Abstract
Introduction
People with mobility limitations can benefit from rehabilitation programmes that provide a high dose of exercise. However, since providing a high dose of exercise is logistically challenging and resource-intensive, people in rehabilitation spend most of the day inactive. This trial aims to evaluate the effect of the addition of affordable technology to usual care on physical activity and mobility in people with mobility limitations admitted to inpatient aged and neurological rehabilitation units compared to usual care alone.
Methods and analysis
A pragmatic, assessor blinded, parallel-group randomised trial recruiting 300 consenting rehabilitation patients with reduced mobility will be conducted. Participants will be individually randomised to intervention or control groups. The intervention group will receive technology-based exercise to target mobility and physical activity problems for 6 months. The technology will include the use of video and computer games/exercises and tablet applications as well as activity monitors. The control group will not receive any additional intervention and both groups will receive usual inpatient and outpatient rehabilitation care over the 6-month study period. The coprimary outcomes will be objectively assessed physical activity (proportion of the day spent upright) and mobility (Short Physical Performance Battery) at 6 months after randomisation. Secondary outcomes will include: self-reported and objectively assessed physical activity, mobility, cognition, activity performance and participation, utility-based quality of life, balance confidence, technology self-efficacy, falls and service utilisation. Linear models will assess the effect of group allocation for each continuously scored outcome measure with baseline scores entered as a covariate. Fall rates between groups will be compared using negative binomial regression. Primary analyses will be preplanned, conducted while masked to group allocation and use an intention-to-treat approach.
Ethics and dissemination
The protocol has been approved by the relevant Human Research Ethics Committees and the results will be disseminated widely through peer-reviewed publication and conference presentations.
Trial registration number
ACTRN12614000936628. Pre-results.
Keywords: mobility, protocol, physical activity, technology
Strengths and limitations of this study.
Adequately powered to detect effects on the use of affordable technology integrated into usual rehabilitation care on important mobility outcomes.
Technologies to enable ongoing exercise are likely to become increasingly important in the future as the proportion of older people in the population increases and resources to provide rehabilitation care become more limited.
One limitation of this study is that the technology prescription and health coaching support requires tailoring to the individual participant, which complicates description of the experimental intervention and the dose of intervention delivered. Careful reporting of the technologies prescribed, the number, mode and topics delivered during the health coaching sessions and the use of practice sheets to record dosage of exercise will be required to accurately communicate the intervention details.
Introduction
Mobility limitation is common in people undertaking inpatient rehabilitation, can result from conditions such as stroke, brain injury, hip fracture and arthritis1 and is exacerbated by physiological ageing and inactivity.2 People with mobility limitation can benefit from rehabilitation programmes,3–5 particularly rehabilitation programmes that contain intensive repetitive exercises.6–9 Systematic reviews of randomised trials show that higher doses of exercise in the post-acute phase are associated with better outcomes in people after stroke5 10 11 and people after hip fracture3 and better fall prevention effects in older people.12 However, observational studies in developed countries have found that people in rehabilitation units spend most of the day alone and inactive, with very little time spent in activities likely to promote recovery.13 14
New technologies potentially provide an affordable way to increase the dose of exercise and overall physical activity for people in rehabilitation. Exercise-based video and computer games/exercises and activity monitors are increasingly being used in rehabilitation settings to provide feedback on motor performance and physical activity. These devices (eg, Nintendo Wii, Microsoft Kinect for Xbox, Fitbit) are relatively inexpensive (A$80–400), widely available and have been shown to enhance enjoyment of exercise15 16 and increase the dose of repetitive exercise completed in rehabilitation settings.17–21
Systematic reviews evaluating new technologies in older adults,22 people with balance impairment23 and stroke survivors24 25 are yet to confidently determine the effect of providing additional exercise using technology on mobility.24 25 The majority of the studies included in these reviews have small sample sizes and the trial designs are either poorly reported or have a high risk of bias. In addition, these studies typically have used only one type of technology for all participants, limiting the applicability of technology across a spectrum of mobility limitations and recovery time. Some technologies tested in studies included in these reviews would be unaffordable for many rehabilitation units, even in more developed countries. A recent randomised feasibility study (n=58; average age 80 years) conducted by our team tested the addition of more affordable, tailored, video-based and computer-based interactive exercises in addition to usual care with usual care alone for people undergoing inpatient aged and neurological rehabilitation.26 This relatively brief intervention (on average 6 intervention sessions over 2 weeks) was well accepted (86% of participants completed the intervention), safe, enjoyable and demonstrated task-specific improvements in balance compared to the usual care group (between-group difference on Maximal Balance Range test at 2 weeks after baseline adjustment was 38 mm, 95% CI 6 to 69), but did not improve overall mobility. Although this tailored approach to delivering task-specific repetitive exercise using a suite of technologies appears promising, it requires rigorous evaluation with an adequately powered randomised controlled trial. We will now conduct such a trial after refining the intervention tested in our pilot trial.
The primary research question is:
What is the effect of the addition of affordable technology to usual care on physical activity levels (upright time) and mobility 6 months after randomisation in people with mobility limitations admitted to inpatient aged and neurological rehabilitation units compared to usual care alone?
Secondary research questions are:
What is the effect of the addition of affordable technology to usual care on physical activity levels and mobility 3 weeks after randomisation in people with mobility limitations admitted to inpatient aged and neurological rehabilitation units compared to usual care alone?
What is the effect of the addition of affordable technology to usual care on cognition (3 weeks and 6 months after randomisation), self-reported physical activity, activity performance and participation, utility-based quality of life, balance confidence, technology self-efficacy (3 and 12 weeks and 6 months after randomisation) and falls (over the 6-month period after randomisation) in people with mobility limitations admitted to inpatient aged and neurological rehabilitation units compared to usual care alone?
How do participants randomised to the intervention group report the usability and enjoyment of technologies prescribed in this trial at 3 and 12 weeks and 6 months after randomisation?
Other research questions are:
What is the cost-effectiveness of the intervention compared to usual care over the 6-month period after randomisation?
What factors predict greater use of technology for participants randomised to the intervention group over the 6-month period after randomisation?
What are the experiences of participants and staff using affordable technology for physical rehabilitation?
Method
Design
A pragmatic assessor-blinded multicentre superiority randomised controlled trial with two parallel groups will be undertaken. The design of the trial is presented in figure 1. The CONSORT statements for non-pharmaceutical27 and pragmatic28 trials will be used to guide trial conduct and will be reported according to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines as well as the TIDieR framework for intervention description.29 30 Using trial data, an Incremental Cost-Effectiveness Ratio will be calculated to assess the intervention's relative costs and benefits in terms of gain in mobility and quality of life. A qualitative substudy using a grounded theory approach with structured interviews will be conducted among a subset (n=30–50) of intervention participants and study staff.
Figure 1.
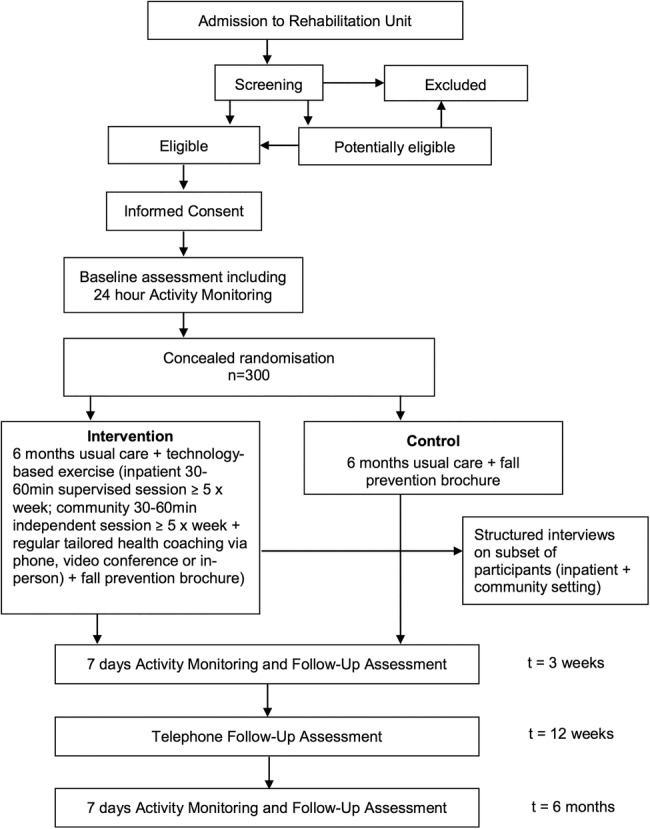
Trial design.
Participants and study sites
Research physiotherapists employed for the trial will recruit 300 inpatients from the aged and neurological rehabilitation wards at two metropolitan hospitals in Sydney and Adelaide, Australia; and from a metropolitan specialised brain injury unit in Sydney, Australia. We anticipate a total of 10 participants to be recruited every 3 weeks with different recruitment rates at each site due to differences in bed numbers and length of stay. All patients admitted to the study wards during the study period will be screened for eligibility in accordance with the inclusion and exclusion criteria. Those patients deemed potentially eligible will continue to be screened until they either meet eligibility or are ineligible. Patients will be eligible for recruitment if they are at least 18 years old; have reduced mobility (Short Physical Performance Battery (SPPB) score of <12);31 clinician-assessed capacity for improvement in mobility; likely life expectancy of more than 12 months; anticipated length of stay of ≥10 days; and an ability to maintain a standing position with the assistance of one person as a minimum standard.
Potential participants will be excluded if they have cognitive impairment likely to interfere with their ability to use the technology; insufficient English language skills to participate in the intervention and no available interpreter; inadequate vision to use the devices; medical condition(s) precluding exercise (unstable cardiac disease, uncontrolled hypertension, uncontrolled metabolic diseases, large abdominal aortic aneurysm or a weight-bearing restriction); lack of interest in the use of the technologies; anticipated discharge to high care residential facility or to a location too far from study site to allow home visits and follow-up assessments.
Recruitment and allocation
A variable block randomisation schedule will be prepared from a computer-generated list of random numbers by a researcher not involved in the trial. The randomisation schedule will incorporate stratification for study site and health condition (whether or not the person has a neurological condition that affects daily activities) and be embedded in a secure online database (REDCap) to achieve allocation concealment. Patients who are identified by the research physiotherapist as fulfilling the eligibility criteria will be invited to participate. Prior to obtaining written consent, the most recent Mini Mental State Examination32 (MMSE) score will be extracted from the clinical notes, or where one has not been completed in the past week, an MMSE will be conducted by the research physiotherapist to determine the patient's capacity to provide informed consent. Informed consent will be sought from the eligible patient, or by proxy from the patient's ‘person responsible’ if they score <21 on the MMSE. Once the participant gives informed consent and completes the baseline assessment (including 24-hour activity monitoring), the research physiotherapist will complete the randomisation process in REDCap to determine allocation to either the intervention group (usual care+technology-based exercise) or the control group (usual care). Owing to the type of intervention, it will not be possible to blind the research physiotherapist delivering the intervention or the study participant to group allocation.
Intervention
Usual care: received by both groups
Participants in both groups will receive usual inpatient and outpatient rehabilitation care. Usual care at the three study sites will involve participants being assessed by hospital-employed physiotherapists who will prescribe a series of repetitive exercises (eg, practice of standing up or stepping). The conduct of these exercises will be supervised by the physiotherapists, physiotherapy assistants or family members. Usual care will also include assessment and tailored management by medical specialists, nurses, occupational therapists, speech pathologists, social workers, nutritionists, orthoptists and other health professionals as required. At time of discharge, participants will be referred to follow-up outpatient therapy and/or prescribed a home exercise programme in accordance with usual practice at the study sites.
Falls prevention information: received by both groups
All participants will be given a falls prevention brochure33 focusing on safe outdoor mobility. This brochure provides simple tips to assist people to be safe when walking in the community, for example, wearing shoes with slip-resistant soles.
Intervention group: technology-based exercise in addition to usual care
The intervention group will receive tailored technology use in addition to usual care. A detailed intervention protocol has been developed to guide the tailored technology use. The protocol includes tables that direct the choice of technology and exercises/games based on the participant's mobility limitations and technology preferences. The protocol will be reviewed quarterly and any appropriate new technologies and games/exercises will be added throughout the trial. Table 1 shows excerpts from the intervention protocol.
Table 1.
Excerpts from the tables within the intervention protocol of various games/exercises from different technologies recommended for use with different mobility limitations
| Mobility task problem | Easy technology: game or exercise | Medium technology: game or exercise | Hard technology: game or exercise |
|---|---|---|---|
|
Standing Up weight borne principally through intact side |
Humac*: weight-bearing; scale; Fysiogaming†: sit to stand (1–10); Stepping Tiles‡: loading the leg in sitting |
Humac: progress difficulty level and boundaries of movement; Fysiogaming: sit to stand (11–20); Stepping Tiles: sit to stand |
Humac: force vs time; Fysiogaming: sit to stand (21–30); Stepping Tiles: sit to stand |
|
Maintaining a standing position decreased loading of the affected leg |
Humac: weightshift ML; WiiFit§: Penguin slide (modified); T-Rex iPAD APP¶: standing exercises |
Humac: targets, roadway, ski; WiiFit: table tilt, ski slalom, heading, balance bubble |
WiiFit: tightrope, tilt city; Humac: pong ML, breakout ML; Xbox kinect your shape fitness evolve 2012: stack em up |
|
Reaching in standing flexes at hips instead of DF at ankles when reaching forward |
Humac: weightshift AP; Fysiogaming: reaching (1–10); AMOUNT iPAD APP**: reaching in standing program |
Humac: progress difficulty level and boundaries of movement; Xbox kinect††adventures: 20 000 leaks |
Humac: progress difficulty level and boundaries of movement; Fysiogaming: reaching (21–30) |
|
Stepping while standing decreased speed of stepping |
Fysiogaming: walking sideways and walk in place (1–10); Stepping Tiles: stepping exercise (small); Wii Family trainer: sprint challenge |
WiiFit: jogging plus; Xbox kinect adventures: space pop, 20 000 leaks; Stepping Tiles: stepping exercise (large) |
WiiFit: Cycling, step basic; Xbox kinect: river rush, rally ball, reflex ridge; Fysiogaming: walking sideways and walk in place (21–30) |
|
Changing directions while walking shuffling feet to change direction |
Stepping Tiles: stepping grid (small) AMOUNT iPAD APP: changing directions while walking program; Fysiogaming: dynamic balance random (1–10) |
Stepping Tiles: stepping grid (large); Fysiogaming: dynamic balance random (11–20); Xbox kinect: stomp it (modified); Wii Family trainer: mole stomper |
AMOUNT iPAD APP: changing directions while walking program; Fysiogaming: dynamic balance random (level 21–30); Xbox kinect: stomp it |
|
Stair climbing decreased hip and knee extension when ascending stairs |
Stepping Tiles: Stepping up and down on a block; iPAD APP: AMOUNT Climbing stairs program; Fitbit‡‡: floors climbed |
WiiFit: step basic (modified) Fitbit: floors climbed Stepping Tiles: as for easy but increase height of block |
WiiFit: step basic Fitbit: floors climbed iPAD APP: AMOUNT Climbing stairs program |
|
Physical activity throughout the day prolonged periods of sitting |
Any technology used in standing | Any technology used in standing; Activity Monitors: Fitbit one/zip, Garmin vivofit§§; AMOUNT iPAD APP: Physical activity throughout the day program |
Any technology used in standing; Activity Monitor: Fitbit one/zip, Garmin vivofit; Smartphone APPs: Runkeeper¶¶ |
*Humac balance system, CSMi Solutions, Stoughton, Massachusetts, USA.
†Fysiogaming, Doctor Kinetic, Amsterdam, the Netherlands.
‡Stepping Tiles, University of Technology Sydney, Sydney, Australia.34
§Nintendo WiiFit, Nintendo, Kyoto, Japan.
¶T-Rex iPAD APP, Repatriation General Hospital, Adelaide, Sydney, Australia.
**AMOUNT iPAD APP The George Institute for Global Health, Sydney, Australia.
††Xbox Kinect, Microsoft Redmond Campus, Redmond, Washington, USA.
‡‡Fitbit, Fitbit Inc, San Francisco, California, USA.
§§Garmin Ltd, Olathe, Kansas, USA.
¶¶Runkeeper, FitnessKeeper, Boston, Massachusetts, USA.
AP, anteroposterior; DF, Dorsiflexion; ML, mediolateral.
Research physiotherapists will be employed at each site to deliver the trial intervention and will be trained in all facets of the trial. The research physiotherapist will determine the most appropriate intervention for each participant based on the intervention protocol and taking into account current impairments and mobility limitations, participant goals, technology experience and preferences and anticipated length of stay as determined from a review of the clinical notes and/or discussion with the participant's usual hospital physiotherapist. Each participant will be asked to use the intervention technologies between 30 and 60 min daily for five or more days per week, supervised and unsupervised (if deemed safe to do so) in addition to usual care. The total duration of the intervention will be 6 months after randomisation and will incorporate inpatient rehabilitation and post-discharge settings. Figure 2 provides a flow diagram of the experimental intervention delivery.
Figure 2.
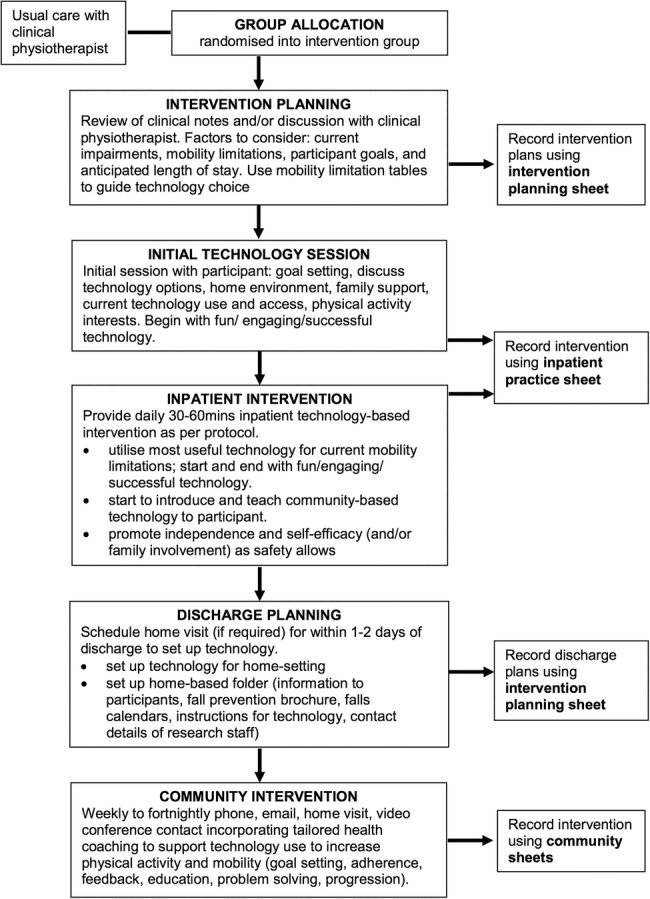
Flow of delivery of experimental intervention.
The prescription of technology to target mobility and physical activity problems will include, but will not be limited to, the use of video and computer games and tablet applications to encourage structured exercise and other forms of physical activity as well as activity monitors to provide feedback on physical activity levels. The chosen technologies include recreational commercially available devices (eg, Fitbit, Fitbit Inc, San Francisco, California, USA) and rehabilitation-specific devices (eg, Humac balance system, CSMi Solutions, Stoughton, Massachusetts, USA). All technologies are relatively low cost (ranging from no cost (Runkeeper app) to A$4000 (Stepping Tiles)), provide feedback on mobility task or physical activity performance or dose, and facilitate individualised tailoring and progression of exercise or physical activity. The technologies were identified through knowledge and previous use by the investigators26 and internet and literature searches of technologies being used and developed for rehabilitation. In addition, technologies were developed by the research team specifically for the trial. Technologies identified were trialled and tested by experienced rehabilitation physiotherapists (LH, KS and DT) and by our consumer representative (RP) who provided feedback on the usability, feedback and enjoyment of the technologies.
While in hospital, the research physiotherapist will initially provide one-on-one supervision to ensure safety and to help participants learn to use the technologies outside of therapy times. Participants will be encouraged to exercise with family/friends or alone, if and when they are judged safe to do so; however, the research physiotherapist will still monitor the sessions to ensure that the prescribed dose is delivered. The amount of assistance required and the time taken to learn to independently use the different technologies will be recorded by the research physiotherapist.
After discharge from the inpatient stay, participants will be encouraged to continue using the technologies at home. Participants will be loaned necessary equipment (stand-alone devices or game consoles, which will be installed by study staff) and trained in the safe use and progression of the games/exercises during a home visit by the research physiotherapist. Support will be provided by the research physiotherapist every 1–2 weeks using a tailored health coaching approach via telephone, email, home visit or videoconference. This support will aim to assist study participants to maintain motivation to continue to use the technologies to improve mobility and physical activity, to identify and address any barriers to technology use at home and to identify the need to modify the program/technology to make it more or less challenging.
Goals will be set collaboratively with each participant and will be recorded and reviewed throughout the intervention phase. Practice recording sheets and information from some of the devices (eg, game play time, number of steps walked) will be used to monitor the dose of the intervention. Intervention fidelity will be monitored via random audits of data forms and observation of intervention sessions by the trial manager. Regular team meetings will be conducted to discuss intervention delivery and the results of fidelity checking.
Outcome measures
The coprimary outcomes will be physical activity (proportion of the day spent upright) and mobility (SPPB) 6 months after randomisation. Secondary outcomes will be physical activity and mobility (3 weeks after randomisation), cognition (3 weeks and 6 months after randomisation), self-reported physical activity, activity performance and participation, utility-based quality of life, balance confidence, technology self-efficacy (3 and 12 weeks and 6 months after randomisation), falls and service utilisation in the 6 months after randomisation. In addition, self-reported measures of technology usability and enjoyment will be obtained from the intervention group (3 and 12 weeks and 6 months after randomisation). All outcomes (excluding activity performance and participation and self-reported physical activity) as well as demographic information such as age and sex, diagnosis, existence of comorbidities (Functional Comorbidity Index)35 and cognitive status (MMSE)32 will be assessed at baseline (prior to randomisation) to enable a description of the sample's baseline characteristics and to obtain values to enter as covariates in the models comparing groups at follow-up.
All outcomes will be assessed by a research staff member who will be trained in the conduct of the outcome assessment and who is unaware of group allocation. Prior to the follow-up assessments, participants will be instructed not to inform the assessor of their group assignment. Follow-up assessments at 3 weeks and 6 months will be conducted in the hospital or in participants' homes where necessary and will involve performance-based tests and questionnaires. Follow-up assessments at 12 weeks will be conducted by mail or phone and will involve questionnaires only. If an assessor becomes unblinded during the 3-week or 12-week assessment, every effort will be made to use a different blinded assessor for the remaining assessments. Regardless of adherence to the intervention protocol, every effort will be made to collect outcome data at all time periods for all participants, unless the participant wishes to withdraw from the study.
Coprimary outcomes
Physical activity has been operationalised as the proportion of the day spent upright. It will be assessed over a 7-day period using the activPAL activity monitor (PAL Technologies Ltd, Glasgow, UK) at baseline (24-hour monitoring), and at 3 weeks and 6 months postrandomisation. The activPAL is a small lightweight sensor attached to the thigh with thin transparent wound dressing material. This device has been used extensively in rehabilitation settings and accurately measures sitting time,36 walking37 and total upright time.38 Using proprietary algorithms, the activPAL classifies an individual’s activity into periods spent sitting, standing and walking. The proportion of the day spent upright at 6 months will be the primary outcome (and the 3-week measure a secondary outcome).
Mobility will be measured using the continuously scored version39 (0–3) of the SPPB.31 The SPPB is a composite performance-based measure of gait, sit-to-stand and standing balance which predicts institutionalisation and death.31 40 It involves measurement of time taken to stand up from a chair five times, time taken to walk 4 m and timed ability to stand unsupported with the feet in three different positions of increasing difficulty (feet together, semitandem and tandem). The 6-month continuously scored SPPB will be the primary outcome measure (and the 3-week data and the total score (0–12) and subscale scores (0–4) as secondary measures).
Secondary outcomes
Self-reported physical activity will be measured with the Incidental and Planned Exercise Questionnaire (IPEQ).41 The IPEQ covers the frequency and duration of planned and incidental physical activity in older people and has excellent psychometric properties to assess physical activity relating to both basic and more demanding activities.
The de Morton Mobility Index (DEMMI)42 will be used as a secondary measure of ‘mobility’. The DEMMI is a 15-item hierarchical measure that covers the mobility spectrum from bed mobility to high-level independent mobility and has been shown to accurately measure and monitor the mobility of older adults across acute, subacute and community settings.42–44 In addition, mobility will also be measured using a timed single leg stance (maximum 30 s), Maximal Balance Range Test45 and Step Test.46
Self-reported activity performance and participation will be measured using the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0).47 The WHODAS 2.0 is a brief 12-item summed self-report measure of activity performance and participation in the prior month covering the six domains of (1) Understanding and communication; (2) Self-care; (3) Mobility (getting around); (4) Interpersonal relationships (getting along with others); (5) Work and household roles (life activities); and (6) Community and civic roles (participation). The WHODAS 2.0 has high internal consistency and test–retest reliability and good concurrent validity with other measures of disability.47 48 In addition, confidence in performing various ambulatory activities without falling or experiencing a sense of unsteadiness will be measured with the Activities-Specific Balance Confidence Scale.49
Cognition: will be assessed using the Trail Making Test (TMT) parts A and B.50 51 This test provides information on scanning, visual search, speed of processing, mental flexibility and executive function.51 TMT part A involves participants drawing to connect 25 consecutive numbers (eg, 1-2-3) and part B involves participants drawing to connect alternating letters and numbers (eg, 1-A-2-B). The difference in time taken to complete each part (B minus A) will be calculated to isolate the executive functioning component of this test.
Utility-based quality of life: will be assessed using the Short Form 6-dimensions questionnaire (SF-6D) calculated from the SF-3652 and the EuroQol 5-dimensions (EQ5D-5L).53 Both of these measures provide a single index value for health and enable determination of quality adjusted life years (QALYs) for use in cost utility analysis.
Falls and health and community service usage: will be assessed over the 6-month period after randomisation. Data will be collected during the inpatient stay using study site incident documentation systems and hospital databases. After discharge, participants will be asked to complete monthly calendars for the remainder of the trial documenting any falls and service usage. Recorded falls will be followed up by a phone call from a blinded assessor to document information about the fall (eg, location, time). Data will be obtained by phone from participants who are unable or unwilling to complete a calendar.
Technology self-efficacy: will be measured using the Modified Computer Self Efficacy Scale.54 Exposure to common technologies (eg, smartphone, computer) in the month prior to hospitalisation and during their inpatient and community components of the trial will be measured using a purposely designed questionnaire. For participants in the intervention group, we will also assess their impression of the ‘usability’ and ‘enjoyment’ of different technologies using the System Usability Scale55 56 and Physical Activity Enjoyment Scale.57 In addition, adherence to the intervention will be calculated using records kept by staff, usage diaries kept by participants and data available from the devices themselves.
Adverse events (minor and serious) will be monitored throughout the trial and any adverse events will be reported to the trial Data Monitoring Committee, which is independent from the Investigator team and has no competing interests. For this trial, an adverse event is defined as an unwanted and usually harmful outcome (eg, fall, seizure, cardiac event). The event may or may not be related to the intervention, but it occurs while the person is participating in the intervention, that is, while they are undertaking mobility or physical activities using technology.
Data analysis and management
Sample size
A total of 300 participants (150 per group) will provide 90% power to detect as significant, at the 5% level, a 15% between-group difference in the coprimary outcome measures. The sample size calculation was undertaken using the sampsi command in Stata V.13 using data from our pilot study26 and unpublished data from a previous study in inpatient rehabilitation.58 The calculation assumed one pre-randomisation measure, one follow-up measure, analysis using linear models with baseline scores entered as covariates and a correlation between premeasures and postmeasures of 0.65. For the continuously scored SPPB score, the intervention group mean was assumed to be 1.89, the control group mean 1.64 and the SD 0.75. For the activPAL, the intervention group upright minutes per day was assumed to be 223, the control group mean 194 and the SD 90. We have conservatively allowed for a 20% dropout rate. This sample size will also be sufficient to detect between-group differences of 10–15% in most of the secondary outcomes.
Data management
All primary and secondary outcome data will initially be collected on paper data forms (and stored securely) and then entered into the secure online REDCap database. User roles and Data Access Groups have been created in REDCap to ensure that staff who are conducting outcome assessments remain blinded to group allocation when entering data into the database. Where feasible, data fields within REDCap have criteria assigned (eg, set range of values) as a double check that valid data are entered into each data field. In addition, 10% of the data entered will be double-checked as part of the data cleaning process.
Analysis of outcomes
Between-group comparisons for each of the continuously scored outcome measures will be made using linear models with baseline scores entered as a covariate. The dichotomous outcomes will be compared between groups using log binomial regression. Fall rates between groups will be compared using negative binomial regression. Interaction terms will be used in the models to assess whether effects of the intervention differed according to age or a neurological versus non-neurological cause of the mobility limitation. Primary analyses will be preplanned, conducted while masked to group allocation and use an intention-to-treat approach. All analyses will be overseen by the study statistician (SH).
Health and community service usage data collected from participant-completed calendars, hospital databases and medical records (length of stay, procedures, reasons for readmission or emergency department visit) will be used to calculate health service utilisation and costs to inform the conduct of an economic evaluation. The cost of the intervention (staff and equipment) will also be calculated from trial records and used in the cost-effectiveness analysis. The Incremental Cost-Effectiveness Ratio will be calculated to assess the relative costs and benefits in terms of gain in mobility (SPPB score change) and quality of life (using the SF-6D and the EQ5D-5L).
Ethics and dissemination
The results of this trial will be disseminated via presentations at local, national and international conferences, peer-reviewed journals and via Investigator institutional websites and media departments.
Discussion
The pragmatic trial design has the advantage that we are testing this intervention in the real world and as such, if found effective, is ready to be implemented in clinical practice. However, the potential limitations of the study include the individualised tailoring of the intervention, the risk of contamination with control and intervention participants on the same wards and the reliance on participant self-report of dosage for the community component of the intervention. These potential limitations will be addressed by a detailed intervention protocol to guide delivery of the intervention, trial technologies only accessible to research staff on the wards and the addition of dosage data from some technologies (eg, step count from the Fitbit; game play time from the Nintendo Wii) to support the self-report data.
This study will be the first trial of tailored exercise using affordable technology integrated with usual rehabilitation care to be adequately powered to detect effects on important mobility outcomes. The significance of this study is in the potential for widespread tailored use of these technologies in rehabilitation to increase the dose of repetitive exercise without dramatic increases in staff costs and thus enhance outcomes in a cost-effective manner. Technologies to enable ongoing exercise are likely to become increasingly important in the future as the proportion of older people in the population increases and resources to provide rehabilitation care become more limited.
Acknowledgments
The authors are grateful to the study participants, hospital staff and study staff (Ashley Rabie, Elizabeth Lynch, Catherine Kirkham, Areti Dakopoulos, Melani Boyce, Frances Moran, Janine Prestes Vargas, Linda Roylance, Tarcisio Campos Folly, Hannah Kastrappi, Heather Paul, Caroline Hafner, Janette Hall, Anna Miles and Abby Schmidt) as well as to Anna Wollstein for study site assistance.
Footnotes
Contributors: CS with input from the other investigators conceived this study. CS, RIL, MC, AMc, HPvdP, STS, KS, MK, BB, KH, SH, LT, DT, SD, SW and RP received funding to conduct this study. LH, KS, DT and RP trialled and tested the technologies with input from all investigators and the research team. LH and MvdB developed the protocol and study materials with input from all investigators. CS, LH, SH and KH will conduct the analyses. All authors approved the final manuscript.
Funding: This work is supported by an Australian National Health and Medical Research Council Project Grant (APP1063751). CS receives salary funding from an Australian National Health and Medical Research Council Fellowship.
Competing interests: None declared.
Ethics approval: Southern Adelaide Clinical Human Research Ethics Committee, Adelaide, Australia (study number 529.13) and the South Western Sydney Local Health District Human Research Ethics Committee, Sydney, Australia (reference number HREC/13/SAC/359).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.AIHW. Australia's Health 2012. Canberra: Australian Institute of Health and Welfare, 2012. [Google Scholar]
- 2.American College of Sports Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009;41:1510–30. 10.1249/MSS.0b013e3181a0c95c [DOI] [PubMed] [Google Scholar]
- 3.Handoll HH, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. [update of Cochrane Database Syst Rev 2004;(4):CD001704; PMID: 15495015]. Cochrane Database Syst Rev 2007;(1):CD001704. [DOI] [PubMed] [Google Scholar]
- 4.Counsell SR, Holder CM, Liebenauer LL et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc 2000;48:1572–81. 10.1111/j.1532-5415.2000.tb03866.x [DOI] [PubMed] [Google Scholar]
- 5.van Peppen RP, Hendriks HJ, van Meeteren NL et al. The development of a clinical practice stroke guideline for physiotherapists in The Netherlands: a systematic review of available evidence. Disabil Rehabil 2007;29:767–83. 10.1080/09638280600919764 [DOI] [PubMed] [Google Scholar]
- 6.Carr J, Shepherd R. Neurological rehabilitation: optimizing motor performance. Oxford: Butterworth-Heinemann, 1998. [Google Scholar]
- 7.Blennerhassett J, Dite W. Additional task-related practice improves mobility and upper limb function early after stroke: a randomised controlled trial. Aust J Physiother 2004;50:219–24. 10.1016/S0004-9514(14)60111-2 [DOI] [PubMed] [Google Scholar]
- 8.Kwakkel G. Impact of intensity of practice after stroke: issues for consideration. Disabil Rehabil 2006;28:823–30. 10.1080/09638280500534861 [DOI] [PubMed] [Google Scholar]
- 9.Wevers L, van de Port I, Vermue M et al. Effects of task-oriented circuit class training on walking competency after stroke: a systematic review. Stroke 2009;40:2450–9. 10.1161/STROKEAHA.108.541946 [DOI] [PubMed] [Google Scholar]
- 10.Kwakkel G, van Peppen R, Wagenaar RC et al. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke 2004;35:2529–39. 10.1161/01.STR.0000143153.76460.7d [DOI] [PubMed] [Google Scholar]
- 11.Veerbeek JM, van Wegen E, van Peppen R et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014;9:e87987 10.1371/journal.pone.0087987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sherrington C, Whitney JC, Lord SR et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008;56:2234–43. 10.1111/j.1532-5415.2008.02014.x [DOI] [PubMed] [Google Scholar]
- 13.West T, Bernhardt J. Physical activity in hospitalised stroke patients. Stroke Res Treat 2012;2012:813765 10.1155/2012/813765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith P, Galea M, Woodward M et al. Physical activity by elderly patients undergoing inpatient rehabilitation is low: an observational study. Aust J Physiother 2008;54:209–13. 10.1016/S0004-9514(08)70028-X [DOI] [PubMed] [Google Scholar]
- 15.Annesi JJ, Mazas J. Effects of virtual reality-enhanced exercise equipment on adherence and exercise-induced feeling states. Percept Mot Skills 1997;85Pt 1):835–44. 10.2466/pms.1997.85.3.835 [DOI] [PubMed] [Google Scholar]
- 16.Lewis GN, Rosie JA. Virtual reality games for movement rehabilitation in neurological conditions: how do we meet the needs and expectations of the users? Disabil Rehabil 2012;34:1880–6. 10.3109/09638288.2012.670036 [DOI] [PubMed] [Google Scholar]
- 17.Betker AL, Desai A, Nett C et al. Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuries. Phys Ther 2007;87:1389–98. 10.2522/ptj.20060229 [DOI] [PubMed] [Google Scholar]
- 18.Betker AL, Szturm T, Moussavi ZK et al. Video game-based exercises for balance rehabilitation: a single-subject design. Arch Phys Med Rehabil 2006;87:1141–9. 10.1016/j.apmr.2006.04.010 [DOI] [PubMed] [Google Scholar]
- 19.Lange B, Flynn S, Proffitt R et al. Development of an interactive game-based rehabilitation tool for dynamic balance training. Top Stroke Rehabil 2010;17:345–52. 10.1310/tsr1705-345 [DOI] [PubMed] [Google Scholar]
- 20.Rosenberg D, Depp CA, Vahia IV et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry 2010;18:221–6. 10.1097/JGP.0b013e3181c534b5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsu JK, Thibodeau R, Wong SJ et al. A “Wii” bit of fun: the effects of adding Nintendo Wii([REGISTERED]) Bowling to a standard exercise regimen for residents of long-term care with upper extremity dysfunction. Physiother Theory Pract 2011;27:185–93. 10.3109/09593985.2010.483267 [DOI] [PubMed] [Google Scholar]
- 22.Miller KJ, Adair BS, Pearce AJ et al. Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: a systematic review. Age Ageing 2014;43:188–95. 10.1093/ageing/aft194 [DOI] [PubMed] [Google Scholar]
- 23.Booth V, Masud T, Connell L et al. The effectiveness of virtual reality interventions in improving balance in adults with impaired balance compared with standard or no treatment: a systematic review and meta-analysis. Clin Rehabil 2014;28:419–31. 10.1177/0269215513509389 [DOI] [PubMed] [Google Scholar]
- 24.Laver KE, George S, Thomas S et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2015;2:CD008349 10.1002/14651858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: a systematic review. J Physiother 2015;61:117–24. 10.1016/j.jphys.2015.05.017 [DOI] [PubMed] [Google Scholar]
- 26.van den Berg M, Sherrington C, Killington M et al. Video and computer-based interactive exercises are safe and improve task-specific balance in geriatric and neurological rehabilitation: a randomised trial. J Physiother 2016;62:20–8. 10.1016/j.jphys.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 27.Boutron I, Moher D, Altman DG et al. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008;148: 295–309. 10.7326/0003-4819-148-4-200802190-00008 [DOI] [PubMed] [Google Scholar]
- 28.Zwarenstein M, Treweek S, Gagnier JJ et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ 2008;337:a2390 10.1136/bmj.a2390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan AW, Tetzlaff JM, Altman DG et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoffmann TC, Glasziou PP, Boutron I et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 31.Guralnik JM, Simonsick EM, Ferrucci L et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–94. 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 32.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 33.Clinical Excellence Commission New South Wales Health, Falls Prevention—in public places Version 1, SHPN: (CEC) 120266. 2012. www.cec.health.nsw.gov.au/_data/assets/pdf_file/0007/258541/10-falls-prevention-in-public-places.pdf (accessed 1 Jul 2014).
- 34.Bongers B, Smith S, Donker V et al. Interactive rehabilitation tiles. Work in progress paper and demo. International Conference on Tangible, Embedded and Embodied Interaction; Munich, Germany, 2014. [Google Scholar]
- 35.Groll DL, To T, Bombardier C et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005;58:595–602. 10.1016/j.jclinepi.2004.10.018 [DOI] [PubMed] [Google Scholar]
- 36.Kozey-Keadle S, Libertine A, Lyden K et al. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc 2011;43:1561–7. 10.1249/MSS.0b013e31820ce174 [DOI] [PubMed] [Google Scholar]
- 37.Ryan CG, Grant PM, Tigbe WW et al. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med 2006;40:779–84. 10.1136/bjsm.2006.027276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grant PM, Ryan CG, Tigbe WW et al. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med 2006;40:992–7. 10.1136/bjsm.2006.030262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Onder G, Penninx BW, Lapuerta P et al. Change in physical performance over time in older women: the Women's Health and Aging Study. J Gerontol A Biol Sci Med Sci 2002;57:M289–93. 10.1093/gerona/57.5.M289 [DOI] [PubMed] [Google Scholar]
- 40.Guralnik JM, Ferrucci L, Pieper CF et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000;55:M221–31. 10.1093/gerona/55.4.M221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Delbaere K, Hauer K, Lord SR. Evaluation of the incidental and planned activity questionnaire (IPEQ) for older people. Br J Sports Med 2010;44:1029–34. 10.1136/bjsm.2009.060350 [DOI] [PubMed] [Google Scholar]
- 42.de Morton NA, Davidson M, Keating JL. The de Morton Mobility Index (DEMMI): an essential health index for an ageing world. Health Qual Life Outcomes 2008;6:63 10.1186/1477-7525-6-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davenport SJ, de Morton NA. Clinimetric properties of the de Morton Mobility Index in healthy, community-dwelling older adults. Arch Phys Med Rehabil 2011;92:51–8. 10.1016/j.apmr.2010.08.023 [DOI] [PubMed] [Google Scholar]
- 44.de Morton NA, Brusco NK, Wood L et al. The de Morton Mobility Index (DEMMI) provides a valid method for measuring and monitoring the mobility of patients making the transition from hospital to the community: an observational study. J Physiother 2011;57:109–16. 10.1016/S1836-9553(11)70021-2 [DOI] [PubMed] [Google Scholar]
- 45.Lord SR, Ward JA, Williams P. Exercise effect on dynamic stability in older women: a randomized controlled trial. Arch Phys Med Rehabil 1996;77:232–6. 10.1016/S0003-9993(96)90103-3 [DOI] [PubMed] [Google Scholar]
- 46.Hill KD. A new test of dynamic standing balance for stroke patients: reliability, validity and comparison with healthy elderly. Physiother Canada 1996;48:257–62. 10.3138/ptc.48.4.257 [DOI] [Google Scholar]
- 47.Rehm J, Üstün TB, Saxena S et al. On the development and psychometric testing of the WHO screening instrument to assess disablement in the general population. Int J Methods Psychiatr Res 1999;8:110–22. 10.1002/mpr.61 [DOI] [Google Scholar]
- 48.Andrews G, Kemp A, Sunderland M et al. Normative data for the 12 item WHO Disability Assessment Schedule 2.0. PLoS ONE 2009;4:e8343 10.1371/journal.pone.0008343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 1995;50A:M28–34. 10.1093/gerona/50A.1.M28 [DOI] [PubMed] [Google Scholar]
- 50.War Department, Adjutant General's Office. Army Individual Test Battery. Manual for directions and scoring. Washington, DC: War Department Adjutant, General's Office, 1944. [Google Scholar]
- 51.Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol 2004;19:203–14. 10.1016/S0887-6177(03)00039-8 [DOI] [PubMed] [Google Scholar]
- 52.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271–92. 10.1016/S0167-6296(01)00130-8 [DOI] [PubMed] [Google Scholar]
- 53.Herdman M, Gudex C, Lloyd A et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Laver K, George S, Ratcliffe J et al. Measuring technology self efficacy: reliability and construct validity of a modified computer self efficacy scale in a clinical rehabilitation setting. Disabil Rehabil 2012;34:220–7. 10.3109/09638288.2011.593682 [DOI] [PubMed] [Google Scholar]
- 55.Brooke J. SUS: a “quick and dirty” usability scale. In: Jordan PW, Thomas B, Weerdmeester BA et al., eds Usability evaluation in industry. London: Taylor & Francis, 1996:189–94. [Google Scholar]
- 56.Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Hum Comput Interact 2008;24:574–94. 10.1080/10447310802205776 [DOI] [Google Scholar]
- 57.Kendzierski D, DeCarlo KJ. Physical activity enjoyment scale: two validation studies. J Sport Exerc Psychol 1991;13:50–64. [Google Scholar]
- 58.Sherrington C, Lord SR, Close JC et al. Development of a tool for prediction of falls in rehabilitation settings (Predict_FIRST): a prospective cohort study. J Rehabil Med 2010;42:482–8. 10.2340/16501977-0550 [DOI] [PubMed] [Google Scholar]


