent class, for each EQ-5D item. Each EQ-5D item has 3 levels: no problems, some problems, extreme problems and thus variation can either be two-level deterioration or improvement, one-level deterioration or improvement, or no change. Results of no change compared to previous assessment are presented below the figure for emphasis on variation between latent classes. EQ-5D is a preference weighted multi-attribute index value for HRQoL
Results of our sensitivity analyses found no significant statistical differences in demographics between individuals included from those excluded, (Table 1A, supplementary appendix). Finally, our results were robust when conducted on the subset of individuals included in our study sample that did not report any illicit opioid use over the study period. Results are presented in the supplementary material (Table 2A & Table 3A).
4. CONCLUSIONS
We found long-term trajectories of HRQoL among individuals with OUD to be stable regardless of self-reported receipt of OAT with methadone. Our findings further suggest that different HRQoL levels existed in our study population. This observed longitudinal stability of HRQoL – measured in 6 month intervals regardless of treatment receipt - appears to be consistent with findings for individuals with OUD in short-term studies focusing on treatment initiation. The short-term improvement effect sizes found by Nosyk et al. (2015) for individuals in OAT were relatively small (0.039–0.072) and subsequently either increased at a diminished rate or decreased; early improvement and subsequent deterioration was also observed in a majority of the individuals with OUD in another study (Nosyk et al., 2011), which also found stable high and low HRQoL classes. Our study suggests that the short-term HRQoL gains following OAT initiation found in aforementioned studies may in fact diminish to baseline levels over time.
In terms of the direct implications on estimating QALYs in the context of CEA, these results suggest that the use of a greater value of HRQoL during OAT engagement compared to being out-of-treatment is likely not representative of the durability of the HRQoL response to OAT, and could over-estimate total QALY gains accrued in treatment. This distinction may be consequential when estimating the relative value for money of alternative treatment modalities and medications in CEA, which rely on health state-specific HRQoL measures to evaluate QALY benefits. Uncertainty surrounding health utility valuations had an effect on the findings in at least one prior CEA for the treatment of OUD (Schackman et al., 2012). Short-term HRQoL improvements associated with OAT initiation may be attributable, in part, to the reduction in drug use, which may wane over the course of treatment. Our findings of a strong negative association between stimulant use and a probability of high HRQoL class contrasted with previous findings of no short-term HRQoL association with stimulant use among individuals receiving treatment for OUD (Nosyk, Bray, et al., 2015), further emphasizing the distinction between the short-term and longitudinal effects of continued drug use. Otherwise, it is possible that the longitudinal stabilization of HRQoL is characterizing a change in perspective rather than the absence of meaningful change in levels of HRQoL. This adaptation to change in HRQoL, or response shift, has been suggested as a potentially important component of the full effect of treatment (Schwartz, Andresen, Nosek, & Krahn, 2007; Sprangers & Schwartz, 1999). We note that our self-reported measure of OAT receipt at the time of the interview lacked potentially important contextual information such as medication dosage, proximity to OAT initiation, and cumulative exposure to treatment. A more detailed examination with more frequent HRQoL measurements and complete information on medication receipt may further clarify the long-term effects of OAT on HRQoL, in the interest of producing unbiased assessments of competing treatment modalities. It should be clear, however, that the QALY gains derived from the reduction in the risk of mortality attributable to OAT (Degenhardt et al., 2011; Evans et al., 2015; Nosyk, Min, et al., 2015), drive results in economic modeling efforts and underline the importance of this life-saving treatment.
Heterogeneous life trajectories of heroin use (Hser, Huang, Chou, & Anglin, 2007) are best treated by long-term care strategies (Bart, 2012; Hser, Longshore, & Anglin, 2007) and our results on the variation in the item responses composing the EQ-5D serve to further emphasize that treatment outcome objectives should be based on a physical, mental and social conceptualization of health and not only on use reduction or cessation. Indeed, lower HRQoL classes had more variation in the item assessing anxiety and depression than higher latent classes while the stably low class had two to three times more variation in the items assessing self-care and ability to conduct usual activities than the stably moderate class. Although treatment for SUD is often delivered in serial episodes resembling acute care (Dennis et al., 2003; McLellan et al., 2005), there has been an emergent movement in the U.S. towards a recovery-oriented model of care (Laudet & White, 2010). Recent findings that mental and/or SUD readmissions account for the largest share of readmissions among adult Medicaid beneficiaries in nineteen states (Trudnak et al., 2014) highlight the need for more widely adopted long-term and comprehensive care consistent with disease etiology. For example, in British Columbia (BC) Canada, guidelines facilitate prescribing methadone for maintenance-oriented or non-time limited OAT (College of Physicians and Surgeons of British Columbia, 2014). Further, methadone is covered in BC for reimbursement under standard provincial drug benefit formularies, whereby ability to pay dictates co-payment levels. Alternatively in the U.S., more than 50% of the 465,467 people admitted for opioid-related treatment in 2011 reported no health insurance (Substance Abuse and Mental Health Services Administration, 2013). Given the changing U.S. policy landscape under the Affordable Care Act, which now requires insurers to treat SUD in the same way they would any other chronic disease, the number of admissions into treatment should increase. Preferably, SUD should thus be considered an opportunity for supplementary care delivery to address individuals’ HRQoL.
This analysis has several limitations. First, given universal coverage of medical care in Canada, widespread access to OAT in BC, and the selective sample we’ve focused on in our analysis (excluding individuals missing biannual assessments), our results may not be generalizable to disparate settings and patient populations. Nonetheless, our study, conducted within a set of prospective cohort studies, represents a rare opportunity to observe HRQoL patterns over an extended timeframe in a highly marginalized population, and thus stands as an important contribution to the literature in this domain. Second, as noted above, our measure of OAT receipt did not capture important contextual factors such as medication dosage and duration of retention, and only focused on one treatment modality. Further study, with more frequent HRQoL measurement and complete information on, ideally, multiple treatment regimens, would help clarify the persistence of the effect of OAT on HRQoL over time.
In conclusion, three different classes of long-term stable HRQoL trajectories existed in our study population of individuals with OUD and with a history of OAT. Current receipt of OAT with methadone did not play a significant role in determining HRQoL trajectory while both physical disability and mental health comorbidities were influential in the probabilistic membership assignment to a lower HRQoL class.
Supplementary Material
Highlights.
Longitudinal health related quality of life (HRQoL) trajectories are described
Longitudinal trajectories were stable regardless of opioid agonist treatment receipt (OAT)
Different HRQoL levels existed in our study population
A greater value of HRQoL during OAT is likely not representative of the durability of the HRQoL response
Quality-adjusted life year benefits could be over-estimated in OAT economic evaluations
Acknowledgments
The authors thank the VIDUS, ACCESS and ARYS study participants for their contribution to the research, as well as current and past researchers and staff. The authors also thank Bruce R. Schackman and Eve Wittenberg.
Footnotes
Conflicts of interest: none.
Declaration of interest: This project is funded by the US National Institutes of Health (R01DA031727 and R01DA033424). In addition, the VIDUS study was supported by the US National Institutes of Health (R01DA011591, U01DA038886). The ACCESS study was supported by the US National Institutes of Health (R01DA021525). The ARYS study was supported by the US National Institutes of Health (R01DA028532) and the Canadian Institutes of Health Research (MOP–102742). This research was undertaken, in part, thanks to the funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr. Evan Wood. The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28(4):321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Astals M, Domingo-Salvany A, Buenaventura CC, Tato J, Vazquez JM, Martin-Santos R, Torrens M. Impact of substance dependence and dual diagnosis on the quality of life of heroin users seeking treatment. Substance Use and Misuse. 2008;43(5):612–632. doi: 10.1080/10826080701204813. [DOI] [PubMed] [Google Scholar]
- Bansback N, Tsuchiya A, Brazier J, Anis A. Canadian valuation of EQ-5D health states: preliminary value set and considerations for future valuation studies. PloS one. 2012;7(2):e31115. doi: 10.1371/journal.pone.0031115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bart G. Maintenance medication for opiate addiction: the foundation of recovery. J Addict Dis. 2012;31(3):207–225. doi: 10.1080/10550887.2012.694598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J, Burrell T, Indig D, Gilmour S. Cycling in and out of treatment; participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend. 2006;81(1):55–61. doi: 10.1016/j.drugalcdep.2005.05.010. [DOI] [PubMed] [Google Scholar]
- Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- Cameron AC, Trivedi PK. Microeconometrics: Methods and Applications. 1. New York (NY): Cambridge University Press; 2005. [Google Scholar]
- Caro JJ, Briggs AH, Siebert U, Kuntz KM. Modeling Good Research Practices—Overview A Report of the ISPOR-SMDM Modeling Good Research Practices Task Force–1. Medical Decision Making. 2012;32(5):667–677. doi: 10.1177/0272989X12454577. [DOI] [PubMed] [Google Scholar]
- College of Physicians and Surgeons of British Columbia. Methadone Maintenance Program: Clinical Practice Guideline. 2014 Retrieved from https://www.cpsbc.ca/files/pdf/MMP-Clinical-Practice-Guideline-2014-02.pdf.
- Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z. Methadone and buprenorphine for the management of opioid dependence: A systematic review and economic evaluation. Health Technology Assessment. 2007;11(9):190. doi: 10.3310/hta11090. [DOI] [PubMed] [Google Scholar]
- De Maeyer J, Van Nieuwenhuizen C, Bongers IL, Broekaert E, Vanderplasschen W. Profiles of quality of life in opiate-dependent individuals after starting methadone treatment: A latent class analysis. International Journal of Drug Policy. 2013;24(4):342–350. doi: 10.1016/j.drugpo.2012.09.005. [DOI] [PubMed] [Google Scholar]
- De Maeyer J, Vanderplasschen W, Broekaert E. Quality of life among opiate-dependent individuals: A review of the literature. International Journal of Drug Policy. 2010;21(5):364–380. doi: 10.1016/j.drugpo.2010.01.010. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M, McLaren J. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106(1):32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26(3):339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkgraaf MGW, van der Zanden BP, de Borgie CAJM, Blanken P, van Ree JM, van den Brink W. Cost utility analysis of co-prescribed heroin compared with methadone maintenance treatment in heroin addicts in two randomised trials. BMJ. 2005;330(15933353):1297–1297. doi: 10.1136/bmj.330.7503.1297. Retrieved from http://www.hubmed.org/display.cgi?uids=15933353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Li L, Min J, Huang D, Urada D, Liu L, … Nosyk B. Mortality among individuals accessing pharmacological treatment for opioid dependence in California, 2006–10. Addiction. 2015;110(6):996–1005. doi: 10.1111/add.12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faggiano F, Vigna-Taglianti F, Versino E, Lemma P. Methadone maintenance at different dosages for opioid dependence. Cochrane Database Syst Rev. 2003;(3):CD002208. doi: 10.1002/14651858.CD002208. [DOI] [PubMed] [Google Scholar]
- Falck RS, Wang J, Siegal HA, Carlson RG. Longitudinal application of the medical outcomes study 36-item short-form health survey with not-in-treatment crack-cocaine users. Medical care. 2000;38(9):902–910. doi: 10.1097/00005650-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Giacomuzzi S, Riemer Y, Ertl M, Kemmler G, Rössler H, Hinterhuber H, Kurz M. Buprenorphine versus methadone maintenance treatment in an ambulant setting: a health-related quality of life assessment. Addiction. 2003;98(5):693–702. doi: 10.1046/j.1360-0443.2003.00352.x. [DOI] [PubMed] [Google Scholar]
- Health Canada. Best Practices, Methadone Maintenance Treatment. 2002 Retrieved from http://www.hc-sc.gc.ca/hc-ps/pubs/adp-apd/methadone-bp-mp/index-eng.php.
- Hser Y, Huang D, Chou C, Anglin M. Trajectories of heroin addiction: growth mixture modeling results based on a 33-year follow-up study. Eval Rev. 2007;31(6):548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- Hser Y, Longshore D, Anglin M. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval Rev. 2007;31(6):515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods & Research. 2007;35(4):542–571. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29(3):374–393. [Google Scholar]
- Karow A, Reimer J, Schäfer I, Krausz M, Haasen C, Verthein U. Quality of life under maintenance treatment with heroin versus methadone in patients with opioid dependence. Drug and Alcohol Dependence. 2010;112(3):209–215. doi: 10.1016/j.drugalcdep.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Kertesz SG, Larson MJ, Horton NJ, Winter M, Saitz R, Samet JH. Homeless chronicity and health-related quality of life trajectories among adults with addictions. Medical care. 2005;43(6):574–585. doi: 10.1097/01.mlr.0000163652.91463.b4. [DOI] [PubMed] [Google Scholar]
- Korthuis PT, Tozzi MJ, Nandi V, Fiellin DA, Weiss L, Egan JE, … Hersh D. Improved Quality of Life for Opioid Dependent Patients Receiving Buprenorphine Treatment in HIV Clinics. Journal of acquired immune deficiency syndromes 1999. 2011;56(Suppl 1):S39. doi: 10.1097/QAI.0b013e318209754c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. Journal of Substance Abuse Treatment. 2010;38(1):51–59. doi: 10.1016/j.jsat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick R, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008;(2) doi: 10.1002/14651858.CD002207.pub3. [DOI] [PubMed] [Google Scholar]
- McLellan T, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA : the journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11015800. [DOI] [PubMed] [Google Scholar]
- McLellan T, McKay J, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Miller PG, Miller WR. What should we be aiming for in the treatment of addiction? Addiction. 2009;104(5):685–686. doi: 10.1111/j.1360-0443.2008.02514.x. [DOI] [PubMed] [Google Scholar]
- Millson P, Challacombe L, Villeneuve PJ, Strike CJ, Fischer B, Myers T, … Hopkins S. Determinants of health-related quality of life of opiate users at entry to low-threshold methadone programs. European Addiction Research. 2006;12(2):74–82. doi: 10.1159/000090426. [DOI] [PubMed] [Google Scholar]
- Muthén B. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran. 2003 doi: 10.1037/1082-989X.8.3.369. [DOI] [PubMed] [Google Scholar]
- Nagin D. Group-based modeling of development. Harvard University Press; 2009. [Google Scholar]
- National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. Effective medical treatment of opiate addiction. Journal of the American Medical Association. 1998;280(22):1936–1943. [PubMed] [Google Scholar]
- Nosyk B, Bray JW, Wittenberg E, Aden B, Eggman AA, Weiss RD, … Schackman BR. Short term health-related quality of life improvement during opioid agonist treatment. Drug and Alcohol Dependence. 2015;157:121–128. doi: 10.1016/j.drugalcdep.2015.10.009. doi: http://dx.doi.org/10.1016/j.drugalcdep.2015.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Guh DP, Bansback NJ, Oviedo-Joekes E, Brissette S, Marsh DC, … Anis AH. Cost-effectiveness of diacetylmorphine versus methadone for chronic opioid dependence refractory to treatment. CMAJ. 2012;184(22410375):317–328. doi: 10.1503/cmaj.110669. Retrieved from http://www.hubmed.org/display.cgi?uids=22410375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Guh DP, Sun H, Oviedo-Joekes E, Brissette S, Marsh DC, … Anis AH. Health related quality of life trajectories of patients in opioid substitution treatment. Drug and Alcohol Dependence. 2011;118(2):259–264. doi: 10.1016/j.drugalcdep.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Nosyk B, MacNab YC, Sun H, Marsh DC, Fischer B, Schechter MT, Anis AH. Proportional hazards frailty models for recurrent methadone maintenance treatment. American Journal of Epidemiology. 2009;170(6):783–792. doi: 10.1093/aje/kwp186. [DOI] [PubMed] [Google Scholar]
- Nosyk B, Min JE, Evans E, Li L, Liu L, Lima VD, … Montaner JS. The effects of opioid substitution treatment and highly active antiretroviral therapy on the cause-specific risk of mortality among HIV positive people who inject drugs. Clinical Infectious Diseases. 2015:civ476. doi: 10.1093/cid/civ476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Sun H, Guh DP, Oviedo-Joekes E, Marsh DC, Brissette S, … Anis AH. The quality of eight health status measures were compared for chronic opioid dependence. Journal of clinical epidemiology. 2010;63(10):1132–1144. doi: 10.1016/j.jclinepi.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling. 2007;14(4):535–569. [Google Scholar]
- Palepu A, Tyndall MW, Joy R, Kerr T, Wood E, Press N, … Montaner JS. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: The role of methadone maintenance therapy. Drug Alcohol Depend. 2006;84(2):188–194. doi: 10.1016/j.drugalcdep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Ponizovsky AM, Grinshpoon A. Quality of life among heroin users on buprenorphine versus methadone maintenance. The American journal of drug and alcohol abuse. 2007;33(5):631–642. doi: 10.1080/00952990701523698. [DOI] [PubMed] [Google Scholar]
- Puigdollers E, Domingo-Salvany A, Brugal MT, Torrens M, Alvarós J, Castillo C, … Vázquez JM. Characteristics of heroin addicts entering methadone maintenance treatment: quality of life and gender. Substance Use and Misuse. 2004;39(9):1353–1368. doi: 10.1081/ja-120039392. [DOI] [PubMed] [Google Scholar]
- Schackman BR, Leff JA, Polsky D, Moore BA, Fiellin DA. Cost-effectiveness of long-term outpatient buprenorphine-naloxone treatment for opioid dependence in primary care. Journal of General Internal Medicine. 2012;27(6):669–676. doi: 10.1007/s11606-011-1962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz CE, Andresen EM, Nosek MA, Krahn GL. Response shift theory: important implications for measuring quality of life in people with disability. Archives of Physical Medicine and Rehabilitation. 2007;88(4):529–536. doi: 10.1016/j.apmr.2006.12.032. [DOI] [PubMed] [Google Scholar]
- Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: Development and testing of the D1 valuation model. Medical care. 2005;43(3):203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Social Science & Medicine. 1999;48(11):1507–1515. doi: 10.1016/s0277-9536(99)00045-3. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, … O’Shaughnessy MV. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS. 1997;11(8):F59–F65. doi: 10.1097/00002030-199708000-00001. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS): 2001–2011. Rockville, MD: 2013. Publication No. (SMA) 13-4772. [Google Scholar]
- The EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Trudnak T, Kelley D, Zerzan J, Griffith K, Jiang HJ, Fairbrother GL. Medicaid Admissions And Readmissions: Understanding The Prevalence, Payment, And Most Common Diagnoses. Health Affairs. 2014;33(8):1337–1344. doi: 10.1377/hlthaff.2013.0632. [DOI] [PubMed] [Google Scholar]
- Tyndall MW, Currie S, Spittal P, Li K, Wood E, O’Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17(6):887–893. doi: 10.1097/00002030-200304110-00014. [DOI] [PubMed] [Google Scholar]
- Uhlmann S, Milloy MJ, Kerr T, Zhang R, Guillemi S, Marsh D, … Wood E. Methadone maintenance therapy promotes initiation of antiretroviral therapy among injection drug users. Addiction. 2010;105(5):907–913. doi: 10.1111/j.1360-0443.2010.02905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Zanden BP, Dijkgraaf MG, Blanken P, de Borgie CA, Ree JMv, Brink Wvd. Validity of the EQ-5D as a generic health outcome instrument in a heroin-dependent population. Drug and Alcohol Dependence. 2006;82(2):111–118. doi: 10.1016/j.drugalcdep.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Veilleux JC, Colvin PJ, Anderson J, York C, Heinz AJ. A review of opioid dependence treatment: pharmacological and psychosocial interventions to treat opioid addiction. Clinical Psychology Review. 2010;30(2):155–166. doi: 10.1016/j.cpr.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Winklbaur B, Jagsch R, Ebner N, Thau K, Fischer G. Quality of life in patients receiving opioid maintenance therapy. A comparative study of slow-release morphine versus methadone treatment. European Addiction Research. 2008;14(2):99. doi: 10.1159/000113724. [DOI] [PubMed] [Google Scholar]
- Wood E, Hogg R, Kerr T, Palepu A, Zhang R, Montaner J. Impact of accessing methadone on the time to initiating HIV treatment among antiretroviral-naive HIV-infected injection drug users. AIDS. 2005;19(8):837–839. doi: 10.1097/01.aids.0000168982.20456.eb. [DOI] [PubMed] [Google Scholar]
- Wood E, Kerr T, Marshall BDL, Li K, Zhang R, Hogg RS, … Montaner JSG. Longitudinal community plasma HIV-1-RNA concentrations and incidence of HIV-1 among injecting drug users: a prospective cohort study. BMJ. 2009;338:1191–1194. doi: 10.1136/bmj.b1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Li K, Montaner JS, Kerr T. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction. 2006;101(5):689–695. doi: 10.1111/j.1360-0443.2006.01385.x. [DOI] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: the ARYS study. Harm Reduct J. 2006;3:18. doi: 10.1186/1477-7517-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang CC. Evaluating latent class analysis models in qualitative phenotype identification. Computational Statistics & Data Analysis. 2006;50(4):1090–1104. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.