Abstract
Introduction: The aim of this study was to compare the antibacterial efficacy of diode laser 810nm and photodynamic therapy (PDT) in reducing bacterial microflora in endodontic retreatment of teeth with periradicular lesion.
Methods: In this in vivo clinical trial, 20 patients who needed endodontic retreatment were selected. After conventional chemo mechanical preparation of root canals, microbiological samples were taken with sterile paper point (PP), held in thioglycollate broth, and then were transferred to the microbiological lab. In the first group, PDT with methylene blue (MB) and diode laser (810 nm, 0.2 W, 40 seconds) was performed and in the second group diode laser (810 nm, 1.2 W, 30 seconds) was irradiated. Then second samples were taken from all canals.
Results: CFU/ml amounts showed statistically significant reduction in both groups (P < 0.001). CFU/ml amounts were compared between the two groups and there was no statistical difference.
Conclusion: PDT and diode laser 810 nm irradiation are effective methods for root canal disinfection. PDT is a suitable alternative for diode laser 810 nm irradiation, because of lower thermal risk on root dentin.
Keywords: Endodontic, Diode laser, PDT
Introduction
Microbial infection plays an important role in persistent periapical lesions.1 Insufficient disinfection of root canals could lead to treatment failure and persistent periapical pathology.2
Conventional techniques of root canal treatments such as mechanical instrumentation and chemical debridement with antimicrobial irrigants, such as sodium hypochlorite (NaOCl), chlorhexidine and calcium hydroxide do not always suffice to predictably render root canals free of bacteria.3,4 Factors such as anatomical complexities, bacterial growth as biofilm, render complete disinfection of the root canal system almost impossible.5
Studies have revealed a success rate of 94% with a negative culture before obturation has decreased to 68%, with a positive culture.2 Resolution of periapical lesions is more achievable when there is negative culture before obturation.6
Cross sectional studies have reported 20%-60% of treatment failure and 52% of endodontic failure in Iranian population.7-10 Existence of intracanal microorganisms would lessen the treatment outcomes of endodontic re-treatment comparing to primary endodontic treatment.2
Based on the previous studies, bacterial microflora in teeth with failed endodontic treatment is different from the microflora of the primary endodontic infection. All culture and PCR based methods have shown that primary endodontic infection is a polymicrobial infection involving fully anaerobic microorganisms,5,11 while the failure of the endodontic treatment is often associated with the facultative gram positive microorganisms.12 There are numerous reports on the presence of Enterococcus faecalis in failed endodontic treatments.2,13
The prognosis of the endodontic retreatment is significantly lower than the endodontic initial therapy due to more resistant microorganisms. Various adjuvant techniques have been used to overcome the problem.14
Several studies have shown that oral bacteria are sensitive to photodynamic therapy (PDT).15,16 In recent years, in vitro17-26 and in vivo27-29 studies have been performed to investigate the antibacterial effect of the PDT on the microorganisms in root canal. Most of these studies have focused on the PDT capability as a complementary technique besides the conventional endodontic treatment.
Using the high-power diode laser is a new approach of disinfection allowing access to the previously unavailable areas, such as the tubular network. The high-power laser achieves this through higher penetrating levels into dental tissue compared to rinsing solutions.30 This study, therefore, compares two types of diode lasers (low-power and high power) in terms of anti-bacterial effect as well as the conventional endodontic retreatment to determine the ideal method of root canal disinfection.
Methods
Subjects were selected among the patients admitted to the Endodontic Department, Shahid Beheshti School of Dentistry, requiring endodontic retreatment. The protocol was approved and registered in the U.S. National Institute of clinical trials (NCT02555488). Twenty healthy patients who had periradicular lesions in radiographic assessment (which had not disappeared after two years of primary endodontic treatment) were chosen by convenience sampling method. Teeth with failures such as fractured instrument, resorption, perforation, ledge, over fillings and transportation were not included in the study. Informed consents were obtained from the patients. After assurance about the previous treatment performed and the presence of radiolucent periradicular lesion detectable by primary radiography, patients underwent root canal retreatment. The treatment procedure included:
Access to the root canals after placing the rubber dam. In order to ensure the minimum contamination, the crown and surrounding areas were washed by 2.5% hypochlorite sodium.
After complete removal of restorative material, gutta percha of the coronal area was removed by the Gates Glidden drills No. 2 & 3 (Dentsply, Maillefer, Switzerland). Then, gutta percha was emitted using H- file (MANI, Japan) and chloroform solvent.
Working length was determined by two radiographies from different angles and the apex finder device (Rapex 5, VDW, Germany). Then, the root canal system was prepared using crown down technique with hand and rotary files up to file No. 30, convergence of 4% and frequent washing with 5 mL of 2.5% NaOCl solution for 5 minutes in the canal. Finally, the root canal was dried by three sterile paper point (PP) (Ariadent, Iran) No. 30, convergence of 2%. The paper points were then transferred to the microbiology laboratory in the thioglycollate solution (Merck, Germany).
In the next stage, the canal was filled by 0.5 mL of 0.01% methylene blue (MB) solution for 5 minutes. This photosensitizer solution was randomly used in half the samples. They were then radiated by laser in the photodynamic process.
The canal was irradiated by the light supply of diode laser Dr. Smile (Lambda Scientifica, Italy) with a wavelength of 810 nm for 40 seconds (0.2 W). Laser beam was directed into the canal by the fiber optic cone with a diameter of 200 μm. The tip of the fiber optic cone was placed at a working length of 1mm and removed at a speed of 2 mm/s with helicoidal motion towards the orifice. After radiation for 10 seconds, the tissues relaxed for 10 seconds.
Finally, after washing the MB solution from inside the canal with normal saline, the final microbiological sample was obtained by three sterile paper points of No. 30 with convergence of 2% reaching the working length. The sample was transferred to the microbiology laboratory in thioglycollate containing tubes.
The Light Supply of High Power Diode Laser
The canals prepared with the conventional endodontic technique were ready for high power diode laser radiation. In order to prevent the surface absorption of the laser energy by water, canals were dried. Afterwards, the canals were irradiated by the diode laser beam Dr. Smile (Lambda Scientifica, Italy) with a wavelength of 810 nm for 30 seconds (0.2 W) by a fiber optic cone with a diameter of 300 μm. The tip of the fiber optic cone was placed at a working length of 1 mm and removed in the speed of 2 mm/s with helicoidal motion towards the orifice. The tissues relaxed for 10 seconds between the motions.
Three sterile PPs No.30 were placed for 1 minute in the working length and final microbiological samples were derived. Before sampling, the canals were doused by 0.5 mL of saline solution. PP were kept in thioglycollate and sent to the microbiology laboratory.
Then, the canals were filled by calcium hydroxide mix with a creamy consistency and the access cavity was temporarily restored by Coltosol (Ariadent, Iran) with a minimum thickness of 4 mm. After 7 days, in the second visit, obturation of root canals was performed by gutta percha (Ariadent, Iran) and AH26 sealer (Dentsply, Maillefer) through cold lateral compaction method and the access cavity was sealed by temporary restorative material. In order to continue the treatment, patients were referred to the prosthesis departments (Figure 1).
Figure 1 .
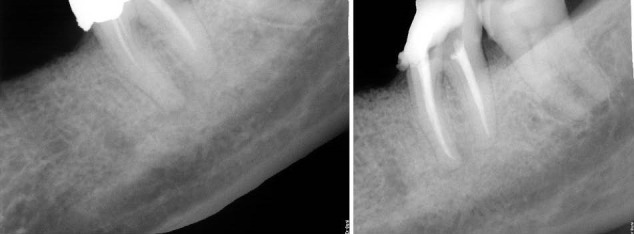
Radiographic Image Before and After Retreatment.
Mediums Used in This Study
Before and after the treatment, sampling on 20 patients was conducted using sterile paper points. PPs were transferred into tubes containing thioglycollate transfer medium. The tubes were immediately sent to the microbiology laboratory, in order to be incubated for 24 hours at 37˚C. For colony forming unit examination, the bacteria were cultured from the broth to the bacteria specific medium using the spread technique: firstly, 9 mL saline containing tubes (concentration of 5.8%) were prepared. Bacteria specific mediums were prepared based on the number of the dilution series. After 24 hours in incubator, 1 mL of each tube was transferred to the saline tube and between the tubes respectively to the last dilution (1 m was discarded of the last tube). After vortexing the tubes, 1 mL of each tube was transferred to the bacteria specific agar containing mediums. The solutions were transferred by L-shaped bar and cultured using the spread technique (this technique spreads the bacteria in the medium and creates single colonies). After 24 hours of incubation (7- 10 days for anaerobic bacteria), colonies were counted. The plates with colony numbers ˂20 and ˃200 were excluded. The result was multiplied by the reversed dilution coefficient and the result was reported as CFU /ml.
Bacterial mediums used included blood agar for streptococci isolation; Mitis salivarius agar Enterococcus faecalis isolation; crystal-violet erythromycin agar (CVE-agar) to isolate Fusobacterium nucleatum; LKV agar for Prevotella isolation and blood agar (containing horse blood) to isolate the Porphyromonas gingivalis. After culture, mediums specific to the anaerobic bacteria were immediately placed in the anaerobic jars with a gas pack soaked in 35 mL of water and incubated for 7-10 days at 37°C. In order to prepare the mediums, 0.5 g of the powder was dissolved in 10 mL of normal sodium hydroxide. By adding 100 mL of distilled water, its volume reached 100 mL and was sterilized for 15 minutes at 121°C autoclave. 1 mL of the mix is sufficient to prepare 1 L of anaerobic bacteria medium. 0.1 g of the commercial ampoule of vitamin K (1 mg/mL) can be used in 1 L of the growth medium for anaerobic bacteria. After the medium cooled (autoclave sterilization), the vitamin and the material were added to it.
Data Analysis Method
Due to the scattered data and abnormal distribution of the variable CFU/ml, median, minimum and maximum were used to compare the CFU/ml values before and after the intervention.
In order to compare the median differences of the variable before and after the intervention, the Wilcoxon one sample test was used. Mann-Whitney test was applied to compare the two interventions (PDT and 810 nm diode laser).
Furthermore, considering the CFU differences before the intervention as well as different microorganism species, comparison of the CFU values of two interventions was performed using the multivariable regression. Data analysis was carried out by SPSS 18.0.
Results
The results of data analysis showed that the values of CFU/ml were significantly reduced in the sample group undergoing the PDT process (P ˂ 0.001; Table 1). Thus, PDT leads to a significant reduction in CFU/ml values in the root canal.
Table 1 . Comparison of CFU/ml Values Before and After the Interventions in Both Groups .
| Index | Intervention | |||
| Before Intervention | Before Intervention | After Intervention | After Intervention | |
| CFU/ml in the group under PDT | CFU/ml in the group under 810 nm diode laser | CFU/ml in the group under PDT | CFU/ml in the group under 810 nm diode laser | |
| Median | 1.5 × 104 | 7.8 × 102 | 0 | 0 |
| Min | 0 | 0 | 0 | 0 |
| Max | 4.4 × 109 | 9.8 × 108 | 3.8 ×105 | 4.6 ×106 |
Abbreviations: PDT, photodynamic therapy.
In addition, the values of CFU /ml in the root canal were significantly reduced after radiation of the 810 nm diode laser. The reduction was significant based on the Wilcoxon one sample statistical analysis (signed-rank test). Table 1 shows comparison of CFU/ml values before and after the intervention in the group of PDT and diode laser.
In order to compare the CFU/ml values between the two groups, Mann-Whitney test was used, which showed no significant difference.
Furthermore, considering the differences of CFU at baseline as well as the different microorganism species, to compare the CFU/ml values of two interventions, the multivariable regression was performed. Given all the above items, no significant difference was observed between the intervention groups in terms of reduction in CFU values.
Considering the difference of the CFU/ml at baseline, CFU/ml values were compared between the two groups. There were only two cases with statistically significant differences which included: Streptococcus species and F. nucleatum.
(a) The two groups had statistically significant differences in CFU at baseline for the Streptococcus species (standardized coefficients beta=-0.52).
When this difference increases by 1 unit, the consequent CFU will be reduced by 0.5 unit. This means that the more the difference of the CFU base line between the two groups, the more consequent CFU outcome will be reduced. In other words, the difference of the CFU baseline leads in an over estimated intervention effect.
(b) The two groups showed statistically significant differences for the F. nucleatum (standardized coefficients beta=+0.53).
The beta value of +0.53 indicates that PDT has higher CFU value than the 810 nm diode laser (by 0.5 unit). The former, thus has lower effects on the species F. nucleatum.
More precisely on B value of 0.5, despite the statistical significance, its clinical insignificance can be noted.
Discussion
Based on the results of the present study, using contemporary disinfection methods such as diode laser (810 nm) and PDT as adjuvant in root canal treatments has significantly reduced the CFU/ml. Thus, they have an effective antiseptic feature.
Both methods effectively reduced the CFU/ml without any statistically significant differences.
The results on the disinfection effect of high power diode lasers are consistent with the studies of Preethee et al30 and De Souza et al.31 Using high power diode lasers, Radaelli et al32 also achieved similar results.
The studies mentioned were all in vivo and based on the microbial culture. Preethee et al30 used PCR for microbiological analysis in addition to the microbial culture methods.
In our study, canal disinfection method along with the high power 810 nm diode laser (1.2 W, laser assisted root canal disinfection) significantly reduced all cultured species. Therefore, it can be extended as an adjuvant root treatment for teeth with apical lesions.
Considering available literature, only Jha et al33 study was inconsistent with our results on the use of the diode lasers. Jha et al33 noted the inability of laser and rotary instrumentation in disinfecting the root canal. Moreover, there are concerns on the heat generated by laser radiation. Udart et al showed the thermal mechanism as the only mechanism of inactivating bacteria while using high power 940 nm diode lasers. Inappropriate use of laser parameters could lead to side effects such as burnt dentine, root ankylosis, cement melting, root degeneration and periradicular necrosis.34
In response to these concerns, Alfredo et al35 suggested that application of 980 nm diode laser (1.5 W) in endodontics is safe in all applied modes regardless of the presence/absence of moisture. Radaelli et al32 recorded the maximum temperature changes of 7.45°C (ΔT) following the application of 830 nm diode lasers (3 and 2.5 W) (CW) in the safe area.
One way to reduce the increased heat risk is using of the oscillatory technique developed by Gutknecht et al.36 During the technique, the fiber was directed out of the canal with a helicoidal motion in the speed of 2 mm/s. Moreover, the tissues underwent a relaxation time to modulate temperature changes.
The results of this study on the effect of PDT is consistent with the those of many other studies such as Ng et al,37 Garcez et al,19,22,29,38,39 Bonsor et al,27,28 Fonseca et al,40 Foschi et al,24 Fimple et al,26 William et al,21 and Asnaashari et al.41
Only, Souza et al study elicited opposed results. They concluded that PDT reduces the number of bacteria in the canal in a statistically insignificant manner. Low concentration of available oxygen within the canal is considered as a possible explanation for deficient bacteria removal.42
Fimple et al observed up to 80% reduction in CFU count by using 2 μg/mL MB and 665 nm diode laser (1 W). This study was different from previous studies because of the use of high power output and simultaneous application of Photosensitizer.26
Several studies have been conducted on PDT Safety. Kashef et al concluded that PDT with MB /TBO has no significant cytotoxic effects on human fibroblasts.43
Compared to conventional antimicrobial rinsing solutions, George and Kishen suggested significantly lower cytotoxicity for PDT.44 In an in vitro experimental study, E. faecalis was killed more quickly than normal fibroblasts. PDT kills 97.7% of bacteria while records dysfunction of 30% of fibroblasts.
Xu et al suggested that PDT can inactivate endodontic pathogens without affecting the survival of the host cells.45 Thus, it can be concluded that PDT is a safe and effective method in clinical application. It has the potential to predictably perform the canal disinfection in one visit, reducing the number of therapy sessions.
Since our study found no significant difference between the two methods (high-power diode laser and PDT), PDT method is advantageous over high power diode laser considering the more probable risks of high power diode laser, including: increased heat; burning and root recession. As a result PDT can be noted as an appropriate alternative.
An advantage of this study was the investigation of the effects of each intervention on cultured bacterial species separately, only F. nucleatum species showed different effects of the interventions and more statistical effectiveness from the high-power diode laser than PDT. Moreover, this finding is not clinically important because of low β coefficient (β=0.53)
Another advantage of the current study was the consideration of the difference of CFU at baseline, meaning the difference may cause mistakes in comparing two interventions by over/under estimating. However, lower consequent CFU/mL were due to lower CFU/mL baseline.
In calculations, the significant difference of CFU baseline was considered only for Streptococcus species. Otherwise, the effect of the intervention on consequent CFU would be overestimated.
In this study, quantitative methods were chosen to examine the microorganisms. In some studies, microbiological evaluations are limited to the presence or absence of bacteria (positive or negative cultures) but the present study is important due to the examination of the common endodontic microorganisms.
Since the present study was implemented in vivo, it is more reliable for clinical application. Surrounding tissues generate more reflective scattered beams, leading to more photons available to photoreaction.
Conclusion
After common chemo mechanical treatment, canal disinfection through PDT method or 810 nm diode laser significantly reduced the CFU/ml. These two techniques did not show statistically significant differences and because of lower side effects, PDT could be preferred compared with diode laser (810 nm). Moreover, no significant differences were observed in any kind of bacterial species cultured in the two methods.
Ethical Considerations
The protocol of the clinical trial which was conducted according to the ethical principles of Declaration of Helsinki (version 2002) was approved by the ethical committee of Shahid Beheshti University of Medical Sciences.
Conflict of Interest
There was no conflict of interest for any of the authors to disclose.
Please cite this article as follows: Asnaashari M, Godiny M, Azari-Marhabi S, Tabatabaei FS, Barati M. Comparison of the antibacterial effect of 810 nm diode laser and photodynamic therapy in reducing the microbial flora of root canal in endodontic retreatment in patients with periradicular lesions. J Lasers Med Sci. 2016;7(2):99-104. doi:10.15171/jlms.2016.17.
References
- 1.Siqueira JF. Endodontic infections: concepts, paradigms, and perspectives. Oral Surg Oral Med Oral Pathol. 2002;94(3):281–293. doi: 10.1067/moe.2002.126163. [DOI] [PubMed] [Google Scholar]
- 2.Sjogren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997;30:297–306. doi: 10.1111/j.1365-2591.1997.tb00714.x. [DOI] [PubMed] [Google Scholar]
- 3.Bystrom A, Sundqvist G. Bacteriologic evaluation of the effect of 05 percent sodium hypochlorite in endodontic therapy. Oral Surg Oral Med Oral Pathol. 1983;55:307–312. doi: 10.1016/0030-4220(83)90333-x. [DOI] [PubMed] [Google Scholar]
- 4.Siqueira JF, Araujo MC, Garcia PF, Fraga RC, Dantas CJ. Histological evaluation of the effectiveness of five instrumentation techniques for cleaning the apical third of root canals. J Endod. 1997;23:499–502. doi: 10.1016/s0099-2399(97)80309-3. [DOI] [PubMed] [Google Scholar]
- 5.Mohammadi Z, Palazzi F, Giardino L, Shalavi S. Microbial biofilms in endodontic infections: an update review. Biomed J. 2013;36(2):59–70. doi: 10.4103/2319-4170.110400. [DOI] [PubMed] [Google Scholar]
- 6.Nair PN, Sjogren U, Krey G, Kahnberg KE, Sundqvist G. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod. 1990;16:580–588. doi: 10.1016/s0099-2399(07)80201-9. [DOI] [PubMed] [Google Scholar]
- 7.Boucher Y, Matossian L, Rilliard F, Machtou P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int Endod J. 2002;35(3):229–238. doi: 10.1046/j.1365-2591.2002.00469.x. [DOI] [PubMed] [Google Scholar]
- 8.Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003;36(3):181–192. doi: 10.1046/j.1365-2591.2003.00640.x. [DOI] [PubMed] [Google Scholar]
- 9.Kirkevang LL, Horsted-Bindslev P, Orstavik D, Wenzel A. A comparison of the quality of root canal treatment in two Danish subpopulations examined 1974-75 and 1997-98. Int Endod J. 2001;34(8):607–612. doi: 10.1046/j.1365-2591.2001.00436.x. [DOI] [PubMed] [Google Scholar]
- 10.Asgary S, Shadman B, Ghalamkarpour Z. et al. Periapical status and quality of root canal fillings and coronal restorations in Iranian population. Iran Endod J. 2010;2:74–82. [PMC free article] [PubMed] [Google Scholar]
- 11.Rolph HJ, Lennon A, Riggio MP. et al. Molecular identification of microorganisms from endodontic infections. J Clin Microbiol. 2001;39:3282–3289. doi: 10.1128/jcm.39.9.3282-3289.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siqueira JF. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001;34:1–10. doi: 10.1046/j.1365-2591.2001.00396.x. [DOI] [PubMed] [Google Scholar]
- 13.Hancock HH, Sigurdsson A, Trope M, Moiseiwitsch J. Bacteria isolated after unsuccessful endodontic treatment in a North American population. Oral Surg Oral Med Oral Pathol. 2001;91:579–586. doi: 10.1067/moe.2001.113587. [DOI] [PubMed] [Google Scholar]
- 14.Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod. 2004;30(1):1–11. doi: 10.1097/00004770-200401000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Wilson M. Photolysis of oral bacteria and its potential use in the treatment of caries and periodontal disease: a review. J App Bacteriol. 1993;75:299–306. doi: 10.1111/j.1365-2672.1993.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 16.Soukos NS, Ximenez-Fyvie LA, Hamblin MR, Socransky SS, Hasan T. Targeted antimicrobial photochemotherapy. Antimicrob Agents Chemother. 1998;42:2595–2601. doi: 10.1128/aac.42.10.2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silbert T, Bird PS, Milburn GJ, Walsh L. Disinfection of root canals by laser dye photosensitization. J Dent Res. 2000;79:569. [Google Scholar]
- 18.Seal GJ, Ng YL, Spratt D, Bhatti M, Gulabivala K. An in vitro comparison of the bactericidal efficacy of lethal photosensitization or sodium hyphochlorite irrigation on Streptococcus intermedius biofilms in root canals. Int Endod J. 2002;35:268–274. doi: 10.1046/j.1365-2591.2002.00477.x. [DOI] [PubMed] [Google Scholar]
- 19.Garcez AS, Nunez SC, Lage-Marques JL, Jorge AO, Ribeiro MS. Efficiency of NaOCI and laser-assisted photosensitization on the reduction of Enterococcus faecalis in vitro. Oral Surg Oral Med Oral Pathol. 2006;102:93–98. doi: 10.1016/j.tripleo.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 20.Soukos NS, Chen PS, Morris JT. et al. Photodynamic therapy for endodontic disinfection. J Endod. 2006;32:979–984. doi: 10.1016/j.joen.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 21.William JA. PCars GJ, Colles MJ Antibacterial action of photoactivated disinfection {PAD} used on endodontic bacteria in planktonic suspension and in artificial and human root canals. J Dent. 2006;34:363–371. doi: 10.1016/j.jdent.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Garcez AS, Ribeiro MS, Tegos GP, Nunez SC, Jorge AO, Hamblin MR. Antimicrobial photodynamic therapy combined with conventional endodontic treatment to eliminate root canal biofilm infection. Lasers Surg Med. 2007;39(1):59–66. doi: 10.1002/lsm.20415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.George S, Kishen A. Photophysical, photochemical, and photobiological characterization of methylene blue formulations for light-activated root canal disinfection. J Biomed Opt. 2007;12:34029–34038. doi: 10.1117/1.2745982. [DOI] [PubMed] [Google Scholar]
- 24.Foschi F, Fontana CR, Ruggiero K. et al. Photodynamic inactivation of Enterococcus faecalis in dental root canals in vitro. Lasers Surg Med. 2007;39:782–787. doi: 10.1002/lsm.20579. [DOI] [PubMed] [Google Scholar]
- 25.Bergmans L, Moisiadis P, Huybrechts B, Van Meerbeek B, Quirynen M, Lambrechts P. Effect of photo-activated disinfection on endodontic pathogens ex vivo. Int Endod J. 2008;41:227–239. doi: 10.1111/j.1365-2591.2007.01344.x. [DOI] [PubMed] [Google Scholar]
- 26.Fimple JL, Fontana CR, Foschi F. et al. Photodynamic treatment of endodontic polymicrobial infection in vitro. J Endod. 2008;34(6):728–734. doi: 10.1016/j.joen.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonsor SJ, Nichol R, Reid TM, Pearson GJ. An alternative regimen for root canal disinfection. Br Dent J. 2005;22:101–105. doi: 10.1038/sj.bdj.4813819. [DOI] [PubMed] [Google Scholar]
- 28.Bonsor SJ, Nichol R, Reid TM, Pearson GJ. Microbiological evaluation of photoactivated disinfection in endodontics (an in vivo study) Br Dent J. 2006;25:337–341. doi: 10.1038/sj.bdj.4813371. [DOI] [PubMed] [Google Scholar]
- 29.Garcez AS, Nunez SC, Hamblin MR, Ribeiro MS. Antimicrobial effects of photodynamic therapy on patients with necrotic pulps and periapical lesion. J Endod. 2008;34:138–142. doi: 10.1016/j.joen.2007.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preethee T, Kandaswamy D, Arathi G, Hannah R. Bactericidal effect of the 908 nm diode laser on Enterococcus faecalis in infected root canals. J Conserv Dent. 2012;15(1):46–50. doi: 10.4103/0972-0707.92606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Souza EB, Cai S, Simionato MR, Lage-Marques JL. High-power diode laser in the disinfection in depth of the root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(1):e68–e72. doi: 10.1016/j.tripleo.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Radaelli CM, Zezell DM, Cai S, Antunes A. Effect of a high power diode laser irradiation in root canal contaminated with E faecalis. International Congress Series. 2003;1248:273–276. [Google Scholar]
- 33.Jha D, Guerrero A, Ngo T, Helfer A, Hasselgren G. Inability of laser and rotary instrumentation to eliminate root canal infection. J Am Dent Assoc. 2006;137:67–70. doi: 10.14219/jada.archive.2006.0023. [DOI] [PubMed] [Google Scholar]
- 34.Udart M. Stock K, Graser R, Hibst R Inactivation of bacteria by high-power 940nm laser irradiation. Med Laser Appl. 2011;26:166–171. doi: 10.1016/j.mla.2011.08.004. [DOI] [Google Scholar]
- 35.Alfredo E, Marchesan MA, Sousa-Neto MD, Brugnera JA. Temperature variation at the external root surface During 980 nm diode laser. J Dent. 2008;36:529–538. doi: 10.1016/j.jdent.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 36.Gutknecht N, Moritz A, Conrads G, Sievert T, Lampert F. Bactericidal effect of the Nd: YAG laser in vitro root canal. J Clin laser Med Surg. 1996;14(2):77–80. doi: 10.1089/clm.1996.14.77. [DOI] [PubMed] [Google Scholar]
- 37.Ng R, Singh F, Papamanou D. A, Song Xi Endodontic Photodynamic therapy Ex vivo. J Endod. 2011;31:217–222. doi: 10.1016/j.joen.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garcez AS, Nunez SC, Hamblim MR, Suzuki H. Photodynamic therapy associated with conventional endodontic treatment in patients with Antibiotic-resistant microflora: a preliminary report. J Endod. 2010;36:1463–1466. doi: 10.1016/j.joen.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Garces AS, Nunez SC, Hamblin MR, Michael R. Antimicrobial comparison on effectiveness of endodontic therapy and endodontic therapy combined with photo- disinfection on patients with periapical lesion: a 6 month follow-up. Proc SPIE. 2008;6846:68460G1–68460G7. doi: 10.1117/12.763705. [DOI] [Google Scholar]
- 40.Fonseca MB, Junior Po, Pullota RC, Filho HF. Photodynamic therapy for root canals infected with Enterococcus faecalis. Photomed Laser Surg J. 2008;26:209–213. doi: 10.1089/pho.2007.2124. [DOI] [PubMed] [Google Scholar]
- 41.Asnaashari M, Mojahedi SM, Asadi Z, Azari-Marhabi S, Maleki A. A comparison of the antibacterial activity of the two methods of photodynamic therapy (using diode laser 810 nm and LED lamp 630 nm) against Enterococcus faecalis in extracted human anterior teeth. Photodiagnosis Photodyn Ther. 2016;13:233–237. doi: 10.1016/j.pdpdt.2015.07.171. [DOI] [PubMed] [Google Scholar]
- 42.Souza LC, Brito PR, Deoliveira JC, Alves FR. Photodynamic therapy with two different photosensitizers as a supplement to instrumentation/irrigation procedures in Promoting Intracanal reduction of Enterococcus faecalis. J Endod. 2010;36:292–296. doi: 10.1016/j.joen.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 43.Kashef N, Sharif Abadi GR, Esmaeeli D, Javid G. Photodynamic in activation of primary human fibroblast by MB and TBO. Photodiagnosis Photodyn Ther. 2012;9:355–358. doi: 10.1016/j.pdpdt.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 44.George S, Kishen A. Advanced noninvasive light- activated disinfection: assessment of cytotoxicity on fibroblast versus antimicrobial activity against Enterococcus faecalis. J Endod. 2007;33:599–602. doi: 10.1016/j.joen.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 45.Xu Y, Young MJ, Battaglino RA. et al. Endodontic antimicrobial photodynamic therapy: safety assessment in mammalian cell cultures. J Endod. 2009;35(11):1567–1572. doi: 10.1016/j.joen.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


